Online communication (including email, social media, and web-based support groups) could be used to enhance cancer treatment decision making and care support. Yet, little is known about whether and how patients with newly diagnosed cancer use these technologies during the treatment decision process and even less is known about whether online communication use influences patient appraisals of decision making. Therefore, we characterized online communication use in a diverse, population-based sample of women with a new diagnosis of breast cancer and assessed whether the use of these modalities resulted in increased satisfaction and decision deliberation during the breast cancer treatment decision process.
Methods
This study was approved by the institutional review boards of the University of Michigan, University of Southern California, and Emory University. A waiver of documentation of informed consent was obtained, and return of the survey was considered written consent. A total of 3631 women aged 20 to 79 years with newly diagnosed breast cancer (stages I–III) as reported to the Surveillance, Epidemiology, and End Results (SEER) registries of Georgia and Los Angeles County from July 2013 through September 2014 were surveyed a mean of 6 months after diagnosis about their treatment experiences as part of the iCanCare Study (2578 respondents [71% response rate]). Those who had complete information regarding online communication use and their appraisal of decision making (decision satisfaction and deliberation) were included in this analysis (N = 2460).
Respondents were asked how often since their diagnosis they used different forms of communication, including email or texting, social media (such as Twitter, Facebook, and blogs), and/or web-based support groups (5-point Likert scales from “never” to “always”) to discuss their breast cancer diagnosis, treatment, or care. A summary measure was then derived to represent and/or use of the 3 different modalities and categorized into never or rarely, some, or frequent use.
Patient appraisal of decision making was assessed using the established 5-item decision satisfaction scale, categorized into high vs lower satisfaction.1,2 We also evaluated a newly developed 4-itemmeasure of deliberation derived from a measure of public deliberation3 and categorized into more vs less deliberation.
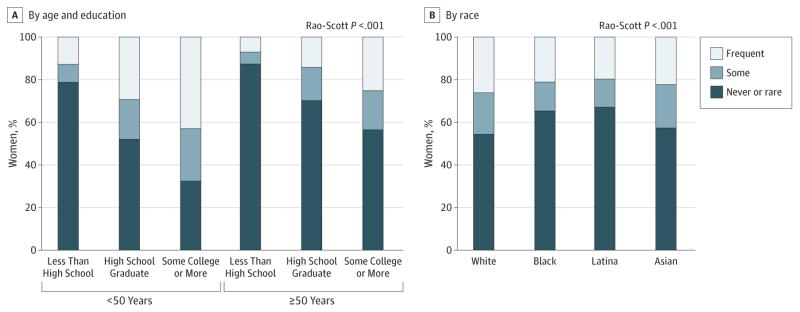
Percentages reported in the Results section are weighted. Bivariate weighted associations between patient demographic characteristics (age, race, and education) and the frequency of online communication use were evaluated using Rao-Scott χ2 tests. Multivariable, weighted logistic regression was then used to estimate the association between the frequency of online communication use and high decision satisfaction and more decision deliberation.
Results
The mean (SD) age at survey was 61.9 (0.2) years; 1398 (59.3%) of the cohort were white, followed by black (429 [16.3%]), Latina (429 [13.6%]), Asian (216 [8.3%]), and other/unknown(58 [2.4%]), and 1725 (72.9%) had some college education or more. Overall, 1002 (41.2%) of women reported some or frequent use of online communication, most commonly for email or texting (834 [34.7%]), with less use of social media (305 [12.3%]) and web-based support groups (289 [11.9%]).
Variation in online communication use across age and education existed, with a stronger association between more education and some or frequent online communication use among the younger women (P < .001) (Figure, A). The frequency of any online communication use also varied across race, with the highest proportion of some or frequent use among white and Asian women (610 [45.6%] and 94 [42.7%]), followed by blacks (151 [34.7%]) and Latinas (133 [32.9%]) (P < .001) (Figure, B).
Figure. Frequency of Online Communication Usea.
aOnline communication use was defined using a summary measure derived to represent and/or use of the 3 different modalities and categorized into never or rare, some (sometimes), or frequent (often or always) use (as measured on a 5-point Likert scale).
Compared with never-users, women who were frequent online communication users more positively appraised their decision making. They were more likely to report a more deliberative decision (adjusted odds ratio, 1.67;95%CI, 1.34–2.10)and were also more likely to report high decision satisfaction (adjusted odds ratio, 1.45; 95%CI, 1.06–1.98) (Table).
Table.
Relationship Between Frequency of Online Communication Use and More Deliberative Decisions and Higher Decision Satisfaction
| Online Communication Use Category | No. (Weighted %) | Adjusted OR (95% CI)a | P Valueb | |
|---|---|---|---|---|
| Less/Low | More/High | |||
| Deliberative decision | ||||
| Never or rare use | 754 (65.3) | 704 (53.2) | 1 [Reference] | <.001 |
| Some use | 184 (16.4) | 244 (18.3) | 1.27 (1.00–1.62) | |
| Frequent use | 211 (18.3) | 363 (28.5) | 1.67 (1.34–2.10) | |
| Decision satisfaction | ||||
| Never or rare use | 297 (64.9) | 1161 (57.4) | 1 [Reference] | .02 |
| Some use | 74 (15.9) | 354 (17.8) | 1.18 (0.85–1.64) | |
| Frequent use | 87 (19.2) | 487 (24.8) | 1.45 (1.06–1.98) | |
Abbreviation: OR, odds ratio.
Weighted and adjusted for age, race, education, family history, and treatment.
Rao-Scott P values.
Discussion
Findings from this study suggest that frequent use of online communication may be associated with more positive appraisal of treatment decision making. However, in this sample, online communication use was limited, with most of the use attributed to email and/or texting and less to social media and web-based support groups. The presence of variation across age, race, and education reinforces that barriers exist to incorporating these modalities broadly across patients with cancer. Additional research is needed before these modalities can be leveraged to improve patient care experiences.
Acknowledgments
Funding/Support: This research was supported by the National Cancer Institute of the National Institutes of Health (P01CA163233).
Footnotes
Author Contributions: Dr Wallner had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Drs Katz and Hawley shared senior authorship.
Study concept and design: Wallner, Martinez, Katz, Hawley.
Acquisition, analysis, or interpretation of data: Wallner, Martinez, Li, Jagsi, Janz, Katz, Hawley.
Drafting of the manuscript: Wallner, Martinez, Katz.
Critical revision of the manuscript for important intellectual content: Wallner, Martinez, Li, Jagsi, Janz, Katz, Hawley.
Statistical analysis: Wallner, Li.
Obtained funding: Jagsi, Janz, Katz, Hawley.
Study supervision: Wallner, Janz.
Conflict of Interest Disclosures: Dr Wallner discloses prior research grant funding from GlaxoSmithKline not related to the topic of this manuscript. No other disclosures are reported.
Role of Funder/Sponsor: The National Cancer Institute had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Previous Presentation: This article was presented in part at the 51st Annual Meeting of the American Society of Clinical Oncology; May 29 to June 2, 2015; Chicago, Illinois.
Additional Contributions: Emily Boltey, BSN, and Jaspreet Uppal, MPH, University of Michigan, provided assistance in preparation of this manuscript. They received no compensation for their contributions.
References
- 1.Holmes-Rovner M, Kroll J, Schmitt N, et al. Patient satisfaction with health care decisions: the satisfaction with decision scale. Med Decis Making. 1996;16(1):58–64. doi: 10.1177/0272989X9601600114. [DOI] [PubMed] [Google Scholar]
- 2.Hawley ST, Janz NK, Hamilton A, et al. Latina patient perspectives about informed treatment decision making for breast cancer. Patient Educ Couns. 2008;73(2):363–370. doi: 10.1016/j.pec.2008.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burkhalter S, Gastil J, Kelshaw T. A conceptual definition and theoretical model of public deliberation in small face-to-face groups. Commun Theory. 2002;12(4):398–422. [Google Scholar]