Abstract
Previous studies of inequality in health and mortality have largely focused on income-based inequality. Maternal education plays an important role in determining access to water and sanitation, and inequalities in child mortality arising due to differential access, especially in low- and middle-income countries such as Peru. This article aims to explain education-related inequalities in child mortality in Peru using a regression-based decomposition of the concentration index of child mortality. The analysis combines a concentration index created along a cumulative distribution of the Demographic and Health Surveys sample ranked according to maternal education, and decomposition measures the contribution of water and sanitation to educational inequalities in child mortality. We observed a large education-related inequality in child mortality and access to water and sanitation. There is a need for programs and policies in child health to focus on ensuring equity and to consider the educational stratification of the population to target the most disadvantaged segments of the population.
Introduction
Child mortality rates are important and sensitive indicators of population health. Low- and middle-income countries (LMICs) grappling with a high burden of infectious diseases have large differences in child mortality rates between the rich and the poor.1–3 This has motivated the investigation of contextual determinants of inequalities in child mortality.4 Measures of economic status such as household wealth represent the resources available to maintain good health and well-being. Yet, inequalities in child mortality exist not only as a difference between the economically poorest and the rest of the population. They follow a social gradient spread across the wealth spectrum and many other social dimensions. Among these dimensions, maternal education has been found to be a significant determinant of inequality in child mortality, with children of less educated mothers being at considerably higher risk.5 Moreover, maternal education, is doubly important for health-equity policies, as even small differences in education levels can influence inequalities in child mortality.5 Social status on the other hand is a composite entity consisting of a number of factors such as education, ethnic and religious affiliation, and geographic location.6 Therefore, complete equivalence between household wealth and socioeconomic inequality cannot be assumed.
Poor access to sanitation and safe drinking water has been widely documented as an easily preventable determinant of child mortality.7 Studies in Mali observed a lack of awareness among women about both recontamination in stored drinking water and the causal relation between microbial agents and diarrheal disease.8 Across national and cultural contexts, maternal education has been found to act through a variety of pathways9–11 that can be distinct from the influence of household wealth, for which the literature is abundant.11,12 These include variables like increased maternal agency in making decisions around a child's health, and the ability to both access and absorb decontextualized messages pertaining to health knowledge gained from sources like broadcast media.12 It has been shown that even for mothers with incomplete primary education, the odds of survival for children under 2 years of age are significantly greater than for illiterate mothers.13 Even where diarrhea is found to be higher among children of partially educated mothers than their illiterate counterparts, this inflation is indicative of the ability of mothers with some education to recognize and therefore report symptoms of the disease.13 Moreover, there is evidence to show that maternal education compensates for poverty.14 It has also been shown that across the globe, while testing the effect of education independent from wealth, children of mothers in a lower wealth band but with higher education experience lesser mortality than wealthier, less educated mothers.9 Thus, maternal education can also influence child health through pathways different from economic determinants only. Much of the existing literature on socioeconomic inequalities in access to water and sanitation has focused on the economic determinants of inequality, generally involving income or indices of household wealth.15,16 To provide a more holistic picture of health disparities, there is a need to address the social factors that contribute to inequalities in access to water and sanitation.
In accordance with existing frameworks, social inequality in child mortality is determined by the inequalities in higher-level variables such as education and more proximal factors such as access to water and sanitation, and their relationships with each other and with inequality in mortality.17 Further, disparities in proximal determinants like access to water and sanitation are not linear, from the poorest to the richest, but follow different patterns depending on the country and average coverage levels. It is therefore necessary to study the relative contribution of each determinant to inequality in child mortality, to tailor policies to a specific pattern of inequality.5 Decomposition methods have been used to understand factors that contribute to socioeconomic inequalities in both health outcomes18,19 and health interventions20–22, and whether public policies enacted to counteract existing inequalities are achieving their purpose.23 By quantitatively documenting the contribution of each determinant, this method can provide insights into potential interventions to reduce health disparities and ensure equity in the long run. Furthermore, many LMICs have undertaken specific reforms to address rising levels of inequalities in education, in access to water and sanitation23 and in health. Studying temporal changes in both resource access and health outcomes, and inequalities therein, can provide insight into the effectiveness of these reforms.
Peru is a highly relevant setting in which to study inequalities in child mortality. Although Peru has achieved the fourth Millennium Development Goal (MDG) of reducing under-five mortality by two-thirds between 2000 and 2015,24 socioeconomic inequalities in child health remain high, particularly in the Andean region.25 This is compounded by the fact that Peru is believed to be at severe risk of water shortages as a result of climate change and subsequent depletion of the Andean glaciers.26 Further, official policies in Peru have been criticized for lacking a broader focus inclusive of the socioeconomic realities in the country.27 Although the role of water access and sanitation and maternal education in child health has been studied previously,28 this study is novel in exploring the contribution of water, sanitation, and hygiene (WASH) access to educational inequalities in child mortality in Peru using decomposition methods.
The objectives of this article are to 1) quantify inequalities in child mortality between groups defined by levels of maternal education, 2) assess the contribution of unimproved water sources and lack of sanitation to these inequalities, and 3) document temporal changes in the contribution of access to water and sanitation to educational inequalities in child mortality in Peru.
Data and Methods
Data spanning 26 years and 10 survey waves from the Demographic and Health Surveys (DHS) for Peru, starting from the first wave in 1986 to the most recent one in 2012, were used in this study. The data were obtained from DHS upon request for this project. These cross-sectional surveys consist of different questionnaires, two of which were used in this project. From the “Birth” questionnaire, the age of the respondent (maternal age), education level, date of birth, and the age at death of each child born were collected. From the “Household” questionnaire, corresponding to each birth record from the “Birth” questionnaire, source of drinking water, sanitation facilities, variables identifying the cluster and household, and variables for various household assets were collected. For each woman between the ages of 15 and 49 years, the number of children born and the number that died under 2 years of age were estimated. Although a longer observation period for births is desirable to reduce censoring effects, it weakens the link between the recorded household characteristics including drinking water sources and sanitation facilities,29 and child mortality. Therefore, children born more than 5 years before the survey date were excluded. Also, to include only those children who were exposed to the full risk of mortality, those born less than 2 years before the survey dates were also excluded. Datasets corresponding to the “Birth” and “Household” questionnaires were merged to allow simultaneous measurement of individual mother-level variables and household-level variables. Consecutive surveys were appended together to create seven time periods (Table 1).
Table 1.
Descriptive statistics of determinants of child mortality
| 1986–1992 | 1996–2000 | 2003–2004 | 2005–2006 | 2007–2008 | 2009–2010 | 2011–2012 | |
|---|---|---|---|---|---|---|---|
| N = 51,459 | N = 135,362 | N = 13,286 | N = 27,461 | N = 46,868 | N = 95,126 | N = 91,755 | |
| Source of drinking water | |||||||
| Bottled water | 0.36 | – | 1.38 | 1.11 | 1.93 | 3.69 | |
| Piped into residence/dwelling | 48.96 | 58.49 | 67.60 | 72.28 | 73.70 | 75.34 | |
| Public tap | 7.34 | 3.44 | 4.80 | 4.17 | 4.38 | 2.98 | |
| Well in residence | 7.98 | 3.98 | No data | 2.97 | 2.15 | 2.84 | 2.20 |
| Public well | 6.10 | 6.34 | 2.84 | 2.91 | 2.61 | 1.93 | |
| Spring | 9.73 | 13.59 | 10.01 | 7.44 | 5.73 | 5.83 | |
| Open water body | 12.96 | 11.78 | 8.13 | 8.58 | 6.90 | 6.47 | |
| Rainwater | 0.04 | 1.47 | 0.03 | 0.19 | 0.18 | 0.28 | |
| Tanker truck | 2.52 | 0.92 | 2.26 | 1.16 | 1.73 | 1.28 | |
| Sanitation facilities | |||||||
| No facilities | 18.09 | 33.19 | 24.49 | 24.81 | 16.04 | 18.12 | 14.42 |
| Inside dwelling | 31.66 | 30.74 | 39.10 | 34.54 | 36.92 | 36.04 | 39.19 |
| Outside dwelling | 1.84 | 1.98 | 2.93 | 4.82 | 6.20 | 11.18 | 11.41 |
| Septic well | – | – | – | 3.88 | 10.59 | 1.60 | 2.33 |
| Pit latrine | 4.50 | 32.73 | 33.01 | 30.26 | 28.48 | 32.34 | 32.07 |
| Latrine on river/lake | 18.52 | 0.48 | 1.01 | 1.40 | 0.03 | 0.02 | |
| River, canal | 25.38 | 1.34 | – | 0.69 | 0.37 | 0.69 | 0.55 |
| Maternal age* | 24.40 (6.04) | 24.30 (6.08) | 24.20 (6.02) | 24.20 (6.05) | 24.10 (6.06) | 24.10 (6.04) | 24.10 (6.07) |
| Maternal education* | 4.90 (4.20) | 5.40 (4.29) | 6.40 (4.63) | 6.40 (4.56) | 6.80 (4.56) | 6.90 (4.50) | 7.10 (4.53) |
| Area of residence | |||||||
| Urban | 39.57 | 49.29 | 49.05 | 49.02 | 53.49 | 53.89 | 54.02 |
| Rural | 60.4 | 50.7 | 51.0 | 51.0 | 46.5 | 46.1 | 45.98 |
| Sex of the child | |||||||
| Female | 48.98 | 49.01 | 49.16 | 48.86 | 49.13 | 49.41 | 49.13 |
| Male | 51.02 | 50.99 | 50.84 | 51.14 | 50.87 | 50.59 | 50.87 |
| Proportion of all child deaths by household wealth | |||||||
| Poorest | 48.70† | 24.10 | 47.90 | 39.20 | 43.80 | 32.10 | 29.50 |
| Poorer | 18.10 | 12.90 | 27.00 | 21.50 | 27.30 | 24.50 | 22.50 |
| Middle | 22.40 | 15.00 | 12.50 | 13.90 | 13.00 | 21.10 | 18.60 |
| Richer | 8.10 | 32.50 | 8.30 | 17.70 | 8.90 | 12.40 | 18.20 |
| Richest | 2.40 | 15.20 | 4.10 | 7.50 | 6.80 | 9.80 | 10.80 |
Figures represent percentage of individual women unless otherwise indicated.
Mean (standard deviation).
Of all children that died during this period, 48.7% were in the poorest 20% by household wealth.
In contrast to the standard MDG indicator of under-five mortality, child mortality in this study was measured as the death of a child before attaining 2 years of age. This was done because a majority of under-five deaths occur within 2 years of life 30 and also because it allowed for a shorter censoring period.31 The variable describing drinking water sources was coded in the survey as follows: bottled water, piped water inside the dwelling, piped water inside yard, public standpipe, well within the dwelling, public well, springs, and open water bodies such as rivers, lakes, dams, and canals. It should be noted here that no distinction was present in surveys between covered and uncovered wells, and protected and unprotected springs, as suggested by the World Health Organization–United Nations Children's Emergency Fund Joint Monitoring Program guidelines.32 As a result, a binary variable was created with all forms of piped water classified as “Improved water sources” and other water sources classified as “Unimproved water sources.” Classification of sanitation facilities varied considerably among the survey waves, and hence two indicator variables for “Basic” (pit latrines and septic wells) and “No sanitation facilities” (latrines over rivers and open defecation into water bodies) were created.
Maternal education was measured in years of formal education completed by each woman surveyed. The median value for “years of education” in each survey was taken as a cut-point to define “high” and “low” levels of education among mothers. An index of household wealth was created for each period, along the lines of the DHS index, but excluding the WASH variables. Multiple correspondence analysis was used to create this index keeping in mind the binary and categorical nature of the variables representing asset ownership.33 The variables included in this index were household electrification, presence of a radio in the household, ownership of a bicycle, car ownership, and building materials of the wall, floor, and roof of the household. The households were then divided into wealth quintiles based on this index and a binary variable to indicate household poverty was created with the bottom two quintiles of wealth designated as poor.
To conduct the decomposition analysis, multilevel regressions with generalized estimating equations for the binomial family with a log link were first used and risk ratios were estimated. The first level of analysis was individual births and the second level was defined by clusters as defined by the DHS surveys. The numbering of clusters was unique only to a given survey and not across all 10 waves. Therefore, a new variable “Community ID” was created, by grouping the cluster number and the year of each survey. To account for potential determinants in the decomposition b as indicated in existing literature,31,32,34 the models were adjusted for sex of the child, maternal age, urban versus rural residence, and household poverty.
Measuring educational inequalities in child health.
The concentration curve and concentration index are measures of inequality that provide a picture of health variation across the entire gradient of a given socioeconomic variable; in this case, the education level of the mother. The concentration index is mathematically defined as twice the area under the concentration curve.35 The index C is often represented in the following form:
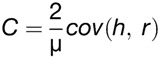 |
(1) |
where h is the health variable, μ is the mean of the health variable, and r represents the fractional rank of the observation in the education distribution. The concentration index ranges from −1 to 1, with 0 signifying perfect equality. For child mortality, the concentration curve lies above the diagonal line and the index takes a negative value indicating that child mortality is concentrated among less educated women.
Decomposing educational inequality in child mortality.
Decomposition of the concentration index allows us to quantify the contribution of each variable to educational inequality in child mortality. For a regression model linking child mortality y to a set of k variables, the concentration index “C” of y can be written as:
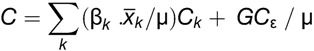 |
(2) |
where Ck represents the concentration index of a specific determinant k, and the first term in Equation (2) constitutes the total deterministic part of C, the concentration index of the outcome. The second term is the concentration index for the residual term in the model. It represents the component of variation in health inequality which remains unexplained by the determinants included in the model and tends to be negligible for a well-specified model.36 The first term,  represents the elasticity of the outcome with respect to each determinant, where μ is the mean value of child mortality y,
represents the elasticity of the outcome with respect to each determinant, where μ is the mean value of child mortality y,  is the mean value of each of the k determinants of health included in the model, and βk is the coefficient from the regression model. The product of the elasticity and the concentration index for each variable forms its contribution to inequality in the outcome.35,36 The above steps were carried out for each time period. Reported results include the concentration index of each variable and its contribution to child mortality.
is the mean value of each of the k determinants of health included in the model, and βk is the coefficient from the regression model. The product of the elasticity and the concentration index for each variable forms its contribution to inequality in the outcome.35,36 The above steps were carried out for each time period. Reported results include the concentration index of each variable and its contribution to child mortality.
Temporal analyses.
Trends in the risk of child mortality due to unimproved water and lack of sanitation were observed by plotting the evolution of risk across time. Temporal changes in inequality and the contribution of the exposures to this inequality were assessed by fixing that no change in the distribution of exposures occurred since the first time period (1986–1992) and calculating the difference in total inequality (see calculation details in Supplemental Information).
Sensitivity analyses.
The 10 surveys were also organized into three periods namely, premillennium, postmillennium (2003–2008), and the most recent period (2009–2012) to assess the impact of a longer time span on the risk of mortality.
Results
Child mortality and socioeconomic indicators.
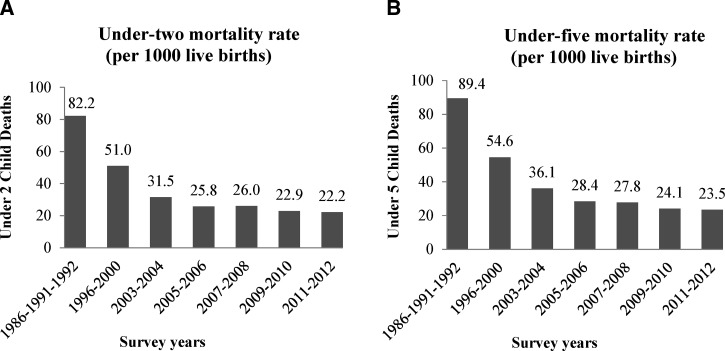
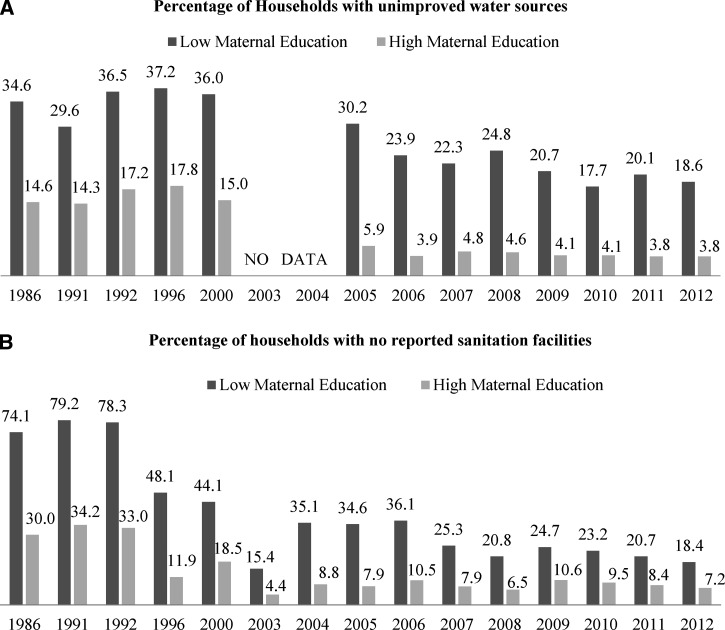
Child mortality in Peru showed a large drop in the premillennium period but has since flattened, although the trend points toward decreasing mortality, as seen in Figure 1 . In Figure 1, it can also be seen that the difference between the under-two mortality rate and under-five mortality rate is quite small and hence under-two mortality serves as a good approximation of under-five mortality which is the standard MDG indicator. Table 1 describes the socioeconomic indicators and primary exposures considered for this study. Figure 2 shows the percentage of households with unimproved sources for drinking water (2a) and no reported sanitation facilities (2b) by groups of high and low maternal education. In all the time periods, important differences were found in child mortality (P < 0.001), access to improved water sources (P < 0.001), and sanitation facilities (P < 0.001) between groups of high and low maternal education, with those in the low-education group doing worse on all counts. Profound differences in child mortality between urban and rural residence (P < 0.001) were also observed in all the time periods.
Figure 1.
Child mortality rates for Peru.
Figure 2.
Population proportions with poor water and sanitation by maternal education.* *The “Low” group represents education less than the median number of years and the “High” group represents education more than or equal to the median years of education of the mother.
Concentration curve and concentration index.
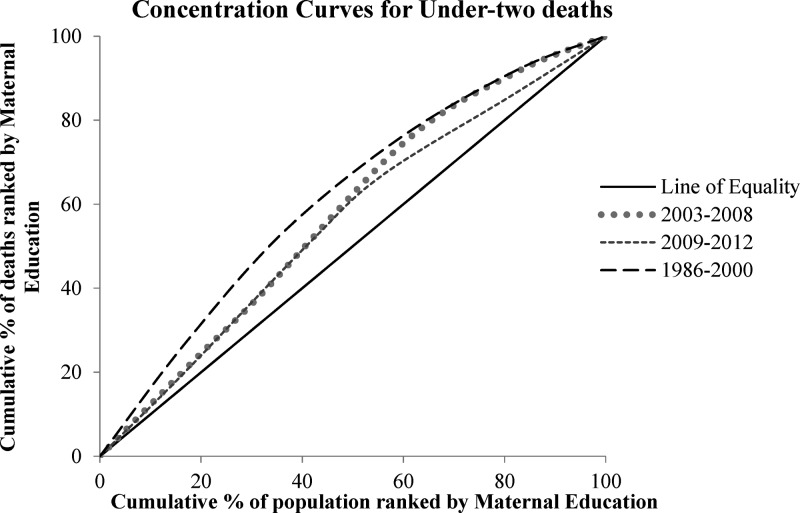
Figure 1 shows the concentration curves which represent the proportion of child mortality concentrated in cumulative proportions of the population where each mother is given a proportional rank across the education distribution. The concentration curves (Figure 3 ) are presented for three aggregate time periods; premillennium, postmillennium (up to 2008), and the last 5 years from available data (2009–2012). All three of the curves lie above the line of equality indicating the concentration of mortality among children of undereducated mothers. Similar curves were plotted to showcase inequalities in access to water and sanitation (Supplemental Figure 1). From Supplemental Table 1, unimproved sources of drinking water, a lack of sanitation facilities, and household poverty appear concentrated at the less educated end of the population distribution, as is seen from the negative sign of the concentration index for these indicators. On the other hand, education and urbanicity are concentrated among those where mothers are more educated. Further, this inequality indicated by the concentration indices is significant in all the time periods for unimproved drinking water, basic and no sanitation facilities, maternal education, household poverty, and urban residence.
Figure 3.
Concentration curves for under-two deaths in Peru.
Decomposition of educational inequality in child mortality.
By decomposing the concentration index of child mortality, the contributions of covariates from the model were estimated. The modeled contribution is a product of the elasticity of child mortality with respect to a given factor and the degree of inequality in that factor by maternal education. Table 2 showcases the β-coefficient, elasticity, absolute contribution, and percentage contribution of each model covariate to educational inequality in child mortality. According to Equations (1) and (2), a negative sign of the absolute contribution occurs in two scenarios, either when the concentration index of a determinant is negative and the elasticity is positive or when the concentration index of a determinant is positive and the elasticity is negative. The former is true for unimproved water source in all of the time periods except 2005–2006 and for basic sanitation in the periods 1996–2000, 2003–2004, 2005–2006, and 2009–2010. It is also the case for no sanitation in the periods 1986–1992, 1996–2000, 2005–2006, 2009–2010, and 2011–2012. It is also true for household poverty. The latter applies to maternal education and urban residence, as both of them are concentrated at the higher end of the education distribution and have a protective effect against child mortality. Unimproved drinking water sources show the highest contribution to educational inequality in the period 2007–2008 (23.5%). This contribution is also important due to the concentration index value for unimproved drinking water in this period. The percentage value of the contributions of each covariate indicates the total contribution to explained-educational-inequalities decreased on average when the exposures were assumed to be equally distributed across the population, by 11% in the case of improved water sources and 21% in the case of advanced sanitation (Table 3).
Table 2.
Decomposition of the concentration index of under-two mortality in Peru
| 1986–1992 (N = 51,459) | 1996–2000 (N = 135,362) | 2003–2004 (N = 13,286) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | Elasticity | Contribution | % Contribution | β | Elasticity | Contribution | % Contribution | β | Elasticity | Contribution | % Contribution | |
| Unimproved drinking water | −0.02 | −0.64 | 0.16 | −0.71 | 0.13 | 6.99 | −1.58 | 6.20 | No data | |||
| Basic sanitation (non-flush, pit type latrines) | 0.18 | 0.61 | 0.03 | −0.12 | 0.17 | 7.43 | −0.39 | 1.54 | 0.12 | 11.11 | −2.10 | 9.80 |
| No sanitation | 0.41 | 22.21 | −4.09 | 17.77 | 0.34 | 16.32 | −4.72 | 18.54 | −0.29 | −19.28 | 5.92 | −27.64 |
| Maternal age (< 20) | 0.21 | 3.97 | −0.03 | 0.12 | 0.34 | 11.17 | 0.00 | −0.01 | 1.05 | 70.11 | −1.08 | 5.04 |
| Maternal age (> 35) | 0.01 | 0.07 | −0.02 | 0.07 | 0.24 | 2.35 | −0.49 | 1.91 | 0.43 | 7.90 | −1.26 | 5.86 |
| Maternal education (0–17 years) | −0.12 | −50.38 | −22.61 | 98.24 | −0.04 | −32.13 | −14.14 | 55.58 | −0.01 | −21.15 | −8.70 | 40.59 |
| Household poverty (bottom 40% of household wealth distribution) | 0.11 | 4.12 | −1.29 | 5.60 | −0.23 | −13.91 | −0.21 | 0.84 | 0.81 | 112.48 | −33.55 | 156.63 |
| Urbanicity | −0.03 | −1.56 | −0.32 | 1.41 | −0.31 | −21.65 | −5.62 | 22.10 | −0.42 | −57.53 | −17.15 | 80.04 |
| Sex of the child (male) | 0.10 | 4.39 | 0.00 | −0.01 | 0.29 | 20.46 | −0.02 | 0.08 | 0.26 | 36.51 | −0.07 | 0.35 |
| Total model contribution | −28.16 | −27.17 | −57.98 | |||||||||
| Residual contribution | 27.88 | −22.37 | 26.98 | −6.78 | 57.91 | −170.68 | ||||||
| 2005–2006 (N = 27,461) | 2007–2008 (N = 46,868) | 2009–2010 (N = 95,126) | ||||||||||
| β | Elasticity | Contribution | %Contribution | β | Elasticity | Contribution | % Contribution | β | Elasticity | Contribution | % Contribution | |
| Unimproved drinking water | −0.14 | −1.23 | 0.28 | −10.17 | 0.72 | 59.43 | −14.15 | 23.54 | 0.14 | 11.14 | −2.53 | 5.44 |
| Basic sanitation (non-flush, pit type latrines) | 0.33 | 2.89 | −0.53 | 18.81 | 0.00 | −0.59 | 0.11 | −0.18 | 0.18 | 21.23 | −3.99 | 8.58 |
| No sanitation | 0.08 | 0.71 | −0.17 | 6.09 | −0.01 | −0.66 | 0.14 | −0.24 | 0.24 | 16.87 | −3.76 | 8.08 |
| Maternal age (< 20) | −0.04 | −0.31 | 0.00 | −0.14 | 0.61 | 49.16 | −1.51 | 2.51 | 0.29 | 26.28 | −0.95 | 2.04 |
| Maternal age (> 35) | −0.82 | −3.89 | 0.56 | −19.90 | 0.30 | 6.43 | −0.78 | 1.29 | 0.22 | 5.23 | −0.49 | 1.05 |
| Maternal education (0–17 years) | −0.01 | −0.98 | −0.39 | 14.03 | −0.03 | −57.08 | −21.77 | 36.20 | −0.03 | −81.64 | −30.18 | 64.91 |
| Household poverty (bottom 40% of household wealth distribution) | 0.33 | 3.07 | −0.87 | 31.19 | 0.33 | 51.82 | −14.47 | 24.06 | 0.14 | 24.83 | −6.53 | 14.04 |
| Urbanicity | −0.34 | −3.17 | −0.89 | 31.81 | −0.12 | −20.30 | −4.90 | 8.15 | 0.02 | 3.25 | 0.78 | −1.68 |
| Sex of the child (male) | −0.01 | −0.10 | 0.00 | 0.00 | 0.04 | 6.21 | 0.01 | −0.01 | 0.30 | 54.55 | −0.11 | 0.23 |
| Total model contribution | −2.01 | −57.31 | −47.74 | |||||||||
| Residual contribution | 1.86 | 28.29 | 57.12 | 4.69 | 47.62 | −2.71 | ||||||
| 2011–2012 (N = 91,755) | ||||||||||||
| β | Elasticity | Contribution | %Contribution | |||||||||
| Unimproved drinking water | 0.20 | 15.60 | −1.95 | 20.44 | ||||||||
| Basic sanitation (non-flush, pit type latrines) | −0.17 | −21.04 | 2.87 | −30.07 | ||||||||
| No sanitation | 0.27 | 14.58 | −2.06 | 21.63 | ||||||||
| Maternal age (< 20) | 0.38 | 35.21 | −1.39 | 14.57 | ||||||||
| Maternal age (> 35) | 0.09 | 2.17 | −0.02 | 0.22 | ||||||||
| Maternal education (0–17 years) | −0.04 | −90.60 | −18.24 | 191.29 | ||||||||
| Household poverty (bottom 40% of household wealth distribution) | 0.14 | 20.00 | −3.51 | 36.78 | ||||||||
| Urbanicity | −0.29 | −55.06 | −7.90 | 82.92 | ||||||||
| Sex of the child (male) | 0.15 | 27.67 | −0.04 | 0.45 | ||||||||
| Total model contribution | −32.24 | |||||||||||
| Residual contribution | 32.21 | −238.22 | ||||||||||
Table 3.
Percentage change in total explained contribution of educational inequality in child mortality
| 1986–1991–1992 | 1996–2000 | 2003–2004 | 2005–2006 | 2007–2008 | 2009–2010 | 2011–2012 | Average change | |
|---|---|---|---|---|---|---|---|---|
| Equal distribution is assumed (concentration index = 0) | ||||||||
| Water | −1.80 | −5.81 | No data | 14.18 | −24.69 | −5.30 | −6.04 | −4.21 |
| Sanitation | −7.86 | −18.80 | 6.59 | −34.72 | 0.44 | −16.23 | 2.50 | −9.72 |
| Concentration index of water and sanitation is fixed at 1986–1992 levels | ||||||||
| Water | 0 | −4.09 | −6.12 | −1.59 | 1.94 | 0.69 | 6.38 | – |
| Sanitation | 0 | −2.61 | −0.27 | 0.57 | −0.13 | 4.64 | −3.49 | – |
Negative values indicate decrease in total explained contribution to inequality compared with existing levels of the concentration index.
Temporal trends.
As is seen in Figure 1, child mortality in Peru declined over time. Coverage of improved water and sanitation facilities increased with diminishing proportions of the population left without access (Figure 2). By observing the percentage contribution over time, it is seen that the contribution due to water increased up to 2007–2008, declined in the next 2 years, and was high in the final period again, at a value of 20.4%. On the other hand, there is considerable fluctuation in the contribution of sanitation to educational inequality, with the highest value (21.6%) being seen only in the final period, for no sanitation facilities. The contribution of maternal education decreased from a very high value of 93.7% in 1986–1992 to 14% in 2005–2006, after which it increased again consistently till the final period. Both household poverty and urbanicity also show fluctuating contributions over time. Inequalities in the distribution of improved water sources and advanced sanitation were also found to decrease over time. If this decrease had not occurred and inequality in water access stayed the same as in 1986–1992, total educational inequality in 2011–2012 would have been larger by over 17% (see details in Supplemental Information). Similarly, if the distribution of sanitation remained unchanged, total educational inequality in child mortality in 2011–2012 would have been higher by 1%.
Discussion
In this study, we have showed that disparities in both child mortality and WASH access are very pronounced between educational groups in Peru. Decomposition analyses showed that unimproved water and sanitation contributed negatively to children of mothers with less education. All analyses of inequality indicate that adequate sanitation or lack thereof contributes more toward educational inequalities in child mortality. Therefore, this article highlights that investments in water and sanitation programs, particularly targeted to vulnerable populations (i.e., low-education populations), should help reduce socioeconomic inequalities in child mortality in Peru.
The role of water and sanitation in health has been previously studied mainly in the context of interventions designed to improve access37 where diarrhea has been the most widely studied outcome.7,38 This study aimed at measuring inequalities in child mortality in Peru, a country which is projected to be among the worst affected by climate change and depletion of natural water reservoirs.39 Previous studies conducted using data from the Peruvian Ministry of Health also confirm a socioeconomic gradient in child mortality within districts in the country, but these estimates were again limited to the measurement of economic determinants.40 By focusing on an educational distribution, we provide an assessment of health inequality that is not strictly material and highlights the importance of socially and educationally motivated health preferences. The results of this study show that it is important for policy makers to achieve convergence between the disparate efforts targeted at improving education, child health, and access to water and sanitation.
Although Peru is relatively on-track for child mortality reduction,41 socioeconomic inequality42 in the country has remained largely static. Welfare policies in LMICs often take the form of conditional cash transfer programs such as JUNTOS in Peru,43 and are aimed at improving nutrition and immunization coverage and ensuring school attendance and uptake of available healthcare. On the other hand, services for water and sanitation usually fall under infrastructural development and may sometimes lack an explicit focus on child health and mortality.
Limitations.
Some limitations of this study deserve mention. First, we restricted the observation period to between 2 and 5 years before the interview date. Günther and Fink44 have pointed out that a household's access to water and sanitation may change more rapidly, but if birth histories are truncated to a shorter period, the number of deaths counted becomes very small to allow for any meaningful conclusions. Moreover, we hypothesized the translation of mother's education into health behavior which could then protect the child's health due to improved sanitary and hygienic conditions within the household. The use of a single variable, namely mother's level of education does not capture such information. Further studies could investigate other dimensions such as sociopsychological variables (norms, attitude, self-efficacy convictions, etc.) or infrastructural components (water resources available, expenditures on public services, etc.) as determinants of health behaviors and children health.
It would also be useful to have information about social and labor factors that determine an individual woman's education. A distinction for slum dwellers in urban areas would have enabled more detail in the interpretation of inequalities. Information for sources of drinking water was absent for the period 2003–2004 in the DHS data. In the period 1996–2000, the sample of population surveyed was skewed to exclude the very poor, as a result of which very few child deaths were recorded and an anomalous effect of increasing mortality risk with increasing wealth was seen in this period.
Future perspectives.
This study also serves as a foundational effort to guide further research in the joint space of child mortality, maternal education, and WASH access. In Peru, when offspring of the initial JUNTOS beneficiary cohort are evaluated, a view of inequalities in mortality in relation to the educational distribution will be available, along with information about the long-term distributional effects of this program. Although health and inequality have a host of determinants unique to each region, these findings apply to most countries experiencing rapid economic growth, and assessing educational inequalities can help pinpoint areas for equity focused policies, especially in densely populated and growing urban areas.
Conclusion
Although the focus of this study is educational inequalities in child mortality, its purpose is not to detract from the broader context of poverty or even isolate health inequalities due to educational differentials. In fact, we have aimed to provide a view of socioeconomic disparities that encompasses issues such as water and sanitation that have long been dealt with either separately or relegated to the margins of the poverty alleviation debate. Through our findings, we highlight the role played by individual factors and their confluence in determining how the balance of deprivation exposes children of less educated mothers to a higher risk of mortality.
Supplementary Material
Supplemental information, tables, and figures.
Footnotes
Authors' addresses: Tasneem Bohra, Master of Public Health, School of Public Health, Ecole des Hautes Études en Santé Publique (EHESP), Rennes, France, E-mail: turbulent.tas@gmail.com. Tarik Benmarhnia and Britt McKinnon, Institute for Health and Social Policy, McGill University, Montreal, Canada, E-mails: tarik.benmarhnia@mcgill.ca and britt.mckinnon@mcgill.ca. Jay S. Kaufman, Department of Epidemiology, Biostatistics, and Occupational Health, McGill University, Montreal, Canada, and Institute for Health and Social Policy, McGill University, Montreal, Canada, E-mail: jay.kaufman@mcgill.ca.
References
- 1.Wagstaff A. Poverty and health sector inequalities. Bull World Health Organ. 2002;80:97–105. [PMC free article] [PubMed] [Google Scholar]
- 2.Makinen M, Waters HR, Rauch M, Almagambetova N, Bitran R, Gilson L, McIntyre D, Pannarunithai S, Prieto AL, Ubilla G, Ram S. Inequalities in health care use and expenditure: empirical data from eight developing countries and countries in transition. Bull World Health Organ. 2000;78:55–65. [PMC free article] [PubMed] [Google Scholar]
- 3.Gwatkin DR. Health inequalities and the health of the poor. Bull World Health Organ. 2000;78:16. [PMC free article] [PubMed] [Google Scholar]
- 4.Karlsson M, Nilsson T, Lyttkens CH, Leeson G. Income inequality and health: importance of a cross-country perspective. Soc Sci Med. 2010;70:875–885. doi: 10.1016/j.socscimed.2009.10.056. [DOI] [PubMed] [Google Scholar]
- 5.Houweling TA, Kunst AE. Socio-economic inequalities in childhood mortality in low- and middle-income countries: a review of the international evidence. Br Med Bull. 2010;93:7–26. doi: 10.1093/bmb/ldp048. [DOI] [PubMed] [Google Scholar]
- 6.Braveman P, Tarimo E. Social inequalities in health within countries: not only an issue for affluent nations. Soc Sci Med. 2002;54:1621–1635. doi: 10.1016/s0277-9536(01)00331-8. [DOI] [PubMed] [Google Scholar]
- 7.Bhutta ZA, Das JK, Walker N, Rizvi A, Campbell H, Rudan I, Black RE. Interventions to address deaths from childhood pneumonia and diarrhoea equitably: what works and at what cost? Lancet. 2013;381:1417–1429. doi: 10.1016/S0140-6736(13)60648-0. [DOI] [PubMed] [Google Scholar]
- 8.Halvorson SJ, Williams AL, Ba S, Dunkel FV. Water quality and waterborne disease in the Niger River Inland Delta, Mali: a study of local knowledge and response. Health Place. 2011;17:449–457. doi: 10.1016/j.healthplace.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 9.Fuchs R, Pamuk E, Lutz W. Education or wealth: which matters more for reducing child mortality in developing countries? Vienna Yearb Popul Res. 2010;8:175–199. [Google Scholar]
- 10.Chou S-Y, Liu J-T, Grossman M, Joyce T. Parental education and child health: evidence from a natural experiment in Taiwan. Am Econ J Appl Econ. 2010;2:63–91. doi: 10.1257/app.2.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greenaway ES, Leon J, Baker DP. Understanding the association between maternal education and use of health services in Ghana: exploring the role of health knowledge. J Biosoc Sci. 2012;44:733–747. doi: 10.1017/S0021932012000041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.LeVine RA, Rowe ML. Maternal literacy and child health in less-developed countries: evidence, processes, and limitations. J Dev Behav Pediatr. 2009;30:340–349. doi: 10.1097/DBP.0b013e3181b0eeff. [DOI] [PubMed] [Google Scholar]
- 13.Basu AM, Stephenson R. Low levels of maternal education and the proximate determinants of childhood mortality: a little learning is not a dangerous thing. Soc Sci Med. 2005;60:2011–2023. doi: 10.1016/j.socscimed.2004.08.057. [DOI] [PubMed] [Google Scholar]
- 14.Jalan J, Ravallion M. Does piped water reduce diarrhea for children in rural India? J Econom. 2003;112:153–173. [Google Scholar]
- 15.Tucker J, MacDonald A, Coulter L, Calow RC. Household water use, poverty and seasonality: wealth effects, labour constraints, and minimal consumption in Ethiopia. Water Resour Rural Dev. 2014;3:27–47. [Google Scholar]
- 16.Bolaane B, Ikgopoleng H. Towards improved sanitation: constraints and opportunities in accessing waterborne sewerage in major villages of Botswana. Habitat Int. 2011;35:486–493. [Google Scholar]
- 17.Mosley WH, Chen LC. An analytical framework for the study of child survival in developing countries. 1984. Bull World Health Organ. 2003;81:140–145. [PMC free article] [PubMed] [Google Scholar]
- 18.Walsh B, Cullinan J. Decomposing socioeconomic inequalities in childhood obesity: evidence from Ireland. Econ Hum Biol. 2015;16:60–72. doi: 10.1016/j.ehb.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 19.Christiani Y, Byles J, Tavener M, Dugdale P. Socioeconomic related inequality in depression among young and middle-adult women in Indonesia's major cities. J Affect Disord. 2015;182:76–81. doi: 10.1016/j.jad.2015.04.042. [DOI] [PubMed] [Google Scholar]
- 20.Doherty E, Walsh B, O'Neill C. Decomposing socioeconomic inequality in child vaccination: results from Ireland. Vaccine. 2014;32:3438–3444. doi: 10.1016/j.vaccine.2014.03.084. [DOI] [PubMed] [Google Scholar]
- 21.Abu-Zaineh M, Mataria A, Moatti J-P, Ventelou B. Measuring and decomposing socioeconomic inequality in healthcare delivery: a microsimulation approach with application to the Palestinian conflict-affected fragile setting. Soc Sci Med. 2011;72:133–141. doi: 10.1016/j.socscimed.2010.10.018. [DOI] [PubMed] [Google Scholar]
- 22.Solmi F, Von Wagner C, Kobayashi LC, Raine R, Wardle J, Morris S. Decomposing socio-economic inequality in colorectal cancer screening uptake in England. Soc Sci Med. 2015;134:76–86. doi: 10.1016/j.socscimed.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 23.Rama M, Li Y, Mitra PK, Newman JL. Addressing Inequality in South Asia. Washington, DC: The World Bank; 2015. p. 197. [Google Scholar]
- 24.United Nations Organization . The Millennium Development Goals Report 2014. New York, NY: United Nations Organization; 2014. [Google Scholar]
- 25.Urke HB, Bull T, Mittelmark MB. Socioeconomic status and chronic child malnutrition: wealth and maternal education matter more in the Peruvian Andes than nationally. Nutr Res. 2011;31:741–747. doi: 10.1016/j.nutres.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 26.Peru Support Group . The Great Water Debate: Cause and Effect in Peru. London, United Kingdom: Peru Support Group; 2008. [Google Scholar]
- 27.Ioris AAR. The geography of multiple scarcities: urban development and water problems in Lima, Peru. Geoforum. 2012;43:612–622. [Google Scholar]
- 28.Checkley W, Gilman RH, Black RE, Epstein LD, Cabrera L, Sterling CR, Moulton LH. Effect of water and sanitation on childhood health in a poor Peruvian peri-urban community. Lancet. 2004;363:112–118. doi: 10.1016/S0140-6736(03)15261-0. [DOI] [PubMed] [Google Scholar]
- 29.Fink G, Günther I, Hill K. The effect of water and sanitation on child health: evidence from the demographic and health surveys 1986–2007. Int J Epidemiol. 2011;40:1196–1204. doi: 10.1093/ije/dyr102. [DOI] [PubMed] [Google Scholar]
- 30.Hill K, Amouzou A. Chapter 3: Trends in child mortality, 1960 to 2000. In: Jamison DT, Feachem RG, Makgoba MW, Bos ER, Baingana FK, Hofman KJ, Rogo KO, editors. Disease and Mortality in Sub-Saharan Africa. 2nd edition. Washington, DC: World Bank; 2006. pp. 15–30. [PubMed] [Google Scholar]
- 31.Pradhan J, Arokiasamy P. Socio-economic inequalities in child survival in India: a decomposition analysis. Health Policy. 2010;98:114–120. doi: 10.1016/j.healthpol.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization (WHO) and United Nations Children's Emergency Fund (UNICEF) Progress on Drinking Water and Sanitation. Geneva, Switzerland: WHO and UNICEF; 2014. [Google Scholar]
- 33.Traissac P, Martin-Prevel Y. Alternatives to principal components analysis to derive asset-based indices to measure socio-economic position in low- and middle-income countries: the case for multiple correspondence analysis. Int J Epidemiol. 2012;41:1207–1210. doi: 10.1093/ije/dys122. [DOI] [PubMed] [Google Scholar]
- 34.Balk D, Pullum T, Storeygard A, Greenwell F, Neuman M. Spatial Analysis of Childhood Mortality in West Africa. Calverton, MD: ORC Macro; 2003. [Google Scholar]
- 35.O'Donnell O, Van Doorslaer E, Wagstaff A, Lindelow M. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation. 1st edition. Washington, DC: The Word Bank; 2008. [Google Scholar]
- 36.Morasae EK, Forouzan AS, Majdzadeh R, Asadi-Lari M, Noorbala AA, Hosseinpoor AR. Understanding determinants of socioeconomic inequality in mental health in Iran's capital, Tehran: a concentration index decomposition approach. Int J Equity Health. 2012;11:18. doi: 10.1186/1475-9276-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Freeman MC, Clasen T, Dreibelbis R, Saboori S, Greene LE, Brumback B, Muga R, Rheingans R. The impact of a school-based water supply and treatment, hygiene, and sanitation programme on pupil diarrhoea: a cluster-randomized trial. Epidemiol Infect. 2014;142:340–351. doi: 10.1017/S0950268813001118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis. 2005;5:42–52. doi: 10.1016/S1473-3099(04)01253-8. [DOI] [PubMed] [Google Scholar]
- 39.Stark J, Guillén S, Brady C. Follow the Water: Emerging Issues of Climate Change and Conflict in Peru. Lima, Peru: U.S. Agency for International Development; 2012. p. 5. [Google Scholar]
- 40.Huicho L, Trelles M, Gonzales F. National and sub-national under-five mortality profiles in Peru: a basis for informed policy decisions. BMC Public Health. 2006;6:173. doi: 10.1186/1471-2458-6-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.United Nations Children's Emergency Fund (UNICEF) The State of the World's Children 2009: Maternal and Newborn Health. New York, NY: UNICEF; 2009. [Google Scholar]
- 42.Muñoz I, Paredes M, Thorp R. Group inequalities and the nature and power of collective action: case studies from Peru. World Dev. 2007;35:1929–1946. [Google Scholar]
- 43.Perova E, Vakis R. 5 years in Juntos: new evidence on the program's short and long-term impacts. Economía. 2012;35:53–82. [Google Scholar]
- 44.Günther I, Fink G. Water, Sanitation and Children's Health Evidence from 172 DHS Surveys. Zurich, Switzerland: Prospects Group; 2010. World Bank Policy Research Paper 5275. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental information, tables, and figures.