Abstract
Platelet activation has been described in patients with chronic inflammation, however in type 2 diabetes mellitus it remains controversial. We compared levels of platelet leucocyte aggregates, monocyte and granulocyte activation across glucose tolerance statuses in mixed ancestry South Africans. Individuals (206) were recruited from Bellville-South, Cape Town, and included 66% with normal glucose tolerance, 18.7% pre-diabetes, 8.7% screen-detected diabetes and 6.3% known diabetes. Monocyte and neutrophil activation were measured by calculating the percentage of cells expressing CD142 and CD69 while platelet monocyte aggregates were defined as CD14++ CD42b+ events and platelet neutrophil aggregates as CD16++ CD42b+ events. The percentage of monocytes and neutrophils expressing CD69 and CD142 was significantly higher in known diabetes and prediabetes, but, lowest in screen-detected diabetes (both p ≤ 0.016). The pattern was similar for platelet monocyte and neutrophil aggregates (both p ≤ 0.003). In robust linear regressions adjusted for age and gender, known diabetes was significantly and positively associated with the percentage of monocytes expressing CD69 [beta 11.06 (p = 0.016)] and CD42b (PMAs) [19.51 (0.003)] as well as the percentage of neutrophils expressing CD69 [14.19 (<0.0001)] and CD42b [17.7 (0.001)]. We conclude that monitoring platelet activation in diagnosed diabetic patients may have a role in the management and risk stratification.
Type 2 diabetes mellitus (T2D) is a metabolic disorder which is characterised by insulin resistance, defective insulin secretion or both. The consequent chronic state of hyperglycaemia is associated with chronic inflammation and atherothrombotic complications. It is thought that the pro-inflammatory environment leads to the vascular endothelial surface attracting both platelets and leucocytes which become activated, bind to the extracellular matrix and play a major role in the development of plaques and pathological thrombosis1.
Hyperinsulinaemia is a key pathogenic feature of T2D and both insulin and glucose has a direct effect on platelet function. It has been reported that glucose induces platelet hyperactivity via direct effects on cellular osmolality2,3 and activation of the protein kinase C (PKC) transduction pathway4. On the other hand, while insulin binds to the insulin receptor (IR) and inhibits platelet activation in normal individuals, recent research has suggested that in patients with T2D, platelets have reduced expression of the receptor and appear to be unable to respond to insulin5. Therefore although further research is needed, this could offer a further explanation for the hyperactivity, increased adhesiveness and responsiveness of platelets in T2D6,7,8.
Activated platelets play a key role in the initiation of both inflammation and coagulation9. Upon activation platelets degranulate and express a repertoire of membrane receptors which enable them to bind to circulating leukocytes via P-selectin6. P-selectin mediated interactions in turn activate leukocyte signal transduction pathways10 and initiate the rapid formation of platelet leukocyte aggregates (PLAs)11. Activated platelets preferentially bind to monocytes and form platelet monocyte aggregates (PMAs)11,12 which are a more sensitive and robust marker of platelet activation than the expression of P-selectin13,14.
Elevated circulating PMAs and PLAs have been described as an early marker of T2D15 and have also been reported in association with thrombotic16 and inflammatory conditions13,17. Importantly both PMA’s and PLA’s have been associated with vascular damage18. Although platelet activation has been described in patients with chronic inflammation, the presence of increased PMA’s in T2D remains controversial and recent research has shown that high risk T2D patients have normal functioning platelets with no increase in PMA’s or PLA’s19.
Therefore, although there is growing evidence that platelets and cells of the innate immune system are involved in the process of chronic inflammation and cardiovascular disease, their role in type 2 diabetes remains unclear. This study therefore aimed to investigate this issue by assessing the activation of neutrophils and monocytes. In addition, platelet activation was assessed by the measurement of platelet leukocyte aggregates across the spectrum of glucose tolerance in South African mixed ancestry individuals.
Materials and Methods
Ethical approval of the study
This investigation is based on the Bellville South (Ward 009) study20 from Cape Town that has been approved by the Research Ethics Committees of the Cape Peninsula University of Technology (CPUT) and Stellenbosch University (respectively, NHREC: REC - 230 408–014 and N14/01/003). For this sub-study, ethical approval was also obtained from the CPUT Health and Wellness Sciences Research Ethics Committee (CPUT/HW-REC 2014/H07). The study was conducted according to the Code of Ethics of the World Medical Association (Declaration of Helsinki). All participants signed written informed consent after all the procedures had been fully explained in the language of their choice.
Study design and procedures
This was a cross-sectional study involving participants from the ongoing Cape Town Vascular and Metabolic Health (VMH) study. VMH is an extension of the Cape Town Bellville South study, which has been described in detail previously20. Participants were eligible for this study if they had undergone an overnight fast and were not on aspirin or anti-inflammatory drugs for a minimum of 14 days prior to sampling. In addition, participants were excluded if they showed clinical signs of recent infection, were pregnant or using immunosuppressant drugs. Data collection was based on a standardised questionnaire which included questions regarding the smoking status of the participant and was available in the electronic form on a password-protected personal digital assistant (PDA). Upon completion of the assessment of each participant, data were automatically encrypted and transmitted via mobile internet connection to a dedicated server, from which they were checked for completion, downloaded and stored for future use. Physical examination involved data collection on blood pressure (BP) which was measured according to the World Health Organisation (WHO) guidelines21, using a semi-automatic digital blood pressure monitor (Omron M6 comfort-preformed cuff BP Monitor) on the right arm in sitting position and at rest for at least 10 minutes. Body weight (to the nearest 0.1 kg) was measured with the subject in light clothing and without shoes, using an Omron body fat meter HBF-511digital bathroom scale, which also measures visceral fat, body fat percent and resting metabolic rate (RMR). Height to the nearest centimetre was measured with a stadiometer, with subjects standing on a flat surface. Body Mass Index (BMI) was calculated as weight per square meter (kg/m2). Waist circumference was measured with a non-elastic tape at the level of the narrowest part of the torso, as seen from the anterior view. Blood Pressure (BP) and anthropometric measurements were performed three times and their average used for analysis.
Biochemical Assays
Blood samples were collected from all participants following an overnight fast. A 2-hour sample was obtained after a 75 g oral glucose tolerance test (OGTT) in participants with no history of doctor diagnosed diabetes mellitus. Routine biochemical parameters were analyzed at an ISO 15189 accredited Pathology practice (PathCare, Reference Laboratory, Cape Town, South Africa). Blood glucose (mmol/L) was measured using the enzymatic hexokinase method (Beckman AU, Beckman Coulter, South Africa). Insulin (mmol/L) was determined by a paramagnetic particle chemiluminescence assay (Beckman DXI, Beckman Coulter, South Africa). HDL-C (mmol/L) was by enzymatic immunoinhibition – End Point (Beckman AU, Beckman Coulter, South Africa). Low-density lipoprotein cholesterol (LDL-C) (mmol/L) was measured by enzymatic selective protection – End Point (Beckman AU, Beckman Coulter, South Africa). Triglycerides (TG) (mmol/L) were estimated by glycerol phosphate oxidase-peroxidase, End Point (Beckman AU, Beckman Coulter, South Africa). Glycated haemoglobin (HbA1c) was measured by High Perfomance Liquid Chromotography (Biorad Variant Turbo, BioRad, South Africa). Ultra sensitive C-reactive protein (U-CRP) was by Latex Particle immunoturbidimetric and the liver enzymes γ-Glutamyltransferase (GGT), alanine aminotransferase (ALT) and aspartate transaminase (AST) were measured using International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) standardized reagents on a Beckman AU (Beckman Coulter, South Africa). Serum cotinine was measured by Competitive Chemiluminescent on Immulite 2000 (Siemens, Southern Africa). Full blood counts and platelets were measured on a Coulter LH 750 hematology analyser (Beckman Coulter, South Africa).
History, fasting glucose, and 2-hour glucose following OGTT were used to group participants for glucose tolerance status as normotolerant, prediabetes (including impaired fasting glycaemia, impaired glucose tolerance or the combination of both), screen-detected diabetes, and known diabetes, following the WHO criteria22. Cotinine levels were used to define smoking status based on a threshold of >50 ng/ml to characterise current smoking23.
Flow cytometry
A volume of 2–3 ml of venous blood was collected into 4.5 ml tubes containing 3.2% sodium citrate (BD Vacutainer, San Jose, CA). To minimise artefactual activation due to tissue factor contamination, the first blood sample drawn was not used for flow cytometry. Measurements of platelet leukocyte aggregates were performed using fresh blood samples stained within 10 minutes of collection and analysed immediately to minimise the effects of time-dependent platelet and leukocyte activation kinetics24. This was made possible by the close proximity of the research clinic and the laboratory, both situated in the Department of Biomedical Sciences, Faculty of Health and Wellness Sciences, Cape Peninsula University of Technology.
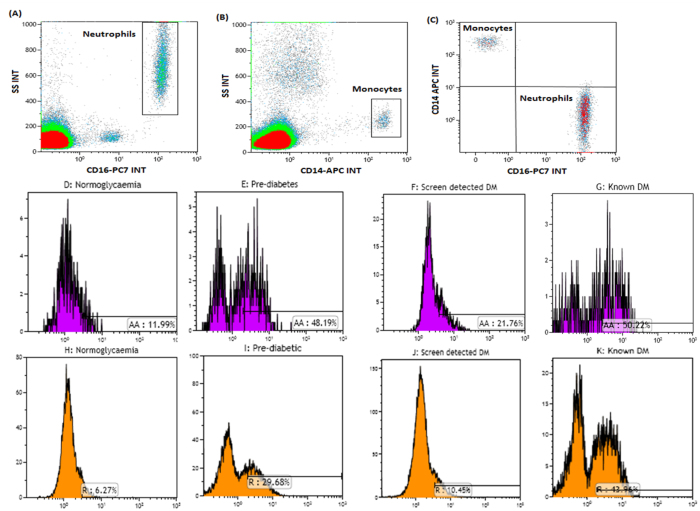
The anti-human CD42b-FITC (SZ2); CD69-PC5 (TP1.55.3), CD14 APC (RM052), CD16-PC7 (3G8) antibodies were all purchased from Beckman Coulter, USA while anti-human CD142-PE (NY2) was purchased from Biolegend Inc, San Diego, CA. A multi-colour panel was set up to measure the levels of monocyte and neutrophil activation in peripheral whole blood. The flow cytometric measurement of PMAs and PNAs was performed as previously described25. Briefly, 50 μl of citrated whole blood was stained using 5 μl of the titrated monoclonal antibody cocktail and incubated for 15 minutes at room temperature. Red blood cell lysis was performed by incubating the samples with 500 μl FACSlyse (BD Biosciences, San Jose, CA) and thereafter diluted with 500 μl of PBS (without calcium or magnesium chloride). The stained cells were processed immediately using the Navios cytometer and analysed with the Kaluza V 1.3 analysis software (Beckman Coulter, USA) using the gating strategy shown in Fig. 1. Bright CD14++ monocytes and CD16++ neutrophils were gated (Fig. 1A,B). A Boolean gate was created (using the logic; Neutrophil “OR” Monocyte) and applied to ensure the gating of classical monocytes (CD14++ CD16−) and unbound neutrophils (CD16++ CD14−) (shown in Fig. 1C). FMO controls were used to distinguish tissue factor (CD142), CD69 (a marker of activation) positive and negative events.
Figure 1. Gating strategy used to measure PMAs and PNAs.
Classical monocytes and neutrophils expressing CD42b were regarded as PMAs and PNAs respectively. CD16++ neutrophils and CD14++ monocytes were gated as shown in (A and B). To further ensure that only classical monocytes (CD14++ CD16−) and unbound neutrophils (CD16++ CD14−) were analysed, the Boolean gate (Neutrophil “OR” Monocyte) was applied (shown in C). The expression of CD42b was then measured on both classical monocytes (D–G) and classical neutrophils (H–K).
The expression of CD42b on CD14++ monocytes and CD16++ neutrophils was assessed (Fig. 1D–K). An FMO control was used to distinguish between platelet bound (CD42b+) and unbound (CD42b−) monocytes and neutrophils. Platelet monocyte aggregates were defined as CD14++ CD42b+ events (Fig. 1D–G) and platelet neutrophil aggregates were defined as CD16++ CD42b+ events (Fig. 1H–K). A minimum of 2000 CD14+ events at a medium flow rate were counted for the analysis of platelet leukocyte aggregates. The mean fluorescent intensity (MFI) of expression was recorded as the geometric mean and was obtained from the relevant flow cytometric histogram using Kaluza v1.3 analysis software.
Quality control measures
Daily cleaning of the flow cell fluidics line was performed using filtered Isoflo and Clenz® (Beckman Coulter, USA). For daily monitoring of instrument performance, flow set beads (Beckman Coulter, USA) and flow check pro beads (Beckman Coulter, USA) were used and plotted on a levy Jennings plot. Antibody titrations were performed to determine the optimal antibody concentrations and colour compensation was performed using the versa comp antibody capture beads (Beckman Coulter, USA).
Statistical analysis
Data were analysed with the used of R statistical software version 3.2.2 [2015-08-14] (The R Foundation for Statistical Computing Platform, Austria). Categorical variables are summarised as count and percentages and quantitative variables as mean (standard deviation) or median (25th–75th percentiles). Variable comparisons across glucose tolerance statuses used chi square test, Analysis of the Variance (ANOVA) and Kruskal-Walis tests. The effects of glucose tolerance status and other predictors on platelet leucocyte aggregates, monocyte and granulocyte activation, was investigated using robust linear regressions models. Unlike conventional least squares based linear regressions, robust regressions are not sensitive to the effects of outliers which can be common with the outcome variables of interest in the current study, or when dealing with relatively small groups of participants. A p-value < 0.05 was used to characterise statistically significant results.
Results
General characteristics of the participants
The study sample comprised of 206 participants which included 136 (66%) with normal glucose tolerance, 39 (18.7%) with prediabetes (impaired fasting glycaemia and/or glucose tolerance), 18 (8.7%) with screen-detected diabetes and 13 (6.3%) with known diabetes all receiving at least metformin therapy (Table 1). The overall mean age was 52.2 (SD = 14.0) years, with a significant variation in glucose tolerance status (p = 0.007). One hundred and forty seven (71.4%) participants were female while eighty eight (42.9%) were smokers. There was no significant difference of both attributes across glucose tolerance status (both p > 0.103). Overall, the mean values (SD) for anthropometric measurements were as follows: body mass index (BMI) 29.5 (8.1) kg/m2, waist circumference 95 (15) cm, hip circumference 108 (15) cm, waist to hip ratio 0.88 (0.08) and systolic blood pressure 129 (24) mmHg. For all these measurements the lowest values occurred in the normo-tolerant group while the highest was amongst participants with screen-detected diabetics. The general characteristics of the participants are summarised in Table 1.
Table 1. Characteristics of 206 participants according to glucose tolerance status.
| Overall | Normol | Pre-diabetes | Screen-detected Diabetes | Known Diabetes | p-value | |
|---|---|---|---|---|---|---|
| N | 206 (100) | 136 (66.0) | 39 (18.9) | 18 (8.7) | 13 (6.3) | |
| Female, n (%) | 147 (71.4) | 95 (69.8) | 29 (74.4) | 13 (72.2) | 10 (76.9) | 0.913 |
| Smoking, n (%) | 88 (42.9) | 65 (48.1) | 13 (33.3) | 4 (22.2) | 6 (46.1) | 0.103 |
| Age (years) | 52.2 (14.0) | 49.8 (14.0) | 57.1 (14.4) | 56.4 (12.2) | 56.5 (7.2) | 0.007 |
| BMI, kg/m2 | 29.5 (8.1) | 28.6 (8.6) | 30.1 (7.3) | 33.6 (5.0) | 31.1 (6.4) | 0.045 |
| Waist-C, cm | 95 (15) | 93 (16) | 98 (13) | 107 (10) | 102 (13) | 0.0005 |
| Hip-C, cm | 108 (15) | 107 (16) | 109 (14) | 111 (9) | 110 (14) | 0.405 |
| Waist-to-hip ratio | 0.88 (0.08) | 0.87 (0.08) | 0.90 (0.07) | 0.96 (0.07) | 0.92 (0.06) | <0.0001 |
| Systolic BP, mmHg | 129 (24) | 124 (23) | 136 (23) | 146 (25) | 129 (17) | 0.0005 |
| Diastolic BP, mmHg | 84 (13) | 83 (13) | 84 (12) | 89 (13) | 87 (9) | 0.222 |
| Visceral fat, levels | 10 [7–13] | 9 [6–12] | 10.5 [8.7–13.2] | 12.5 [10.0–13.7] | 12.0 [9.7–14.0] | 0.0008 |
| Body fat, % | 42.2 [30.4–49.2] | 41.2 [27.5–48.4] | 44.3 [33.6–48.7] | 49.4 [40.1–51.4] | 45.9 [35.5–50.6] | 0.044 |
| RMR, Kcal | 1469 [1324–1625] | 1461 [1300–1601] | 1460 [1378–1623] | 1564 [1498–1622] | 1542 [1416–1708] | 0.146 |
| HbA1c (%) | 6.0 (1.2) | 5.6 (0.4) | 5.9 (0.6) | 7.3 (1.2) | 8.7 (2.5) | <0.0001 |
| FBG, mmol/L | 5.5 (2.2) | 4.7 (0.5) | 5.5 (0.7) | 8.1 (2.6) | 10.8 (4.6) | <0.0001 |
| 2-hour glucose, mmol/L | 7.0 (3.3) | 5.4 (1.3) | 8.9 (1.4) | 14.7 (3.7) | — | <0.0001 |
| Fasting insulin, mIU/L | 7.6 [5.0–10.9] | 6.8 [4.2–9.5] | 9.1 [6.3–13.9] | 12.4 [8.1–20.1] | 12.4 [8.1–20.1] | <0.0001 |
| 2-hour insulin, mIU/L | 47.4 [24.7–79.4] | 35.0 [17.8–63.6] | 70.3 [48.2–112.4] | 72.7 [44.9–88.6] | — | <0.0001 |
| TC, mmol/L | 5.3 (1.1) | 5.3 (1.1) | 5.1 (0.9) | 6.0 (1.2) | 5.6 (1.1) | 0.027 |
| HDL-C, mmol/L | 1.3 (0.3) | 1.3 (0.3) | 1.3 (0.3) | 1.1 (0.2) | 1.0 (0.2) | 0.010 |
| LDL-C, mmol/L | 3.3 (1.0) | 3.3 (0.9) | 3.2 (0.9) | 4.0 (1.0) | 3.7 (0.9) | 0.009 |
| Triglycerides, mmol/L | 1.2 [0.9–1.7] | 1.1 [0.8–1.6] | 1.4 [0.9–1.8] | 1.7 [1.4–2.3] | 1.6 [1.2–2.5] | <0.0001 |
| U-CRP, mg/L | 4.0 [1.9–9.5] | 3.6 [1.4–9.1] | 3.9 [1.9–6.5] | 7.3 [3.8–14.7] | 8.7 [3.0–12.6] | 0.023 |
| Cotinine, ng/mL | 10 [10–279] | 10 [10–293] | 10 [10–243] | 10 [10–10] | 10 [10–269] | 0.191 |
| γGT, U/L | 31 [21–45] | 30 [20–40] | 27 [22–41] | 61 [37–82] | 31 [26–68] | 0.002 |
| AST, U/L | 22 [19–26] | 22 [19–25] | 21 [18–25] | 24 [21–32] | 22 [15–30] | 0.271 |
| ALT, U/L | 17 [13–23] | 17 [13–22] | 17 [13–21] | 28 [20–36] | 20 [13–27] | 0.002 |
| RBCx10^12/l | 4.72 [4.36–5.00] | 4.70 [4.34–5.01] | 4.60 [4.32–4.90] | 4.91 [4.58–5.26] | 4.73 [4.38–4.97] | 0.127 |
| Haematocrit, L/L | 41 [39–44] | 42 [39–44] | 41 [39–44] | 41 [39–44] | 41 [40–43] | 0.936 |
| Haemoglobin, g/dL | 13.6 [12.8–14.4] | 13.6 [12.8–14.4] | 13.5 [12.7–14.2] | 13.5 [13.0–14.1] | 13.6 [13.0–14.1] | 0.930 |
| MCV, fl | 89 [85–93] | 89 [85–93] | 89 [86–94] | 84 [79–88] | 90 [85–92] | 0.019 |
| MCH, pg | 29 [28–30] | 29 [28–31] | 29 [28–31] | 28 [26–29] | 30 [29–30] | 0.024 |
| MCHC, g/dL | 33 [32–33] | 33 [32–33] | 33 [32–33] | 33 [32–33] | 33 [32–33] | 0.644 |
| RDW, % | 14.1 [13.4–14.8] | 14.0 [13.5–14.8] | 14.1 [13.3–14.8] | 14.8 [14.0–15.3] | 13.6 [13.0–13.8] | 0.022 |
| WCC x10^9/l | 7.45 [6.30–9.30] | 7.30 [6.10–9.30] | 7.70 [6.50–9.10] | 7.55 [6.87–9.05] | 7.90 [7.50–10.70] | 0.490 |
| Lymphocytes, x10^9/l | 2.20 [1.80–2.63] | 2.20 [1.80–2.65] | 2.20 [1.80–2.60] | 2.30 [1.85–2.87] | 2.30 [1.90–2.50] | 0.772 |
| Lymphocytes % | 29.7 [23.6–35.9] | 30.0 [23.3–36.5] | 28.8 [24.6–34.9] | 31.9 [25.0–36.0] | 27.4 [21.1–32.7] | 0.695 |
| Monocytes, x10^9/l | 0.50 [0.40–0.60] | 0.50 [0.40–0.60] | 0.40 [0.33–0.50] | 0.40 [0.33–0.50] | 0.50 [0.40–0.55] | 0.151 |
| Monocytes % | 6.0 [5.1–7.4] | 6.4 [5.4–7.7] | 5.4 [4.9–6.5] | 5.1 [4.4–5.9] | 6.0 [5.1–6.9] | 0.001 |
| Neutrophils, x10^9/l | 4.60 [3.60–5.80] | 4.30 [3.30–5.67] | 4.80 [3.82–6.12] | 4.90 [4.00–5.67] | 4.90 [4.00–5.67] | 0.257 |
| Neutrophils % | 60.5 [54.7–66.6] | 59.8 [52.9–66.4] | 63.1 [56.2–66.5] | 59.4 [56.0–67.5] | 62.7 [60.0–71.4] | 0.189 |
| Basophils, x10^9/l | 0.01 [0.01–0.02] | 0.01 [0.01–0.01] | 0.01 [0.01–0.01] | 0.01 [0.01–0.01] | 0.01 [0.01–0.04] | 0.356 |
| Basophils % | 0.4 [0.3–0.6] | 0.5 [0.3–0.6] | 0.4 [0.3–0.5] | 0.4 [0.3–0.5] | 0.3 [0.3–0.7] | 0.224 |
| Eosinophils, x10^9/l | 0.13 [0.10–0.20] | 0.19 [0.10–0.30] | 0.10 [0.10–0.20] | 0.14 [0.10–0.20] | 0.10 [0.10–0.20] | 0.096 |
| Eosinophil % | 1.0 [1.1–3.1] | 2.2 [1.4–3.4] | 1.7 [1.0–2.4] | 2.0 [1.1–2.5] | 1.1 [0.8–2.2] | 0.023 |
| Platelets, x10^9/l | 270.0 [225.0–315.5] | 271.0 [226.0–318.2] | 278.0 [237.7–322.5] | 251.0 [236.2–288.7] | 2230 [200.0–318.0] | 0.527 |
γGT, γ-Glutamyltransferase; ALT, Alanine aminotransferase; AST, Aspartate transaminase; BMI, Body mass index; BP, blood pressure; FBG, Fasting blood glucose; Hip-C, Hip circumference; MCH, mean cell haemoglobin; MCHC, mean corpuscular haemoglobin concentration; HDL-C, High density lipoprotein cholesterol; LDL-C, Low density lipoprotein cholesterol; MCV, mean cell volume; RBC, Red cell count; RDW, Red cell distribution width; RMR, Resting metabolic rate; TC, Total cholesterol U-CRP, ultra-sensitive C-reactive protein; Waist-C, Waist circumference; WCC, White cell count.
Biological profile
The median percentage of visceral fat in the overall sample was 10% and ranged from 9% in normo-tolerant individuals to 12.5% in screen-detected diabetes (p = 0.0008). Similarly the median percentage of body fat was 42.2% and ranged from 41.2% in the normo-tolerant group to 49.4% in participants with screen-detected diabetes (p = 0.044). Median resting metabolic rates were similar across all glucose tolerance groups (p = 0.146). The mean values (SD) for other biochemical measurements were 6.0% (1.2) for HbA1c, 5.5 (2.2) mmol/l for fasting glucose, 5.3 (1.1) mmol/l for total cholesterol, 1.3 (0.3) mmol/l for HDL cholesterol, and 3.3 (1.0) for measured LDL cholesterol. A median value of 7.6 U/l and 1.2 mmol/l was obtained for fasting insulin and triglycerides respectively and as expected there was a significant difference across the various glucose tolerance statuses (all p < 0.027), (Table 1). Median U-CRP, GGT and ALT also varied between the different groups (all p < 0.023), while values for cotinine and AST did not (both p > 0.191).
Haematological profile
The full blood count parameters across all groups of participants were within the normal range. The median white cell count was 7.45 × 109/l and the platelet count was 270 × 109/l. The distribution of white cells was similar across all groups however the percentage of monocytes was lowest among screen-detected diabetics (p = 0.001). Although average haemoglobin, haematocrit and red cell measurements were within normal ranges, differences in the distribution across glucose tolerance statuses were apparent for mean cell volume (p = 0.019) mostly driven by high values in the known diabetics group (p = 0.019).
Activation antigen expression on circulating monocytes and neutrophils
The median percentage of monocytes and neutrophils expressing the activation antigen CD69 was significantly different across glucose tolerance groups, being higher in known diabetics (26.2%), followed by the prediabetic group (16.9%), then screen detected diabetes (10.6%) and normo-tolerant (14.1%) (p = <0.016). An equivalent pattern was observed for neutrophils (p = 0.002) and the percentage of monocytes expressing CD142 (tissue factor), (p = 0.009). The percentage of neutrophils expressing tissue factor was similar across all groups of participants (p = 0.903), and there was no significant difference in the mean fluorescent intensity (MFI) of expression for any of the measured antigens across all glucose tolerance groups (Table 2).
Table 2. Activation antigen expression according to glucose tolerance status.
| Variables | Overall | Normoglycemia | Pre-diabetes | Screen-detected Diabetes | Known Diabetes | p-value |
|---|---|---|---|---|---|---|
| Markers of Monocyte activation | ||||||
| %CD69 expression | 14.7 [5.99–27.8] | 14.1 [5.0–25.1] | 16.9 [7.2–38.6] | 10.6 [6.9–14.8] | 26.2 [14.2–37.8] | 0.016 |
| CD69 MFI | 2.9 [2.4–3.8] | 2.9 [2.3–3.7] | 3.2 [2.5–4.8] | 2.8 [1.8–3.7] | 2.9 [2.6–3.5] | 0.240 |
| %CD42b expression | 36.9 [17.8–52.9] | 35.7 [18.8–49.5] | 44.6 [18.7–61.7] | 17.6 [11.7–43.6] | 65.1 [37.2–76.2] | 0.004 |
| CD42 MFI | 5.7 [4.3–7.6] | 5.6 [4.3–7.6] | 6.0 [4.6–7.6] | 5.7 [4.3–8.7] | 6.1 [4.6–7.3] | 0.980 |
| %CD142 expression | 5.9 [2.9–12.3] | 5.5 [2.5–10.4] | 7.2 [4.5–17.1] | 3.5 [2.2–7.7] | 12.0 [5.2–17.1] | 0.009 |
| CD142 MFI | 2.4 [2.1–4.4] | 2.3 [2.1–4.3] | 2.7 [2.1–5.0] | 3.1 [2.0–7.1] | 2.3 [2.1–2.4] | 0.713 |
| Markers of Neutrophil activation | ||||||
| %CD69 expression | 5.5 [2.1–14.1] | 5.0 [1.9–12.0] | 7.6 [2.8–14.6] | 2.1 [1.2–6.4] | 20.8 [10.1–24.0] | 0.002 |
| CD69 MFI | 2.7 [2.3–3.3] | 2.7 [2.2–3.4] | 2.7 [2.4–3.2] | 2.7 [2.2–3.7] | 2.4 [2.0–3.0] | 0.556 |
| %CD42b expression | 22.0 [6.2–38.5] | 21.5 [6.2–37.2] | 26.0 [7.5–40.8] | 8.9 [4.1–23.9] | 50.4 [23.8–53.0] | 0.003 |
| CD42b MFI | 4.5 [3.4–5.8] | 4.4 [3.4–5.5] | 5.0 [3.8–6.6] | 4.5 [3.7–5.7] | 4.3 [3.6–5.4] | 0.493 |
| %CD142 expression | 12.5 [5.7–12.5] | 5.5 [2.6–12.1] | 5.4 [3.5–15.2] | 7.4 [1.9–10.7] | 7.5 [3.7–12.2] | 0.903 |
| CD142 MFI | 3.7 [2.3–6.5] | 3.7 [2.3–6.3] | 4.2 [2.7–6.7] | 5.2 [3.6–6.5] | 2.6 [2.3–3.3] | 0.124 |
Platelet activation as measured by the percentage of monocytes and neutrophils (PMA’s and PNA’s) expressing CD42b was significantly different across glucose tolerance groups, being highest in known diabetes followed by prediabetes, and lowest in screen-detected diabetes (p = <0.003), Table 2 and Fig. 1.
Robust regression analysis
In robust linear regressions adjusted for age and gender, known diabetes was significantly and positively associated with the percentage of monocytes expressing CD69 [beta 11.06 (p-value = 0.016)], CD42b (PMAs) [19.51(0.003)], % of neutrophils expressing CD69 [14.19 (<0.0001)] and CD42b [17.7 (0.001)] Table 3. In similar robust regression models BMI was negatively associated with the percentage of monocytes expressing CD69 [beta −0.377 (p = 0.020)], CD42b [−0.441 (0.034)] and CD142 [−0.155 (0.021)]. The percentage of neutrophils expressing CD142 was also negatively associated with BMI [−0.155 (0.021)] while borderline associations were apparent with CD69 (p = 0.071) and CD42b (p = 0.056); Table 3. No significant associations were detected between markers of platelet, monocyte or neutrophil activation and gender, age, U-CRP levels and markers of glucose homeostasis.
Table 3. Regression beta coefficients (p-values) from multiple robust linear models for the prediction of markers of platelet activation and platelet leucocytes aggregates, accounting for the potential effect of sex and age, diabetes and adiposity.
| Predictors | Markers of Monocyte activation |
Markers of Neutrophil activation |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| %CD69 | CD69 MFI | %CD42 | CD42 MFI | %CD142 | CD142 MFI | %CD69 | CD69 MFI | %CD42 | CD42 MFI | %CD142 | CD142 MFI | |
| Sex (male) | 0.427 (0.876) | −0.101 (0.565) | 3.133 (0.367) | −0.304 (0.426) | −0.132 (0.903) | −0.002 (0.991) | 0.720 (0.554) | −0.140 (0.300) | 2.127 (0.547) | −0.025 (0.921) | −0.131 (0.903) | −0.663 (0.069) |
| Smoking | 2.841 (0.273) | −0.032 (0.851) | 2.736 (0.433) | 0.029 (0.936) | 1.770 (0.161) | −0.079 (0.573) | 1.499 (0.189) | 0.037 (0.782) | 2.490 (0.455) | 0.025 (0.918) | 1.770 (0.161) | −0.366 (0.379) |
| Age | 0.009 (0.917) | −0.009 (0.102) | 0.110 (0.329) | −0.009 (0.471) | 0.057 (0.102) | 0.003 (0.546) | −0.007 (0.951) | 0.001 (0.749) | 0.079 (0.489) | 0.006 (0.434) | 0.057 (0.102) | −0.019 (0.112) |
| BMI | −0.377 (0.020) | −0.001 (0.947) | −0.441 (0.034) | −0.025 (0.288) | −0.155 (0.021) | 0.003 (0.704) | −0.171 (0.071) | −0.006 (0.472) | −0.375 (0.056) | −0.007 (0.689) | −0.155 (0.021) | 0.031 (0.292) |
| U-CRP | 0.086 (0.207) | 0.003 (0.609) | 0.071 (0.400) | 0.006 (0.512) | −0.008 (0.842) | −0.005 (0.217) | 0.024 (0.532) | <−0.0001 (0.994) | −0.018 (0.800) | −0.003 (0.802) | −0.008 (0.842) | 0.015 (0.130) |
| Glucose tolerance status | ||||||||||||
| Normotolerent | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Prediabetes | 4.115 (0.169) | 0.460 (0.034) | 4.312 (0.300) | 0.594 (0.228) | 1.203 (0.372) | 0.112 (0.530) | 1.513 (0.279) | 0.146 (0.386) | 2.153 (0.529) | 0.470 (0.141) | 1.203 (0.372) | 0.254 (0.580) |
| New Diabetes | −5.884 (0.157) | −0.023 (0.926) | −10.450 (0.066) | 0.400 (0.557) | −1.902 (0.289) | 0.140 (0.584) | −2.178 (0.248) | −0.231 (0.355) | −8.412 (0.069) | 0.133 (0.754) | −1.902 (0.289) | 1.405 (0.019) |
| Known diabetes | 11.061 (0.016) | 0.165 (0.605) | 19.513 (0.003) | 0.266 (0.717) | 3.121 (0.138) | −0.089 (0.726) | 14.195 (<0.0001) | −0.087 (0.721) | 17.697 (0.001) | 0.169 (0.725) | 3.121 (0.138) | −0.758 (0.259) |
| HbA1c | 0.431 (0.784) | 0.033 (0.683) | 0.602 (0.758) | 0.089 (0.688) | −0.119 (0.793) | 0.016 (0.779) | −0.055 (0.927) | −0.007 (0.924) | 0.050 (0.971) | 0.095 (0.339) | −0.119 (0.793) | 0.052 (0.766) |
| FBG | 0.685 (0.275) | 0.036 (0.300) | 1.353 (0.065) | 0.080 (0.273) | 0.108 (0.645) | −0.001 (0.986) | 0.541 (0.067) | −0.012 (0.659) | 0.952 (0.127) | 0.054 (0.288) | 0.109 (0.645) | −0.052 (0.578) |
| Fasting insulin | −0.011 (0.964) | −0.004 (0.251) | −0.122 (0.714) | −0.004 (0.596) | −0.031 (0.176) | −0.0001 (0.996) | −0.030 (0.741) | −0.003 (0.347) | −0.089 (0.604) | −0.0004 (0.990) | −0.031 (0.176) | −0.002 (0.969) |
For regression using glucose tolerance status as predictor, the subgroup of participants with normal glucose tolerance (normotolerant) served as reference group for all comparisons. This means beta coefficients for other glucose tolerance subgroups represents the absolute change in the level of each marker of interest, from the mean level in the subgroup of participants with normal glucose tolerance.
Discussion
Findings from the current study showed a differential distribution of levels of monocyte/neutrophil activation and platelet leucocyte aggregates by glucose tolerance status, mostly driven by high levels in participants with known diabetes, and to some extent low levels in those with screen-detected diabetes. These findings were further confirmed in robust regressions, whereby, known diabetes was significantly and positively associated with the percentage of monocytes or neutrophils expressing CD69 or CD142.
Although no association between U-CRP and the activation of platelets, monocytes or neutrophils could be detected in this study, elevated percentages of pro-inflammatory monocytes and neutrophils expressing both tissue factor (TF) and CD69 were observed in known diabetic participants. The alteration of activation antigens on cells of the innate immune system in type 2 diabetics has been previously described26,27,28 while others have reported that the activation of these cells together with the pro-inflammatory environment are linked to the progression of the disease and the onset of complications such as cardiovascular diseases29,30.
Tissue factor (CD142), which was increased on the surface of monocytes in this study, plays an important role in linking the process of inflammation with a pro-thrombotic environment. CD142 initiates the extrinsic pathway of coagulation by activating Factor VII and plays a role in stimulating the activation of platelets and leucocytes and the release of pro-inflammatory cytokines29,31. The expression of TF in type 2 diabetes however remains controversial. A study by Vambergue et al., reported no changes to monocyte tissue factor activity in T2D patients when compared to healthy individuals32. Notably however, this study was performed on a cohort of T2D patients who were not obese and in addition, the authors used an enzyme linked immunosorbent assay to measure soluble TF rather than cell surface expression32. The differing methodologies, BMI and glycaemic index could explain why the expression of tissue factor on monocytes in diabetes remains controversial.
The ability of granulocytes to synthesise and express Tissue Factor also remains controversial33,34. Neutrophils may acquire TF via direct interactions with activated monocytes35 and therefore could be implicated in the development of cardiovascular disease. The neutrophils in our study did not have significantly increased tissue factor expression in comparison to normal but did express CD69 which implies that they are activated and do contribute to the pro-inflammatory environment.
A number of researchers have further reported that untreated diabetic patients have dysfunctional monocytes and neutrophils which have defective activation, abnormal chemotaxis, phagocytosis and killing ability. Of note many of these functions are restored after treatment with glucose control agents36,37. Overall, although numbers are small, our results have shown that the activation status of monocytes and neutrophils were lower among the screen-detected diabetic participants and higher in the pre diabetic and known diabetic groups treated with at least metformin. This pattern could suggest that the persistently elevated levels of activation within the innate immune system eventually leads to immune exhaustion and dysfunction, a common finding in patients with newly diagnosed but untreated diabetes36,37,38. Treatment with drugs such as metformin restore immune function, however as the disease progresses the activation of monocytes and neutrophils increases leading to the formation of platelet leucocyte aggregates (PLAs) which are associated with the development of cardiovascular complications and thrombotic plaques18,19.
Platelet Monocyte Aggregates (PMA’s) are a robust measure of platelet activation and are also an indicator of vascular damage13. In agreement with our findings, several studies however, have failed to show an association between elevated PMAs and markers of glucose control19,39. Platelet leucocyte aggregates while increased in the prediabetic and known diabetic groups were lower in patients who had been newly diagnosed. This phenomenon seems to support the theory that the activation of platelets is not linked to glucose metabolism but rather the progression of the disease and the onset of vascular complications19,40. This theory remains controversial however, and a study by Patkό et al., reported a direct association between elevated levels of PMAs and fasting plasma glucose levels. Of note this was a small cohort of 14 T2D patients with no clinical signs of inflammation15. This could imply that the increased circulating levels of PMAs involve multifactorial mechanisms that act in synergy at a cellular level. These could be associated with both monocyte and platelet activation which initiate a cascade of signalling events which drive the formation of PMAs.
This was a cross-sectional study with no objective assessment of the presence of vascular complications to possibly explain some of our correlations. Longitudinal studies are therefore needed to probe the underlying mechanisms involving PMAs and increased monocyte-neutrophil interactions in T2D. There were an unequal number of participants across our glucose tolerance subgroups, and it is likely that the small number in some subgroups might have affected our capacity to uncover and characterise some of the associations.
The strengths of our study include the efforts to ensure reproducibility and standardization of flow cytometry based PLA measurement by following the guidelines recommended by the British International Committee of Haematology24. Artefactual platelet activation was avoided by minimising the time between sample collection and data acquisition, the omission of washing steps, mechanical stimulation due to centrifugation and the avoidance of buffers containing magnesium chloride and calcium chloride. In addition bias was avoided by only revealing the glycaemic status of the participants after the results had been processed and analysed.
In conclusion, this study has demonstrated increased levels of activated monocytes, neutrophils and platelets in patients with known diabetes which are not associated with markers of glucose metabolism. Platelet leucocyte aggregate formation increases as cardiovascular complications develop and therefore the monitoring of leucocyte activation and platelet leukocyte aggregates in type 2 diabetes may be crucial in the management and risk stratification of patients at risk of developing thrombotic complications.
Additional Information
How to cite this article: Davison, G. M. et al. Platelet, monocyte and neutrophil activation and glucose tolerance in South African Mixed Ancestry individuals. Sci. Rep. 7, 40329; doi: 10.1038/srep40329 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Acknowledgments
We thank the Bellville South (Ward 009) community for participating in the study. We are also grateful to the Bellville South community Health Forum for supporting the engagement with the Bellville South community. This research project was funded by the South African Medical Research Council (MRC) with funds from National Treasury under its Economic Competitiveness and Support Package (MRC-RFA-UFSP-01-2013/VMH Study). Any opinion, finding and conclusion or recommendation expressed in this material is that of the author(s) and the MRC does not accept any liability in this regard.
Footnotes
Author Contributions G.M.D.: substantial contributions to conception and design, interpretation of data; drafting the article, final approval of the version to be published; B.B.N.: provided technical supervision, analysed results and final approval of the version to be published; Z.M.: performed experiments, analysed data and final approval of the version to be published; G.M.H.: statistical analysis, editorial input and final approval of the version to be published; A.P.K.: statistical analysis and interpretation, revising it critically for important intellectual content; final approval of the version to be published; R.T.E.: revising it critically for important intellectual content; final approval of the version to be published; T.E.M.: substantial contributions to conception and design, acquisition of data, analysis and interpretation of data; drafting the article, final approval of the version to be published.
References
- Grundy S. M. Prevention Conference VI: Diabetes and Cardiovascular Disease: Executive Summary: Conference Proceeding for Healthcare Professionals From a Special Writing Group of the American Heart Association. Circulation; 105, 2231–2239 (2002). [DOI] [PubMed]
- Sudic D. et al. High glucose levels enhance platelet activation: involvement of multiple mechanisms. Br J Haematol 133, 315–322 (2006). [DOI] [PubMed] [Google Scholar]
- Keating F. K., Sobel B. E. & Schneider D. J. Effects of increased concentrations of glucose on platelet reactivity in healthy subjects and in patients with and without diabetes mellitus. Am J Cardiol 92, 1362–1365 (2003). [DOI] [PubMed] [Google Scholar]
- Assert R. et al. Regulation of protein kinase C by short term hyperglycaemia in human platelets in vivo and in vitro. Diabetologia 44(2), 188–195 (2001). [DOI] [PubMed] [Google Scholar]
- Ferreira I. L. et al. Platelet inhibition by insulin is absent in type 2 diabetes mellitus. Arterioscler. Thromb. Vasc. Biol. 26, 417–422 (2006). [DOI] [PubMed] [Google Scholar]
- Fontana P. et al. P2Y12 H2 haplotype is a associated with peripheral arterial disease A case-control study. Circulation 108(24), 2971–2973 (2003). [DOI] [PubMed] [Google Scholar]
- Kornerup K. N., Salmon G. P., Pitchford S. C., Liu W. L. & Page C. P. Circulating platelet-neutrophil complexes are important for subsequent neutrophil activation and migration. J Appl Physiol 109(3), 758–767 (2010). [DOI] [PubMed] [Google Scholar]
- Rondina M. T., Weyrich A. S. & Zimmerman G. A. Platelets as cellular effectors of inflammation in vascular diseases. Circ Res 112, 1506–1519 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon C. et al. Platelet ADP receptors contribute to the initiation of intravascular coagulation. Blood 103(2), 594–600 (2004). [DOI] [PubMed] [Google Scholar]
- Levi M. & van der Poll T. Two-way interactions between inflammation and coagulation. Trends Cardiovasc Med 15, 254–259 (2005). [DOI] [PubMed] [Google Scholar]
- Ahn K. C. et al. Preferential binding of platelets to monocytes over neutrophils under flow. Biochem Biophys Res Commun 329(1), 345–355 (2005). [DOI] [PubMed] [Google Scholar]
- Arber N. et al. The State of leucocyte adhesiveness/aggregation in the peripheral blood: a new and independent marker of mental stress. Stress Med 7(2), 75–78 (1991). [Google Scholar]
- Michelson A. D., Barnard M. R., Krueger L. A., Valeri C. R. & Furman M. I. Circulating monocyte-platelet aggregates are a more sensitive marker of in vivo platelet activation than platelet surface P-selectin studies in baboons, human coronary intervention, and human acute myocardial infarction. Circulation 104(13), 1533–1537 (2001). [DOI] [PubMed] [Google Scholar]
- Pearson L. et al. A rapid flow cytometric technique for the detection of platelet-monocyte complexes, activated platelets and platelet-derived microparticles. Int J Lab Hematol 31, 430–439 (2009). [DOI] [PubMed] [Google Scholar]
- Patkó Z. 1. et al. Elevation of monocyte-platelet aggregates is an early marker of type 2 diabetes. Interv Med Appl Sci 4, 181–185 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Théorêt J. F. et al. P-selectin ligation induces platelet activation and enhances microaggregate and thrombus formation. Throm Res 128, 243–250 (2011). [DOI] [PubMed] [Google Scholar]
- Ramasamy R., Yan S. F. & Schmidt A. M. Receptor for AGE (RAGE): Signaling mechanisms in the pathogenesis of diabetes and its complications. Ann N Y Acad Sci 1243, 88–102 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elalamy I. et al. Circulating platelet – leukocyte aggregates: A marker of microvascular injury in diabetic patients. Throm Res 121(6), 843–848 (2008). [DOI] [PubMed] [Google Scholar]
- Shlomai G. et al. High-risk type-2 diabetus mellitus patients, without prior ischaemic events, have normal blood platelet functionality profiles: a cross sectional study. Cardiovasc Diabetol 14, 80 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erasmus R. T. et al. High prevalence of diabetes mellitus and metabolic syndrome in a South African coloured population: baseline data of a study in Bellville, Cape Town. S Afr Med J 102, 841–844 (2012). [DOI] [PubMed] [Google Scholar]
- Chalmers J. et al. and the Guidelines Subcommittee of the World Health Organization. 1999 World Health Organization-International Society of Hypertension guidelines for the management of hypertension. Clin Exp Hypertens 21, 1009–1060 (1999). [DOI] [PubMed] [Google Scholar]
- Alberti K. G. & Zimmet P. Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15, 539–553 (1998). [DOI] [PubMed] [Google Scholar]
- Benowitz N. L., Bernert J. T., Caraballo R. S., Holiday D. B. & Wang J. Optimal serum cotinine levels for distinguishing cigarette smokers and nonsmokers within different racial/ethnic groups in the United States between 1999 and 2004. Am J Epidemiol 169, 236–248 (2009). [DOI] [PubMed] [Google Scholar]
- Harrison P. et al. Guidelines for the laboratory investigation of heritable disorders of platelet function. Br J Haematol 155, 30–44 (2011). [DOI] [PubMed] [Google Scholar]
- Nkambule B. B., Davison G. & Ipp H. Platelet leukocyte aggregates and markers of platelet aggregation, immune activation and disease progression in HIV infected treatment naive asymptomatic individuals. J Thromb Thrombolysis 40, 458–467 (2015). [DOI] [PubMed] [Google Scholar]
- Giuletti A. et al. Monocytes from type 2 diabetic patients have a pro-inflammatory profile 1,25-Dihydroxyvitamin D3 works as anti-inflammatory. Diabetes Res Clin Pract 77(1), 47–57 (2007). [DOI] [PubMed] [Google Scholar]
- Sampson M. J., Davies I. R., Brown J. C., Ivory K. & Hughes D. A. Monocyte and neutrophil adhesion molecule expression during acute hyperglycemia and after antioxidant treatment in type 2 diabetes and control patients. Arterioscler Thromb Vasc Biol 22, 1187–1193 (2002). [DOI] [PubMed] [Google Scholar]
- van Oostrom A. J., van Wijk J. P., Sijmonsma T. P., Rabelink T. J. & Castro Cabezas M. Increased expression of activation markers on monocytes and neutrophils in type 2 diabetes. Neth J Med 62, 320–325 (2004). [PubMed] [Google Scholar]
- Steffel J., Luscher T. & Tanner F. C. Tissue factor in cardiovascular diseases: Molecular mechanisms and clinical implications. Circulation 113, 722–731 (2006). [DOI] [PubMed] [Google Scholar]
- Mazzone A. et al. Increased expression of neutrophil and monocyte adhesion molecules in unstable coronary artery disease. Circulation 88(2), 358–363 (1993). [DOI] [PubMed] [Google Scholar]
- Yang M. et al. The role of mononuclear cell tissue factor and inflammatory cytokines in patients with chronic thromboembolic pulmonary hypertension. J Throm Thrombolysis 42(1), 38–45 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vambergue A. et al. Factor VII, tissue factor pathway inhibitor, and monocyte tissue factor in diabetes mellitus: influence of type of diabetes, obesity index, and age. Thromb Res 101(5), 367–375 (2001). [DOI] [PubMed] [Google Scholar]
- Sambola A. et al. Role of risk factors in the modulation of tissue factor activity and blood thrombogenicity. Circulation. Am Heart Assoc 107(7), 973–7 (2003). [DOI] [PubMed] [Google Scholar]
- Maugeri N. et al. Human polymorphonuclear leukocytes produce and express functional tissue factor upon stimulation1. J Thromb Haemost 4(6), 1323–1330 (2006). [DOI] [PubMed] [Google Scholar]
- Sovershaev M. A. et al. No evidence for the presence of tissue factor in high-purity preparations of immunologically isolated eosinophils. J Thromb Haemost 6(10), 1742–1749 (2008). [DOI] [PubMed] [Google Scholar]
- Egorina E. M., Sovershaev M. A., Olsen J. O. & Østerud B. Granulocytes do not express but acquire monocyte-derived tissue factor in whole blood: evidence for a direct transfer. Blood 111(3), 1208–1216 (2008). [DOI] [PubMed] [Google Scholar]
- Lecube A., Pachón G., Petriz J., Hernández C. & Simó R. Phagocytic activity is impaired in type 2 diabetes mellitus and increases after metabolic improvement. PLos One. 6(8), e23366 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geerlings S. E. & Hoepelman A. I. M. Immune dysfunction in patients with diabetes mellitus (DM). FEMS Immunol Med Microbiol 26, 259–265 (1999). [DOI] [PubMed] [Google Scholar]
- Treweeke A. T. et al. N-Acetylcysteine inhibits platelet–monocyte conjugation in patients with type 2 diabetes with depleted intraplatelet glutathione: a randomised controlled trial. Diabetologia 55(11), 2920–2928 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmalbach B. et al. Determinants of platelet-leukocyte aggregation and platelet activation in stroke. Cerebrovasc Dis 39(3–4), 176–180 (2015). [DOI] [PubMed] [Google Scholar]