Highlights
-
•
Inflammatory myofibroblastic tumor, most common involvement is seen in the lungs, but in this case liver gallbladder, pylorus, 1st part of duodenum was involved.
-
•
Most specific feature of IMTs, whose main cell type is myofibroblasts, is the ability to mimic malignancy.
-
•
Surgery is the main treatment.
Keywords: Inflammatory myofibroblastic tumor, Liver, Gallbladder, Pylorus, 1st Part of duodenum, CT SCAN, Extended cholycystectomy + billroth II gastrectomy
Abstract
Inflammatory myofibroblastic tumors are rare benign tumors that can mimic malignancy of unknown aetiology. It has spectrum of myofibroblastic proliferation along with varying amount of inflammatory infiltrate. Recently, the concept of this lesion being reactive has been challenged based on the clinical demonstration of recurrences and metastasis and cytogenetic evidence of acquired clonal chromosomal abnormalities. We hereby report a case of inflammatory myofibroblastic tumor involving liver, gallbladder pylorus and 1st part of duodenum.
1. Introduction
Inflammatory myofibroblastic tumor (IMT) occurs more frequently in childhood and the most common involvement is seen in the lungs. Different terms have been applied to the lesion, namely,inflammatory pseudotumor, fibrous xanthoma, plasma cell granuloma, pseudosarcoma, lymphoid hamartoma, myxoid hamartoma, inflammatory myofibrohistiocytic proliferation, benign myofibroblatoma, and most recently, inflammatory myofibroblastic tumor [1]. Primary inflammatory myofibroblastic tumors of the gallbladder are rather infrequent. The present knowledge is based on case reports.
IMT was first observed in lungs and described by Bunn in 1939. It was named as IMT by Umiker et al. because it mimics malignant neoplasm clinically, radiologically and histopathologically [1]. Initiating factors such as reactive,infections, autoimmune and neoplastic processes, has been proposed but the aetiology of most remains unknown.
2. Presentation of case
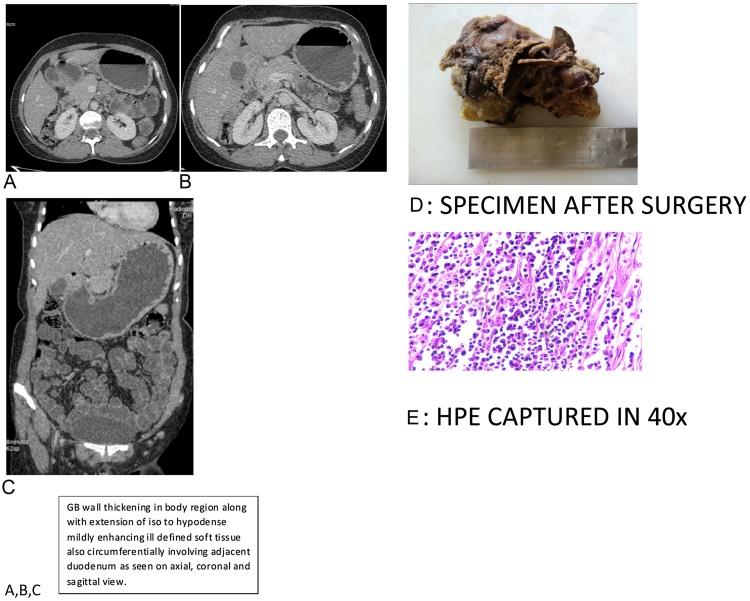
We present a case of 36 yrs old female who came to surgery OPD having chief complaint of bloating of abdomen and dyspepsia for 5 months. On examination her vitals were stable. On abdominal examination it was Soft, no organomegaly noted. Routine Blood investigation were within normal limits. Ultrasonography of whole abdomen revealed gall bladder calculi with asymmetric wall thickening (9 mm). The interface with liver is hazy. As noted by ultasonography of having asymmetric wall thickening CT SCAN was done. CT SCAN abdomen report revealed-GB shows mild diffuse wall thickening with asymmetric wall thickening in body region extending along the adjacent duodenum with circumferential thickening of the duodenal wall causing slight luminal narrowing with mild proximal gastric distention. Fat plane between GB & lesion poorly visualised with mild hepatic altered attenuation (depth upto 1 cm). No significant biliary dilation (Fig. 1 (A,B,C)). As the patient was only presenting with bloating of abdomen & dyspepsia, without any significant features of obstruction, upper GI endoscopy was done to rule out any hiatal disorders, ulcers & to take biopsies if possible. Upper GI endoscopy was also normal. Hence planing was to do Extended cholecystectomy. But intraoperatively it was found that there were lots of adhesion at gall bladder- liver interface & pylorus on palpating gallbladder wall appeared thick with full of calculi. There was thick & hard mass like feeling at pylorus which was extending to 1st part of duodenem. Hence, Extended cholecystectomy with resection of pylorus and 1st part of duodenum with peripancreatic lymph node dissection, billrothII anastomosis done under general anaesthesia & specimen sent for HPE (Fig. 1 D). Histopathology shows-Inflamatory myofibroblastic tumor with involvement of liver & resected end of pylorus & duodenum with associated chronic cholecystitis (Fig. 1 E).
Fig. 1.
(A,B,C) GB wall thickening in body region along with extension of iso to hypodense mildly enhancing ill defined soft tissue also circumferentially involving adjacent duodenum as seen on axial, coronal and sagittal view. (CT SCAN).
Contribution of all athours were there, as from preoperative preparation to postoperative outcome, as the patient was discharged from hospital unevenfully after histopathology report, & instructed to follow up.
3. Discussion
Inflammatory myofibroblastic tumors are rare benign structures with unknown aetiology.IMT occurs mainly in children and young adult.IMT in the pediatric abdomen have clinical importance because the lesion often mimic malignant neoplasm, such as sarcoma, lymphomas, or metastases [2].
Lymphocytes, plasma cells, histiocytes, fibroblasts and myofibroblasts are the basic components of IMT, present in variable proportions.
Four basic histologic patterns are commonly seen as follows:
-
a.)
Dominant lymphoplasmacytic infiltrate;
-
b.)
Dominant lymphohistiocytic infiltrate;
-
c.)
Young and active myofibroblastic process and
-
d.)
Predominantly collagenized process with lymphocytic infiltrate.
The lymphoplasmacytic IMT consists of a mature lymphoid and plasma cell infiltrate with germinal centers, hence the name given is plasma cell granuloma [3]. Lymphohistiocytic IMT most commonly resembles an infectious process as foamy histiocytes are predominant [3]. Collagenized IMT is less cellular and resembles a desmoid tumor but with a prominent inflammatory infiltrate. A zonation/maturation effect may be observed. The most specific feature of IMTs, whose main cell type is myofibroblasts, is the ability to mimic malignancy. A histopathological examination of the IMTs revealed numerous lymphocytes, plasma cells and histiocytes settled between the spindle cells and fibrous tissues [4]. Although IMT was first described by Brunn, its pathological entities were identified in detail by Umiker and Iverson in 1954 [5]. Two theories have been emphasised to explain the aetiopathogenesis: the first is an abnormal host response to tissue damage, while the second is disorders in immunological responses [6], [7]. IMTs are known to be benign tumors with no capacity to metastasise. However, these tumors are known to infiltrate surrounding tissues due to their severe proliferative capacity and they are thus known to recur frequently, even after resection [8].
The most frequently involved organ in the abdomen is the liver, while primary gallbladder involvement is quite rare. Present knowledge about this entity is based on case reports in the literature [9]. The clinical picture in cases with IMT depends on the organ of involvement and site of the organ; abdominal pain, jaundice and ascites might be the presenting symptoms, according to the localisation in the liver involvement.
Gallbladder involvement, on the other hand, may result in acute cholecystitis, biliary colic, obstructive jaundice and cholangitis may be seen in cases with extension to the common bile duct. In our case symptoms were abdominal pain and dyspepsia. CT demonstrated involvement of liver, gallbladder, pylorus, & 1st part of duodenum,which is rare. Hence, intraoperatively Extended cholycystectomy + BillrothII gastrectomy done.
4. Conclusion
Inflamatory myofibroblastic tumor of liver, gallbladder,pylorus, duodenum is rare. Hence,surgery is the main treatment.
Conflicts of interest
None.
Funding
None.
Ethical approval
None.
Consent
Yes.
Author contribution
Dr Lakshmi sinha – study concept,design & writing paper.
Dr Arsad hasan – writing paper.
Dr Akhilesh kumar singh – writing paper.
Dr poonam prasad bhadani – pathology updates.
Dr achuta nand jha – radoilogy interpretation.
Dr Prashant kumar singh – data collection.
Dr Manoj Kumar – data interpretation.
Guarantor
Dr Lakshmi Sinha.
Contributor Information
Lakshmi Sinha, Email: dr.sannu2010@gmail.com.
Arshad Hasan, Email: arshadsurgery@gmail.com.
Akhilesh Kumar Singh, Email: dr.akhi2010@gmail.com.
Poonam Prasad Bhadani, Email: bhadanipunam@gmail.com.
Achyuta Nand Jha, Email: radiologysolution@gmail.com.
Prashant Kumar Singh, Email: pras_doc@yahoo.com.
Manoj Kumar, Email: drmanojk@aiimspatna.org.
References
- 1.Poh C.F., Priddy R.W., Dahlman D.M. Intramandibular inflammatory myofibroblastic tumor: A true neoplasm or reactive lesion. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005;100:460–466. doi: 10.1016/j.tripleo.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 2.kim Su Jin, Kim Woo Sun, Cheon Jung-Eun, Shin Su-Mi, Youn Byung Jae, Kim In-One, Yeon Kyung Mo. Am. J. Roentgenol. 2009;193:1419–1424. doi: 10.2214/AJR.09.2433. [DOI] [PubMed] [Google Scholar]
- 3.Margaret S., Silloo B.K., Gnepp D.R. Nonsquamous pathology of the larynx, hypopharynx, and trachea. In: Gnepp D.R., editor. Diagnostic Surgical Pathology of the Head and Neck. 4th ed. W.B. Saunders Company; New York: 2001. pp. 287–288. [Google Scholar]
- 4.Makimoto Y., Nabeshima K., Iwasaki H., Ishiquro A., Miyoshi T., Shiraishi T. Inflammatory myofibroblastic tumor of the posterior mediastinum: an older adult case with anaplastic lymphoma kinase abnormalities determined using immunohistochemistry and fluorescence in situ hybridization. Virchows Arch. 2005;446:451–455. doi: 10.1007/s00428-004-1170-6. [DOI] [PubMed] [Google Scholar]
- 5.Wang T.Y., Chou J.W., Shih Y.S., Hsieh T.C. Inflammatory myofibroblastic tumor mimicking adrenal incidentaloma. Intern. Med. 2011;50:165–166. doi: 10.2169/internalmedicine.50.4545. [DOI] [PubMed] [Google Scholar]
- 6.Meis-Kindblom J.M., Kjellström C., Kindblom L.G. Inflammatory fibrosarcoma: update, reappraisal, and perspective on its place in the spectrum of inflammatory myofibroblastic tumors. Semin. Diagn. Pathol. 1998;15:133–143. [PubMed] [Google Scholar]
- 7.Fletcher C.D. Myofibroblastic tumors: an update. Verh. Dtsch. Ges. Pathol. 1998;82:75–82. [PubMed] [Google Scholar]
- 8.Coffin C.M., Watterson J., Priest J.R., Dehner L.P. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am. J. Surg. Pathol. 1995;19:859–872. doi: 10.1097/00000478-199508000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Karahan O.I., Işin S., Baykara M., Coşkun A. Case report: Inflammatory pseudotumor of the liver with target-like appearance. Tani Girisim Radyol. 2003;9:75–77. [PubMed] [Google Scholar]