Abstract
Purpose
Previous research describing how informal cancer caregiving impacts employment has been conducted in small samples or a single disease site. This paper provides population-based estimates of the effect of cancer caregiving on employment and characterizes the employment changes made by caregivers.
Methods
The sample comprised cancer survivors with a friend or family caregiver, participating in either the Medical Expenditure Panel Survey Experiences with Cancer Survivorship Survey (ECSS) (n=458) or the LIVESTRONG 2012 Survey for People Affected by Cancer (SPAC) (n=4,706). Descriptive statistics characterized the sample of survivors and their caregivers’ employment changes. Multivariable logistic regression identified predictors of caregivers’ extended employment changes, comprising time off and changes to hours, duties or employment status.
Results
Among survivors with an informal caregiver, 25% from the ECSS and 29% from the SPAC reported their caregivers made extended employment changes. Approximately 8% of survivors had caregivers who took time off from work lasting ≥ 2 months. Caregivers who made extended employment changes were more likely to care for survivors treated with chemotherapy or transplant; closer to diagnosis or end of treatment; who experienced functional limitations; and made work changes due to cancer themselves compared to caregivers who did not make extended employment changes.
Conclusions
Many informal cancer caregivers make employment changes to provide care during survivors’ treatment and recovery.
Implications for cancer survivors
This study describes cancer caregiving in a prevalent sample of cancer survivors, thereby reflecting the experiences of individuals with many different cancer types and places in the cancer treatment trajectory.
Keywords: neoplasms, caregivers, employment, cost-of-illness, quality of life
BACKGROUND
The number of cancer survivors who have been diagnosed with cancer at any time in the past has increased over 400% since the mid-1970s, reaching 14.5 million in 2014 [1]. During this period, cancer treatment has evolved as more effective therapies have been developed and the administration of those therapies has shifted to the outpatient setting [2]. The growing use of oral cancer agents represents another major change in cancer care delivery [3, 4]. Because oral cancer agents are self-administered outside of the health care setting, cancer survivors are responsible for adhering to sometimes complicated treatment regimens.
Cancer survivors rely on their family and friends during treatment, recovery, and beyond as they manage their care and any late or lasting effects of treatment [5, 6]. According to the National Caregiving Alliance, approximately 7% of all unpaid caregivers in the past 12 months cited cancer as the main reason that they were providing care [7]. Cancer survivors’ need for informal caregiver support (i.e., support from family and friends) will fluctuate in response to the demands of cancer treatment and with the severity of their disease [8, 9]. Throughout the course of treatment and beyond, the scope of tasks that informal caregivers are called upon to provide are diverse and include direct care, help with household tasks, transportation to and from medical appointments, and emotional support [5, 10]. The time demands of cancer caregiving can be substantial [8]. A range of issues have been reported by informal cancer caregivers, including psychosocial and emotional problems, physical health problems, and decreased quality of life [5, 11, 9, 12]. For individuals who are employed, the time spent providing care can impel caregivers to take time off from work, which can lead to lost wages and financial hardship [12-15].
Although research has begun to explore the impact of informal cancer caregiving on employment, most studies to date have been conducted in small samples or in a single disease site [13, 16, 17, 10, 11, 18], thus, limiting our understanding of the extent to which cancer caregiving impacts employment outcomes. To address these gaps, the current paper analyzes data from two surveys, the 2011 Medical Expenditure Panel Survey (MEPS) Experiences with Cancer Survivorship Survey (ECSS), a nationally representative sample of cancer survivors; and the LIVESTRONG 2012 Survey for People Affected by Cancer (SPAC), a large internet-based non-probability sample of cancer survivors. Because both surveys were conducted in a prevalent sample of cancer survivors, the current study reflects the experiences of survivors with many different cancer types and places in the cancer treatment trajectory.
MATERIALS AND METHODS
Data sources
ECSS
The MEPS is a nationally representative sample of the United States civilian non-institutionalized population. The MEPS ECSS was administered to adult cancer survivors in 2011 and included questions about economic burden and informal cancer caregiving. Participants were identified for the supplement if they responded “yes” to the MEPS question, “Have you ever been told by a doctor or other health professional that you had cancer or a malignancy of any kind?” The response rate for the core MEPS in 2011 was 54.9% and the response rate for the Experiences with Cancer Survey was 90.0%, yielding an overall response rate of 49.4%. Analyses were based on a sample of 458 cancer survivors who reported having an informal caregiver. Detailed information about the development and methodology of the MEPS and the ECSS can be found elsewhere [19, 20].
SPAC
The LIVESTRONG Foundation fielded questions from the ECSS to self-selected cancer survivors as part of the 2012 SPAC. More information about the survey can be found on the LIVESTRONG Foundation's website (http://www.livestrong.org/what-we-do/our-approach/livestrong-research-library/livestrong-surveys/). Although based on a non-probability sample, raking (a post-stratification approach for adjusting survey sample weights) was conducted so the survey estimates using these weights equaled the estimated population totals derived from the ECSS sample for each key characteristic including age, sex, race/ethnicity and region, so the population distribution of these key characteristics would look the same in the two samples [21]. Analyses were based on a sample of 4,706 cancer survivors who reported having an informal caregiver.
Study Measures and Sources
The study measures and corresponding sources are described below. When an item was assessed in both surveys, the measures were identical, except where otherwise noted.
Questions analyzed from both the ESCC and the SPAC
Cancer survivor characteristics
Data were collected on survivors’ current age, sex, education, race/ethnicity and marital status. Respondents from the SPAC were asked whether they were married or had a domestic partner, whereas respondents from the ECSS were asked whether they were married. Information was collected on participants’ cancer site, years since diagnosis, and years since the end of treatment. Survivors’ employment changes were assessed with the question, “at any time since your first cancer diagnosis, did you take extended paid time off from work, unpaid time off, or make a change in your hours, duties or employment status. Whether cancer limited survivors’ outside activities or their ability to perform mental tasks was also captured. Survivors were asked to think about the time when they were diagnosed with cancer to the present. Survivors with more than one type of cancer were asked to think about their experiences across all of them. When that was not possible, survivors were asked to think about the most severe, followed by the most recent.
Informal caregiving
Cancer survivors were asked about the presence of an informal caregiver with the question, “Since the time you were first diagnosed with cancer, has any friend or family member provided care to you during or after your cancer treatment?”
Extended employment changes among caregivers
Survivors who reported that they had a caregiver were asked, “Because of your cancer, its treatment, or the lasting effects of that treatment, did any of your caregivers ever take extended paid time off from work, unpaid time off, or make a change in their hours, duties or employment status?” Hereafter, “yes” responses to this question are referred to as making extended employment changes.
Questions analyzed from the SPAC
Source of informal care (SPAC)
Survivors were asked which friends and/or family members provided them with care. Responses included: parent(s), brother/sister, child(ren), spouse/partner, friend(s), extended family members and other. Survivors could identify more than one caregiver.
Types of employment changes among caregivers (SPAC)
Survivors reporting that their caregivers made extended employment changes were asked whether the caregivers took paid or unpaid leave and the duration of paid and unpaid leave. Survivors were also asked whether their caregivers made changes to their work schedule, changed their job duties, retired early, delayed retirement, or made “other” changes to their work arrangement.
Analyses
Descriptive statistics were used to characterize the sample, the proportion of cancer survivors whose caregivers made extended employment changes and the types of employment changes they made. For the 1,189 survivors who responded that their caregiver made “other” changes to their work arrangement and who provided a written description, text responses were independently coded by two of the co-authors (ED and JR) and categorized as: 1) modified schedule, work load, and job responsibilities, 2) took time off, 3) lost opportunities (e.g., quit, delayed looking for work, refused promotion), or 4) other. Inter-rater reliability was measured using Cohen's kappa, and agreement between the two raters was high (κ = 0.903). Separate multivariable logistic regression models were used to identify predictors of caregivers’ extended employment changes and Wald F tests were used to identify differences between survivors whose caregivers made extended employment changes and survivors whose caregivers did not make extended employment changes. The model for cancer site included age group, race, and marital status. All other models adjusted for gender, age group, race, and marital status. Individuals reporting a diagnosis of only non-melanoma skin cancer were excluded from all analyses, as has been done in other studies [22, 23]. All analyses were conducted in SUDAAN and estimates were weighted to account for the complex survey design of the ECSS and the raked weights that were applied to the SPAC [21].
RESULTS
Presence of a caregiver
Thirty-seven percent (n=458) of cancer survivors in the ECSS reported having an informal caregiver, representing approximately 6.1 million people in the population, whereas 84% (n=4,706) of cancer survivors in the SPAC reported having an informal caregiver. Across both surveys, the majority of survivors who reported having a caregiver were older than age 65, female, white, married, with education of some college or more, and ≥2 years post-diagnosis (Table 1). However, survivors in the ECSS tended to be older, less educated, female, unmarried, further from diagnosis and the end of treatment and made no work changes due to cancer as compared to survivors in the SPAC.
Table 1.
Characteristics of cancer survivors who received informal care in conjunction with cancer treatment or the late and lasting effects of treatment (ECSS and SPAC).
| Received informal care during or after cancer treatment1 | ||||
|---|---|---|---|---|
| Experiences with Cancer Survivorship Survey (ECSS) (n=458) | Survey for People Affected by Cancer (SPAC) (n=4,706) | |||
| N | % | N | % | |
| Current age | ||||
| 18-54 | 115 | 23.8 | 2,664 | 27.9 |
| 55-64 | 116 | 24.1 | 1,379 | 22.3 |
| 65+ | 227 | 52.1 | 662 | 49.7 |
| Sex | ||||
| Male | 157 | 35.2 | 1,524 | 40.9 |
| Female | 301 | 64.8 | 3,157 | 58.7 |
| Education | ||||
| High school graduate or less | 228 | 40.0 | 346 | 7.9 |
| Some college or more | 229 | 59.9 | 4,318 | 91.2 |
| Race/ethnicity | ||||
| White | 369 | 89.8 | 4,288 | 90.7 |
| Black | 69 | 7.7 | 94 | 3.1 |
| Other | 20 | 2.5 | 284 | 5.2 |
| Marital status2 | ||||
| Married and female | 142 | 34.0 | 2,162 | 38.3 |
| Married and male | 107 | 25.4 | 1,168 | 32.5 |
| Not married and female | 159 | 30.7 | 962 | 19.7 |
| Not married and male | 50 | 9.8 | 346 | 8.0 |
| Cancer site | ||||
| Breast | 123 | 25.1 | 1,442 | 27.4 |
| Prostate | 48 | 10.8 | 238 | 10.0 |
| Colorectal | 32 | 6.8 | 304 | 6.7 |
| Multiple | 48 | 10.4 | 516 | 14.7 |
| Other single cancers | 207 | 46.9 | 2,206 | 41.2 |
| Years from first cancer diagnosis | ||||
| <2 | 52 | 12.5 | 983 | 18.5 |
| 2-5 | 133 | 28.4 | 1,834 | 34.7 |
| 6-10 | 89 | 17.5 | 986 | 22.4 |
| 11+ | 159 | 37.6 | 902 | 24.3 |
| Years from last treatment | ||||
| <1 | 140 | 32.0 | 1,332 | 29.3 |
| 1-2 | 53 | 10.2 | 1,288 | 25.0 |
| 3-4 | 36 | 7.8 | 649 | 13.0 |
| 5+ | 195 | 44.5 | 1,326 | 29.4 |
| Never treated/missing | 34 | 5.5 | 111 | 3.3 |
| Made work changes due to cancer | ||||
| Yes | 197 | 43.3 | 3,213 | 57.8 |
| No | 254 | 55.9 | 1,459 | 41.4 |
Note: Weighted percentages may not equal 100% due to missing data.
The presence of an informal caregiver was assessed with the question, “Since the time you were first diagnosed with cancer, has any friend or family member provided care to you during or after your cancer treatment?”
Respondents to the SPAC were asked whether they were married or had a domestic partner, whereas respondents to the ECSS were asked whether they were married.
Note: Estimates were weighted to account for the complex survey design of ECSS and the raked weights that were applied to the SPAC.
Over 75% of SPAC survivors reported that their spouse or partner served as their informal caregiver (data not shown). Additionally, SPAC survivors reported that friend(s) (48%), child(ren) (40%), siblings (28%), parent(s)(23%), extended family member (11%) or other individual (7%) provided informal care.
Extended employment changes
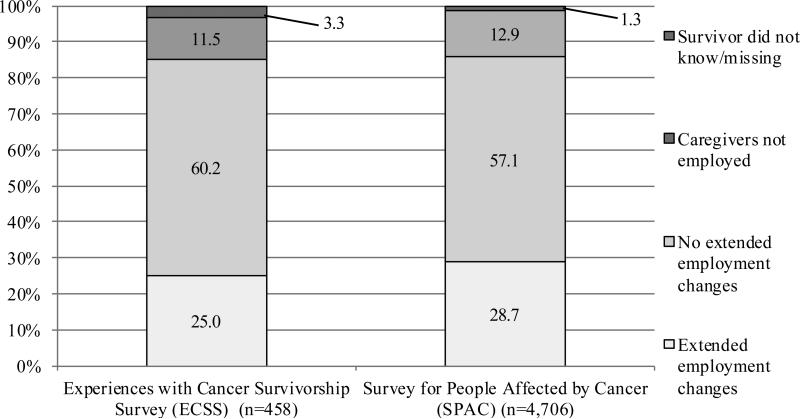
Of survivors who had a caregiver, 25% (n=120) from the ECSS reported that their caregiver made extended employment changes (Figure 1). This finding represents approximately 1.5 million people in the population. Approximately 60% of survivors in the ECSS reported that their caregivers did not make extended employment changes and 12% reported that their caregivers were not employed. Likewise, 29% (n=1,677) of survivors from the SPAC reported that their caregivers made extended employment changes (Figure 1). Approximately 57% of the survivors in the SPAC reported that their caregivers did not make extended employment changes and 13% reported that their caregivers were not employed.
Figure 1.
Proportion of informal caregivers who made extended employment changes (ECSS and SPAC) 1
1 Extended employment changes were assessed with the question, “because of your cancer, its treatment, or the lasting effects of that treatment, did any of your caregivers ever take extended paid time off from work, unpaid time off, or make a change in their hours, duties or employment status?”
Note: Estimates were weighted to account for the complex survey design of the ECSS and the raked weights that were applied to the SPAC.
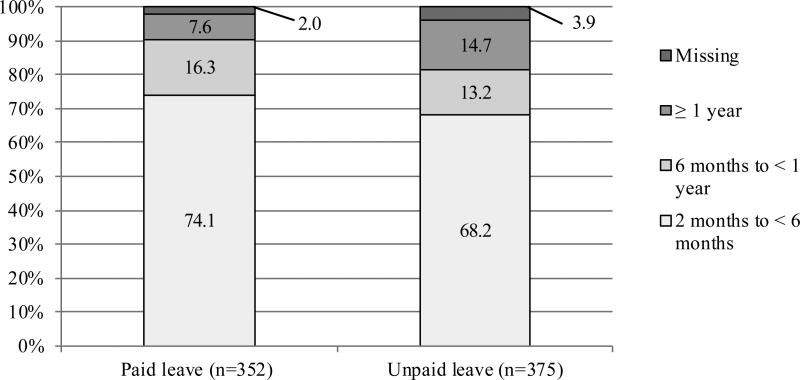
Types of employment changes
Eight percent of SPAC survivors reported that their caregivers took time off from work lasting two months or longer, consisting of paid leave (2.1%), unpaid leave (2.8%) or a combination of the two (3.2%) (Table 2). Of the 352 SPAC survivors who reported that their caregivers took paid time off from work, 74.1% took leave lasting 2 months to < 6 months and 16.3% took leave lasting 6 months to < 1 year (Figure 2). Of the 375 SPAC survivors who took unpaid time off from work, 68.2% took leave lasting 2 months to < 6 months and 13.2% took leave lasting 6 months to < 1 year (Figure 2). A small percentage of caregivers changed from working full time to part time, changed to a less demanding job or altered their retirement plans (Table 2). In addition, among the 21.2% (n=1,239) of SPAC survivors who reported that their informal caregivers made “other” employment changes, an analysis of written text responses suggested that 38.9% of the caregivers made adjustments to their work schedule, work load, and/or job responsibilities, 32.9% took time off from work lasting less than two months or on an episodic basis, 12.2% experienced lost work opportunities such as losing a job, changing jobs, delaying looking for work or not taking a promotion, and 8.6% made other changes.
Table 2.
Types of employment changes made by caregivers (SPAC) (n=4,706)1
| N | %2 | |
|---|---|---|
| Caregivers took extended leave from work for ≥ 2 months3 | ||
| Paid leave only | 147 | 2.1 |
| Unpaid leave only | 168 | 2.8 |
| Both paid and unpaid leave | 204 | 3.2 |
| No extended leave | 4,122 | 90.4 |
| Caregiver changed from working full time to part time | 132 | 2.5 |
| Caregiver changed to a less demanding job | 138 | 2.4 |
| Caregiver retired early | 96 | 2.1 |
| Caregiver delayed retirement | 182 | 3.6 |
| Caregiver made other type of work arrangement | 1,239 | 21.2 |
Survivors reporting that their caregivers made extended employment changes for at least two months were asked whether the caregivers took paid or unpaid time off from work. Survivors were also asked whether their caregivers made changes to their work schedule, changed their job duties, retired early, delayed retirement, or made “other” changes to their work arrangement.
Percentages may not sum to 100 due to missing data.
Four people could not be grouped into one of the categories of extended leave: 1 person who reported that his/her caregiver(s) took extended paid time off work but had a missing response for whether the caregiver(s) took extended unpaid time off work and 3 people who reported that their caregivers took extended unpaid time off work but had a missing response for whether the caregivers took extended paid time off work.
Note: Estimates were weighted to account for the raked weights applied to the Survey for People Affected by Cancer (SPAC).
Figure 2.
Proportion of caregivers who took extended time off from work for ≥ 2 months by duration of leave (SPAC)1
1 Survivors reporting that their caregivers made extended employment changes for at least two months were asked whether their caregivers took paid or unpaid time off from work. Survivors who reported that their caregiver took paid or unpaid time off from work were asked about the duration of paid and unpaid leave, respectively.
Note: Estimates were weighted to account for the raked weights that were applied to the Survey for People Affected by Cancer (SPAC).
Predictors of Extended Employment Changes among Informal Caregivers
SPAC survivors whose caregivers took extended paid or unpaid leave from work, or made a change in their hours, duties or employment status differed from survivors whose caregivers did not make extended employment changes (Table 3). SPAC survivors whose caregivers made extended employment changes were more likely to have been treated with chemotherapy or bone marrow / peripheral blood stem cell transplant and less likely to have been treated with surgery. They were also more likely to be fewer years from diagnosis and their last cancer treatment. Finally, survivors whose caregivers made extended employment changes were more likely to report functional limitations (i.e., cancer limited their outside activities and ability to perform mental tasks) compared to survivors whose caregivers did not make extended employment changes. These survivors were also more likely to have made work changes due to cancer themselves.
Table 3.
Survivors’ characteristics as predictors of caregivers’ extended employment changes (SPAC)
| Caregiver made extended employment changes (n=1,677) | Caregiver made no extended employment changes (n=2,572) | ||||||
|---|---|---|---|---|---|---|---|
| n | Unadjusted %1 | Adjusted %2 | n | Unadjusted %1 | Adjusted %2 | p-value5 | |
| Cancer site | |||||||
| Breast | 465 | 24.0 | 23.5 | 840 | 30.1 | 30.4 | <.001 |
| Prostate | 40 | 6.3 | 6.8 | 158 | 11.4 | 11.0 | |
| Colorectal | 120 | 8.3 | 8.1 | 147 | 5.9 | 6.0 | |
| Hematologic3 | 246 | 12.8 | 12.6 | 288 | 10.4 | 10.5 | |
| Other single cancers | 591 | 35.1 | 34.4 | 841 | 27.6 | 28.0 | |
| Multiple cancers | 180 | 13.5 | 14.5 | 257 | 14.6 | 14.1 | |
| Cancer treatment4 | |||||||
| Chemotherapy | 1,231 | 74.1 | 72.9 | 1,520 | 54.5 | 55.3 | <.001 |
| Radiation | 819 | 51.4 | 50.3 | 1,289 | 48.4 | 48.9 | .585 |
| Surgery | 1,229 | 69.5 | 68.4 | 1,975 | 75.3 | 75.8 | .002 |
| Bone Marrow or peripheral blood stem cell transplant | 113 | 7.2 | 7.5 | 67 | 2.9 | 2.9 | <.001 |
| Other | 518 | 32.1 | 31.8 | 760 | 29.1 | 29.3 | .299 |
| Years from diagnosis | |||||||
| 0-2 | 665 | 37.5 | 36.2 | 760 | 26.1 | 26.7 | <.001 |
| 3-5 | 426 | 23.2 | 22.5 | 639 | 22.3 | 22.8 | |
| 6-10 | 303 | 19.6 | 20.4 | 570 | 24.6 | 24.2 | |
| >10 | 240 | 19.6 | 20.9 | 552 | 27.0 | 26.2 | |
| Years from last treatment | |||||||
| <1 | 535 | 36.5 | 37.2 | 632 | 25.7 | 25.4 | <.001 |
| 1-2 | 482 | 27.2 | 26.7 | 660 | 25.5 | 25.7 | |
| 3-4 | 206 | 12.7 | 12.4 | 370 | 13.8 | 14.0 | |
| 5-9 | 243 | 13.4 | 13.4 | 475 | 20.2 | 20.1 | |
| ≥10 | 139 | 10.2 | 10.3 | 326 | 14.8 | 14.7 | |
| Cancer limited survivor's outside activities | |||||||
| Yes | 1,491 | 89.8 | 89.2 | 1,926 | 71.3 | 71.9 | <.001 |
| No | 137 | 10.2 | 10.8 | 588 | 28.7 | 28.1 | |
| Cancer interfered with survivor's ability to perform mental tasks | |||||||
| Yes | 1,124 | 62.1 | 59.6 | 1,305 | 41.4 | 42.7 | <.001 |
| No | 510 | 37.9 | 40.4 | 1,207 | 58.6 | 57.3 | |
| Survivor made work changes due to cancer | |||||||
| Yes | 1,237 | 70.5 | 68.3 | 1,658 | 56.2 | 57.4 | <.001 |
| No | 390 | 29.5 | 31.7 | 843 | 43.8 | 42.6 | |
Estimates were weighted to account for the raked weights applied to the SPAC.
The multivariable model for cancer site adjusted for age group, race, and marital status. All other multivariate models adjusted for gender, age group, race, and marital status.
Hematologic cancers include: leukemia, Hodgkin lymphoma, non-Hodgkin lymphoma, and other hematologic.
In the models of cancer treatment, the receipt of each treatment type (yes/no) was analyzed separately and compared between survivors whose caregiver made extended employment changes and survivors whose caregiver did not make extended employment changes.
p-values were calculated from the adjusted analyses
DISCUSSION
Although research has begun to characterize some of the challenges faced by informal caregivers, few studies have examined the impact on employment among informal caregivers of cancer survivors. Further, what we know about the economic impact of cancer caregiving is largely based on small studies conducted in a single-disease site, which may not be representative of the larger population of cancer survivors. In the current study, approximately one quarter of survivors reported that their caregivers made extended employment changes. Based on data from the ECSS, this represents approximately 1.5 million people in the population. In the SPAC, spouses or partners were most frequently cited as caregivers followed by friends and children. The ECSS did not include information about the source of informal caregiving. However, results from the SPAC are consistent with the larger caregiving literature, which has found that most caregivers of cancer survivors are spouses [9, 8]. An analysis of written responses, provided by the 21.2% of survivors who reported that their caregivers made “other” work changes, revealed that caregivers made a broad array of changes to their schedules, job responsibilities and in some cases their careers in order to transport the survivor to and from their medical appointments and provide care during recovery. These findings are consistent with previous research reporting that cancer caregivers miss work, work fewer hours, or make career changes as a result of their caregiving responsibilities [13, 12, 14, 24, 15]. Furthermore, research suggests that the level of work impairment among cancer caregivers is greater than among the general population [25].
In this study, survivors participating in the SPAC were much more likely to report having a caregiver than survivors participating in the ECSS (84% vs. 37%), possibly due to the convenience sample and differences among respondents with respect to age, gender, education, marital status, time since diagnosis and treatment, and level of impairment. Differences in age, sex, race/ethnicity and region between the ECSS and SPAC samples were minimized by weighting. However, it is probable that other differences between the samples contributed to the large discrepancies in reports of informal care. For example, survivors in the SPAC were closer to diagnosis and may have better recall of informal caregiving. Further, at the time of the survey, survivors in the SPAC were more likely to be married. Given that most caregivers are spouses, survivors in the SPAC may have had greater opportunity for having a caregiver. Finally, survivors in the SPAC were more likely to make work changes due to cancer, suggesting that they may have been more limited as a result of their cancer and by extension may have had a greater need for a caregiver.
The current study suggests that approximately 8% of SPAC survivors had caregivers who took 2 or more months of paid or unpaid time off from work. The cost of informal cancer caregiving is substantial [12, 24, 26]. Previous research estimated that the total value of informal cancer caregiving in the first two years after diagnosis is approximately $47,710 [8]. However, estimates varied by cancer site and stage at diagnosis [8]. Other studies estimating the opportunity cost of informal caregiving have employed different methodologies and assumptions, making it difficult to directly compare their results [27, 10, 9]. However, collectively these studies suggest that the opportunity cost of providing informal cancer care is substantial and should be considered in evaluations of the costs associated with treatment and in efforts to quantify the economic burden of cancer.
SPAC survivors whose caregivers made extended employment changes differed from SPAC survivors whose caregivers did not make extended employment changes in terms of their treatment, time since diagnosis and the end of treatment, functional limitations, and work disability due to cancer. Previous research supports these findings that the burden of caregiving differs by the survivor's disease severity and phase of treatment. For example, time spent caregiving and the associated economic burden are greatest in the acute treatment phase of care and at the end of life [10, 11, 27]. The economic burden of informal cancer caregiving is also higher for patients with more advanced disease [9, 8].
Existing policies governing leave from work could mitigate some of the burden of cancer caregiving. For example, the Family and Medical Leave Act (FMLA) allows eligible employees to take up to 12 weeks of unpaid, job-protected leave in a 12 month period for certain family and medical reasons with continuation of group health insurance coverage [28]. However, not all employers and employees are covered under the law and leave is unpaid, which may limit uptake among lower income populations. The current study suggests that approximately a quarter of caregivers (25% from ECSS and 29% SPACC) make employment changes that include taking paid and unpaid leave from their jobs and 8% of SPAC survivors reported that their caregivers took leave from work lasting ≥ 2 months. Although it is probable that some of the caregivers in our sample were covered by the FMLA, we do not have data about which caregivers were covered and whether access to FMLA benefits influenced decisions about taking time off.
In contrast to FMLA, paid sick leave provides a way for employed caregivers to take time off from work without a loss of income. Nevertheless, sick leave does not always apply to the care of sick family members. At present, the proportion of workers employed outside the federal government with paid sick leave is only 65% [29]. Paid sick leave is less common in certain industries (e.g., service) and only 26% of part time workers and 34% of those in the lowest 25% of wages for their occupation have paid-sick leave at their job [29]. However, it is unknown whether sick leave policies that cover the care of sick family members differ across industries and occupation. Approximately 6% of SPAC survivors reported that their caregivers took unpaid time off or a mix of paid and unpaid time off for at least two months, suggesting limited access to paid sick leave that could be used to care for a family member. Taking unpaid leave is financially undesirable for many individuals. Further, when taken outside the context of FMLA, unpaid leave may have negative repercussions, such as earning a poor performance evaluation or being fired. Thus, policies to expand the availability of sick leave that could be used to care for a sick family member could benefit working adults who are also caregivers. Additionally, leave-banking or leave-sharing programs, where employees may donate accrued leave either to an employer managed “leave bank” or directly to another employee could make it possible for a caregiver to take extended time off from work while still being paid [30, 31].
Strategies to mitigate the impact of cancer and other chronic illness on patients and their caregivers could also occur in the workplace. Opportunities for flexible work schedules, alternative work arrangements, job-sharing, and telecommuting could each make it easier for someone to arrange their work life such that they can fulfill both their employee and caregiver responsibilities [32]. The current study suggests that caregivers’ make a range of modifications to their work lives to fulfill their caregiving responsibilities, including taking time off, modifying their schedule and/or job responsibilities, and changing jobs completely. Thus, a range of workplace accommodations may be useful to address different caregiving situations. There is a dearth of intervention research conducted with cancer caregivers, and additional work is needed to explore the types of workplace accommodations that are most effective.
Finally, solutions could occur at the level of health care systems. Providers and other hospital or clinic staff can help caregivers by regularly assessing caregiver needs and connecting caregivers to available community resources [32]. The Veterans Administration has launched a suite of services to support the caregivers of veterans, which could be a model for addressing the needs of cancer caregivers [33]. These supports include peer support, home-based care, including homemaker and home health aide services, and respite care as well as financial assistance in certain cases. In the current study, survivors treated with chemotherapy or transplant, who were closer to diagnosis and the end of treatment and who experienced the greatest functional limitations, operationalized as being limited outside activities, limited in the ability to perform mental tasks, and made work changes themselves, were more likely to have a caregiver who also made extended employment changes. It is particularly important to identify caregivers who are at greatest risk for making extended work changes and to tailor interventions and services accordingly.
Limitations
This study had some limitations. The number of cancer survivors in the ECSS was relatively small, which prevented an in-depth analysis of cancer caregiving. Data on caregivers’ extended employment changes were reported by the cancer survivor. It is possible that the survivors were not fully aware of the extent of employment changes made by their caregivers and either under- or overestimated the employment effects experienced by their caregivers. Neither survey collected detailed demographic or specific employment information about the caregivers, so we are unable to assess how economic impact differs by characteristics of the caregiver. Most participants with a cancer history in the ECSS and SPAC were long-term cancer survivors, so it was not possible to explore issues in newly diagnosed cancers or cancers with short survival. Thus this study may underestimate the impact of caregiving, which tends to be greatest during treatment and at the end of life [34]. Additionally, 91% of SPAC respondents had at least some college education, so the analyses based on SPAC items alone may not be representative of cancer survivors with lower education. This study focused on informal caregiving. However, we did not have data on the availability of formal, paid caregivers which could influence survivors need for informal care. Finally, survivors were asked about employment changes made by caregivers at any point following their diagnosis, so we do not know the timing of these changes or if they fully estimated the ongoing, though more limited caregiving (e.g., transportation), that occurred post-recovery.
Conclusions
Despite these limitations, this paper provides population-based estimates of impact on employment of informal cancer caregiving based on nationally representative data from the ECSS and an assessment of employment changes among informal caregivers from the SPAC, a large convenience sample of cancer survivors. As more cancer treatments are delivered orally or on an outpatient basis or to a growing population of older adults who are also managing other chronic conditions, the demand for caregivers is expected to increase. Given the rising prevalence of cancer and its impact not only on survivors’ but also caregivers’ ability to work [35, 36], the economic burden of cancer will substantially increase. Additional research is needed to fully understand and address the needs of informal cancer caregivers and to evaluate the impact of potential solutions to mitigate the impact of caregiving on employment.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Cancer Institute, the Centers for Disease Control and Prevention, or the American Cancer Society.
The authors have no conflicts of interest to disclose and this work had no specific funding
COMPLIANCE WITH ETHICAL STANDARDS
The authors declare that they have no conflicts of interest. This article does not contain any studies with human participants performed by any of the authors.
REFERENCES
- 1.American Cancer Society . Cancer Treatment and Survivorship Facts & Figures 2014-2015. American Cancer Society2014; Atlanta, GA: [Google Scholar]
- 2.Hajdu SI, Vadmal M, Tang P. A note from history: Landmarks in history of cancer, part 7. Cancer. 2015;121(15):2480–513. doi: 10.1002/cncr.29365. doi:10.1002/cncr.29365. [DOI] [PubMed] [Google Scholar]
- 3.Weingart SN, Brown E, Bach PB, Eng K, Johnson SA, Kuzel TM, et al. NCCN Task Force Report: Oral chemotherapy. J Natl Compr Canc Netw. 2008;6(Suppl 3):S1–14. [PubMed] [Google Scholar]
- 4.Geynisman DM, Wickersham KE. Adherence to targeted oral anticancer medications. Discovery medicine. 2013;15(83):231–41. [PMC free article] [PubMed] [Google Scholar]
- 5.Stenberg U, Ruland CM, Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psychooncology. 2010;19(10):1013–25. doi: 10.1002/pon.1670. doi:10.1002/pon.1670. [DOI] [PubMed] [Google Scholar]
- 6.Romito F, Goldzweig G, Cormio C, Hagedoorn M, Andersen BL. Informal caregiving for cancer patients. Cancer. 2013;119(Suppl 11):2160–9. doi: 10.1002/cncr.28057. doi:10.1002/cncr.28057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Alliance for Caregiving in Collaboration with AARP [July 6, 2015];2015 Report: Caregiving in the U.S. Available at http://www.caregiving.org/wp-content/uploads/2015/05/2015_CaregivingintheUS_Final-Report-June-4_WEB.pdf. June 2015.
- 8.Yabroff KR, Kim Y. Time costs associated with informal caregiving for cancer survivors. Cancer. 2009;115(18 Suppl):4362–73. doi: 10.1002/cncr.24588. doi:10.1002/cncr.24588. [DOI] [PubMed] [Google Scholar]
- 9.Van Houtven CH, Ramsey SD, Hornbrook MC, Atienza AA, van Ryn M. Economic burden for informal caregivers of lung and colorectal cancer patients. Oncologist. 2010;15(8):883–93. doi: 10.1634/theoncologist.2010-0005. doi:10.1634/theoncologist.2010-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hanly P, Ceilleachair AO, Skally M, O'Leary E, Staines A, Kapur K, et al. Time costs associated with informal care for colorectal cancer: an investigation of the impact of alternative valuation methods. Appl Health Econ Health Policy. 2013;11(3):193–203. doi: 10.1007/s40258-013-0013-5. doi:10.1007/s40258-013-0013-5. [DOI] [PubMed] [Google Scholar]
- 11.Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ. 2004;170(12):1795–801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mosher CE, Champion VL, Azzoli CG, Hanna N, Jalal SI, Fakiris AJ, et al. Economic and social changes among distressed family caregivers of lung cancer patients. Support Care Cancer. 2013;21(3):819–26. doi: 10.1007/s00520-012-1585-6. doi:10.1007/s00520-012-1585-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mazanec SR, Daly BJ, Douglas SL, Lipson AR. Work productivity and health of informal caregivers of persons with advanced cancer. Research in nursing & health. 2011;34(6):483–95. doi: 10.1002/nur.20461. doi:10.1002/nur.20461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carey M, Paul C, Cameron E, Lynagh M, Hall A, Tzelepis F. Financial and social impact of supporting a haematological cancer survivor. Eur J Cancer Care (Engl) 2012;21(2):169–76. doi: 10.1111/j.1365-2354.2011.01302.x. doi:10.1111/j.1365-2354.2011.01302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Warner EL, Kirchhoff AC, Nam GE, Fluchel M. Financial Burden of Pediatric Cancer for Patients and Their Families. J Oncol Pract. 2014 doi: 10.1200/JOP.2014.001495. doi:10.1200/JOP.2014.001495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sherwood PR, Donovan HS, Given CW, Lu X, Given BA, Hricik A, et al. Predictors of employment and lost hours from work in cancer caregivers. Psychooncology. 2008;17(6):598–605. doi: 10.1002/pon.1287. doi:10.1002/pon.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bradley CJ, Dahman B. Time away from work: employed husbands of women treated for breast cancer. J Cancer Surviv. 2013;7(2):227–36. doi: 10.1007/s11764-012-0263-5. doi:10.1007/s11764-012-0263-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mosher CE, Jaynes HA, Hanna N, Ostroff JS. Distressed family caregivers of lung cancer patients: an examination of psychosocial and practical challenges. Support Care Cancer. 2013;21(2):431–7. doi: 10.1007/s00520-012-1532-6. doi:10.1007/s00520-012-1532-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yabroff KR, Dowling E, Rodriguez J, Ekwueme DU, Meissner H, Soni A, et al. The Medical Expenditure Panel Survey (MEPS) experiences with cancer survivorship supplement. J Cancer Surviv. 2012;6(4):407–19. doi: 10.1007/s11764-012-0221-2. doi:10.1007/s11764-012-0221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MEPS-HC Sample Design and Collection Process . Agency for Healthcare Research and Quality. Rockville, Md: http://www.meps.ahrq.gov/survey_comp/hc_data_collection.jsp. [Google Scholar]
- 21.Willis G, Yabroff KR, Liu B, Wilson MK, Nutt S, de Moor JS, Kent E, Virgo K, Ekwueme D, Rodriguez J. A Comparison of Probability and Non-Probability Samples.. Presented at the annual meeting of the American Association for Public Opinion Research; Hollywood, FL. May, 2015. [Google Scholar]
- 22.Yabroff KR, Short PF, Machlin S, Dowling E, Rozjabek H, Li C, et al. Access to preventive health care for cancer survivors. Am J Prev Med. 2013;45(3):304–12. doi: 10.1016/j.amepre.2013.04.021. doi:10.1016/j.amepre.2013.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weaver KE, Rowland JH, Bellizzi KM, Aziz NM. Forgoing medical care because of cost: assessing disparities in healthcare access among cancer survivors living in the United States. Cancer. 2010;116(14):3493–504. doi: 10.1002/cncr.25209. doi:10.1002/cncr.25209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arrossi S, Matos E, Zengarini N, Roth B, Sankaranayananan R, Parkin M. The socio economic impact of cervical cancer on patients and their families in Argentina, and its influence on radiotherapy compliance. Results from a cross-sectional study. Gynecol Oncol. 2007;105(2):335–40. doi: 10.1016/j.ygyno.2006.12.010. doi:10.1016/j.ygyno.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 25.Goren A, Gilloteau I, Lees M, DaCosta Dibonaventura M. Quantifying the burden of informal caregiving for patients with cancer in Europe. Support Care Cancer. 2014;22(6):1637–46. doi: 10.1007/s00520-014-2122-6. doi:10.1007/s00520-014-2122-6. [DOI] [PubMed] [Google Scholar]
- 26.Longo CJ, Fitch M, Deber RB, Williams AP. Financial and family burden associated with cancer treatment in Ontario, Canada. Support Care Cancer. 2006;14(11):1077–85. doi: 10.1007/s00520-006-0088-8. doi:10.1007/s00520-006-0088-8. [DOI] [PubMed] [Google Scholar]
- 27.Hayman JA, Langa KM, Kabeto MU, Katz SJ, DeMonner SM, Chernew ME, et al. Estimating the cost of informal caregiving for elderly patients with cancer. J Clin Oncol. 2001;19(13):3219–25. doi: 10.1200/JCO.2001.19.13.3219. [DOI] [PubMed] [Google Scholar]
- 28.The Family and Medical Leave Act of 1993.
- 29.Bureau of Labor Statistics USDoL, editor. Employee Benefits in the United States-March. 2015 [Google Scholar]
- 30. 5 U.S.C. 6331-6340.
- 31. 5 CFR part 630, subpart I.
- 32.Lynn J. Strategies to ease the burden of family caregivers. JAMA. 2014;311(10):1021–2. doi: 10.1001/jama.2014.1769. doi:10.1001/jama.2014.1769. [DOI] [PubMed] [Google Scholar]
- 33.Affairs UDoV [October 8 2015];VA Caregiver Support. http://www.caregiver.va.gov/support/support_services.asp.
- 34.Kim Y, Given BA. Quality of life of family caregivers of cancer survivors: across the trajectory of the illness. Cancer. 2008;112(11 Suppl):2556–68. doi: 10.1002/cncr.23449. doi:10.1002/cncr.23449. [DOI] [PubMed] [Google Scholar]
- 35.Mehnert A. Employment and work-related issues in cancer survivors. Crit Rev Oncol Hematol. 2011;77(2):109–30. doi: 10.1016/j.critrevonc.2010.01.004. doi:S1040-8428(10)00005-3 [pii] 10.1016/j.critrevonc.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 36.de Boer AG, Taskila T, Ojajarvi A, van Dijk FJ, Verbeek JH. Cancer survivors and unemployment: a meta-analysis and meta-regression. JAMA. 2009;301(7):753–62. doi: 10.1001/jama.2009.187. doi:301/7/753 [pii] 10.1001/jama.2009.187. [DOI] [PubMed] [Google Scholar]