Abstract
Objectives:
The aim of this study was to examine the presence of antimicrobial resistance / susceptibility strains of Escherichia coli in inpatients and outpatients.
Materials and methods:
It is a retrospective study carried out at the Department of Microbiology, Parasitology and Virology Faculty of Medicine, University of Sarajevo. In cooperation with the Microbiological laboratory of the Cantonal Hospital Zenica and the Microbiological laboratory of the General Hospital Tesanj, 3863 urine samples were processed in the period from March 1st to March 31st 2016.
Results:
Our study showed that E. coli had the highest antimicrobial resistance to trimethoprim / sulfamethoxazole (38.61%), followed by amoxicillin / clavulanic acid (19.62%), ciprofloxacin (9.49%), gentamicin (8.86%), cephalexin (8.23%), nitrofurantoin (8.23%), cefuroxime (7.52%), ceftazidime (6.33%), cefuroxime (89.87%), amikacin (4.43%).
Conclusions:
The isolated strains of E. coli showed the highest resistance to trimethoprim / sulfamethoxazole and amoxicillin / clavulanic acid. The isolated strains of E. coli showed the greatest susceptibility to amikacin and ceftazidime. Gender distribution of positive E. coli isolates showed statistically significant differences in favor of females.
Keywords: E. coli, antimicrobial resistance, susceptibility
1. INTRODUCTION
Urinary tract infections are, after respiratory, the most common infection in humans (1). At least 80-90% of outpatient and 30-50% of inpatient urinary tract infections is caused by uropathogenic Escherichia coli (E. coli) (2). Specific human populations are at increased risk of developing urinary tract infection (UTI). These groups include children, pregnant women, the elderly, postmenopausal women, patients with spinal cord injuries and/or with catheters, patients with diabetes, multiple sclerosis, patients with human immunodeficiency virus (HIV) and patients with previous urological abnormalities (3). In children with a suspected urinary tract infection, the most common management strategy is to treat empirically with an antibiotic while waiting for results of culture and susceptibility testing. Young children are more vulnerable to immediate and long term complications, such as renal scarring and renal failure, and therefore require prompt appropriate treatment. Escherichia coli is the most common cause of bacteriaemia and also causes meningitis in neonates (4). Although urinary tract infections can occur in both men and women, it is more common in adult women than adult men.
In addition to frequency, urinary tract infections are also recurrent, and due to the resistance of uropathogenic bacteria to antibiotics, the access to alternative therapeutic procedures is growing (5).
The high frequency of infections, not only leads to major economic costs, but also to a decrease in labor productivity and high morbidity of patients (1). The aim of treatment for acute urinary tract infections is the eradication of pathogens, relief of symptoms, and reduction of the risk of permanent damage to the kidneys. The choice of medicaments for initial, empirical treatment (pending the outcome of susceptibility testing) is based on local sensitivities. The sensitivity of bacteria to antibiotics varies in relation to the geographical region, due to frequent use and misuse (6).
Since the discovery of antibiotics and their widespread use, many bacteria have developed mechanisms that make them resistant to some, but in some cases to almost all antibiotics (7). In Europe, the antimicrobial resistance of Gram-negative bacteria is increasing, especially E. coli, which accounts for the majority of invasive Gram-negative strains in European countries (8). Antimicrobial resistance is recognized threat to health, internationally. The contribution of primary healthcare is particularly important as this is where about 80% of all antibiotics used within the health service are prescribed (4).
Continuing education as well as the implementation of effective measures of activities to prevent and control infections may also reduce the occurrence of resistance (9). The aim of this study was to determine the frequency of outpatient and inpatient urinary tract infections caused by E. coli and to examine the presence of antimicrobial resistance / susceptibility strains of Escherichia coli in inpatients and outpatients.
2. MATERIAL AND METHODS
During the period from March 1st until March 31st, 2016, 3863 urine samples were tested in the region of Zenica-Doboj Canton, Bosnia and Herzegovina.
Midstream, clean-catch urine samples were sent to the laboratory for standard urinalysis and culture. The tested material was an urine sample of patients with symptoms of urinary tract infections processed in the Microbiological laboratory of the Cantonal Hospital in Zenica and the Microbiological laboratory of the General Hospital Tesanj, Bosnia and Herzegovina.
Bacteriological analysis of urine samples included microscopic identification, cultivation, standard biochemical testing and antimicrobial susceptibility testing. Urine samples were inoculated on blood agar and Endo agar, with incubation of 37°C for 24 hours. After the incubation period, we determined the number of bacteria in 1 ml of urine. Significant number of bacteria in urine (> 105 bacteria/ml) were tested to the basic biochemical reactions characteristic for E. coli, including double sugar, peptone water, mannitol, urea, and citrate. After the detection and identification of bacteria, we approached analyzing antimicrobial susceptibility by disc-diffusion method according to EUCAST (The European Committee on Antimicrobial Susceptibility Testing) standards. For susceptibility testing of Enterobacteriaceae it is used Mueller-Hinton (MH) agar by disc-diffusion method.
In our study, the susceptibility of E. coli was tested on the following antimicrobials: amoxicillin / clavulanic acid (AMC) 30 mg (ratio 20:10), cephalexin (CN) 30 mg, cefuroxime (CXM) 30 mg, ceftazidime (CAZ) 30 mg, amikacin (AK) 30 mg, gentamicin (GEN) 10 mg, ciprofloxacin (CIP) 5 mg, nitrofurantoin (NIT) 100 mg, trimethoprim / sulfamethoxazole (STX) 5 mg.
For the statistical analysis we used SPSS software program (Statistical Package for Social Sciences) version 24.0. Results of descriptive statistical analysis were broken down according to frequency and presented in absolute numbers and percentages. Differences between groups were tested by Mann-Whitney U test. The Shapiro-Wilk test was used for testing the significance of differences deviations from the normal distribution. Results are presented in tabular form and graphically, and accepted statistical level of significance difference was p<0.05.
3. RESULTS
The research showed that out of 3863 urine culture examined, 452 (11.70%) was positive and 3411 (88.30%) of tested urine culture was negative.
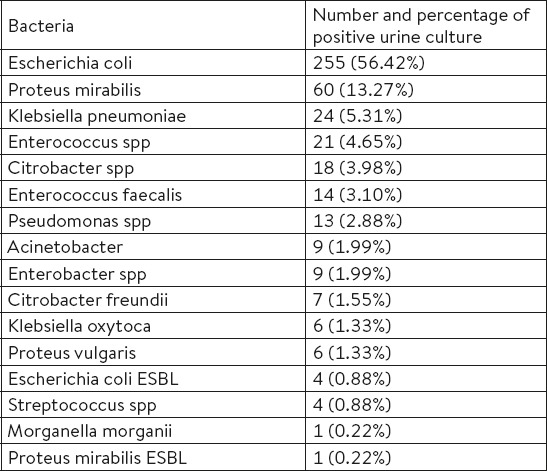
Table 1. shows the frequency of causes for positive urine culture and it can be seen that from a total of 452 samples of positive urine culture, 56.42% of samples were positive on E. coli. There were 13.27% of samples with positive urine culture on Proteus mirabilis, followed by 5.31% of samples positive on Klebsiella pneumoniae, Enterococcus spp (4.65%), Citrobacter spp (3.98%), Enterococcus faecalis (3.10%) and Pseudomonas spp (2.88%). Other bacteria had incidence of less than 2% of positive urine culture samples.
Table 1.
Distribution of bacteria in positive urine culture
Urine cultures positive for E. coli (255) were isolated in 158 patients. Out of 158 patients, 123 (77.85%) were outpatients, while 35 (22.15%) were inpatients. Based on gender distribution positive test for E. coli was recorded in 142 (89.87%) female patients and 16 (10.13%) male patients. There was a statistically significant difference in favor of females (p<0.05).
Based on the age distribution, patients with isolated E. coli were split in four age groups: age 0 to 6, age 7 to 18, age 19 to 60 and age group over 60. It has seen that 54 patients (34.18%) were in the age group 19 to 60 years, 53 patients (33.54%) were in the age group over 60 years, 36 patients (22.78) were in the age group 0 to 6 years and 15 patients (9.49%) were in the age group 7 to 18.
Based on gender distribution in each age group (Figure 1.) There is a significant difference (p=0.001). Within females, significantly lowest incidence is in the age group from 7 to 18 years (p<0.001). Within males, there are no significant differences by age group (p=0.751).
Figure 1.
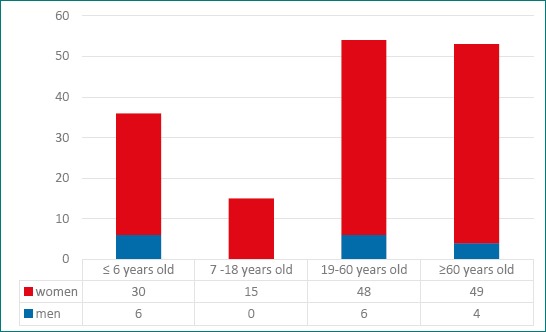
The ratio of gender and age groups of patients with isolated E. coli
Figure 2.
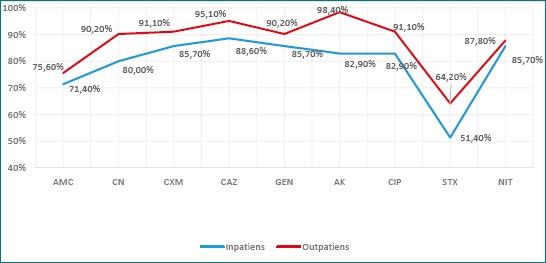
The susceptibility of E. coli strains to antibiotics of inpatients and outpatients
Figure 3.
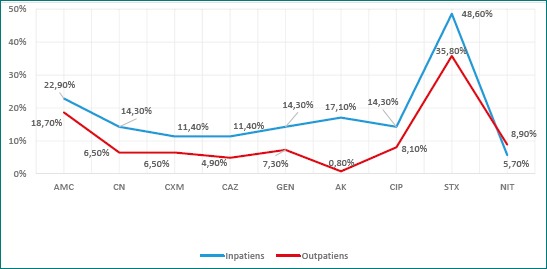
The resistance of E. coli strains to antibiotics of inpatients and outpatients
There was no significant difference in susceptibility between the groups any of the antibiotics.
The greatest resistance of E. coli strains was observed to trimethoprim / sulfamethoxazole, in both, inpatients (48.60%) and outpatients (35.80%). The lowest resistance of E. coli strains of inpatients was observed to nitrofurantoin (5.70%), while the lowest resistance of E. coli strains of outpatients was observed to amikacin (0.80%). Amikacin resistance in inpatients amounted to 17.10%, while in outpatients was 0.80%, therefore there was a statistically significant difference (p <0.001).
4. DISCUSSION
Urinary tract infections are one of the most common bacterial infection that can affect the bladder, urethra or kidneys. Escherichia coli, as gram-negative bacteria, is the dominant cause and can be easily grown in the laboratory.
E. coli causes more than 80% of urinary tract infections in previously healthy women. First, there is fecal contamination of periurethral area, then the bacteria spreads on ascending through the bladder and causes cystitis. These infections of the lower urinary tract, in some cases, can affect the kidneys and cause acute pyelonephritis, which consequently may result in bacteremia and sepsis (10).
According to our study, of 158 patients with E. coli 142 (89.87%) patients were female and 16 patients (10.13%) were males. There was a statistically significant difference in favor of females (p <0.05). Malmartel (11) also in its research conducted in France proved the prevalence of female gender, where 86.4% of E. coli positive urine culture were women. The reason for this may be that, anatomically, women have a shorter urethra which facilitates the ascending spread of bacteria (5).
By examining the frequency of E. coli in hospital and outpatients, we came to the result that 77.85% were outpatients and 22.15% were hospital patients. Sahuquillo-Arce et al. (12) with his study in Spain, which included 25 microbiological laboratories also proved that the isolates from the community are more common than the hospital ones.
Treatment of urinary tract infections is becoming more complicated with an increase of the number of resistant strains to antibiotics and prevalence of antibiotic resistance mechanisms. The majority of strains of E. coli were identified as resistant to the antibiotics such as ampicillin, amoxicillin / clavulanic acid, norfloxacin, cefuroxime, ceftriaxone, and trimethoprim/sulfamethoxazole (13). The emergence of antibiotic resistance is a major threat to public health, which is driven by excessive use of antibiotics. Antibiotics are among the most frequently prescribed medications in hospitalized patients, which are often prescribed inappropriately. The positive urine cultures are the trigger for antibiotic therapy in hospitalized patients. The guidelines recommend avoiding antibiotic therapy in bacteriuria in the absence of symptoms, with a few exceptions, such as pregnancy. Despite the recommendations, antibiotic treatment is prevalent and every day contributes to increasing antibiotic resistance, increased costs, and antibiotic side effects, such as Clostridium difficile infection (14).
According to the results of our study, E. coli strains showed the highest antimicrobial susceptibility to amikacin (94.94%) and ceftazidime (93.67%). The sensitivity of E. coli to cefuroxime was 89.87%, ciprofloxacin 89.24%, gentamicin 89.24%, cefalexin 87.97%, nitrofurantoin 87.97%, amoxicillin / clavulanic acid 74.68%, trimethoprim / sulfamethoxazole 61.39 %, indicating that the E. coli is significantly sensitive to all tested antibiotics (p<0.01; p <0.05).
The greatest resistance strains of E. coli to antibiotics in our study showed trimethoprim/sulfamethoxazole (38.61%) and amoxicillin / clavulanic acid (19.62%). E. coli resistance to ciprofloxacin was 9.49%, gentamicin 8.86%, cephalexin 8.23%, nitrofurantoin 8.23%, cefuroxime 7.52%, ceftazidime 7.52% and amikacin 4.43%.
In research conducted at the Department of Urology of the University Clinical Centre in Sarajevo, the highest level of resistance of E. coli found on trimethoprim / sulfamethoxazole (55%) and ampicillin (53%), followed by ciprofloxacin 17%, amoxicillin / clavulanic acid and gentamicin 16.6% (15).
The in vitro activities of trimethoprim / sulfamethoxazole and amoxicillin / clavulanic acid found in our study suggest that they would provide adequate alternative therapy in locations where trimethoprim / sulfamethoxazole use is no longer prudent because of elevated (>10 to 20%) rates of resistance.
Bacteria have developed mechanisms of genetic adaptation, and a result of the use of antibiotics is always faster or slower development of resistance. Because of the increase in bacterial resistance to antibiotics it is necessary to consistently monitor and be aware of resistance rates for specific pathogens in their own environment. If the resistance to the antibiotic is higher than 20%, the antibiotic should not be prescribed in an empirical antimicrobial therapy (16). The current global threat of antimicrobial resistance, an urgent need for it to be controlled, and the discovery of new antibacterial products has prompted many scientists to take measures such as rational use of antibiotics, infection control in health care, the formation of a strategy to reduce risk factors in the environment, the development of rapid diagnostic tests, promoting research on the prevention and control of antimicrobial resistance, the development of new antimicrobial and antibacterial agents strategies, improving awareness of population on the use of antibiotics and the risk of increasing their resistance in order to prevent the development and spread of resistance to antibiotics in the world (17). It is not a new problem, but it is becoming increasingly dangerous and requires urgent investment of effort and resources into its resolution (18).
5. CONCLUSIONS
Our research has shown that the largest number of E. coli isolates was found among outpatient population. Considering the highest resistance percentages of trimethoprim / sulfamethoxazole and amoxicillin / clavulanic acid, in both, outpatients and inpatients, we can conclude that these agents are not suitable for the empirical treatment of urinary tract infections. From our study, it is evident that unbiased surveillance of pathogens is important for antimicrobial decision-making. Unfortunately, such a database is non-existent in Zenica-Doboj Canton, as in other Cantons of Bosnia and Herzegovina. The results of our study indicate the existence of a great need for prevention of urinary tract infections rational use of antibiotics, as well as the multidisciplinary approach to further control the development of resistance.
Footnotes
• Author’s contribution: Mufida Aljicevic and Velma Rebic – collecting data from primary care and hospital and processing to Excel. Sabina Mahmutovic-Vranic – collection of literature on antibiotic resistance. Kadrija Abduzaimovic and Sabina Sestic – collecting medical history and send samples to the laboratory.
• Declaration of interest: There is no conflict of interest.
REFERENCES
- 1.Mobley H, Alteri C. Development of a Vaccine against Escherichia coli Urinary Tract Infections. Pathogens. 2015;5(1):1. doi: 10.3390/pathogens5010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ejrnæs K. Bacterial characteristics of importance for recurrent urinary tract infections caused by Escherichia coli. Dan Med Bull. 2011 Apr;58:4. [PubMed] [Google Scholar]
- 3.Jepson RG, Williams G, Craig JC. Cranberries for preventing urinary tract infections (updated review) Prescriber. 2013;24(4):20. [Google Scholar]
- 4.Bryce Ashley, et al. “Global Prevalence Of Antibiotic Resistance In Paediatric Urinary Tract Infections Caused By Escherichia Coli And Association With Routine Use Of Antibiotics In Primary Care:Systematic Review And Meta-Analysis”. BMJ. 2016:i939. doi: 10.1136/bmj.i939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Brien V, Hannan T, Schaeffer A, Hultgren S. Are you experienced? Understanding bladder innate immunity in the context of recurrent urinary tract infection. Current Opinion in Infectious Diseases. 2015;28(1):97–105. doi: 10.1097/QCO.0000000000000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stojanovic V, Milosevic B. Rezistencija Escherichiae Coli, najcesceg uzrocnika infekcija urinarnog trakta kod dece, na antibiotike. Med Pregl. 2010;63(1-2):109–12. doi: 10.2298/mpns1002109s. [DOI] [PubMed] [Google Scholar]
- 7.Džidic S, Suskovic J, Kos B. Antibiotic Resistance Mechanisms in Bacteria:Biochemical and Genetic Aspects. Food Technol. Biotechnol. 2008;46(1):11–21. [Google Scholar]
- 8.Lüthje P, Brauner A. Novel Strategies in the Prevention and Treatment of Urinary Tract Infections. Pathogens. 2016;5(1):13. doi: 10.3390/pathogens5010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakas B. Sarajevo: Ministarstvo zdravstva Kantona Sarajevo; 2016. Strateski program za kontrolu otpornosti bakterija na antibiotike za podrucje kantona Sarajevo za period 2012.–2016. godina. [Google Scholar]
- 10.Mobley H. Measuring Escherichia coli Gene Expression during Human Urinary Tract Infections. Pathogens. 2016;5(1):7. doi: 10.3390/pathogens5010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malmartel AGhasarossian C. Epidemiology of urinary tract infections, bacterial species and resistances in primary care in France. Eur J Clin Microbiol Infect Dis. 2016;35(3):447–51. doi: 10.1007/s10096-015-2560-1. [DOI] [PubMed] [Google Scholar]
- 12.Sahuquillo-Arce J, Selva M, Perpinan H, Gobernado M, Armero C, Lopez-Quilez A, et al. Antimicrobial Resistance in More than 100,000 Escherichia coli Isolates According to Culture Site and Patient Age, Gender, and Location. Antimicrobial Agents and Chemotherapy. 2011;55(3):1222–8. doi: 10.1128/AAC.00765-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma G, Sharma S, Sharma P, Chandola D, Dang S, Gupta S, Gabrani R. Escherichia coli biofilm:development and therapeutic strategies. J Appl Microbiol. 2016 Mar;:1–11. doi: 10.1111/jam.13078. [DOI] [PubMed] [Google Scholar]
- 14.Grein JD, Kahn KL, Eells SJ, Choi SK, Go-Wheeler M, Hossain T, Riva MY, Nguyen MH, Rekha Murthy A, Miller LG. Treatment for Positive Urine Cultures in Hospitalized Adults:A Survey of Prevalence and Risk Factors in 3 Medical Centers. Infect Control Hosp Epidemiol. 2016 Mar;37(3):319–26. doi: 10.1017/ice.2015.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Junuzovic Dz, Hasanbegovic M, Zvizdic S, Hamzic S, Zunic L. The Connection Between Endourological Procedures and Occurrence of Urinary Infections. Mater Sociomed. 2014 Aug;26(4):237–41. doi: 10.5455/msm.2014.237-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Culig J, Mlinaric-Džepina A, Leppee M, Vranes J. Rezistencija uropatogenih sojeva bakterije Escherichia coli kod trudnica i žena generativne dobi u usporedbi s potrosnjom antibiotika u Zagrebu. Med Glas. 2010;7(1):54–9. [PubMed] [Google Scholar]
- 17.Roca I, Akova M, Baquero F, Carlet J, Cavaleri M, Coenen S, et al. The global threat of antimicrobial resistance:science for intervention. New Microbes and New Infections. 2015;6:22–9. doi: 10.1016/j.nmni.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vranic Sabina, Aida Uzunovic. “Antimicrobial Resistance Of Escherichia Coli Strains Isolated From Urine At Outpatient Population:A Single Laboratory Experience”. Materia Socio Medica 28.2. 2016:121. doi: 10.5455/msm.2016.28.121-124. [DOI] [PMC free article] [PubMed] [Google Scholar]


