Abstract
Objectives
Acute infectious diseases are the most common cause of under-5 mortality. However, the hospital burden of non-neonatal pediatric sepsis has not previously been described in the resource poor setting. The objective of this study was to determine the prevalence of sepsis among children 6 months to 5 years of age admitted with proven or suspected infection and to evaluate the presence of sepsis as a predictive tool for mortality during admission.
Design
In this Prospective cohort study we used the pediatric International Consensus Conference definition of sepsis to determine the prevalence of sepsis among children admitted to the pediatric ward with a proven or suspected infection. The diagnosis of sepsis, as well as each individual component of the sepsis definition, were evaluated for capturing in-hospital mortality.
Setting
The pediatric ward of two hospitals in Mbarara, Uganda
Patients
Admitted children between 6 months and 5 years with a confirmed or suspected infection.
Interventions
None
Measurements and Main Results
One thousand three hundred and seven (1307) subjects with a confirmed or suspected infection were enrolled and 65 children died (5.0%) during their admission. One thousand one hundred and twenty-one (85.9%) met the systemic inflammatory response syndrome criteria, and therefore were defined as having sepsis. The sepsis criteria captured 61 deaths, demonstrating a sensitivity and specificity of 95% (95% CI 90% – 100%) and 15% (95% CI 13% – 17%), respectively. The most discriminatory individual component of the SIRS criteria was the leukocyte count which alone had a sensitivity of 72% and a specificity of 56% for the identification of mortality in hospital.
Conclusions
This study is among the first to quantify the burden of non-neonatal pediatric sepsis in children with suspected infection, using the international consensus sepsis definition, in a typical resource constrained setting in Africa. This definition was found to be highly sensitive in identifying those who died, but had very low specificity as most children who were admitted with infections had sepsis. The SIRS-based sepsis definition offers little value in identification of children at high risk of in-hospital mortality in this setting.
Key words (MeSH): Sepsis, Pediatrics, Uganda, Communicable Diseases, Global Health
Introduction
Pediatric sepsis is defined by the Pediatric International Consensus Conference as the presence of the systemic inflammatory response syndrome (SIRS) in association with a confirmed or suspected infection.1 The current sepsis definitions consist of a continuum of syndromes progressing from sepsis (above) to severe sepsis to septic shock based on the presence of organ dysfunction. These definitions were initially developed for use in clinical research but have been progressively introduced into clinical care. In adults, for instance, the systemic inflammatory response syndrome, has been incorporated into emergency department early warning scores for serious infectious illness.2 These definitions also form the basis for guideline development in both adults and pediatrics in developed countries.3 In the resource constrained context, however, sepsis as a syndrome is largely absent from the pediatric global health lexicon, with the notable exception of neonatal sepsis. This is surprising given the fact that most admitted children suffer from infections as compared to all other pathologies. Rather, infectious disease is considered vertically, with a disease specific focus rather than an infectious syndrome based approach.4 While this approach fits well with the incorporation of disease specific treatment algorithms, it neglects the fact that multiple diseases may exist concurrently, and that a general syndrome of severe infection may be helpful in defining risk and guiding treatment in these populations.
Although sepsis, with its definitions of increasing severity, may be helpful as early warning signs of risk among children admitted with infectious diseases, only well-resourced centers can actually provide such diagnoses since the resources required are often not available or too costly for routine use in low resource settings. This is a clear and recognized limitation of the current definitions of sepsis.5 Even the most basic SIRS-based definition of sepsis requires a white blood cell count which is often not available in lower level health facilities. Currently no studies have been conducted in resource constrained settings to determine the prevalence of sepsis at the time of hospital admission, nor its ability to identify children who die of an infectious illness. The purpose of this study was to determine the hospital burden of pediatric sepsis using its most basic definition (SIRS in association with suspected or proven infection), among children admitted with suspected infection, and to evaluate the presence of sepsis as a predictor of infectious disease-associated mortality during admission.
Materials and Methods
This study was conducted as a secondary analysis of a previously conducted study evaluating pediatric post-discharge mortality in Uganda. The methods have been previously described in detail.6 Briefly, this was a two-site, hospital-based cohort study in Mbarara, Uganda. All children between 6 months and 5 years of age who were admitted to either site with a suspected or proven infection were screened for eligibility. Enrollment occurred between March 2012 and January 2013. A research nurse obtained consent from a parent/guardian of all enrolled children and then collected admission variables including vital signs and blood for a laboratory testing, including HIV, malaria, and a complete blood count. Demographic variables including age, sex, known comorbidities, anthropometric variables (weight, length/height, mid-upper arm circumference), length of stay, discharge diagnosis and in-hospital vital status were also obtained. All children received routine care in accordance to the Ugandan national guidelines during their admission under the care of the hospital medical team.7 The medical team included pediatricians, medical residents, medical interns, nurses and nursing interns. This study was approved by the research ethics boards of the University of British Columbia (Vancouver, Canada) and the Mbarara University of Science and Technology (Mbarara, Uganda).
Outcomes and objectives
The primary outcome was the burden (prevalence) of sepsis (SIRS) among admitted subjects admitted with a proven or suspected infection, and to determine its performance (sensitivity, specificity and positive/negative predictive values) in predicting death during admission. Sepsis was defined following the Pediatric International Consensus Conference definition as the presence of the systemic inflammatory response syndrome (SIRS) in association with a confirmed or suspected infection (Table 1). Since temperature was measured via an axillary probe, it was assumed to be 0.5°C lower than a core temperature, based on Stine et al.8 Therefore, the threshold for meeting the hyperthermia cut-off was reduced from 38.5°C to 38.0°C. Secondary outcomes included the proportion of subjects meeting the cut-off points for each component of the sepsis definitions (heart rate, respiratory rate, leukocyte count, temperature) and the proportion of subjects meeting the sepsis definition by each defining criteria (temperature with leukocyte count, temperature with heart rate, temperature with respiratory rate, leukocyte count with respiratory rate and leukocyte with heart rate) and to determine the predictive performance characteristics of these individual criteria in predicting mortality.
Table 1.
| a. Definition of Sepsis |
|---|
| Systemic inflammatory response syndrome (SIRS) |
| Presence of at least 2 of the following, one of which must be abnormal temperature or leukocyte count |
| Core temperature > 38.5°C or < 36°C |
| Tachycardia or Bradycardia (see below) in the absence of external stimulus, drugs etc. |
| Tachypnea (see below) not related to underlying neuromuscular disease or anesthesia |
| Leukocyte count elevated or depressed (see below) |
| Infection |
| Suspected or proven infection caused by any pathogen OR a clinical syndrome associated with a high probability of infection |
| b. Age-specific cut-offs for heart rate, respiratory rate and leukocyte count | ||||
|---|---|---|---|---|
| Age group | Heart Rate, Beats/Min | Respiratory Rate, Breaths/Min |
Leukocyte Count × 103/mm3 |
|
| Tachycardia | Bradycardia | |||
| 1 mo – 1 yr | > 180 | < 90 | > 34 | > 17.5 or < 5 |
| 2 yr – 5 yr | > 140 | N/A | > 22 | > 15.5 or < 6 |
Statistical analysis and sample size
The sample size was 1307 subjects, the sample enrolled for the primary study analysis previously reported.9 Analysis was primarily descriptive. Proportions were calculated along with 95% confidence intervals. All analyses were conducted using SAS 9.3 (Carey, NC).
Results
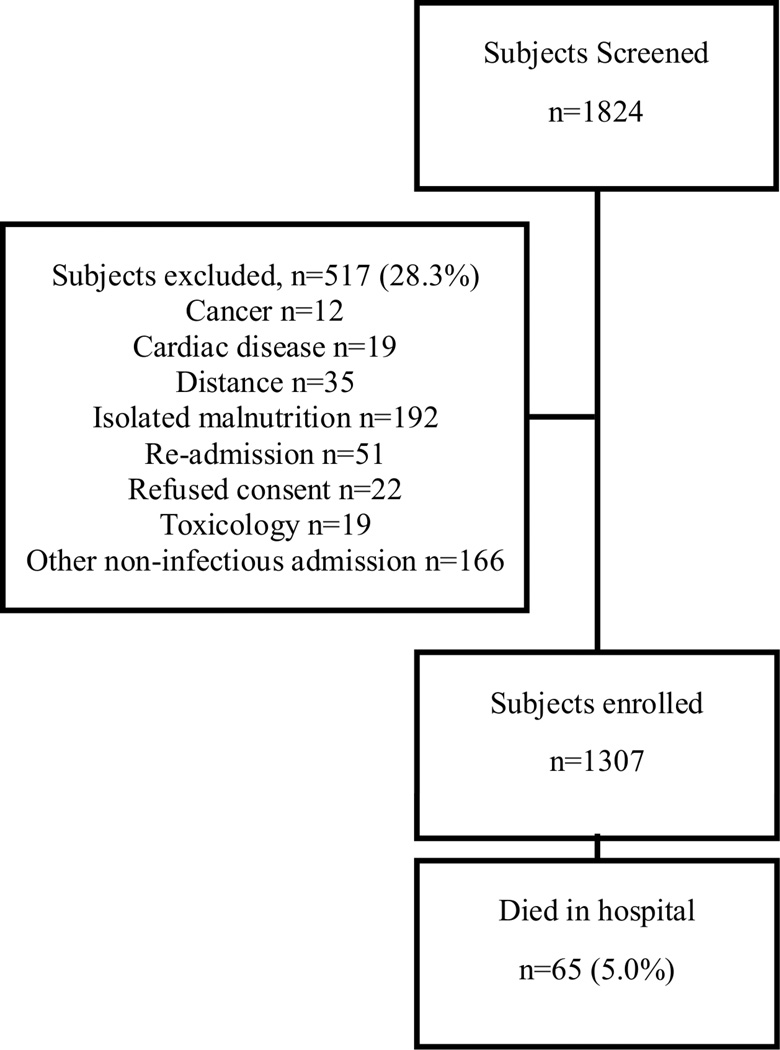
One thousand three hundred and seven (1307) subjects with a confirmed or suspected infection were enrolled following the screening of 1824 admitted subjects during the course of the study (Figure 1). The median age of enrolled subjects was 18 months (IQR 11 – 34) and 717 (54.9%) were male (Table 2). Among the enrolled subjects, 380 (29.1%) were underweight (weight for age z-score < −2), 473 (36.2%) were wasted (weight for height/length z-score <−2) and 368 (28.5%) were stunted (length/height for age z-score <−2). The most common diagnoses made by the medical team during the course of admission included pneumonia (31%), clinical malaria (50%) and gastroenteritis/diarrhea (8%). The median length of stay was 3 days (IQR 2 – 5).
Figure 1.
Consort diagram of study flow
Table 2.
Characteristics of subjects (n=1307)
| General characteristics | Frequency, n (%) |
|---|---|
| Age (months), median (IQR) | 18 (11–34) |
| Male sex | 717 (54.9) |
| Length of stay (days), median (IQR) | 3 (2 – 5) |
| Discharge AMA | 120 (9.7) |
| Duration of illness < 7 days | 841 (64.3) |
| Final diagnoses | |
| Pneumonia | 410 (31.4) |
| Clinical malaria | 659 (50.4) |
| Parasitemia | 434 (33.5) |
| Gastroenteritis | 102 (7.8) |
| Meningitis | 39 (3.0) |
| Comorbidities | |
| HIV | 66 (5) |
| Tuberculosis | 23 (1.8) |
| Anthropometrics | |
| Underweight (WAZ <−2) | 372 (28.6) |
| Severe underweight (WAZ <−3) | 206 (15.9) |
| Wasting (WHZ <−2) | 454 (35.3) |
| Severe Wasting (WHZ <−3) | 237 (18.4) |
| Stunting (HAZ < −2) | 368 (28.5) |
| Severe Stunting (HAZ < −3) | 185 (14.3) |
| MUAC < 125 | 187 (14.5) |
| MUAC < 115 | 94 (7.3) |
| Distance from hospital | |
| < 30 minutes | 339 (25.9) |
| 30 minutes – 1 hour | 290 (22.2) |
| > 1 hour | 678 (51.9) |
AMA: against medical advice; WAZ: weight for age z-score; WHZ: weight for height z-score; HAZ: height for age z-score; MUAC: mid-upper arm circumference
Sepsis and mortality
Over the course of admission, 65 children died (5.0%). The median time to death was 2 days from admission (IQR 1 – 5). Out of the 1307 subjects enrolled with a confirmed or suspected infection, 1121 (85.9%) met the systemic inflammatory response syndrome criteria, and therefore were defined as having sepsis. The sepsis criteria identified 61 out of 64 deaths (1 death was excluded due to missing data resulting in inability to determine SIRS status) among children admitted with an infection, demonstrating a sensitivity and specificity of 95% and 15%, respectively, p=0.027. The corresponding positive and negative predictive values were 5.4% and 98.4%, respectively (Table 3). Of those who died, 27 (42%), 19 (29%), 7 (11%) and 7 (11%) had a final diagnosis of malaria, pneumonia, diarrhea and meningitis, respectively (Table 4). Seven (11%) were diagnosed with more than one primary infection (pneumonia + malaria, pneumonia + meningitis etc.) and 8 (12%) were diagnosed with sepsis that was unspecified.
Table 3.
Characteristics of individual criteria for SIRS and sepsis in study sample
| Criteria | n (%) N = 1307 |
Sensitivity* (95% CI) |
Specificity* (95% CI) |
PPV (%) | NPV (%) |
|---|---|---|---|---|---|
| WBC criteria only | 587 (45.2) | 0.72 (0.61 – 0.83) | 0.56 (0.53 – 0.59) | 7.8 | 97.5 |
| Temp. criteria only | 1042 (79.7) | 0.86 (0.78 – 0.95) | 0.21 (0.18 – 0.23) | 5.4 | 96.6 |
| Heart rate criteria only | 453 (34.7) | 0.38 (0.25 – 0.50) | 0.66 (0.63 – 0.68) | 5.3 | 95.3 |
| RR criteria only | 1246 (95.4) | 0.94 (0.88 – 1.00) | 0.05 (0.03 – 0.06) | 4.8 | 93.3 |
| Sepsis (WBC + Temp.) | 478 (36.8) | 0.59 (0.47 – 0.72) | 0.64 (0.62 – 0.67) | 8.0 | 96.8 |
| Sepsis (WBC + HR) | 219 (16.9) | 0.27 (0.16 – 0.38) | 0.84 (0.82 – 0.86) | 7.8 | 95.7 |
| Sepsis (WBC + RR) | 572 (44.1) | 0.68 (0.56 – 0.80) | 0.57 (0.54 – 0.60) | 7.5 | 97.3 |
| Sepsis (Temp. + HR) | 399 (30.6) | 0.33 (0.21 – 0.45) | 0.70 (0.67 – 0.72) | 5.3 | 95.3 |
| Sepsis (Temp. + RR) | 1001 (76.7) | 0.81 (0.71 – 0.91) | 0.23 (0.21 – 0.26) | 5.2 | 96.1 |
| Sepsis (Full definition) | 1121 (85.9) | 0.95 (0.90 – 1.00) | 0.15 (0.13 – 0.17) | 5.4 | 98.4 |
The sensitivity and specificity refer to the proportion of deaths captured and the proportion of survivors captured by each of the individual SIRS and sepsis criteria, respectfully.
PPV = positive predictive value; NPV = negative predictive value; WBC = leukocyte count; Temp. = axillary temperature; HR = heart rate; RR = respiratory rate
Table 4.
Final diagnoses among those who died as reported by medical team (N = 65)
| Diagnosis | n* (%) |
|---|---|
| Malaria | 27 (41) |
| Pneumonia | 19 (29) |
| Diarrhea | 7 (11) |
| Meningitis | 7 (11) |
| No infection | 2 (3) |
| Sepsis (source not defined) | 8 (12) |
| TB | 2 (3) |
| Measles | 1 (1.5) |
| Any combination | 7 (11) |
numbers add to more than 65 due to overlapping diagnoses in some study subjects
The proportion of children meeting each SIRS criteria and those meeting the sepsis definition based on each combination are shown on Table 3. Overall, 587 (45%) of subjects had a leukocyte abnormality (12% below the age-threshold and 88% above). One thousand and forty-two (80%) had a temperature abnormality, of whom 36 (3.5%) were hypothermic and 1006 (96.5%) were hyperthermic. Four hundred and fifty-three (35%) had a heart rate abnormality. One thousand two hundred forty-six (95%) were tachypneic according to the SIRS criteria. For the five combinations of criteria defining SIRS, abnormal temperature with tachypnea was the most sensitive (81%) providing positive and negative predictive values of 4.8% and 93.3%. The combination of abnormal leukocyte with abnormal heart rate was the most specific (84%) in the prediction of mortality (PPV 7.8%; NPV 95.7). The distribution of diagnoses between these groups did not differ substantially. The presence of any two or any three criteria did not result in any additional improvement in the sensitivity or specificity. Having any two criteria had sensitivity equal to the full sepsis definition, but had lower specificity (0.12) and having any three criteria had equal sensitivity but significantly lower specificity (0.47) than the use of WBC alone.
Septic vs non-septic children
Several differences were noted between those who fulfilled the sepsis criteria and those who did not (Table 5). Older age was associated with sepsis diagnosis, with a mean age of 24.1 months and 20.8 months in those diagnosed with sepsis and no sepsis, respectively, p=0.0059. Children with sepsis had a slightly lower median SpO2 (94% vs 95%), p=0.002). Paradoxically, children with sepsis had higher height for age z-scores. Sepsis was not associated with differences in mid-upper arm circumference, weight for age z-score or weight for height/length z-score. Further, sepsis was not associated with length of stay, hemoglobin at admission or HIV status.
Table 5.
Differences between children fulfilling sepsis criteria and those not fulfilling criteria
| Variable | No sepsis (n=184) | Sepsis (n=1121) | p |
|---|---|---|---|
| Age in months (sd) | 24.2 (15.7) | 20.8 (14.9) | 0.006 |
| Median SpO2 in percent (IQR) | 94 (89–96) | 95 (90–97) | 0.002 |
| Length of stay in days (sd) | 4.6 (4.3) | 4.8 (4.0) | 0.7 |
| WAZ (sd) | −1.2 (1.8) | −1.4 (1.9) | 0.28 |
| HAZ (sd) | −0.6 (2.7) | −1.1 (2.8) | 0.02 |
| WHZ (sd) | −1.4 (2.1) | −1.2 (2.0) | 0.21 |
| MUAC (sd) | 141 (17) | 138 (20) | 0.07 |
| Hg in g/dl (sd) | 8.8 (3.1) | 9.2 (2.6) | 0.11 |
| Percent HIV positive | 5.5% | 3.4% | 0.23 |
| In-hospital mortality | 1.6% | 5.4% | 0.03 |
WAZ: weight for age z-score; WHZ: weight for height z-score; HAZ: height for age z-score; MUAC: mid-upper arm circumference
Discussion
This study is one of the first to quantify the burden of non-neonatal pediatric sepsis among children with proven or suspected infections, using the international consensus definition of sepsis, in a typical resource constrained hospital setting in Africa. The burden of sepsis is very high with most children admitted to hospital with a suspected or confirmed infection being septic by this definition (over 85%). Of all screened subjects (with and without a proven/suspected infection) over 60% were septic. Five percent of admitted children died during the course of their hospital stay. Deaths occurred early during admission, a common observation in this setting. Nearly all enrolled children who died were septic at the time of admission. However, while sepsis was sensitive in identifying children who died it lacked specificity and suggests the need for more specific criteria to identify children at high risk of mortality.
Application of the international consensus definitions of severe sepsis or septic shock may be an alternative starting point in identification of children at high risk of in-hospital mortality. Of the four criteria used in the SIRS definition, an abnormal respiratory rate, followed by an abnormal temperature, were the most common criteria present at admission, with an abnormal respiratory rate occurring in over 95% of children admitted with a suspected infectious illness. The leukocyte count appeared to be the most discriminatory variable among the SIRS variables, with a sensitivity and specificity of 72% and 56%, respectively. This confirms the importance of this parameter in the SIRS definition. However, the resources required for obtaining leukocyte counts are not available in the majority of hospitals and health centers in resource poor countries.
Few studies have evaluated SIRS (or SIRS based-sepsis) in the pediatric context. Hospital studies in Latvia and India have evaluated SIRS prevalence in children but have not evaluated these criteria as potential risk-markers.10,11 In an adult context, a recent study found that among over 100,000 adult ICU patients with severe sepsis (infection with organ dysfunction), nearly 90% were SIRS positive. More importantly, they found that SIRS criteria poorly defined the transition point to death.12 This re-affirms others who have suggested that the SIRS-based sepsis criteria are not ideal for risk prediction.13,14
Several risk scoring models have been developed for the purpose of predicting pediatric mortality, such as the Pediatric Risk of Mortality (PRISM) and the Pediatric Index of Mortality (PIM) models.15–17 These models, developed in high resource environments, have little utility in low resource settings where there are major differences in underlying patient characteristics (malnutrition, HIV etc.) and lack of resources required to measure important variables necessary for these models (ex. fi02, base excess etc.). Thus, in resource poor settings, triage scores and risk prediction are not well established. In an effort to improve care in resource poor countries alternatives such as the emergency triage assessment and treatment (ETAT) program of the WHO has been developed and implemented with notable success in Malawi, where significant reductions in in-hospital mortality were observed.18 This program included the application of a triage system alongside improved coordination with outpatient departments, improved patient flow and extensive training. While the scaling of triage programs such as ETAT must be encouraged, the development of risk-scoring tools could enhance the triage process and aid in clinical management and resource allocation to vulnerable children. Moreover, a robust triage process should be intimately linked with treatment protocols including monitoring to improve outcomes. Another system, the integrated management of childhood illness (IMCI) is well-recognized and increasingly utilized for the diagnosis and treatment of common childhood illnesses in resource poor settings, but has no integrated approach to risk stratification. The use of danger signs could be used for this purpose, and has been evaluated in Tanzania to determine its predictive characteristics.19 In a referral hospital in Northern Tanzania, the presence of one or more danger signs had a sensitivity and specificity of 76% and 38%, respectively to capture children who died in hospital. In our study, a sole leukocyte abnormality had similar characteristics with a sensitivity and specificity of 72% and 56%, respectively. Our research group’s recent analysis of the dataset from which this present study is described has derived a prediction model using only the readily available variables of weight for age z-score, Blantyre coma score and HIV status. Our model had a sensitivity of 83% and specificity of 76% for mortality, significantly higher than either a SIRS based criteria or an IMCI based criteria (submitted).9
Although we found that sepsis as defined by the international consensus conference adds little value in prediction, we feel that “the sepsis syndrome” (infection with organ dysfunction) adds value to the approach to diagnosis and treatment in resource limited settings and that the failure to recognize this is a major drawback in delivering of care in these settings where resources including personnel are few with limited clinical skills and poor laboratory facilities. It is an approach that brings pragmatic solutions for providing care in less than ideal conditions a notion supported by experts in global health.20 In addition, this oversight has led to “the sepsis syndrome” not being recognized as a cause of death in children in the Global Burden of Diseases Statistics which impedes investments and major efforts to address sepsis.21
This study is subject to several limitations. First, sepsis criteria were evaluated only at a single point in time, the time of admission and could not assess the development of sepsis throughout the hospital admission. Second, this study only evaluated the presence of SIRS in those with a proven or suspected infection. Of the 517 excluded subjects who were admitted due to non-infectious reasons, the prevalence of SIRS (and mortality) remains unknown in this context. Related to this is the fact that suspected infections may not have been proven in many cases. This is a limitation in the environment where this research was conducted where significant resource limitations make such investigations difficult, if not impossible to conduct on a routine basis. Another limitation is that this study did not evaluate the care received by subjects during their hospital stay as a means to determine if therapy was relevant to outcome. Finally, this study is limited by the fact that it only enrolled subjects from two hospitals and therefore may not be representative of other hospitals and health centers in East Africa. Other areas with different patient acuity and varying proportions of diseases (such as malaria) may significantly alter the performance of a sepsis diagnosis in relation to in-hospital mortality.
Conclusion
In conclusion, sepsis is present among most children 6 months to 5 years admitted to the hospital in Uganda. The consensus definition of sepsis, while sensitive in capturing children who die during hospitalization, lacks specificity. Other methods of risk stratification should be used to aid in triage in this context, and new and more specific definitions of sepsis relevant to this context must be developed.
Acknowledgments
Funding: This study was funded through internal funds by the Center for International Child Health, BC Children’s Hospital, Vancouver, BC
We gratefully acknowledge the contributions of Annet Twinomuguni, Justine Kamazima, Agaba Collins, Clare Komugisha, Solome Kobugyenyi, Alexander Mutungi and Hassan Bariahikwa. Without their dedication this study could not have been completed.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare
References
- 1.Goldstein B, Giroir B, Randolph A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6(1):2–8. doi: 10.1097/01.PCC.0000149131.72248.E6. [DOI] [PubMed] [Google Scholar]
- 2.Corfield AR, Lees F, Zealley I, et al. Utility of a single early warning score in patients with sepsis in the emergency department. Emerg Med J. 2014;31(6):482–487. doi: 10.1136/emermed-2012-202186. [DOI] [PubMed] [Google Scholar]
- 3.Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign. Crit Care Med. 2013;41(2):580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 4.Duke T. Systemic inflammatory response syndrome and bacteremia in developing countries. Pediatr Crit Care Med. 2010;11(1):153–154. doi: 10.1097/PCC.0b013e3181bc5828. [DOI] [PubMed] [Google Scholar]
- 5.Wiens MO, Kumbakumba E, Kissoon N, Ansermino JM, Ndamira A, Larson CP. Pediatric sepsis in the developing world: challenges in defining sepsis and issues in post-discharge mortality. Clin Epidemiol. 2012;4:319–325. doi: 10.2147/CLEP.S35693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wiens MO, Kumbakumba E, Larson CP, et al. Postdischarge mortality in children with acute infectious diseases: derivation of postdischarge mortality prediction models. BMJ Open. 2015;5(11):e009449. doi: 10.1136/bmjopen-2015-009449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uganda Clinical Guidelines 2010: National Guidelines on the Managment of Common Conditions. Uganda: Kampala; 2010. [Google Scholar]
- 8.Stine Ca, Flook DM, Vincze DL. Rectal Versus Axillary Temperatures: Is There a Significant Difference in Infants Less Than 1 Year of Age? J Pediatr Nurs. 2012;27(3):265–270. doi: 10.1016/j.pedn.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 9.Wiens MO. Childhood mortality from acute infectious diseases in Uganda: Studies in sepsis and post-discharge mortality. 2015 http://hdlhandlenet/2429/53787. [Google Scholar]
- 10.Pavare J, Grope I, Gardovska D. Prevalence of systemic inflammatory response syndrome(SIRS) in hospitalized children: a point prevalence study. BMC Pediatr. 2009;9(1):25. doi: 10.1186/1471-2431-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ganjoo S, Ahmad K, Qureshi UA, Mir ZH. Clinical Epidemiology of SIRS and Sepsis in Newly Admitted Children. Indian J Pediatr. 2014 Aug;82:698–702. doi: 10.1007/s12098-014-1618-x. [DOI] [PubMed] [Google Scholar]
- 12.Kaukonen K-M, Bailey M, Pilcher D, Cooper DJ, Bellomo R. Systemic Inflammatory Response Syndrome Criteria in Defining Severe Sepsis. 2015:1629–1638. doi: 10.1056/NEJMoa1415236. [DOI] [PubMed] [Google Scholar]
- 13.Brilli RJ, Goldstein B. Pediatric sepsis definitions: past, present, and future. Pediatr Crit Care Med. 2005;6(3 Suppl):S6–S8. doi: 10.1097/01.PCC.0000161585.48182.69. [DOI] [PubMed] [Google Scholar]
- 14.Vincent JL, Opal SM, Marshall JC, Tracey KJ. Sepsis definitions: Time for change. Lancet. 2013;381(9868):774–775. doi: 10.1016/S0140-6736(12)61815-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pollack M, Ruttimann U, Getson P. Pediatric risk of mortality (PRISM) score. [Accessed February 20, 2015];Crit Care Med. 1988 16(11):1110–1116. doi: 10.1097/00003246-198811000-00006. http://journals.lww.com/ccmjournal/Abstract/1988/11000/Pediatric_risk_of_mortality__PRISM__score.6.aspx. [DOI] [PubMed] [Google Scholar]
- 16.Shann F, Pearson G, Slater a, Wilkinson K. Paediatric index of mortality (PIM): a mortality prediction model for children in intensive care. Intensive Care Med. 1997;23(2):201–207. doi: 10.1007/s001340050317. [DOI] [PubMed] [Google Scholar]
- 17.Slater A, Shann F, Pearson G. PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med. 2003;29(2):278–285. doi: 10.1007/s00134-002-1601-2. [DOI] [PubMed] [Google Scholar]
- 18.Molyneux E, Ahmad S, Robertson A. Improved triage and emergency care for children reduces inpatient mortality in a resource-constrained setting. Bull World Health Organ. 2006;84(04):314–319. doi: 10.2471/blt.04.019505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clifton DC, Ramadhani HO, Msuya LJ, et al. Predicting mortality for paediatric inpatients where malaria is uncommon. Arch Dis Child. 2012;97(10):889–894. doi: 10.1136/archdischild-2012-301812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riviello ED, Sugira V, Twagirumugabe T. Sepsis research and the poorest of the poor. Lancet Infect Dis. 2015;15(5):501–503. doi: 10.1016/S1473-3099(15)70148-9. [DOI] [PubMed] [Google Scholar]
- 21.Kissoon N, Uyeki TM. Sepsis and the Global Burden of Disease in Children. JAMA Pediatr. 2015;(14):1–2. doi: 10.1001/jamapediatrics.2015.3241. [DOI] [PMC free article] [PubMed] [Google Scholar]