Abstract
AIM
To investigate and summarise the current evidence surrounding management of Bouveret’s syndrome (BS).
METHODS
A MEDLINE search was performed for the BS. The search was conducted independently by two clinicians (Yahya AL-Habbal and Matthew Ng) in April 2016. A case of BS is also described.
RESULTS
A total of 315 articles, published from 1967 to 2016, were found. For a clinically meaningful clinical review, articles published before 01/01/1990 and were excluded, leaving 235 unique articles to review. Twenty-seven articles were not available (neither by direct communication nor through inter-library transfer). These were also excluded. The final number of articles reviewed was 208. There were 161 case reports, 13 reviews, 23 images (radiological and clinical images), and 11 letters to editor. Female to male ratio was 1.82. Mean age was 74 years. Treatment modalities included laparotomy in the majority of cases, laparoscopic surgery, endoscopic surgery and shockwave lithotripsy.
CONCLUSION
There is limited evidence in the literature about the appropriate approach. We suggest an algorithm for management of BS.
Keywords: Bouveret’s syndrome, Biliary anomalies, Endoscopy, Digestive system, Duodenal obstruction diagnosis, Gallstones surgery, Gallstones complications, Duodenal obstruction etiology, Duodenal obstruction surgery, Intestinal fistula diagnosis, Humans
Core tip: Bouveret’s syndrome is gastric outlet obstruction secondary to an impacted gallstone in the duodenum or stomach. There is limited evidence surrounding management of this rare syndrome. Here we systematically review the published cases and recommend a treatment algorithm to clinicians facing this syndrome in future.
INTRODUCTION
Bouveret’s syndrome (BS) was first described by Beaussier in 1770, but reported in the literature first by Leon Bouveret in 1896, where he had two cases[1]. Leon Bouveret was actually an internist but supported surgery[2]. BS is gastric outlet obstruction secondary to a gallstone impacted in the duodenum or stomach.
We report a 39-year-old lady who presented with upper abdominal pain and vomiting. She was diagnosed with BS after scans and endoscopy. Her gallstone was successfully removed by gastroscopy. Though her symptoms continued, a literature review was sought to manage her according to the recent evidence. Almost all the case reports and limited case series were in favour of conservative management. She was managed expectantly, but represented with ongoing pain.
The patient underwent laparoscopic cholecystectomy. The fistula was dissected and closed laparoscopically. On intra-operative cholangiogram, she had more bile duct stones which were treated by laparoscopic bile duct exploration and stone extraction. She did well in the post-operative course.
MATERIALS AND METHODS
MEDLINE and PubMed searches were performed for the terms BS. The search was conducted in April 2016. Three hundred and fifteen articles, published between 1967 and 2016, were identified. For a clinically meaningful clinical review, articles published before 01/01/1990 and were excluded, leaving 235 unique articles to review. Twenty-seven articles were not available (neither by direct communication nor through inter-library transfer). The final number of articles reviewed was 208 (Figure 1A).
Figure 1.
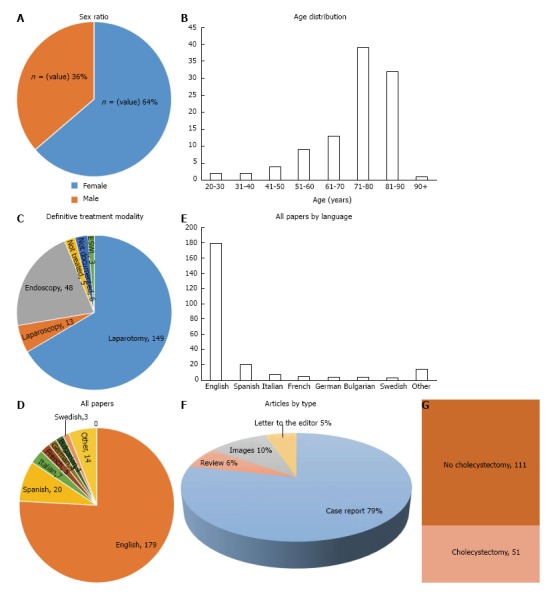
MEDLINE and PubMed searches were performed for the terms Bouveret’s syndrome. A: Sixty-four percent of the identified cases in the literature were female; B: Bouveret’s syndrome is more common in elderly patients, with the majority of cases occurring above 71 years of age; C: While some cases were successfully treated endoscopically, the majority of cases require open surgical management; D and E: Articles not in English were translated to English using dependable medical dictionaries; F: Results of the literatures; G: In patients receiving surgical stone retrieval, the majority did not receive a concurrent or delayed cholecystectomy.
Data from retrieved articles were independently reviewed by the two authors (Yahya AL-Habbal and Matthew Ng) and data was extracted using a standardised collection tool. Data was analysed with descriptive statistics. In contrast to classic meta-analyses, statistical analysis was performed where the outcome was calculated as the percentages of an event (without comparison) in pseudo-cohorts of observed patients.
RESULTS
Articles comprised 161 case reports[3-163], 13 reviews[164-176], 23 images reports (radiological and clinical images[177-198] and 11 letters to the editor[199-209], as illustrated in (Figure 1F).
Articles were written in multiple languages. English articles constituted the main bulk of the literature (176 articles, 77%). The rest were Spanish (20 articles, 9%), Italian (7 articles, 3%) French (5 articles, 2%), and other languages (13%). These other languages include: Bulgaria, South Korean, Japanese, German, Romanian, Turkish, Hungarian, Ukrainian, and Czech. Articles not in English were translated to English using dependable medical dictionaries (Figure 1D and E).
A 39 years old lady presenting to the emergency department with two-week history of epigastric and right upper quadrant pain. The pain was constant, dull, and radiating to the back, she had acidity and reflux symptoms, nausea and vomiting. There was no history of jaundice, or weight loss.
On examination she was mildly dehydrated. Pulse rate was 92 beats/min and temperature was 37.3°. She was tender in the epigastrium and right upper quadrant, with a negative Murphy’s sign.
Initial blood tests showed high white cells count 13.9 × 109. Her liver functions were deranged. Bilirubin was 14 IU/L, ALP 285 IU/L, ALT 335 IU/L, GGT 445 IU/L, and ALT 0f 205 IU/L. Her lipase was mildly raised at 455 IU/L (normal range < 45 IU/L).
With this mixed picture the initial differential diagnosis was cholangitis or pancreatitis, or Mirrizzi syndrome.
The patient was referred for an ultrasound (US) scan. The images were degraded by pneumobilia and, while difficult to characterize, demonstrated a contracted gallbladder without stones. Common bile duct was 10 mm with mild intrahepatic biliary tree dilatation (Figure 2). CT scan obtained to further characterize the gallbladder demonstrated large-volume pneumobilia, a fistula between the distal stomach and the collapsed gallbladder, and oral contrast in the region of the gallbladder neck.
Figure 2.
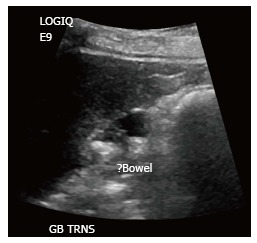
Common bile duct was 10 mm with mild intrahepatic biliary tree dilatation.
There was an opacity in the stomach that was interpreted as hypo-dense gallstone in the stomach (Figures 3 and 4). At this point the diagnosis of cholecysto-gastric fistula secondary to gallstone disease with subsequent intermittent gastric outlet was made.
Figure 3.

Coronal section of computed tomography scan.
Figure 4.

Cross section of computed tomography scan showing gallstone in the stomach and pneumobilia. The gallbladder is contracted and gas-filled.
Upper GI endoscopy confirmed the presence of gallstone in the stomach and fistula orifice (Figure 5). The stone was successfully retrieved by snare (Figure 6). Patient’s symptoms improved significantly and ultimately discharged home after 2 d. Her liver functions normalized before discharge. Given that there was no evidence of any further gallstones, and after reviewing the current evidence and practice, we decided to manage her expectantly.
Figure 5.
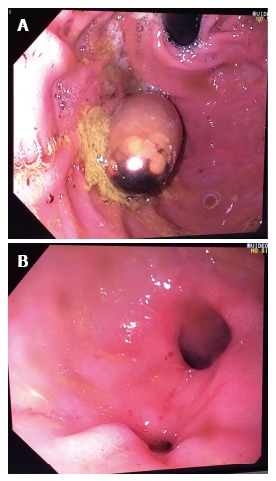
Upper gastrointestinal endoscopy confirmed the presence of gallstone in the stomach (A) and fistula orifice (B).
Figure 6.

The stone was successfully retrieved by snare.
Upon follow up, it was found that the patient was still complaining of abdominal pain. An MRCP done at this point that showed more gallstones have fallen into the bile duct.
She underwent a laparoscopic cholecystectomy. The operation revealed adhesions between the gallbladder and distal stomach. No real fistular tract was seen, but dense adhesions were ligated by an Endoloop. Intra-operative cholangiogram confirmed bile duct stones. These were difficult to be retrieved by trans-cystic exploration. A laparoscopic bile duct exploration was performed. Several stones were successfully retrieved. Bile duct repaired primarily by 4/0 monofilament non-absorbable suture material. The postoperatrive course has been uneventful.
DISCUSSION
BS is a rare cause of gastric outlet obstruction caused by gallstones. The stone(s) tend to migrate secondary to fistulation. The fistula can be cholecystogastric (less common) or more commonly, cholecystoduodenal. BS constitutes 1%-3% of cases of gall stone ileus which in turn complicates only 0.3%-4% cases of cholelithisasis[91,107]. BS can be associated with high mortality (up to 12%) mainly due to the frailty of patients[136]. The pathophysiology is usually caused by prolonged pressure, ischemia, and then fistulation and stone migration. The stone(s) then obstruct the gastric outlet or duodenum. A collection of small stones can produce the same picture[210]. Malignancy can also produce fistulation and stone migration. This has been reported by Sharma et al[35] where the patient underwent laparotomy and stone extraction with gastro-jejunostomy to relieve the obstruction, while Shinoda et al[34] offered a curative cancer resection and fistula repair in a similar case of fistulating cancer.
In one interesting variant of BS, a patient presented with upper abdominal pain 10 years after Roux-en-Y Billroth II resection for benign disease. A stone retrieved from the duodenum after laparotomy[64]. There have been a few cases in the literature where BS presented with pancreatitis[33,122]. The stone(s) can be lodged tightly in the duodenum causing necrosis and intra or extra-peritoneal perforation[109].
BS has been reported many times as a single case report. A few reports included more than one case[99,130,153,160,163,173,188]. These patients usually present with abdominal pain and vomiting as universally reported. There was one case in which the vomiting was severe to the point of causing Boerhaaves oesophageal rupture[63]. The diagnosis is usually late given the uncommon and vague nature of its symptoms. In about one-third of cases the diagnosis can be made by a plain abdominal film that demonstrates the classical Rigler’s triad of a dilated stomach, pneumobilia, and a radio-opaque shadow in the region of the duodenum representing the ectopic gallstone[47,209-213]. There have been some reported cases of migrating stone into the mediastinum after relieving an obstructed duodenum of BS via endoscope[71]. Ultrasound can be helpful as indicated in some papers[184], but the study can be greatly degraded by the presence of gas in the biliary tree. Historical data shows that the diagnosis has only been made preoperatively in 50% of cases[80]. Due to the nearby inflammation, the gallbladder can be FDG/PET positive[178].
Spontaneous resolution can occur when the impacted stone falls back away from the pyloric orifice[16], but this can be associated with further bowel obstruction distal to the stomach and duodenum (gall stone ileus)[114,141]. On the other hand, the condition can be fatal due to the profound metabolic derangement[13], and later by sepsis and multi-organ failure[62].
In our review, the sex (female to male) ratio was (1.82), female being 64% and male being 36% (Figure 1A). Age distribution of these cases showed majority of cases being elderly patients above 60 years old with the average age of (74 ± 13), and minority less than 30 years old (Figure 1B).
There are multiple available treatment modalities. This includes laparotomy, laparoscopy, endoscopy and ESWL (Figure 1C). Majority of cases were treated with laparotomy and stone extraction through either an enterotomy or gastrotomy (146 cases, 71%). Successful laparoscopic treatment was also possible (13 cases, 6%). Some of patients had a radical procedure where the procedure was combined with cholecystectomy (51 cases, 25%), as illustrated in (Figure 1G). The advantages of doing cholecystectomy is not only removing the source of stones, but eliminating the theoretical carcinogenic risk of gastro-intestinal juices contacting the biliary tree[212]. Cholecystectomy has been described as a single procedure combined with fistula dissection and closure, or as a separate procedure done later on elective or semi-urgent basis (like our case).
With the recent advents in endoscopic technology, endoscopic treatment was tried in 160 cases (77%) and was successful in removing the stone in 46 cases of patients (29%). This was either through direct visualization and retrieval of the stone or combined with a lithotripsy method (laser, mechanical, shockwave). This is more than the reported 10% success rate in earlier narrative review of BS[168]. In recent years, therapeutic endoscopy has been more frequently and successfully used to extract the obstructing stone(s). This might be attributed to improved lithotripsy, better optical instruments and improved graspers and nets to extract gallstones.
Extracorporeal shock-wave lithotripsy (ESWL) has been described by Gemmel et al[115], Chick et al[181], Dumonceau et al[130] and Tanwar et al[23] which was successful combined with either endoscopy alone or laparotomy to remove stone fragments from distal bowels. Intracorporeal lithotripsy using water jet[6], or other mechanical methods[139], have been described.
It is estimated that up to 90% of patients will need some form of surgical intervention[173]. These interventions can vary but mainly depend on the patient’s age and co-morbidities. The vast majority of these stones pass spontaneously without producing obstruction. Stones that obstruct the digestive tract are usually greater than 2-2.5 cm in diameter[175]. Cholecystostomy has been tried to treat associated cholecystitis but this has not been associated with a great deal of success[145]. Sometimes, to alleviate the obstruction and allow patients to eat and drink, an interim bypass procedure has been described[53]. Subtotal cholecystectomy and drain tube insertion is another option which is safe and successful[8,178].
A minority of cases in the literature were not treated due to either severely compromised patients or spontaneous resolution (5 cases, 2%). In addition, there were some reports where the treatment modality was not mentioned (6 cases, 3%).
After reviewing the (review) articles of BS, it was noted the majority of these reviews are more or less narrative reviews and not systematic, except three reviews[165,166,170]. A summary of these articles can be found in Table 1. There were issues with the previously done reviews being either limited to English language (thus excluding almost 15% of the literature) or incomplete not including all the papers. The limitation of our paper is the fact that we excluded 27 articles as we could not get them through multiple available channels. But almost all of these articles were published prior to 1995 and are case reports including single cases, or images for doctors.
Table 1.
Review articles
| Ref. | Year | No. articles | No. cases | Age (mean ± SD) | %Female | Endoscopy performed | Nonsurgical treatment success | Enterolithotomy | Cholecystectomy | Mortality/major complications |
| Cappell et al[165] | 2006 | 111 | 128 | 74.1 ± 11.1 | 65.10% | 63% | 18.00% | 98/128 = 76.6% | 40/98 = 40.8% | 16/98 = 16.3% |
| Lowe et al[170] | 2005 | 39 | 44 | 73 ± 13.5 | 68% | 51% | 13.60% | 40/44 = 90.9% | 36% | 19%-24% |
| Frattaroli et al[166] | 1997 | 79 | 79 | 68.6 | 65% | 60% | 14% | 93% | Not reported | 12%-33% |
Finally, the term pseudo BS has been used in the literature once to describe the condition of gall stones and gastric outlet obstruction due to external duodenal or pyloric compression (akin to Mirizzi’s type I)[213].
In conclusion, with the current paucity of high level of scientific evidence about BS, the management remains highly arbitrary. Here we present a young patient with BS who failed conservative measures, and suggest a treatment algorithm for these patients. The management of this uncommon condition should be tailored to the patient’s clinical presentation and morbidities. Perhaps a more radical treatment (which might include cholecystectomy) should be offered to young patients and patients with ongoing symptoms. Whenever possible, endoscopic approach should be offered first after immediate resuscitation, with stone extraction and lithotripsy as two options. If that fails, surgical management with enterolithotomy or gastrolithotomy depended on stone position. We do not recommend immediate cholecystectomy or fistula dissection as this can be associated with significant morbidity and mortality. Delayed cholecystectomy and fistula repair should be offered electively to patients with persistent symptoms or patients younger than 50 years old.
ACKNOWLEDGMENTS
Eastern Health Library Service, Box Hill Library, Victoria, Australia for their assistance in retrieving full-text articles.
COMMENTS
Background
Bouveret’s syndrome (BS) is a rare complication of gallstone disease, where a gallstone erodes into the duodenum and causes gastric outlet obstruction following impaction in the stomach or duodenum. The stone must be removed to restore normal function of the gastrointestinal tract. This may be done via laparotomy or laparoscopic stone removal, or more recently, using lithotripsy with or without endoscopic retrieval to dislodge the stone.
Research frontiers
The literature surrounding BS is sparse and consists mainly of case reports and series. Reviews of these cases have been few and far between, with the most recent dating back to 2006. In this time, endoscopy, endoscopic interventions, and laparoscopy have improved, potentially offering new options for managing these patients.
Innovations and breakthroughs
In this study the authors systematically reviewed the published cases of BS from 1990 to the present. While laparotomy and laparoscopy were performed in a significant number of cases, endoscopic treatment has become much more successful with the advent of improved lithotripsy, improved endoscopic retrieval devices, and improved visualisation. Extracorporeal shockwave lithotripsy has also been successfully used in multiple cases.
Applications
They recommend that patients presenting with BS should be initially managed with attempted endoscopic retrieval, with or without lithotripsy, followed by open or laparoscopic surgical retrieval via enterotomy or gastrotomy if unsuccessful. In younger, healthier patients, a delayed cholecystectomy may be performed, however in older or multiply comorbid patients, this may be omitted from the treatment algorithm.
Terminology
BS is gastric obstruction due to an impacted gallstone in the duodenum or gastric outlet. Lithotripsy is the act of breaking a stone into multiple smaller pieces. This may be effected with extracorporeal shock waves, using a mechanical lithotripter, or a laser device.
Peer-review
In this systematic review, the authors have presented a thorough and critical analysis of the published cases of BS, and recommended an appropriate treatment algorithm for future cases.
Footnotes
Conflict-of-interest statement: The authors declare no conflicts of interest regarding this manuscript.
Data sharing statement: The dataset and statistical analysis is available from the corresponding author at yahya.al-habbal@easternhealth.org.au.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Australia
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: September 6, 2016
First decision: September 29, 2016
Article in press: December 9, 2016
P- Reviewer: Du JJ, He ST, Liu BR S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
References
- 1.Melamed JL, Parker ML. Cholecystogastric fistula; report of a case. J Am Med Assoc. 1956;160:463–464. doi: 10.1001/jama.1956.02960410039009a. [DOI] [PubMed] [Google Scholar]
- 2.Wickbom G. [The man behind the syndrome: Leon Bouveret. The internist who supported surgery] Lakartidningen. 1993;90:162, 165. [PubMed] [Google Scholar]
- 3.Zoricić I, Vukusić D, Rasić Z, Trajbar T, Sever M, Lojo N, Crvenković D. [Bile stone ileus with cholecystoduodenal fistula--Bouveret’s syndrome] Acta Med Croatica. 2011;65:63–66. [PubMed] [Google Scholar]
- 4.Zafar A, Ingham G, Jameel JK. “Bouveret’s syndrome” presenting with acute pancreatitis a very rare and challenging variant of gallstone ileus. Int J Surg Case Rep. 2013;4:528–530. doi: 10.1016/j.ijscr.2013.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu K, Yang J, Zhen J, Zhou X. Bouveret’s syndrome: a rare cause of gastric outlet obstruction. Chin Med J (Engl) 2014;127:3377. [PubMed] [Google Scholar]
- 6.Yokoyama T, Ashizawa T, Hibi K, Okada R, Suzuki Y, Takagi M, Shinohara Y, Sugimoto K, Aoki T. [A case of gastric outlet obstruction by gallstone (Bouveret’s syndrome) treated by EHL] Nihon Shokakibyo Gakkai Zasshi. 2005;102:1293–1298. [PubMed] [Google Scholar]
- 7.Yau KK, Siu WT, Tsui KK. Migrating gallstone: from Bouveret’s syndrome to distal small bowel obstruction. J Laparoendosc Adv Surg Tech A. 2006;16:256–260. doi: 10.1089/lap.2006.16.256. [DOI] [PubMed] [Google Scholar]
- 8.Yang D, Wang Z, Duan ZJ, Jin S. Laparoscopic treatment of an upper gastrointestinal obstruction due to Bouveret’s syndrome. World J Gastroenterol. 2013;19:6943–6946. doi: 10.3748/wjg.v19.i40.6943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong CS, Crotty JM, Naqvi SA. Pneumobilia: a case report and literature review on its surgical approaches. J Surg Tech Case Rep. 2013;5:27–31. doi: 10.4103/2006-8808.118616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wonaga A, Fritz V, D’Alessandro M, Waldbaum C. [Bouveret syndrome: unusual cause of upper gastrointestinal bleeding] Acta Gastroenterol Latinoam. 2010;40:159–161. [PubMed] [Google Scholar]
- 11.Wittenburg H, Mössner J, Caca K. Endoscopic treatment of duodenal obstruction due to a gallstone (“Bouveret’s syndrome”) Ann Hepatol. 2005;4:132–134. [PubMed] [Google Scholar]
- 12.Williams NE, Gundara JS, Roser S, Samra JS. Disease spectrum and use of cholecystolithotomy in gallstone ileus transection. Hepatobiliary Pancreat Dis Int. 2012;11:553–557. doi: 10.1016/s1499-3872(12)60224-0. [DOI] [PubMed] [Google Scholar]
- 13.Wight CO, Seed M, Yeo WW, McCulloch TA. Gastric outflow obstruction caused by gall stones and leading to death by complex metabolic derangement. J Clin Pathol. 1997;50:963–965. doi: 10.1136/jcp.50.11.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Werner CR, Graepler F, Glatzle J, Stüker D, Kratt T, Schmehl J, Bitzer M, Königsrainer A, Malek NP, Goetz M. Proximal duodenal obstruction--Bouveret’s syndrome revisited. Endoscopy. 2013;45 Suppl 2 UCTN:E231–E232. doi: 10.1055/s-0033-1344324. [DOI] [PubMed] [Google Scholar]
- 15.Warren DJ, Peck RJ, Majeed AW. Bouveret’s Syndrome: a Case Report. J Radiol Case Rep. 2008;2:14–17. doi: 10.3941/jrcr.v2i4.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wagholikar GD, Ibrarullah M. Bouveret’s syndrome--an unusual cause of spontaneous resolution of gastric outlet obstruction. Indian J Gastroenterol. 2004;23:109–110. [PubMed] [Google Scholar]
- 17.Vigneri S, Scialabba A, Termini R, Fornaciari M, Ficano L, Pintacuda S. A temporary endoscopic solution that significantly improves the prognosis of Bouveret’s syndrome. Surg Endosc. 1991;5:226–228. doi: 10.1007/BF02653271. [DOI] [PubMed] [Google Scholar]
- 18.Venkatesh SK, Thyagarajan MS, Gujral RB, Gupta A. Sonographic diagnosis of Bouveret’s syndrome. J Clin Ultrasound. 2003;31:163–166. doi: 10.1002/jcu.10149. [DOI] [PubMed] [Google Scholar]
- 19.Veloso N, Silva JD, Pires S, Godinho R, Medeiros I, Gonçalves L, Viveiros C. Bouveret’s syndrome. Gastroenterol Hepatol. 2014;37:523–524. doi: 10.1016/j.gastrohep.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 20.Van Dam J, Steiger E, Sivak MV. Giant duodenal gallstone presenting as gastric outlet obstruction: Bouveret‘s syndrome. J Clin Gastroenterol. 1992;15:150–153. doi: 10.1097/00004836-199209000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Thomson WL, Miranda S, Reddy A. An unusual presentation of cholecystoduodenal fistula: vomiting of gallstones. BMJ Case Rep 2012; 2012 doi: 10.1136/bcr-2012-007009. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thompson RJ, Gidwani A, Caddy G, McKenna E, McCallion K. Endoscopically assisted minimally invasive surgery for gallstones. Ir J Med Sci. 2009;178:85–87. doi: 10.1007/s11845-007-0096-9. [DOI] [PubMed] [Google Scholar]
- 23.Tanwar S, Mawas A, Tutton M, O’Riordan D. Successful Endoscopic Management of Bouveret’s Syndrome in a Patient with Cholecystoduodenocolic Fistulae. Case Rep Gastroenterol. 2008;2:346–350. doi: 10.1159/000151581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tan YM, Yeo AW, Wong CY. Multiple giant duodenal gallstones causing gastric outlet obstruction: Bouveret’s minefield revisited. Hepatogastroenterology. 2003;50:1975–1977. [PubMed] [Google Scholar]
- 25.Stein PH, Lee C, Sejpal DV. A Rock and a Hard Place: Successful Combined Endoscopic and Surgical Treatment of Bouveret’s Syndrome. Clin Gastroenterol Hepatol. 2015;13:A25–A26. doi: 10.1016/j.cgh.2015.07.044. [DOI] [PubMed] [Google Scholar]
- 26.Solmaz Tuncer A, Gürel S, Coşgun Z, Büber A, Cakmaz R, Hasdemir OA. A Rare Presentation of Xanthogranulomatous Cholecystitis as Bouveret’s Syndrome. Case Rep Radiol. 2012;2012:402768. doi: 10.1155/2012/402768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smolilo D, Bhandari M, Wilson TG, Brooke-Smith M, Watson DI. Bouveret’s syndrome: gastric outlet obstruction caused by a gallstone. ANZ J Surg. 2013;83:996–997. doi: 10.1111/ans.12227. [DOI] [PubMed] [Google Scholar]
- 28.Smith Z, Totten J, Hughes A, Strote J. Delayed diagnosis of gastric outlet obstruction from bouveret syndrome in a young woman. West J Emerg Med. 2015;16:151–153. doi: 10.5811/westjem.2014.10.23049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh AK, Shirkhoda A, Lal N, Sagar P. Bouveret’s syndrome: appearance on CT and upper gastrointestinal radiography before and after stone obturation. AJR Am J Roentgenol. 2003;181:828–830. doi: 10.2214/ajr.181.3.1810828. [DOI] [PubMed] [Google Scholar]
- 30.Simůnek R, Bohatá S, Kala Z. [Bouveret’s syndrome--a rare case of proximal ileus of biliary etiology] Rozhl Chir. 2009;88:119–122. [PubMed] [Google Scholar]
- 31.Simpson J, Lobo D. Gastrointestinal: Bouveret’s syndrome. J Gastroenterol Hepatol. 2014;29:1339. doi: 10.1111/jgh.12629. [DOI] [PubMed] [Google Scholar]
- 32.Simonek J, Lischke R, Drábek J, Pafko P. [Bouveret’s syndrome: biliary ileus manifested by acute upper gastrointestinal hemorrhage and impaired gastric emptying] Rozhl Chir. 2002;81:259–261. [PubMed] [Google Scholar]
- 33.Sica GS, Sileri P, Gaspari AL. Laparoscopic treatment of Bouveret’s syndrome presenting as acute pancreatitis. JSLS. 2005;9:472–475. [PMC free article] [PubMed] [Google Scholar]
- 34.Shinoda M, Aiura K, Yamagishi Y, Masugi Y, Takano K, Maruyama S, Irino T, Takabayashi K, Hoshino Y, Nishiya S, et al. Bouveret’s syndrome with a concomitant incidental T1 gallbladder cancer. Clin J Gastroenterol. 2010;3:248–253. doi: 10.1007/s12328-010-0170-0. [DOI] [PubMed] [Google Scholar]
- 35.Sharma D, Jakhetia A, Agarwal L, Baruah D, Rohtagi A, Kumar A. Carcinoma Gall Bladder with Bouveret’s Syndrome: A Rare Cause of Gastric Outlet Obstruction. Indian J Surg. 2010;72:350–351. doi: 10.1007/s12262-010-0145-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shah SK, Walker PA, Fischer UM, Karanjawala BE, Khan SA. Bouveret syndrome. J Gastrointest Surg. 2013;17:1720–1721. doi: 10.1007/s11605-013-2244-z. [DOI] [PubMed] [Google Scholar]
- 37.Sethi S, Kochar R, Kothari S, Thosani N, Banerjee S. Good Vibrations: Successful Endoscopic Electrohydraulic Lithotripsy for Bouveret’s Syndrome. Dig Dis Sci. 2015;60:2264–2266. doi: 10.1007/s10620-014-3424-8. [DOI] [PubMed] [Google Scholar]
- 38.Schweiger F, Shinder R. Duodenal obstruction by a gallstone (Bouveret’s syndrome) managed by endoscopic stone extraction: a case report and review. Can J Gastroenterol. 1997;11:493–496. doi: 10.1155/1997/182768. [DOI] [PubMed] [Google Scholar]
- 39.Sans M, Feu F, Panés J, Piqué JM, Terés J. [Duodenal obstruction by biliary lithiasis (Bouveret’s syndrome)] Gastroenterol Hepatol. 1996;19:519–520. [PubMed] [Google Scholar]
- 40.Sánchez Sánchez MR, Bouzón Caamaño F, Carreño Villarreal G, Alonso Blanco RA, Galarraga Gay MA, Alvarez Obregón R. [Bouveret syndrome. A case-report] Rev Clin Esp. 2003;203:399–400. doi: 10.1157/13049441. [DOI] [PubMed] [Google Scholar]
- 41.Salah-Eldin AA, Ibrahim MA, Alapati R, Muslah S, Schubert TT, Schuman BM. The Bouveret syndrome: an unusual cause of hematemesis. Henry Ford Hosp Med J. 1990;38:52–54. [PubMed] [Google Scholar]
- 42.Sakarya A, Erhan MY, Aydede H, Kara E, Ozkol M, Ilkgül O, Ozsoy Y. Gallstone ileus presenting as gastric outlet obstruction (Bouveret’s syndrome): a case report. Acta Chir Belg. 2006;106:438–440. doi: 10.1080/00015458.2006.11679926. [DOI] [PubMed] [Google Scholar]
- 43.Sağlam F, Sivrikoz E, Alemdar A, Kamalı S, Arslan U, Güven H. Bouveret syndrome: A fatal diagnostic dilemma of gastric outlet obstruction. Ulus Travma Acil Cerrahi Derg. 2015;21:157–159. doi: 10.5505/tjtes.2015.62558. [DOI] [PubMed] [Google Scholar]
- 44.Rossi D, Khan U, McNatt S, Vaughan R. Bouveret syndrome: a case report. W V Med J. 2010;106:18–22. [PubMed] [Google Scholar]
- 45.Rogart JN, Perkal M, Nagar A. Successful Multimodality Endoscopic Treatment of Gastric Outlet Obstruction Caused by an Impacted Gallstone (Bouveret’s Syndrome) Diagn Ther Endosc. 2008;2008:471512. doi: 10.1155/2008/471512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reinhardt SW, Jin LX, Pitt SC, Earl TM, Chapman WC, Doyle MB. Bouveret’s syndrome complicated by classic gallstone ileus: progression of disease or iatrogenic? J Gastrointest Surg. 2013;17:2020–2024. doi: 10.1007/s11605-013-2301-7. [DOI] [PubMed] [Google Scholar]
- 47.Rehman A, Hasan Z, Saeed A, Jamil K, Azeem Q, Zaidi A, Abduallah K, Rustam T. Bouveret’s syndrome. J Coll Physicians Surg Pak. 2008;18:435–437. [PubMed] [Google Scholar]
- 48.Rahelić V, Zelić M, Grbas H, Depolo A, Kezele B. Bouveret’s syndrome--case report. Zentralbl Chir. 2009;134:260–262. doi: 10.1055/s-0028-1098694. [DOI] [PubMed] [Google Scholar]
- 49.Radonak J, Vajó J, Jéger T, Stebnický M, Eperjesi O. [Recurrent acute hemorrhage in the duodenum as a symptom of Bouveret’s syndrome] Rozhl Chir. 2000;79:228–230. [PubMed] [Google Scholar]
- 50.Qamrul Arfin SM, Haqqi SA, Shaikh H, Wakani AJ. Bouveret’s syndrome: successful endoscopic treatment of gastric outlet obstruction caused by an impacted gallstone. J Coll Physicians Surg Pak. 2012;22:174–175. [PubMed] [Google Scholar]
- 51.Puri V, Lee RW, Amirlak BA, Lanspa SJ, Fitzgibbons RJ. Bouveret syndrome and gallstone ileus. Surg Laparosc Endosc Percutan Tech. 2007;17:328–330. doi: 10.1097/SLE.0b013e31806c7dc2. [DOI] [PubMed] [Google Scholar]
- 52.Polistena A, Santi F, Tiberi R, Bagarani M. Endoscopic treatment of Bouveret’s syndrome. Gastrointest Endosc. 2007;65:704–706. doi: 10.1016/j.gie.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 53.Pissas A, Mingat J, Massot C, Vincent J, Bouchet Y. [An usual observation of Bouveret syndrome (author’s transl)] Sem Hop. 1981;57:1740–1742. [PubMed] [Google Scholar]
- 54.Pickhardt PJ, Friedland JA, Hruza DS, Fisher AJ. Case report. CT, MR cholangiopancreatography, and endoscopy findings in Bouveret’s syndrome. AJR Am J Roentgenol. 2003;180:1033–1035. doi: 10.2214/ajr.180.4.1801033. [DOI] [PubMed] [Google Scholar]
- 55.Patel JC, Lesur G, De Cervens T, Renier JF, Hardy C, Favas A, Gompel H, Dupuy P. [Antropyloric lithiasic obstruction. A variant of Bouveret’s syndrome] Chirurgie. 1991;117:417–419. [PubMed] [Google Scholar]
- 56.Panov TA, Kiossev KT, Losanoff JE. Bouveret’s syndrome: a rare consequence of malignant cholecystoduodenal fistula. Mil Med. 1994;159:755–757. [PubMed] [Google Scholar]
- 57.Palomeque-Jiménez A, Calzado-Baeza S, Reyes-Moreno M. Bouveret syndrome: an infrequent presentation of gallstone ileus. Rev Esp Enferm Dig. 2012;104:324–325. doi: 10.4321/s1130-01082012000600008. [DOI] [PubMed] [Google Scholar]
- 58.O’Neill C, Colquhoun P, Schlachta CM, Etemad-Rezai R, Jayaraman S. Gastric outlet obstruction secondary to biliary calculi: 2 cases of Bouveret syndrome. Can J Surg. 2009;52:E16–E18. [PMC free article] [PubMed] [Google Scholar]
- 59.O’Dwyer JC, O’Dwyer HM, Lee MJ. Bouveret’s syndrome: a rare complication of cholecystolithiasis. Australas Radiol. 2005;49:427–429. doi: 10.1111/j.1440-1673.2005.01477.x. [DOI] [PubMed] [Google Scholar]
- 60.Nyui S, Osanai H, Masuoka H, Ohba S, Ebata T, Yoshida Y. Gastric outlet syndrome caused by a gallstone: report of a case. Surg Today. 1998;28:412–415. doi: 10.1007/s005950050152. [DOI] [PubMed] [Google Scholar]
- 61.Newton RC, Loizides S, Penney N, Singh KK. Laparoscopic management of Bouveret syndrome. BMJ Case Rep 2015; 2015 doi: 10.1136/bcr-2015-209869. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nabais C, Salústio R, Morujão I, Sousa FV, Porto E, Cardoso C, Fradique C. Gastric outlet obstruction in a patient with Bouveret’s syndrome: a case report. BMC Res Notes. 2013;6:195. doi: 10.1186/1756-0500-6-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Modi BP, Owens C, Ashley SW, Colson YL. Bouveret meets Boerhaave. Ann Thorac Surg. 2006;81:1493–1495. doi: 10.1016/j.athoracsur.2005.04.049. [DOI] [PubMed] [Google Scholar]
- 64.Mittal S, Sutcliffe RP, Rohatgi A, Atkinson SW. A possible variant of Bouveret’s syndrome presenting as a duodenal stump obstruction by a gallstone after Roux-en-Y gastrectomy: a case report. J Med Case Rep. 2009;3:7301. doi: 10.1186/1752-1947-3-7301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Menon NJ, Reid PJ, Ribeiro BF. Bouveret’s syndrome: an unusual case of pyloroduodenal obstruction. Hosp Med. 2002;63:432–433. doi: 10.12968/hosp.2002.63.7.1990. [DOI] [PubMed] [Google Scholar]
- 66.Melero MJ, Heredia R, Lell A, Volpacchio M. [Bouveret syndrome (gastric or duodenal obstruction due to biliary lithiasis)] Medicina (B Aires) 2010;70:88. [PubMed] [Google Scholar]
- 67.Matur R, Yucel T, Gurdal SO, Akpinar A. [Bouveret’S syndrome: gastric outlet obstruction by a gallstone] Ulus Travma Derg. 2002;8:179–182. [PubMed] [Google Scholar]
- 68.Matincheva R, Deredzhian S, Ivanov S. [Case of a biliodigestive fistula--a variant of Bouveret’s syndrome] Vutr Boles. 1984;23:60–64. [PubMed] [Google Scholar]
- 69.Masson JW, Fraser A, Wolf B, Duncan K, Brunt PW, Sinclair TS. Bouveret’s syndrome: gallstone ileus causing gastric outlet obstruction. Gastrointest Endosc. 1998;47:104–105. doi: 10.1016/s0016-5107(98)70308-6. [DOI] [PubMed] [Google Scholar]
- 70.Masannat YA, Caplin S, Brown T. A rare complication of a common disease: Bouveret syndrome, a case report. World J Gastroenterol. 2006;12:2620–2621. doi: 10.3748/wjg.v12.i16.2620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Martin-Cuesta L, Marco de Lucas E, Pellon R, Sanchez E, Piedra T, Arnaiz J, Parra JA, Lopez-Calderon M. Migrating intrathoracic gallstone: imaging findings. J Thorac Imaging. 2008;23:272–274. doi: 10.1097/RTI.0b013e3181833ee6. [DOI] [PubMed] [Google Scholar]
- 72.Marsdin EL, Kreckler S, Alzein A, D’Costa H. Choledochal-duodenal fistula presenting as an upper GI bleed. BMJ Case Rep 2011; 2011 doi: 10.1136/bcr.05.2011.4275. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Marschall J, Hayton S. Bouveret’s syndrome. Am J Surg. 2004;187:547–548. doi: 10.1016/j.amjsurg.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 74.Malvaux P, Degolla R, De Saint-Hubert M, Farchakh E, Hauters P. Laparoscopic treatment of a gastric outlet obstruction caused by a gallstone (Bouveret’s syndrome) Surg Endosc. 2002;16:1108–1109. doi: 10.1007/s004640042033. [DOI] [PubMed] [Google Scholar]
- 75.Makker J, Muthusamy VR, Watson R, Sedarat A. Electrohydraulic lithotripsy and removal of a gallstone obstructing the duodenum: Bouveret syndrome. Gastrointest Endosc. 2015;81:1021–1022. doi: 10.1016/j.gie.2014.10.045. [DOI] [PubMed] [Google Scholar]
- 76.Maiss J, Hochberger J, Hahn EG, Lederer R, Schneider HT, Muehldorfer S. Successful laserlithotripsy in Bouveret’s syndrome using a new frequency doubled doublepulse Nd: YAG laser (FREDDY) Scand J Gastroenterol. 2004;39:791–794. doi: 10.1080/00365520410005937. [DOI] [PubMed] [Google Scholar]
- 77.López-Martínez JA, Delgado-Carlo MM, Palacio-Vélez F, Arenas-Espino G, Granja-Posada E, Senado-Lara I, García-Alvarado L. [Bouveret’s syndrome. Case report] Cir Cir. 2004;72:317–322. [PubMed] [Google Scholar]
- 78.López Rosés L, Toscano J, Iñiguez F, Santos E, Pérez Carnero A. [Successful endoscopic therapy in a case of Bouveret’s syndrome] Rev Esp Enferm Dig. 1994;85:483–485. [PubMed] [Google Scholar]
- 79.Liao Z, Li ZS, Ye P. Bouveret’s syndrome. Gastrointest Endosc. 2007;65:703–704. doi: 10.1016/j.gie.2006.06.054. [DOI] [PubMed] [Google Scholar]
- 80.Leopaldi E, Ambrosiani N, Campanelli G. [Pyloric stenosis caused by gallstone (Bouveret’s syndrome). Presentation of a further case] Minerva Chir. 1991;46:405–409. [PubMed] [Google Scholar]
- 81.Lenz P, Domschke W, Domagk D. Bouveret’s syndrome: unusual case with unusual therapeutic approach. Clin Gastroenterol Hepatol. 2009;7:e72. doi: 10.1016/j.cgh.2009.04.021. [DOI] [PubMed] [Google Scholar]
- 82.Lawther RE, Diamond T. Bouveret’s syndrome: gallstone ileus causing gastric outlet obstruction. Ulster Med J. 2000;69:69–70. [PMC free article] [PubMed] [Google Scholar]
- 83.Langhorst J, Schumacher B, Deselaers T, Neuhaus H. Successful endoscopic therapy of a gastric outlet obstruction due to a gallstone with intracorporeal laser lithotripsy: a case of Bouveret’s syndrome. Gastrointest Endosc. 2000;51:209–213. doi: 10.1016/s0016-5107(00)70421-4. [DOI] [PubMed] [Google Scholar]
- 84.Kumar A, Chaturvedi S, Agrawal S, Gautam A. Gallstone obstruction of the duodenum (Bouveret’s syndrome) Indian J Gastroenterol. 1995;14:77–78. [PubMed] [Google Scholar]
- 85.Kishi K, Yamada K, Sugiyama T. Gastric outlet obstruction caused by a large gallstone in the duodenum (Bouveret’s syndrome) Clin Gastroenterol Hepatol. 2008;6:e11. doi: 10.1016/j.cgh.2007.12.027. [DOI] [PubMed] [Google Scholar]
- 86.Khan AZ, Escofet X, Miles WF, Singh KK. The Bouveret syndrome: an unusual complication of gallstone disease. J R Soc Promot Health. 2002;122:125–126. doi: 10.1177/146642400212200216. [DOI] [PubMed] [Google Scholar]
- 87.Khalsa B, Rudersdorf P, Dave D, Smith BR, Lall C. 63-year-old male with gastric outlet obstruction. Case Rep Radiol. 2014;2014:767165. doi: 10.1155/2014/767165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Keller M, Epp C, Meyenberger C, Sulz MC. Unspecific abdominal symptoms and pneumobilia: a rare case of gastrointestinal obstruction. Case Rep Gastroenterol. 2014;8:216–220. doi: 10.1159/000364818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Katsinelos P, Dimiropoulos S, Tsolkas P, Baltagiannis S, Kapelidis P, Galanis I, Papaziogas B, Georgiadou E, Vasiliadis I. Successful treatment of duodenal bulb obstruction caused by a gallstone (Bouveret’s syndrome) after endoscopic mechanical lithotripsy. Surg Endosc. 2002;16:1363. doi: 10.1007/s00464-002-4200-y. [DOI] [PubMed] [Google Scholar]
- 90.Kasano Y, Tanimura H, Yamaue H, Uchiyama K, Hayashido M, Hama T. Duodenal obstruction by gallstone: case report of Bouveret’s syndrome. Nihon Geka Hokan. 1997;66:111–115. [PubMed] [Google Scholar]
- 91.Kalwaniya DS, Arya SV, Guha S, Kuppuswamy M, Chaggar JG, Ralte L, Chejera R, Sharma A. A rare presentation of gastric outlet obstruction (GOO) - The Bouveret’s syndrome. Ann Med Surg (Lond) 2015;4:67–71. doi: 10.1016/j.amsu.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Joshi D, Vosough A, Raymond TM, Fox C, Dhiman A. Bouveret’s syndrome as an unusual cause of gastric outlet obstruction: a case report. J Med Case Rep. 2007;1:73. doi: 10.1186/1752-1947-1-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jones TA, Davis ME, Glantz AI. Bouveret’s syndrome presenting as upper gastrointestinal hemorrhage without hematemesis. Am Surg. 2001;67:786–789. [PubMed] [Google Scholar]
- 94.Jayakumar L, Vernick J, Waheed U. Bouveret’s syndrome: a rock in a hard place. Am Surg. 2012;78:E404–E406. [PubMed] [Google Scholar]
- 95.Jafferbhoy S, Rustum Q, Shiwani M. Bouveret’s syndrome: should we remove the gall bladder? BMJ Case Rep 2011; 2011 doi: 10.1136/bcr.02.2011.3891. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ivekovic H, Deban O, Rustemovic N, Ostojic R, Skegro M. Freehand endoscopic lithotripsy for Bouveret’s syndrome. Acta Gastroenterol Belg. 2012;75:375–376. [PubMed] [Google Scholar]
- 97.Ivashchenko VV, Skvortsov KK, Zhuravleva IuI, Skvortsov KK, Koĭko MA. [Successful treatment of Bouveret syndrome in elderly woman patient] Klin Khir. 2000;(6):60. [PubMed] [Google Scholar]
- 98.Iuchtman M, Sternberg A, Alfici R, Sternberg E, Fireman T. [Iatrogenic gallstone ileus as a new complication of Bouveret’s syndrome] Harefuah. 1999;136:122–124, 174. [PubMed] [Google Scholar]
- 99.Iñíguez A, Butte JM, Zúñiga JM, Crovari F, Llanos O. [Bouveret syndrome: report of four cases] Rev Med Chil. 2008;136:163–168. [PubMed] [Google Scholar]
- 100.Iancu C, Bodea R, Al Hajjar N, Todea-Iancu D, Bălă O, Acalovschi I. Bouveret syndrome associated with acute gangrenous cholecystitis. J Gastrointestin Liver Dis. 2008;17:87–90. [PubMed] [Google Scholar]
- 101.Hütter G. [Bouveret syndrome. What is obstructing the duodenum?] MMW Fortschr Med. 2015;157:5. doi: 10.1007/s15006-015-2615-3. [DOI] [PubMed] [Google Scholar]
- 102.Hussain A, Obaid S, El-Hasani S. Bouveret’s syndrome: endoscopic or surgical treatment. Updates Surg. 2013;65:63–65. doi: 10.1007/s13304-011-0131-2. [DOI] [PubMed] [Google Scholar]
- 103.Hürlimann R, Enzler M, Binswanger RO, Meyenberger C. [Bouveret syndrome--a rare gallstone complication] Z Gastroenterol. 1995;33:445–448. [PubMed] [Google Scholar]
- 104.Huebner ES, DuBois S, Lee SD, Saunders MD. Successful endoscopic treatment of Bouveret‘s syndrome with intracorporeal electrohydraulic lithotripsy. Gastrointest Endosc. 2007;66:183–184; discussion 184. doi: 10.1016/j.gie.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 105.Heyd RL, Solinger MR, Howard AL, Rosser JC. Acute upper gastrointestinal hemorrhage caused by gallstone impaction in the duodenal bulb. Dig Dis Sci. 1992;37:452–455. doi: 10.1007/BF01307742. [DOI] [PubMed] [Google Scholar]
- 106.Hernández Garcés HR, Andrain Sierra Y, del Rio-Mendoza JR, Gutierrez Revatta E, Moutary I. [Bouveret Syndrome. First case diagnosed in Santa Maria del Socorro, Ica, Peru] Rev Gastroenterol Peru. 2014;34:69–72. [PubMed] [Google Scholar]
- 107.Heneghan HM, Martin ST, Ryan RS, Waldron R. Bouveret’s syndrome--a rare presentation of gallstone ileus. Ir Med J. 2007;100:504–505. [PubMed] [Google Scholar]
- 108.Heinrich D, Meier J, Wehrli H, Bühler H. Upper gastrointestinal hemorrhage preceding development of Bouveret’s syndrome. Am J Gastroenterol. 1993;88:777–780. [PubMed] [Google Scholar]
- 109.Harthun NL, Long SM, Wilson W, Choudhury A. An unusual case of Bouveret’s syndrome. J Laparoendosc Adv Surg Tech A. 2002;12:69–72. doi: 10.1089/109264202753486975. [DOI] [PubMed] [Google Scholar]
- 110.Hameed K, Ahmad A, Baghomian A. Bouveret’s syndrome, an unusual cause of upper gastrointestinal bleeding. QJM. 2010;103:697–698. doi: 10.1093/qjmed/hcq015. [DOI] [PubMed] [Google Scholar]
- 111.Goldstein EB, Savel RH, Pachter HL, Cohen J, Shamamian P. Successful treatment of Bouveret syndrome using holmium: YAG laser lithotripsy. Am Surg. 2005;71:882–885. [PubMed] [Google Scholar]
- 112.Giese A, Zieren J, Winnekendonk G, Henning BF. Development of a duodenal gallstone ileus with gastric outlet obstruction (Bouveret syndrome) four months after successful treatment of symptomatic gallstone disease with cholecystitis and cholangitis: a case report. J Med Case Rep. 2010;4:376. doi: 10.1186/1752-1947-4-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.George J, Aufhauser DD, Raper SE. Bouveret‘s Syndrome Resulting in Gallstone Ileus. J Gastrointest Surg. 2015;19:1189–1191. doi: 10.1007/s11605-015-2778-3. [DOI] [PubMed] [Google Scholar]
- 114.Gencosmanoglu R, Inceoglu R, Baysal C, Akansel S, Tozun N. Bouveret’s syndrome complicated by a distal gallstone ileus. World J Gastroenterol. 2003;9:2873–2875. doi: 10.3748/wjg.v9.i12.2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Gemmel C, Weickert U, Eickhoff A, Schilling D, Riemann JF. Successful treatment of gallstone ileus (Bouveret’s syndrome) by using extracorporal shock wave lithotripsy and argon plasma coagulation. Gastrointest Endosc. 2007;65:173–175. doi: 10.1016/j.gie.2006.05.025. [DOI] [PubMed] [Google Scholar]
- 116.Gan S, Roy-Choudhury S, Agrawal S, Kumar H, Pallan A, Super P, Richardson M. More than meets the eye: subtle but important CT findings in Bouveret’s syndrome. AJR Am J Roentgenol. 2008;191:182–185. doi: 10.2214/AJR.07.3418. [DOI] [PubMed] [Google Scholar]
- 117.Gajendran M, Muniraj T, Gelrud A. A challenging case of gastric outlet obstruction (Bouveret’s syndrome): a case report. J Med Case Rep. 2011;5:497. doi: 10.1186/1752-1947-5-497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gaduputi V, Tariq H, Rahnemai-Azar AA, Dev A, Farkas DT. Gallstone ileus with multiple stones: Where Rigler triad meets Bouveret’s syndrome. World J Gastrointest Surg. 2015;7:394–397. doi: 10.4240/wjgs.v7.i12.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Foets TC, Weusten BL, van Es HW, Boerma D. [An 84 year old man with gastric outlet obstruction] Ned Tijdschr Geneeskd. 2014;158:A7550. [PubMed] [Google Scholar]
- 120.Finn H, Bienia M. [Determination of gallstone ileus using emergency gastroscopy] Z Gesamte Inn Med. 1981;36:85–87. [PubMed] [Google Scholar]
- 121.Ferreira LE, Topazian MD, Baron TH. Bouveret’s syndrome: diagnosis and endoscopic treatment. Clin Gastroenterol Hepatol. 2008;6:e15. doi: 10.1016/j.cgh.2007.12.055. [DOI] [PubMed] [Google Scholar]
- 122.Fenchel RF, Krige JE, Bornman PC. Bouveret’s syndrome complicated by acute pancreatitis. Dig Surg. 1999;16:525–527. doi: 10.1159/000018782. [DOI] [PubMed] [Google Scholar]
- 123.Fejes R, Kurucsai G, Székely A, Luka F, Altorjay A, Madácsy L. Gallstone Ileus, Bouveret’s Syndrome and Choledocholithiasis in a Patient with Billroth II Gastrectomy - A Case Report of Combined Endoscopic and Surgical Therapy. Case Rep Gastroenterol. 2010;4:71–78. doi: 10.1159/000208993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fedidat R, Safadi W, Waksman I, Hadary A. Choledochoduodenal fistula: an unusual case of pneumobilia. BMJ Case Rep 2014; 2014 doi: 10.1136/bcr-2014-206798. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Farman J, Goldstein DJ, Sugalski MT, Moazami N, Amory S. Bouveret’s syndrome: diagnosis by helical CT scan. Clin Imaging. 1998;22:240–242. doi: 10.1016/s0899-7071(98)00012-6. [DOI] [PubMed] [Google Scholar]
- 126.Fancellu A, Niolu P, Scanu AM, Feo CF, Ginesu GC, Barmina ML. A rare variant of gallstone ileus: Bouveret’s syndrome. J Gastrointest Surg. 2010;14:753–755. doi: 10.1007/s11605-009-0918-3. [DOI] [PubMed] [Google Scholar]
- 127.Ezberci F, Kargi H, Ergin A. Gastric outlet obstruction by a gallstone (Bouveret’s syndrome) Surg Endosc. 2000;14:372. doi: 10.1007/s004640010050. [DOI] [PubMed] [Google Scholar]
- 128.Erlandson MD, Kim AW, Richter HM, Myers JA. Roux-en-Y duodenojejunostomy in the treatment of Bouveret syndrome. South Med J. 2009;102:963–965. doi: 10.1097/SMJ.0b013e3181b17dde. [DOI] [PubMed] [Google Scholar]
- 129.Englert ZP, Love K, Marilley MD, Bower CE. Bouveret syndrome: gallstone ileus of the duodenum. Surg Laparosc Endosc Percutan Tech. 2012;22:e301–e303. doi: 10.1097/SLE.0b013e318262ec13. [DOI] [PubMed] [Google Scholar]
- 130.Dumonceau JM, Delhaye M, Devière J, Baize M, Cremer M. Endoscopic treatment of gastric outlet obstruction caused by a gallstone (Bouveret’s syndrome) after extracorporeal shock-wave lithotripsy. Endoscopy. 1997;29:319–321. doi: 10.1055/s-2007-1004197. [DOI] [PubMed] [Google Scholar]
- 131.Dugalić D, Colović R, Savić M. [Duodenal obstruction caused by gallstones (Bouveret syndrome)] Acta Chir Iugosl. 1990;37:75–82. [PubMed] [Google Scholar]
- 132.Doycheva I, Limaye A, Suman A, Forsmark CE, Sultan S. Bouveret’s syndrome: case report and review of the literature. Gastroenterol Res Pract. 2009;2009:914951. doi: 10.1155/2009/914951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Dimov R, Deenichin G, Uchikov A, Molov V, Ivanov V, Stefanov Ch. [Bouveret’ syndrome or secondary duodenal obstruction caused by gallstones. Case report] Khirurgiia (Sofiia) 2005;(4-5):53–55. [PubMed] [Google Scholar]
- 134.Dillon CK, Ali A, Perry A. Laparoscopic management of gastric outlet obstruction. ANZ J Surg. 2009;79:663–664. doi: 10.1111/j.1445-2197.2009.05034.x. [DOI] [PubMed] [Google Scholar]
- 135.Csermely L, Tárnok F, Varga G, Tüske G. [Bouveret syndrome diagnosed by endoscopy] Orv Hetil. 1990;131:2715–2717. [PubMed] [Google Scholar]
- 136.Crespo Pérez L, Angueira Lapeña T, Defarges Pons V, Foruny Olcina JR, Cano Ruiz A, Benita León V, Gónzalez Martín JA, Boixeda de Miquel D, Milicua Salamero JM. [A rare cause of gastric outlet obstruction: Bouveret’s syndrome] Gastroenterol Hepatol. 2008;31:646–651. doi: 10.1016/S0210-5705(08)75813-8. [DOI] [PubMed] [Google Scholar]
- 137.Crans CA, Cloney DJ. Bouveret’s syndrome: an unusual twist on the classic cause. South Med J. 1991;84:1049–1051. [PubMed] [Google Scholar]
- 138.Costil V, Jullès MC, Zins M, Loriau J. Bouveret’s syndrome. An unusual localization of gallstone ileus. J Visc Surg. 2012;149:e284–e286. doi: 10.1016/j.jviscsurg.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 139.Cipolletta L, Bianco MA, Cipolletta F, Meucci C, Prisco A, Rotondano G. Successful endoscopic treatment of Bouveret’s syndrome by mechanical lithotripsy. Dig Liver Dis. 2009;41:e29–e31. doi: 10.1016/j.dld.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 140.Chilovi F, Farris P, Heinrich P. Bouveret’s syndrome. Gastrointest Endosc. 2002;56:112. doi: 10.1067/mge.2002.123424. [DOI] [PubMed] [Google Scholar]
- 141.Charalambous CP, Midwinter M, Bancewicz J. Unusual presentation of Bouveret’s syndrome. J Gastroenterol. 2002;37:476–478. doi: 10.1007/s005350200070. [DOI] [PubMed] [Google Scholar]
- 142.Carvalheiro J, Mendes S, Sofia C. Bouveret’s syndrome: a rare cause of abdominal pain in the elderly. Asian J Endosc Surg. 2014;7:93. doi: 10.1111/ases.12073. [DOI] [PubMed] [Google Scholar]
- 143.Bruni R, Bartolucci R, Biancari F, Cataldi C. [Bouveret’s syndrome] G Chir. 1993;14:439–441. [PubMed] [Google Scholar]
- 144.Brice R, Chivot C, Deguisne JB, Sabbagh C. [Hematemesis of unusual cause] Rev Med Interne. 2015;36:365–366. doi: 10.1016/j.revmed.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 145.Brennan GB, Rosenberg RD, Arora S. Bouveret syndrome. Radiographics. 2004;24:1171–1175. doi: 10.1148/rg.244035222. [DOI] [PubMed] [Google Scholar]
- 146.Bonam R, Vahora Z, Harvin G, Leland W. Bouveret’s Syndrome with Severe Esophagitis and a Purulent Fistula. ACG Case Rep J. 2014;1:158–160. doi: 10.14309/crj.2014.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bhama JK, Ogren JW, Lee T, Fisher WE. Bouveret’s syndrome. Surgery. 2002;132:104–105. doi: 10.1067/msy.2002.117196. [DOI] [PubMed] [Google Scholar]
- 148.Bernardin E, Boati S, Bona D, Abraham M, Saino G, Bonavina L. [Bouveret’s syndrome: a rare clinical variant of gallstone ileus] Chir Ital. 2005;57:267–270. [PubMed] [Google Scholar]
- 149.Baudet-Bourgarel A, Boruchowicz A, Gambiez L, Paris JC. [Bouveret syndrome revealed by hematemesis] Gastroenterol Clin Biol. 1996;20:112–113. [PubMed] [Google Scholar]
- 150.Barranco B, Eloubeidi MA, Canakis J, Johnson LF, Shore G, Wilcox CM. Bouveret’s syndrome. Gastrointest Endosc. 2002;56:736. doi: 10.1067/mge.2002.128697. [DOI] [PubMed] [Google Scholar]
- 151.Baharith H, Khan K. Bouveret syndrome: when there are no options. Can J Gastroenterol Hepatol. 2015;29:17–18. doi: 10.1155/2015/215643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Báez-García JJ, Martínez-Hernández-Magro P, Iriarte-Gállego G. [Bouveret’s syndrome; a case report] Rev Gastroenterol Mex. 2009;74:118–121. [PubMed] [Google Scholar]
- 153.Avén H, Gözen M. [Bouveret syndrome--when gallstone causes duodenal obstruction. Unusual and very difficult diagnosis to make] Lakartidningen. 2014;111:1843–1845. [PubMed] [Google Scholar]
- 154.Arioli D, Venturini I, Masetti M, Romagnoli E, Scarcelli A, Ballesini P, Borghi A, Barberini A, Spina V, De Santis M, et al. Intermittent gastric outlet obstruction due to a gallstone migrated through a cholecysto-gastric fistula: a new variant of “Bouveret’s syndrome”. World J Gastroenterol. 2008;14:125–128. doi: 10.3748/wjg.14.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ariche A, Czeiger D, Gortzak Y, Shaked G, Shelef I, Levy I. Gastric outlet obstruction by gallstone: Bouveret syndrome. Scand J Gastroenterol. 2000;35:781–783. doi: 10.1080/003655200750023480. [DOI] [PubMed] [Google Scholar]
- 156.Apel D, Jakobs R, Benz C, Martin WR, Riemann JF. Electrohydraulic lithotripsy treatment of gallstone after disimpaction of the stone from the duodenal bulb (Bouveret‘s syndrome) Ital J Gastroenterol Hepatol. 1999;31:876–879. [PubMed] [Google Scholar]
- 157.Andersson EJ, Kullman EP, Halldestam IR, Einarsson C, Borch K. Bouveret’s syndrome followed by gallstone entrapment in the stomach: an uncommon cause of upper gastrointestinal bleeding and gastric retention. Eur J Surg. 2000;166:183–185. doi: 10.1080/110241500750009582. [DOI] [PubMed] [Google Scholar]
- 158.Alsolaiman MM, Reitz C, Nawras AT, Rodgers JB, Maliakkal BJ. Bouveret’s syndrome complicated by distal gallstone ileus after laser lithotropsy using Holmium: YAG laser. BMC Gastroenterol. 2002;2:15. doi: 10.1186/1471-230X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Algın O, Ozmen E, Metin MR, Ersoy PE, Karaoğlanoğlu M. Bouveret syndrome: evaluation with multidetector computed tomography and contrast-enhanced magnetic resonance cholangiopancreatography. Ulus Travma Acil Cerrahi Derg. 2013;19:375–379. doi: 10.5505/tjtes.2013.97254. [DOI] [PubMed] [Google Scholar]
- 160.Ah-Chong K, Leong YP. Gastric outlet obstruction due to gall stones (Bouveret syndrome) Postgrad Med J. 1987;63:909–910. doi: 10.1136/pgmj.63.744.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Afzal M, Ghosh D, Leigh T. Mechanical lithotripsy for Bouveret’s syndrome. Gut. 2007;56:733–734; author reply 734. doi: 10.1136/gut.2006.111591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Geron N, Hazzan D, Shiloni E. Bouveret’s syndrome as a rare complication of cholecystolithiasis: report of a case. Surg Today. 2003;33:66–68. doi: 10.1007/s005950300013. [DOI] [PubMed] [Google Scholar]
- 163.Mengual-Ballester M, Guillén-Paredes MP, Cases-Baldó MJ, García-García ML, Aguayo-Albasini JL. Gastrointestinal bleeding and bowel obstruction as a presentation of Bouveret syndrome. Cir Cir. 2011;79:557–559. [PubMed] [Google Scholar]
- 164.Brezean I, Aldoescu S, Catrina E, Fetche N, Marin I, Păcescu E. Gallstone ileus: analysis of eight cases and review of the literature. Chirurgia (Bucur) 2010;105:355–359. [PubMed] [Google Scholar]
- 165.Cappell MS, Davis M. Characterization of Bouveret’s syndrome: a comprehensive review of 128 cases. Am J Gastroenterol. 2006;101:2139–2146. doi: 10.1111/j.1572-0241.2006.00645.x. [DOI] [PubMed] [Google Scholar]
- 166.Frattaroli FM, Reggio D, Guadalaxara A, Illomei G, Lomanto D, Pappalardo G. Bouveret’s syndrome: case report and review of the literature. Hepatogastroenterology. 1997;44:1019–1022. [PubMed] [Google Scholar]
- 167.Kaushik N, Moser AJ, Slivka A, Chandrupatala S, Martin JA. Gastric outlet obstruction caused by gallstones: case report and review of the literature. Dig Dis Sci. 2005;50:470–473. doi: 10.1007/s10620-005-2460-9. [DOI] [PubMed] [Google Scholar]
- 168.Koulaouzidis A, Moschos J. Bouveret’s syndrome. Narrative review. Ann Hepatol. 2007;6:89–91. [PubMed] [Google Scholar]
- 169.Lee W, Han SS, Lee SD, Kim YK, Kim SH, Woo SM, Lee WJ, Koh YW, Hong EK, Park SJ. Bouveret’s syndrome: a case report and a review of the literature. Korean J Hepatobiliary Pancreat Surg. 2012;16:84–87. doi: 10.14701/kjhbps.2012.16.2.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Lowe AS, Stephenson S, Kay CL, May J. Duodenal obstruction by gallstones (Bouveret’s syndrome): a review of the literature. Endoscopy. 2005;37:82–87. doi: 10.1055/s-2004-826100. [DOI] [PubMed] [Google Scholar]
- 171.Mavroeidis VK, Matthioudakis DI, Economou NK, Karanikas ID. Bouveret syndrome-the rarest variant of gallstone ileus: a case report and literature review. Case Rep Surg. 2013;2013:839370. doi: 10.1155/2013/839370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Moschos J, Pilpilidis I, Antonopoulos Z, Paikos D, Tzilves D, Kadis S, Katsos I, Tarpagos A. Complicated endoscopic management of Bouveret’s syndrome. A case report and review. Rom J Gastroenterol. 2005;14:75–77. [PubMed] [Google Scholar]
- 173.Nickel F, Müller-Eschner MM, Chu J, von Tengg-Kobligk H, Müller-Stich BP. Bouveret’s syndrome: presentation of two cases with review of the literature and development of a surgical treatment strategy. BMC Surg. 2013;13:33. doi: 10.1186/1471-2482-13-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Penkov N. [Bouveret syndrome (review of literature and case report)] Khirurgiia (Sofiia) 2003;59:31–33. [PubMed] [Google Scholar]
- 175.Qasaimeh GR, Bakkar S, Jadallah K. Bouveret’s Syndrome: An Overlooked Diagnosis. A Case Report and Review of Literature. Int Surg. 2014;99:819–823. doi: 10.9738/INTSURG-D-14-00087.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Rodriguez Romano D, Moreno Gonzalez E, Jiménez Romero C, Selas PR, Manzanera Díaz M, Abradelo de Usera M, Hernández Ga Gallardo D. Duodenal obstruction by gallstones (Bouveret’s syndrome). Presentation of a new case and literature review. Hepatogastroenterology. 1997;44:1351–1355. [PubMed] [Google Scholar]
- 177.Antonini F, Belfiori V, Macarri G. Bouveret’s syndrome: a rare complication of gallstone disease. Liver Int. 2013;33:1132. doi: 10.1111/liv.12123. [DOI] [PubMed] [Google Scholar]
- 178.Aras M, Inanir S, Tuney D. Bouveret’s syndrome on FDG PET/CT: a rare life-threatening complication of gallstone disease. Rev Esp Med Nucl Imagen Mol. 2014;33:125–126. doi: 10.1016/j.remn.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 179.Baloyiannis I, Symeonidis D, Koukoulis G, Zachari E, Potamianos S, Tzovaras G. Complicated cholelithiasis: an unusual combination of acute pancreatitis and bouveret syndrome. Case Rep Gastroenterol. 2012;6:459–464. doi: 10.1159/000341512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Calvo Espino P, García Pavía A, Artés Caselles M, Sánchez Turrión V. [Bouveret syndrome: variant of gallstone ileus] Cir Esp. 2014;92:e3. doi: 10.1016/j.ciresp.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 181.Chick JF, Chauhan NR, Mandell JC, de Souza DA, Bair RJ, Khurana B. Traffic jam in the duodenum: imaging and pathogenesis of Bouveret syndrome. J Emerg Med. 2013;45:e135–e137. doi: 10.1016/j.jemermed.2013.04.058. [DOI] [PubMed] [Google Scholar]
- 182.Djuric-Stefanovic A, Pesko P, Saranovic D. Education and imaging. Hepatobiliary and pancreatic: Bouveret’s syndrome. J Gastroenterol Hepatol. 2011;26:1216. doi: 10.1111/j.1440-1746.2011.06792.x. [DOI] [PubMed] [Google Scholar]
- 183.Gijón-de-la-Santa L, Camarero-Miguel A, Pérez-Retortillo JA, Ramia-Ángel JM. Bouveret’s syndrome: evaluation with multidetector CT. Rev Esp Enferm Dig. 2014;106:283–284. [PubMed] [Google Scholar]
- 184.Guntau J, Oelckers M, Rathgeber T, Lock G. [Sonographic diagnosis of Bouveret’s syndrome] Dtsch Med Wochenschr. 2007;132:315–318. doi: 10.1055/s-2007-959326. [DOI] [PubMed] [Google Scholar]
- 185.Gupta M, Garg D. Bouveret’s syndrome. Indian J Gastroenterol. 2013;32:351. doi: 10.1007/s12664-012-0190-4. [DOI] [PubMed] [Google Scholar]
- 186.Herbener TE, Basile V, Nakamoto D, Butler HE, Pickering SP. Abdominal case of the day. Bouveret’s syndrome. AJR Am J Roentgenol. 1997;169:250, 252–253. doi: 10.2214/ajr.169.1.9207534. [DOI] [PubMed] [Google Scholar]
- 187.Joshi RM, Shetty TS, Singh R, Raja S, Satish R, Prabhu SV. Bouveret’s syndrome. Indian J Gastroenterol. 2009;28:79. doi: 10.1007/s12664-009-0028-x. [DOI] [PubMed] [Google Scholar]
- 188.Marco Doménech SF, López Mut JV, Fernández Garcia P, San Miguel Moncín MM, Gil Sánchez S, Jornet Fayos J, Tudela Ortells X. [Bouveret’s syndrome: the clinical and radiological findings] Rev Esp Enferm Dig. 1999;91:144–148. [PubMed] [Google Scholar]
- 189.McKee JD, Tendler D, Chittani R. Image of the month. Bouveret’s syndrome. Gastroenterology. 1997;112:682, 1059. [PubMed] [Google Scholar]
- 190.Mullady DK, Ahmad J. Clinical challenges and images in GI. Gallstone impacted in duodenum causing gastric outlet obstruction (Bouveret syndrome) Gastroenterology. 2007;133:1075, 1394. doi: 10.1053/j.gastro.2007.08.056. [DOI] [PubMed] [Google Scholar]
- 191.Negi RS, Chandra M, Kapur R. Bouveret syndrome: Primary demonstration of cholecystoduodenal fistula on MR and MRCP study. Indian J Radiol Imaging. 2015;25:31–34. doi: 10.4103/0971-3026.150136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Ng SS, Lai PB, Lee JF, Lau WY. Soft-tissue case 41. Bouveret’s syndrome. Can J Surg. 2001;44:336, 364–365. [PMC free article] [PubMed] [Google Scholar]
- 193.Prachayakul V, Aswakul P, Kachintorn U. Atypical clinical presentation of typical endoscopic finding of Bouveret’s syndrome. Endoscopy. 2011;43 Suppl 2 UCTN:E55–E56. doi: 10.1055/s-0030-1256059. [DOI] [PubMed] [Google Scholar]
- 194.Ramos Soria F, Morales Coca C, Bustamante Maldonado E, Vida Mombiela F. [Bouveret syndrome] Med Clin (Barc) 2008;131:480. doi: 10.1157/13126961. [DOI] [PubMed] [Google Scholar]
- 195.Rodgers AD. Hepatobiliary and pancreatic: Bouveret’s syndrome. J Gastroent Hepat. 2003;18:1210–1210. doi: 10.1046/j.1440-1746.2003.t01-1-03196.x. [DOI] [PubMed] [Google Scholar]
- 196.Sharma D, Sood R, Tomar A, Jhobta A, Thakur S, Sood RG. Bouveret’s Syndrome: 64-Slice CT Diagnosis and Surgical Management-A Case Report. Case Rep Radiol. 2012;2012:701216. doi: 10.1155/2012/701216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Tüney D, Cimşit C. Bouveret’s syndrome: CT findings. Eur Radiol. 2000;10:1711–1712. doi: 10.1007/s003300000444. [DOI] [PubMed] [Google Scholar]
- 198.Zippi M, Di Stefano P, Manetti G, Febbraro I, Traversa G, Mazzone AM, De Felici I, Mattei E, Occhigrossi G. Bouveret’s syndrome: description of a case. Clin Ter. 2009;160:367–369. [PubMed] [Google Scholar]
- 199.Park SH, Lee SW, Song TJ. Another new variant of Bouveret’s syndrome. World J Gastroenterol. 2009;15:378–379. doi: 10.3748/wjg.15.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Qandeel H, Tayyem R, Mahmud S. Bouveret’s syndrome with cholecysto-colic fistula. S Afr J Surg. 2010;48:134. [PubMed] [Google Scholar]
- 201.Mumoli N, Cei M, Luschi R, Carmignani G, Orlandi F. Bouveret syndrome. Emerg Med J. 2010;27:525. doi: 10.1136/emj.2008.068676. [DOI] [PubMed] [Google Scholar]
- 202.Gundling F, Helmberger T, Schepp W. Duodenal perforation due to a gallstone in small intestinal gallstone ileus: “Bouveret’s syndrome”. Turk J Gastroenterol. 2009;20:232–233. doi: 10.4318/tjg.2009.0015. [DOI] [PubMed] [Google Scholar]
- 203.Menéndez P, Gambi D, Villarejo P, Cubo T, Padilla D, Martín J. [Biliary ileus as a consequence of a cholecystoduodenal fistula (Bouveret syndrome)] Rev Clin Esp. 2008;208:321–322. doi: 10.1157/13123202. [DOI] [PubMed] [Google Scholar]
- 204.Doody O, Ward E, Buckley O, Hogan B, Torreggiani WC. Bouveret’s syndrome variant. Digestion. 2007;75:126–127. doi: 10.1159/000104975. [DOI] [PubMed] [Google Scholar]
- 205.Buchs NC, Azagury D, Chilcott M, Nguyen-Tang T, Dumonceau JM, Morel P. Bouveret’s syndrome: management and strategy of a rare cause of gastric outlet obstruction. Digestion. 2007;75:17–19. doi: 10.1159/000101561. [DOI] [PubMed] [Google Scholar]
- 206.Rivera Irigoín R, Ubiña Aznar E, García Fernández G, Navarro Jarabo JM, Fernández Pérez F, Sánchez Cantos A. [Successful treatment of Bouveret’s syndrome with endoscopic mechanical lithotripsy] Rev Esp Enferm Dig. 2006;98:790–792. doi: 10.4321/s1130-01082006001000011. [DOI] [PubMed] [Google Scholar]
- 207.Losanoff JE, Richman BW, Jones JW. Endoscopic management of Bouveret‘s syndrome. Surgery. 2003;133:230; author reply 230–231. doi: 10.1067/msy.2003.66. [DOI] [PubMed] [Google Scholar]
- 208.Ondrejka P. Bouveret’s syndrome treated by a combination of extracorporeal shock-wave lithotripsy (ESWL) and surgical intervention. Endoscopy. 1999;31:834. [PubMed] [Google Scholar]
- 209.Kjossev KT, Losanoff JE. Endoscopic management of Bouveret’s syndrome. Can J Gastroenterol. 1998;12:168. [PubMed] [Google Scholar]
- 210.Patel A, Agarwal S. The yellow brick road of Bouveret syndrome. Clin Gastroenterol Hepatol. 2014;12:A24. doi: 10.1016/j.cgh.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 211.Liew V, Layani L, Speakman D. Bouveret’s syndrome in Melbourne. ANZ J Surg. 2002;72:161–163. doi: 10.1046/j.1445-2197.2002.02319.x. [DOI] [PubMed] [Google Scholar]
- 212.Zong KC, You HB, Gong JP, Tu B. Diagnosis and management of choledochoduodenal fistula. Am Surg. 2011;77:348–350. [PubMed] [Google Scholar]
- 213.Ha JP, Tang CN, Li MK. Pseudo-Bouveret’s syndrome. Asian J Surg. 2004;27:246–248. doi: 10.1016/S1015-9584(09)60044-0. [DOI] [PubMed] [Google Scholar]


