Abstract
Mucopolysaccharidosis I and II are lysosomal storage disorders that, despite treatment with hematopoietic cell transplantation (HCT) and/or enzyme replacement therapy (ERT), continue to cause significant skeletal abnormalities leading to pain, stiffness, physical dysfunction, and short stature. Tumor necrosis factor – alpha (TNF-α) is elevated in individuals with MPS I and II and associated with pain and physical dysfunction. Therefore, we evaluated the safety and effects of the TNF-α inhibitor adalimumab in patients with MPS I and II in a 32-week, randomized, double blind, placebo-controlled, crossover study of adalimumab at a dose of 20 mg (weight 15–<30 kg) or 40 mg (weight ≥ 30 kg) administered subcutaneously every other week or saline placebo for 16 weeks. Participants were evaluated at baseline, week 16, and week 32 with the Children's Health Questionnaire – Parent Form 50 (CHQ-PF50), the Pediatric Pain Questionnaire (PPQ), range-of-motion (ROM) measurements, anthropometry, six-minute walk test (6MWT), hand dynamometer, and laboratory evaluations for safety. The primary outcome was safety and primary efficacy outcome was bodily pain (BP) measured by the CHQ-PF50. Two subjects, one with MPS I and one with MPS II, completed the study. Adalimumab was well tolerated and there were no serious adverse events. Standardized BP scores for age and gender were higher (i.e. less pain) at the end of the treatment versus placebo phase for both subjects. Subject #1 became unblinded during treatment due to skin erythema. Behavior measured by both CHQ-PF50 and parental report improved during treatment compared to placebo in both subjects. ROM improved by > 5° in seven of eight joints in Subject #1 and five of eight joints in Subject #2 (range 7.0° to 52.8°). There was no change in the PPQ, 6MWT, or hand dynamometer. Data from this small pilot study suggest that treatment with adalimumab is safe, tolerable, and may improve ROM, physical function, and possibly pain, in children with MPS I or II. However, additional clinical trials are needed before this therapy should be recommended as part of clinical care.
Keywords: Mucopolysaccharidosis, Inflammation, Joint, Bone
1. Introduction
The mucopolysaccharidoses (MPS) are a group of lysosomal storage diseases resulting from specific lysosomal enzyme deficiencies that result in lysosomal accumulation of glycosaminoglycans (GAG) in most body tissues. Despite treatment with hematopoietic cell transplantation (HCT) and/or enzyme replacement therapy (ERT), individuals with MPS I or II continue to have significant skeletal abnormalities (i.e., kyphosis, scoliosis, genu valgum), joint contractures, stiffness, pain, and severe short stature [1], [2], [3], [4], [5], [6].
GAG deposition has been identified in bone and cartilage in humans and animal models of MPS [7], [8], [9], [10], [11], [12], [13], [14], [15]. This deposition in cartilage induces inflammation, chondrocyte apoptosis, and hyperplasia of the synovial membranes of MPS animals [12], [14], and is similar to joint changes in juvenile idiopathic arthritis (JIA), rheumatoid arthritis (RA), and ankylosing spondylitis (AS) [12], [13], [14], [15], [16]. In animal models of MPS, GAG continues to accumulate despite treatment with ERT, and accumulated GAG activates toll-like receptor-4 (TLR-4), similar to lipopolysaccharide (LPS), in synovial chondrocytes and monocyte/macrophages [13], [14], [17]. TLR-4 activation increases expression and secretion of TNF- α, interleukin - 1β (IL-1β), and receptor activator of nuclear factor kappa-B ligand (RANKL) resulting in local inflammatory joint disease and systemic inflammation [12], [13], [17], [18]. Matrix-degrading metalloproteinases (MMP-1, -2, -9, and -13) are also elevated in the MPS I and VI animals, and likely contribute to the degradation of articular cartilage [16], [17]. Finally, localized increased bone resorption in bone surrounding knee joints of MPS I mice [16], and proteoglycan loss in joints of MPS IX animals [19] has been reported.
MPS animal models show improvement in joint disease and mobility after treatment with TNF-α inhibition [13], [15]. Presymptomatic MPS VI rats treated with a rat specific TNF- α inhibitor in addition to ERT (recombinant human N-acetylgalactosamine-4-sulfatase) developed significantly less synovial villi (marker of joint inflammation that is seen in rheumatoid arthritis), a greater improvement in performance on rotarod testing at higher speeds (20 and 30 RPM), and a trend toward increased femora (6% longer) and tibia (14% longer) lengths, compared to animals treated with ERT alone [15]. In another study of 6-month-old MPS VI rats with advanced bone disease and 1-month-old presymptomatic MPS VI rats treated with the TNF- α inhibitor infliximab, TNF- α and RANKL levels decreased to levels similar to normal rats within 4–8 weeks post-injection, and in the 6-month-old MPS VI rats with advanced bone disease, the percent of apoptotic cells in articular cartilage measured by TUNEL staining decreased significantly from that seen in untreated animals and was no different than in normal animals [16].
Furthermore, children and adolescents with MPS have elevated plasma levels of TNF-α and high levels of TNF-α directly correlate with their severity of pain and decreased physical function [20]. This is not surprising as TNF-α has a myriad of well-described local and systemic effects. For example, TNF-α 1) incites further inflammation through activation of monocytes to inflammatory macrophages that produce other cytokines such as IL-1β and RANKL, 2) recruits neutrophils and other phagocytes, 3) causes cellular apoptosis, and 4) increases endothelial permeability, all of which drive further inflammation. In addition, TNF-α is involved in the release of prostanoids such as prostaglandin E2 that cause systemic pain (i.e. myalgia). This cascade of events causes collateral tissue damage and joint abnormalities, systemic inflammation, and pain as is characteristic of rheumatologic joint diseases [21], [22] and MPS.
In summary, 1) animal models of MPS have revealed joint abnormalities similar to those seen in inflammatory joint disease and improvement in inflammation, joint pathology, and physical function when treated with TNF- α inhibition, and 2) individuals with MPS have high levels of plasma TNF-α that are associated with pain and physical disability despite current therapies. Therefore, we conducted a pilot study to collect data on the safety, tolerability and effect of adalimumab (AbbVie) on pain and physical function in individuals with MPS I or II. Secondary objectives included evaluating the effects of adalimumab on ROM, growth, endurance (6MWT), and muscle strength (handgrip dynamometer).
2. Methods
2.1. Patients and screening
Inclusion criteria were age ≥ 5 years of age, diagnosis of MPS I or II (genetic testing or enzyme activity plus elevated urine GAG), treatment with ERT for ≥ 1 year or no ERT for ≥ 1 year, weight ≥ 15 kg, bodily pain reported by the CHQ-PF50 or SF-36 > 1 SD below the general population mean (i.e. more pain), and ≥ 3 joints with limitations in ROM. Exclusion criteria were history of HCT < 2 years prior to enrollment, immune suppression therapy < 1 year prior to enrollment, active graft versus host disease, current diagnosis or history of lymphoma or other malignancy, current active infection, history of serious opportunistic infection, positive M. tuberculosis (TB) skin test, positive chest X-ray, or a recent exposure to TB, congestive heart failure defined by an ejection fraction < 50% measured by ECHO, demyelinating disorders (e.g., central nervous system [CNS] disorders including multiple sclerosis and optic neuritis and peripheral nervous system disorders including Guillain-Barre syndrome), hematologic abnormalities (e.g., pancytopenia, aplastic anemia), hepatitis B infection (active or chronic carrier), latex sensitivity, pregnancy or breastfeeding, known or suspected allergy to adalimumab or related products, participation in simultaneous therapeutic study that involved an investigational study drug or agent within 4 weeks of study enrollment, and requirement for live vaccine exposure that would be expected to occur during the time frame of the study.
Informed consent was obtained from all parents/guardians of the subjects and assent from subjects cognitively able to provide assent. The Los Angeles Biomedical Research Institute John F. Wolf, M.D. Human Subjects Committee approved the protocol.
2.2. Design
This was a randomized, double blind, placebo-controlled, 32-week, crossover pilot study of adalimumab in subjects with MPS I or II treated with ERT and/or HCT. Subjects were randomized 1:1 in a permuted block fashion with potential block sizes of 2. Subjects were treated with adalimumab or placebo for 16 weeks (i.e., 8 doses) then crossed over to the other group for 16 weeks. Subjects were treated with adalimumab (20 mg [weight 15–<30 kg] or 40 mg [weight ≥ 30 kg]) or saline placebo administered subcutaneously every other week for 16 weeks, then crossed-over to the other group for 16 weeks. The placebo was similar to the active treatment in appearance.
At the screening visit the patient's symptoms, medical history, demographic and clinical characteristics were recorded, eligibility was confirmed, and eligible patients randomized as described above. Parents were given a diary and were asked to record date of injections, symptoms, any other pain or anti-inflammatory medications, and adverse events.
Measurements of pain, physical function, and anthropometry were measured at baseline (day 0), weeks 16 and 32. The baseline visit occurred on the same day as the screening visit. Pain was measured by the Children's Health Questionnaire – Parent Form 50 (CHQ-PF50) and the Pediatric Pain Questionnaire (PPQ). The CHQ-PF50 Bodily Pain (BP) Score evaluates parent-report of both severity and frequency of their child's bodily pain over the past 4 weeks, and the PPQ includes a parent- and a patient-reported visual analogue scale consisting of two 100 mm horizontal lines that measure both present pain and pain in the past week. Physical function was measured by the CHQ-PF50 Physical Function (PF) Score and Physical Summary (PhS) Score, ROM, 6-minute walk test (6MWT), and hand-grip dynamometer. The CHQ-PF50 evaluates parent-report of limitations in their child's physical function in activities such as play, getting around school, climbing stairs, and taking care of activities of daily living (e.g. eating, dressing, bathing, going to the toilet). Additional quality of life and behavioral outcomes were measured by CHQ-PF50. ROM was measured by the same two individuals at each visit. ROM sites (shoulder flexion, elbow extension, knee extension, and hip extension) were chosen based on common areas of MPS related disease. Anthropometric measurements (standing height, sitting height, and arm span) were measured three times and the average taken. Urine GAG was measured by Spectrophotometry (Mayo Medical Laboratories; Rochester, MN) a baseline, weeks 16 and 32. Safety was assessed with physician obtained history and physical examination and laboratory evaluations (complete blood count [CBC], liver function tests [LFTs], and anti-double stranded DNA [anti-dsDNA] antibodies) at baseline, weeks 16 and 32; safety laboratory evaluations were also obtained at weeks 4, 8, 20, and 24.
2.3. Statistical analysis
Data are presented in descriptive fashion due to the small sample size of this pilot study. All analyses and graphing were performed with the use of STATA software, version 14.0.
3. Results
3.1. Study participants
Three participants enrolled in the study and two participants completed the study (see Table 1). One withdrew before randomization for reasons unrelated to the study. Two subjects underwent randomization, completed all study visits, and are included in this report. The rate of adherence to study drug was 100% as assessed according to diary entries and 100% as assessed according to the amount of returned study drug syringes.
Table 1.
Subject baseline characteristics.
| Patient no. | Sex/age (yr) | Diagnosis | ERT (y/n) | h/o HCT (y/n) | Diagnosis |
|---|---|---|---|---|---|
| 1 | M/15 | Hurler syndrome | No | Yes | Urine GAG 139.9 mg/L Leukocyte α-L-iduronidase activity 0 nmol/h/mg protein |
| 2 | M/6 | Hunter syndrome – attenuated | Yes | No | 260G > A IDS gene mutation |
M-male; ERT = enzyme replacement therapy; HCT = hematopoietic cell transplantation; GAG = glycosaminoglycans; IDS = iduronate-2-sulfatase.
3.2. Safety outcomes
Adverse events occurred in both subjects during treatment with adalimumab (100%) and during placebo (100%) (Table 2). All adverse events were classified as mild in severity and resolved spontaneously except for sinusitis and two upper respiratory infections (URIs) that required oral antibiotic therapy (all occurring during placebo). Subject #1 experienced mood lability beginning approximately 4 weeks after the last adalimumab dose that was reported by both the patient's teachers and parents. All safety laboratory evaluations were normal throughout the study except transient mild thrombocytopenia occurring in Subject #1 described in Table 5.
Table 2.
Adverse events.
| Patient no. | Event | Severity | During treatment or placebo? | Comments |
|---|---|---|---|---|
| 1 | Diarrhea | Mild | Treatment | Resolved after 2 days without intervention. |
| 1 | Thrombocytopenia | Mild | Treatment | Resolved by 2 week recheck without intervention |
| 1 | Mood lability | Mild | Placebo | Persisted until the end of the study |
| 1 | URI | Mild | Placebo | Resolved with 10 days antibiotic therapy. |
| 1 | Headache | Mild | Placebo | Resolved with ibuprofen |
| 2 | Sinusitis | Mild | Placebo | Resolved on day 3 of 10 day antibiotic therapy. |
| 2 | URI | Mild | Placebo | Resolved on day 7 of 10 day antibiotic therapy. |
| 2 | Injection site erythema | Mild | Treatment | Lasted up to 24 h with each injection |
URI = upper respiratory infection.
Table 5.
Anthropometric measures during treatment (Tx) versus placebo (PBO). > 2 cm/yr improvements are bolded.
| Outcomes | Treatment |
Placebo |
Difference Tx-PBO |
|||
|---|---|---|---|---|---|---|
| Patient no. |
Patient no. |
Patient no. |
||||
| 1 | 2 | 1 | 2 | 1 | 2 | |
| Standing height, cm/yr | 0.1 | 9.4 | − 2.7 | 4.2 | 2.8 | 5.2 |
| Arm span, cm/yr | 3.3 | 4.8 | − 7.6 | 10.4 | 10.9 | − 5.6 |
| Sitting height, cm/yr | − 0.1 | 1.0 | 0.9 | 4.5 | − 1.0 | − 3.5 |
3.3. Primary efficacy outcome - pain (CHQ-PF50, PPQ)
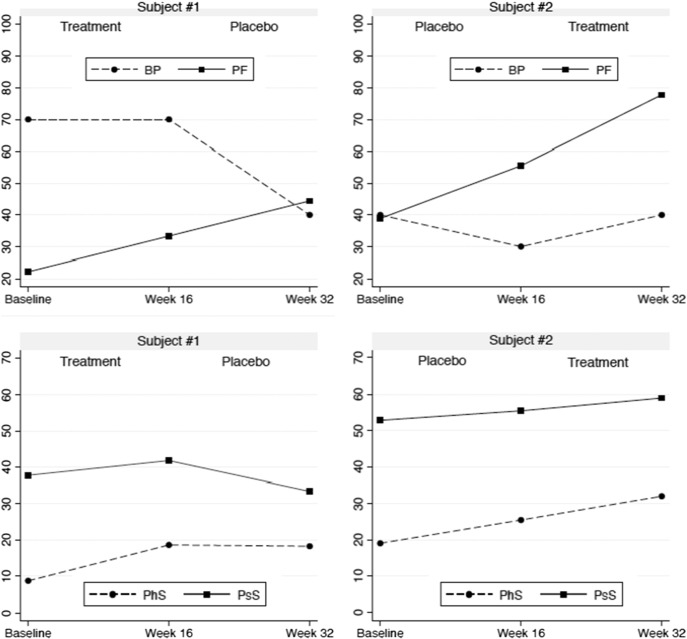
Changes of 5.0 to 10.0 points on the CHQ-PF50 are considered to be clinically meaningful [23], [24], [25]. Using this metric, both subjects had a positive response to treatment (Table 3 and Fig. 1). Although Subject #1 had no change in pain during treatment with active drug, he had a significant increase in pain (decrease in the Bodily Pain Score) when he switched to placebo (Fig. 1). Subject #2 had an increase in pain of 10 points during placebo and a decrease of 10 points during treatment (Fig. 1). Standardization of these scores for age and gender showed an improvement of + 1.4 standard deviations (SD) in Subject #1 and + 1.0 SD in Subject #2 in change of CHQ-PF50 BP scores during treatment versus placebo (Table 3). There was no significant benefit in reported pain when measured by the PPQ (data not shown).
Table 3.
Changes in CHQ-PF50 Z-scores (adjusted for age and gender) during treatment (Tx) versus placebo (PBO). > 0.5 SDS improvements are bolded.
| Outcomes | Treatment change |
Placebo change |
Difference Tx-PBO |
|||
|---|---|---|---|---|---|---|
| Patient no. |
Patient no. |
Patient no. |
||||
| 1 | 2 | 1 | 2 | 1 | 2 | |
| PhS | 1.0 | 0.7 | 0.0 | 0.6 | 1.0 | 0.1 |
| PsS | 0.4 | 0.4 | − 0.8 | 0.3 | 1.2 | 0.1 |
| GH | 0.2 | 0.2 | 0.4 | 1.1 | − 0.2 | − 0.9 |
| BP | 0.0 | 0.5 | − 1.4 | − 0.5 | 1.4 | 1.0 |
| PF | 0.7 | 1.4 | 0.7 | 1.0 | 0.0 | 0.4 |
| RP | 1.8 | 0.0 | 0.0 | 0.0 | 1.8 | 0.0 |
| PT | 1.1 | 0.0 | − 1.1 | 0.5 | 2.2 | − 0.5 |
| PE | 0.0 | 1.2 | − 0.4 | 0.8 | 0.4 | 0.4 |
| REB | 1.7 | 0.0 | − 1.7 | 0.0 | 3.4 | 0.0 |
| SE | -0.5 | 0.2 | 0.0 | 0.9 | − 0.5 | − 0.7 |
| MH | 0.7 | 0.4 | 0.0 | 0.7 | 0.7 | − 0.3 |
| BE | 0.0 | 0.5 | − 0.7 | − 1.0 | 0.7 | 1.5 |
PF = physical functioning; RP = role/social-physical; GH = general health; BP = bodily pain (lower = worse pain); PT = parental impact-time; PE = parental impact-emotional; REB = role/social-emotional/behavioral; SE = self-esteem; MH = mental health; BE = behavior; PhS = Physical Health Summary Score (PF, RP,GH, BP, PT, PE); PsS = Psychosocial Health Summary Score (PT, PE, REB, SE, MH, BE); increase means an improvement for all scales except BP (bodily pain) where increase in score = decrease in pain.
Fig. 1.
Changes in pain (BP), physical function (PF), Physical Health Summary Score (PhS), and Psychosocial Health Summary Score (PsS) measured by the CHQ-PF50, during treatment versus placebo. Increase in score means an improvement for all scales except BP where increase in score = decrease in pain.
3.4. Secondary efficacy outcomes - CHQ-PF50, physical function (ROM, 6MWT, handgrip), anthropometry, and urine GAG
Physical function, behavioral and quality-of-life outcomes measured by the CHQ-PF50 are shown in Table 4 and Fig. 1. When using a cutoff of a difference in change of > 0.5 SD, Subject #1 had a positive response during treatment compared to placebo for 8 of the 12 CHQ-PF50 outcome measures and patient #2 had a positive response in 2 of the 12 outcome measures. Improvements in bodily pain and behavior were the only two measures with improvements during treatment in both subjects. Both subjects had a worsening of standardized scores on the CHQ-PF50 for General Health (GH) and Self Esteem (SE); Subject #2 also had a worsening in Parental Impact-Time (PT) and Mental Health (MH).
Table 4.
Changes in range-of-motion (ROM) during treatment (Tx) versus placebo (PBO). > 5° improvements are bolded.
| Outcomes | Treatment change |
Placebo change |
Difference Tx-PBO |
|||
|---|---|---|---|---|---|---|
| Patient no. |
Patient no. |
Patient no. |
||||
| 1 | 2 | 1 | 2 | 1 | 2 | |
| Shoulder flexion – left, ° | − 0.5 | 20.2 | − 13.5 | 43.8 | 13.0 | − 23.6 |
| Shoulder flexion – right, ° | 10.5 | 49.2 | − 17.5 | 23.2 | 28.0 | 26.0 |
| Elbow extension – left, ° | 5.8 | 17.3 | − 2.5 | − 13.7 | 8.3 | 31.0 |
| Elbow extension – right, ° | 21.3 | 19.0 | − 10.0 | − 16.0 | 31.3 | 35.0 |
| Hip extension – left, ° | 41.3 | − 13.8 | − 11.5 | − 11.1 | 52.8 | − 2.7 |
| Hip extension – right, ° | 31.5 | 4.8 | 0.0 | − 2.2 | 31.5 | 7.0 |
| Knee extension – left, ° | 0.3 | 14.3 | − 11.5 | − 10.4 | 11.8 | 24.7 |
| Knee extension – right, ° | − 7.3 | 6.7 | 1.0 | 4.4 | − 8.3 | 2.3 |
For ROM (Table 4), Subject #1 had a positive response (defined as an improvement in ROM of > 5° during treatment compared to placebo) to adalimumab versus placebo in bilateral shoulder flexion, bilateral elbow extension, left knee extension, and bilateral hip flexion. Subject #2 had a positive response to adalimumab versus placebo in the right shoulder flexion, bilateral elbow extension, bilateral knee extension, and right hip flexion. There was no effect on 6MWT or handgrip (data not shown).
Anthropometric data are shown in Table 5. Growth velocity (annualized cm/yr change in standing height) was > 2 cm/yr higher during treatment with adalimumab versus placebo in both subjects. For Subject #1 the standing height and arm span annualized change was negative during placebo and unchanged or positive during treatment, possibly suggesting an increase in contracture during placebo versus treatment. For Subject #2 the arm span and sitting height annualized change was greater during placebo versus treatment. Possible reasons for these findings are improved arm growth and spine growth during placebo, and/or measurement error/variability.
There was no change in urine GAG during the study. Subject #1 urine GAG at baseline was 6.3 mg/mmol creatinine, 5.7 mg/mmol creatinine after 16 weeks treatment, and then 6.2 mg/mmol creatinine after 16 weeks placebo (normal for age < 6.5 mg/mmol creatinine). Subject #2 urine GAG at baseline was 17.4 mg/mmol creatinine, 16 mg/mmol creatinine after 16 weeks placebo, and then 18 mg/mmol creatinine after 16 weeks treatment (normal for age < 12 mg/mmol creatinine).
3.5. Anecdotal responses
Parents provided feedback throughout the study in a journal and by unsolicited emails; in addition, parents were queried at the completion of the study, after unblinding, for their opinions on their child's response to therapy. Quotes from parents' observations after stopping adalimumab (first quote before unblinding; second quote after unblinding):
“… behaviors have been increased the past two days. May be in pain... Behaviors are still increased. Seems to be one extreme to another… I had calls from his teacher twice last week and extreme behavior at home once this week.”
“… has stopped drawing completely because of the joint pain. He is also back to being more emotional towards the end of the day... His physical therapist also noticed that his range of motion has gotten worse… The only thing this has changed is him being off the Humira.”
4. Discussion
This study describes the use of a TNF-α inhibitor in two patients with MPS. We found that adalimumab was well tolerated and that it had beneficial clinical effects on pain, range-of-motion, behavior and growth in both participants, one with MPS type I and one with MPS type II.
TNF-α is elevated in individuals with MPS I or II [20] and contributes to pain through both driving a local inflammatory response and releasing prostanoids such as prostaglandin E2 that cause systemic pain (i.e. myalgia) [21]. We hypothesize that the benefit in pain management seen in both of our subjects was directly related to inhibition of this pathway. Of note, Subject #1 had no significant improvement in CHQ-PF50 BP score during treatment with adalimumab, which could be interpreted as no benefit from treatment, or as a benefit from treatment when comparing the BP score at the end of placebo which was lower (i.e. more pain) versus the end of treatment. Using this approach, in Subject #1 there is a treatment effect of 43% (BP standardized score at Baseline 70, Week 16 70, Week 32 40) and CHQ-BP50 BP score treatment effect in Subject #2 was 33% (BP standardized score at Baseline 40, Week 16 30, Week 32 40).
Joint stiffness persists as a significant problem for patients with MPS I and II despite treatment with ERT or HCT [26], [27], [28], [29]. One 12-month study of ERT in patients with MPS II reported changes in ROM of up to 19° [28]. In comparison, we found changes of up to 35° following treatment with adalimumab in the participant with MPS II (Subject #2), who was on ERT at study entry. For MPS I, one retrospective chart review found severe ROM deficits (defined as restriction of ≥ 90° for shoulder abduction) in five out of sixteen patients [29]. The effects of ERT on joint ROM in patients with MPS IA (attenuated MPS I; Hurler-Scheie and Scheie syndromes) have been well described [30], [31], [32]. One study found that after 2 years of treatment with laronidase, patients with MPS IA had on average improvements in shoulder flexion of 29° (range 5°–50°) [31]. We found comparable changes of 13° and 28° in the participant with MPS type IH (Subject #1), who had been previously treated with hematopoietic stem cell transplantation, over just 16 weeks of treatment with adalimumab.
Both subjects had significant worsening of behavior measured by the CHQ-PF50 Behavior Score and by parental report after discontinuation of adalimumab. It is possible that some of the difficult behaviors in children with MPS who are cognitively delayed may be related to pain. For example, for Subject #1, both his teachers and parents noticed worsening in his behavior and mood beginning approximately 4 weeks after his last dose of adalimumab and his parent reported increased pain during treatment with placebo compared to adalimumab. Worsening in pain, mood, and behavior also occurred for Subject #2 approximately 4 weeks after discontinuing adalimumab per parental report (after the conclusion of the study). Studies in patients with rheumatoid arthritis suggest that the effects of adalimumab can last for 4 weeks to 3 months after cessation of therapy, consistent with our observations [33].
The primary safety concern when treating with TNF-α inhibitors, like adalimumab, is infection particularly disseminated M. tuberculosis. We screened both subjects for M. tuberculosis exposure at baseline and both were negative. Neither developed a chronic cough during the treatment period and so no further testing for tuberculosis was performed. Other more common infections reported to increase during treatment with adalimumab include sinusitis (11%) and upper respiratory infections (17%); headache is also common (12%). These AEs occurred in both subjects during treatment with placebo, and are common ailments in patients with MPS.
This study is limited by the small sample size. The duration of the study is short, particularly for the safety outcomes. Finally, the presence of erythema at the injection sites for Subject #2 in effect unblinded the parents, subject, coordinators, and PI; however, the individuals who measured ROM and anthropometry were not privy to this information and so remained blinded throughout the study. This unblinding of the subject and parents may have influenced their responses to the CHQ-PF50 and the PPQ where the parents' response on the CHQ-PF50 indicated improvement at the end of the treatment phase versus the subject's response on the PPQ indicated no significant improvement. However, this discrepancy was present for Subject #1 as well where the blinding was maintained and the parent answered both pain questions due to cognitive limitations of Subject #1. Despite these limitations, we found improvements in ROM, behavior, and growth in both subjects during treatment with adalimumab.
5. Conclusions
In conclusion, although joint and other skeletal disease in MPS are complex and likely due to a multifaceted interplay of inflammatory and mechanical factors, data from this small pilot study suggests that treatment with adalimumab may improve physical function, and possibly pain, in children with MPS I or II. A larger study of adalimumab in individuals with MPS I and II is indicated.
Acknowledgements
We gratefully acknowledge the study participants and parents as well as Nathalia Cressey and Angel (Jun) Zozobrado who made this project possible. The research described was supported by the MPS1 Foundation and the NIH/National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number UL1TR000124. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the MPS1 Foundation, the CTSI or the NIH.
Contributor Information
Lynda E. Polgreen, Email: lpolgreen@labiomed.org.
Alicia Kunin-Batson, Email: kunin003@umn.edu.
Kyle Rudser, Email: rudser@umn.edu.
Richard K. Vehe, Email: vehex001@umn.edu.
Jeanine J. Utz, Email: utzx0002@umn.edu.
Chester B. Whitley, Email: whitley@umn.edu.
Patricia Dickson, Email: pdickson@labiomed.org.
References
- 1.E.B. Fung, J.A. Johnson, J. Madden, T. Kim, P. Harmatz, Bone density assessment in patients with mucopolysaccharidosis: a preliminary report from patients with MPS II and VI, J. Pediatr. Rehabil. Med. 3 (n.d.) 13–23. [PMC free article] [PubMed]
- 2.Polgreen L.E., Tolar J., Plog M., Himes J.H., Orchard P.J., Whitley C.B., Miller B.S., Petryk A. Growth and endocrine function in patients with Hurler syndrome after hematopoietic stem cell transplantation. Bone Marrow Transplant. 2008;41:1005–1011. doi: 10.1038/bmt.2008.20. [DOI] [PubMed] [Google Scholar]
- 3.E. Oussoren, M.M. Brands, G.J. Ruijter, A.T. der Ploeg, A.J. Reuser, Bone, joint and tooth development in mucopolysaccharidoses: relevance to therapeutic options, Biochim. Biophys. Acta 1812 (n.d.) 1542–56. [DOI] [PubMed]
- 4.Weisstein J.S., Delgado E., Steinbach L.S., Hart K., Packman S. Musculoskeletal manifestations of Hurler syndrome: long-term follow-up after bone marrow transplantation. J. Pediatr. Orthop. 2004;24:97–101. doi: 10.1097/00004694-200401000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Link B., de Camargo Pinto L.L., Giugliani R., Wraith J.E., Guffon N., Eich E., Beck M. Orthopedic manifestations in patients with mucopolysaccharidosis type II (Hunter syndrome) enrolled in the Hunter Outcome Survey. Orthop. Rev. Pavia. 2010;2 doi: 10.4081/or.2010.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones S.A., Parini R., Harmatz P., Giugliani R., Fang J., Mendelsohn N.J. The effect of idursulfase on growth in patients with Hunter syndrome: data from the Hunter Outcome Survey (HOS) Mol. Genet. Metab. 2013;109:41–48. doi: 10.1016/j.ymgme.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Monroy M.A., Ross F.P., Teitelbaum S.L., Sands M.S. Abnormal osteoclast morphology and bone remodeling in a murine model of a lysosomal storage disease. Bone. 2002;30:352–359. doi: 10.1016/s8756-3282(01)00679-2. [DOI] [PubMed] [Google Scholar]
- 8.Rimoin D.L., Silberberg R., Hollister D.W. Chondro-osseous pathology in the chondrodystrophies. Clin. Orthop. Relat. Res. 1976:137–152. [PubMed] [Google Scholar]
- 9.Nuttall J.D., Brumfield L.K., Fazzalari N.L., Hopwood J.J., Byers S. Histomorphometric analysis of the tibial growth plate in a feline model of mucopolysaccharidosis type VI. Calcif. Tissue Int. 1999;65:47–52. doi: 10.1007/s002239900656. [DOI] [PubMed] [Google Scholar]
- 10.Russell C., Hendson G., Jevon G., Matlock T., Yu J., Aklujkar M., Ng K.Y., Clarke L.A. Murine MPS I: insights into the pathogenesis of Hurler syndrome. Clin. Genet. 1998;53:349–361. doi: 10.1111/j.1399-0004.1998.tb02745.x. [DOI] [PubMed] [Google Scholar]
- 11.Silveri C.P., Kaplan F.S., Fallon M.D., Bayever E., August C.S. Hurler syndrome with special reference to histologic abnormalities of the growth plate. Clin. Orthop. Relat. Res. 1991:305–311. [PubMed] [Google Scholar]
- 12.Simonaro C.M., D'Angelo M., Haskins M.E., Schuchman E.H. Joint and bone disease in mucopolysaccharidoses VI and VII: identification of new therapeutic targets and biomarkers using animal models. Pediatr. Res. 2005;57:701–707. doi: 10.1203/01.PDR.0000156510.96253.5A. [DOI] [PubMed] [Google Scholar]
- 13.Simonaro C.M., Ge Y., Eliyahu E., He X., Jepsen K.J., Schuchman E.H. Involvement of the Toll-like receptor 4 pathway and use of TNF-α antagonists for treatment of the mucopolysaccharidoses. Proc. Natl. Acad. Sci. 2010;107:222–227. doi: 10.1073/pnas.0912937107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simonaro C.M., Haskins M.E., Schuchman E.H. Articular chondrocytes from animals with a dermatan sulfate storage disease undergo a high rate of apoptosis and release nitric oxide and inflammatory cytokines: a possible mechanism underlying degenerative joint disease in the mucopolysaccharidoses. Lab. Investig. J. Tech. Methods Pathol. 2001;81:1319–1328. doi: 10.1038/labinvest.3780345. [DOI] [PubMed] [Google Scholar]
- 15.Eliyahu E., Wolfson T., Ge Y., Jepsen K.J., Schuchman E.H., Simonaro C.M. Anti-TNF-alpha therapy enhances the effects of enzyme replacement therapy in rats with mucopolysaccharidosis type VI. PLoS One. 2011;6 doi: 10.1371/journal.pone.0022447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Oliveira P.G., Baldo G., Mayer F.Q., Martinelli B., Meurer L., Giugliani R., Matte U., Xavier R.M. Characterization of joint disease in mucopolysaccharidosis type I mice. Int. J. Exp. Pathol. 2013;94:305–311. doi: 10.1111/iep.12033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simonaro C.M., D'Angelo M., He X., Eliyahu E., Shtraizent N., Haskins M.E., Schuchman E.H. Mechanism of glycosaminoglycan-mediated bone and joint disease: implications for the mucopolysaccharidoses and other connective tissue diseases. Am. J. Pathol. 2008;172:112–122. doi: 10.2353/ajpath.2008.070564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simonaro C.M. Cartilage and chondrocyte pathology in the mucopolysaccharidoses: the role of glycosaminoglycan-mediated inflammation. J. Pediatr. Rehabil. Med. 2010;3:85–88. doi: 10.3233/PRM-2010-0120. [DOI] [PubMed] [Google Scholar]
- 19.Martin D.C., Atmuri V., Hemming R.J., Farley J., Mort J.S., Byers S., Hombach-Klonisch S., Csoka A.B., Stern R., Triggs-Raine B.L. A mouse model of human mucopolysaccharidosis IX exhibits osteoarthritis. Hum. Mol. Genet. 2008;17:1904–1915. doi: 10.1093/hmg/ddn088. [DOI] [PubMed] [Google Scholar]
- 20.Polgreen L.E., Vehe R.K., Rudser K., Kunin-Batson A., Utz J.J., Dickson P., Shapiro E., Whitley C.B. Elevated TNF-α is associated with pain and physical disability in mucopolysaccharidosis types I, II, and VI. Mol. Genet. Metab. 2016;117:427–430. doi: 10.1016/j.ymgme.2016.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bresnihan B. Preventing joint damage as the best measure of biologic drug therapy. J. Rheumatol. 2002;65:39–43. [PubMed] [Google Scholar]
- 22.Chatzidakis I., Mamalaki C. T cells as sources and targets of TNF: implications for immunity and autoimmunity. Curr. Dir. Autoimmun. 2010;11:105–118. doi: 10.1159/000289200. [DOI] [PubMed] [Google Scholar]
- 23.Tugwell P., Wells G., Strand V., Maetzel A., Bombardier C., Crawford B., Dorrier C., Thompson A. Clinical improvement as reflected in measures of function and health-related quality of life following treatment with leflunomide compared with methotrexate in patients with rheumatoid arthritis: sensitivity and relative efficiency to detect a treatment effect in a twelve-month, placebo-controlled trial. Leflunomide Rheumatoid Arthritis Investigators Group. Arthritis Rheum. 2000;43:506–514. doi: 10.1002/1529-0131(200003)43:3<506::AID-ANR5>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 24.Strand V., Singh J.A. Newer biological agents in rheumatoid arthritis: impact on health-related quality of life and productivity. Drugs. 2010;70:121–145. doi: 10.2165/11531980-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 25.Kosinski M., Zhao S.Z., Dedhiya S., Osterhaus J.T., Ware J.E., Jr. Determining minimally important changes in generic and disease-specific health-related quality of life questionnaires in clinical trials of rheumatoid arthritis. Arthritis Rheum. 2000;43:1478–1487. doi: 10.1002/1529-0131(200007)43:7<1478::AID-ANR10>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 26.Muenzer J., Wraith J.E., Beck M., Giugliani R., Harmatz P., Eng C.M., Vellodi A., Martin R., Ramaswami U., Gucsavas-Calikoglu M., Vijayaraghavan S., Wendt S., Wendt S., Puga A.C., Puga A., Ulbrich B., Shinawi M., Cleary M., Piper D., Conway A.M., Conway A.M., Kimura A. A phase II/III clinical study of enzyme replacement therapy with idursulfase in mucopolysaccharidosis II (Hunter syndrome) Genet. Med. Off. J. Am. Coll. Med. Genet. 2006;8:465–473. doi: 10.1097/01.gim.0000232477.37660.fb. (doi:10.109701.gim.0000232477.37660.fb) [DOI] [PubMed] [Google Scholar]
- 27.Muenzer J., Gucsavas-Calikoglu M., McCandless S.E., Schuetz T.J., Kimura A. A phase I/II clinical trial of enzyme replacement therapy in mucopolysaccharidosis II (Hunter syndrome) Mol. Genet. Metab. 2007;90:329–337. doi: 10.1016/j.ymgme.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 28.Okuyama T., Tanaka A., Suzuki Y., Ida H., Tanaka T., Cox G.F., Eto Y., Orii T. Japan Elaprase Treatment (JET) study: idursulfase enzyme replacement therapy in adult patients with attenuated Hunter syndrome (Mucopolysaccharidosis II, MPS II) Mol. Genet. Metab. 2010;99:18–25. doi: 10.1016/j.ymgme.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 29.Schmidt M., Breyer S., Löbel U., Yarar S., Stücker R., Ullrich K., Müller I., Muschol N. Musculoskeletal manifestations in mucopolysaccharidosis type I (Hurler syndrome) following hematopoietic stem cell transplantation. Orphanet J. Rare Dis. 2016;11 doi: 10.1186/s13023-016-0470-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kakkis E.D., Muenzer J., Tiller G.E., Waber L., Belmont J., Passage M., Izykowski B., Phillips J., Doroshow R., Walot I., Hoft R., Neufeld E.F. Enzyme-replacement therapy in mucopolysaccharidosis I. N. Engl. J. Med. 2001;344:182–188. doi: 10.1056/NEJM200101183440304. [DOI] [PubMed] [Google Scholar]
- 31.Sifuentes M., Doroshow R., Hoft R., Mason G., Walot I., Diament M., Okazaki S., Huff K., Cox G.F., Swiedler S.J., Kakkis E.D. A follow-up study of MPS I patients treated with laronidase enzyme replacement therapy for 6 years. Mol. Genet. Metab. 2007;90:171–180. doi: 10.1016/j.ymgme.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 32.Clarke L.A., Wraith J.E., Beck M., Kolodny E.H., Pastores G.M., Muenzer J., Rapoport D.M., Berger K.I., Sidman M., Kakkis E.D., Cox G.F. Long-term efficacy and safety of laronidase in the treatment of mucopolysaccharidosis I. Pediatrics. 2009;123:229–240. doi: 10.1542/peds.2007-3847. [DOI] [PubMed] [Google Scholar]
- 33.den Broeder A., van de Putte L., Rau R., Schattenkirchner M., Van Riel P., Sander O., Binder C., Fenner H., Bankmann Y., Velagapudi R., Kempeni J., Kupper H. A single dose, placebo controlled study of the fully human anti-tumor necrosis factor-alpha antibody adalimumab (D2E7) in patients with rheumatoid arthritis. J. Rheumatol. 2002;29:2288–2298. [PubMed] [Google Scholar]