Abstract
Background
Limited health literacy is associated with low adherence to asthma controller medications among older adults.
Objective
We sought to describe the causal pathway linking health literacy to medication adherence by modeling asthma illness and medication beliefs as mediators.
Methods
We recruited adults aged 60 years and older with asthma from hospital and community practices in New York, New York, and Chicago, Illinois. We measured health literacy and medication adherence using the Short Test of Functional Health Literacy in Adults and the Medication Adherence Rating Scale, respectively. We used validated instruments to assess asthma illness and medication beliefs. We assessed cognition using a cognitive battery. Using structural equation modeling, we modeled illness and medication beliefs as mediators of the relationship between health literacy and adherence while controlling for cognition.
Results
Our study included 433 patients with a mean age of 67 ± 6.8 years. The sample had 84% women, 31% non-Hispanic blacks, and 39% Hispanics. The 36% of patients with limited health literacy were more likely to have misconceptions about asthma (P < .001) and asthma medications (P < .001). Health literacy had a direct effect (β = 0.089; P < .001) as well as an indirect effect on adherence mediated by medications concerns (β = 0.033; P = .002). Neither medication necessity (β = 0.044; P = .138) nor illness beliefs (β = 0.007; P = .143) demonstrated a mediational role between health literacy and adherence.
Conclusions
Interventions designed to improve asthma controller medication adherence in older adults may be enhanced by addressing concerns about medications in addition to using communication strategies appropriate for populations with limited health literacy and cognitive impairments.
Keywords: Asthma, elderly, health literacy, adherence, medication beliefs, illness beliefs, cognition
Although the prevalence of asthma in older adults is similar to that in the young and middle-aged, older adults bear a disproportionate burden of asthma morbidity and mortality.1–3 In 2009, older adults represented only 12% of all patients with asthma in the United States,4 yet more than half of all deaths from asthma occurred among adults older than 65 years.2 Similarly, asthma hospitalization rates were more than 3 times as high among those older than 65 years (25.5 per 10,000) compared with 15- to 44-year-olds (7.2 per 10,000).2
Low rates of adherence to asthma controller medications may contribute to the poor outcomes observed among older adults with asthma.5,6 Inhaled corticosteroids, the mainstay of asthma controller medications and asthma management, decrease asthma symptoms and reduce emergency room visits, hospitalizations, and death,7 yet less than 50% of older adults with asthma use them as prescribed.8,9 There are various factors associated with underuse of asthma controller medications ranging from barriers to the specific treatment, including complex and costly regimens,10 patient/provider-level barriers, such as provider perceptions about the time required to complete patient counseling11,12 and a poor patient-provider relationship,13 to patient-level barriers including polypharmacy from a combination of chronic conditions14 and a lack of motivation to manage chronic illnesses.13 A growing body of research highlights the impact of 3 additional patient-level factors: (1) limitations in health literacy, defined by the Institute of Medicine as “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions,”15 (2) misconceptions about asthma and the medications used to treat it,16 and (3) impairments in cognition.17
We have demonstrated that limited health literacy, as measured using the Short Test of Functional Health Literacy in Adults (S-TOFHLA), is associated with inaccurate illness beliefs, namely, that asthma is present only when there are symptoms, that asthma is not a chronic condition, and that asthma is curable.18 Limited health literacy was also associated with having more concerns about medications on the Beliefs about Medications Questionnaire (BMQ), including that medications were addictive and greater concerns about medication side effects.19–21 Similarly, limitations in health literacy and cognition are independently associated with lower medication adherence among patients with asthma.17,22,23
Although it is well established that limited health literacy impacts medication adherence, the mechanisms by which this happens are uncertain. One potential mechanism is that health literacy influences beliefs about asthma and the medications used to treat it through its impact on information acquisition, which subsequently impacts medication adherence. To test illness and medication beliefs as mediators on the pathway linking health literacy and medications adherence, we performed structural equation modeling with data from a cohort of older adults with asthma.
METHODS
Participants and setting
Data for this analysis came from the Asthma Beliefs and Literacy in the Elderly study, a prospective cohort of adults aged 60 years and older with asthma.24 Briefly, patients were recruited from hospital- and community-based primary care and pulmonary practices in New York, New York, and Chicago, Illinois, between December 2009 and May 2012. Participants were eligible for the study if they were English or Spanish speaking, were 60 years or older, and had persistent moderate or severe asthma diagnosed by a clinician. Those who had chronic obstructive pulmonary disease, other chronic lung diseases, or more than 10 pack-year history of smoking were excluded. Once participants provided informed consent, they underwent a standardized, in-person interview in their preferred language (English or Spanish). Participants were excluded from this analysis if they did not complete the health literacy assessment. The study was approved by the institutional review boards at the Icahn School of Medicine at Mount Sinai and the Feinberg School of Medicine at Northwestern University.
Measures
Sociodemographic characteristics and potential variables along the causal pathway connecting health literacy to medication adherence were assessed: health literacy, illness and medication beliefs, cognition, and medication adherence.
Health literacy
Health literacy was measured using the S-TOFHLA.25 The S-TOFHLA is a 36-item reading comprehension and 4-item numeracy exercise. The reading comprehension test has 2 health care–related passages with every fifth to seventh word deleted. Participants select words that best complete each sentence. The numeracy test assesses health care–related quantitative capacity, such as the ability to understand numerical information on prescription bottles. Individual items were summed for a total score of 0 to 100, where inadequate is 0 to 53, marginal is 54 to 66, and adequate is 67 to 100. The S-TOFHLA has been validated for use in English and Spanish.25 Before conducting the analyses, we examined the distribution of scores and found that few patients were in the lowest categories. As a result, we dichotomized the health literacy scores as adequate (>_67) or limited (<67).
Illness and medication beliefs
Beliefs about asthma were assessed with the 8-item Brief Illness Perceptions Questionnaire (B-IPQ).26 The B-IPQ is based on Leventhal’s Common Sense Model of Self-Regulation and relies on the theory that patients’ mental models, or representations of an illness, provide the framework through which they understand and manage their illnesses.27,28 This model has served as a framework for understanding patients’ experiences of symptoms, treatment adherence, and care seeking for a range of conditions, including cardiovascular diseases, diabetes, cancer, and asthma.18 An overall B-IPQ score was computed by summing the items, with a total score ranging from 0 to 80; higher scores indicate a more negative or threatening view of the illness. We also reported specific beliefs from the B-IPQ that have been found to be strongly predictive of adherence to controller medications.18,29 Beliefs about asthma controller medications were assessed using the BMQ, a 10-item scale that can be tailored to measure beliefs about medications for a specific chronic illness.30 It is divided into 2 domains—concerns and necessity. Higher scores on the concerns subscale indicate greater concern about side effects and long-term dependence on asthma controller medications. Higher scores on the necessity subscale represent greater belief in the necessity of asthma controller medications for preserving one’s health.
Cognition
Cognitive function was measured using a selection of tests from the Alzheimer’s Disease Centers’ Uniform Data Set with extensive normative data.31 The neuropsychological battery was designed to assess immediate recall, executive function, verbal fluency, and processing speed. Assessment of immediate recall was done using the Wechsler Memory Scale Story A (WMS-immediate). The WMS-immediate requires participants to listen to a short story and immediately repeat as many details as possible.32 Assessment of executive function was done through the Trail Making Test Part B (Trails B). The Trails B represents the time required to sequentially connect a series of alternating letters and numbers scattered across a page in alphanumeric order.33 Verbal fluency was tested through animal naming whereby participants are given 1 minute to name as many animals as possible.33 Last, working memory was assessed through the use of the Weschler Adult Intelligence Scale III Letter-Number Sequencing.32 In this test, participants listen to a sequence of letters and numbers spoken by the interviewer, and then repeat them back in ascending number and alphabetical order.
Medication adherence
Adherence to asthma controller medications was measured using the 10-item Medication Adherence Rating Scale (MARS).34 The MARS is composed of statements about medication use behaviors, including regular versus as-needed use and intentional versus unintentional nonadherence. Respondents are asked how often they exhibit each behavior, with 5 options ranging from “always” to “never.” MARS has high interitem reliability (Cronbach α = 0.85), good test-retest reliability (r = 0.65; P < .001), and correlates strongly with objective measurements of asthma controller medication adherence.34 A mean MARS score between 1 and 5 was calculated from the answers to individual items; higher scores indicate better adherence. Participants with a mean MARS score of 4.5 or more were coded as having good adherence.34,35
Sociodemographic characteristics
Demographic variables, including age, sex, race/ethnicity, educational attainment, and income, were collected via self-report using validated items. We also collected data on the length of time since asthma diagnosis and whether participants had ever been intubated.
Statistical analysis
We tested associations between baseline demographic characteristics and health literacy using chi-square or ANOVA tests. We also used chi-square tests to conduct bivariate tests of association between (1) health literacy and each of illness and medication beliefs and cognition and (2) between the 3 factors—health literacy, illness and medication beliefs, and cognitive function—and medication adherence.
We used structural equation modeling to assess the indirect effect that health literacy has on medication adherence through illness beliefs, medication beliefs subscale items (concern and necessity), and cognition. Health literacy and medication adherence were entered into the model as continuous variables using the S-TOFHLA and mean MARS scores, respectively. The 2 domains of medication beliefs (concerns and necessity) were modeled separately as latent factors. The 5 items from the BMQ concerns subscale were used as indicators for medication concerns, and the 5 items from the BMQ necessity subscale were used as indicators for medication necessity. Illness beliefs were entered as a continuous variable summing the responses from the B-IPQ. A latent variable was created for cognitive function using the overall scores of WMS-immediate recall, Trails B, animal naming, and letters-numbers sequencing tests as the indicators. The model was adjusted for age, sex, race/ethnicity, English proficiency, and educational attainment.
The proportion of the total effect of health literacy on adherence attributable to the mediators was calculated by taking the ratio of the indirect effect divided by the total effect. The indirect effect for a pathway is calculated by multiplying the parameter estimates for each relationship in the pathway. Estimation for SEM was performed using maximum likelihood. The fit of the models was assessed using the root mean square error of approximation and the comparative fit index.36 In general, a root mean square error of approximation of more than 0.10 indicates a poor fit, 0.05 to 0.10 indicates a marginal fit, and less than 0.05 indicates a close fit. A comparative fit index of more than 0.90 indicates that the model has an adequate fit. Analyses were conducted with SAS 9.3 (SAS Institute Inc, Cary, NC) and Mplus7 (Muthen & Muthen, Los Angeles, Calif).
RESULTS
A total of 1972 patients were identified from the hospitals’ databases as having a diagnosis of asthma between December 2009 and May 2012. Of these, 531 (27.8%) were ineligible. Reasons for ineligibility included the following: no or mild asthma (52.2%), 10 or more pack-year smoking history (16.6%), another chronic lung disease (15.6%), and cognitive impairment, death, or another reason (15.6%). In addition, 466 (27.4%) were unreachable and 523 (27.4%) refused. Of the 452 (23.7%) enrolled in the study, 19 (4.2%) patients were excluded from this analysis because they did not complete the health literacy assessment, leaving a sample size of 433. The mean age of the participants was 67 ± 6.8 years, with 84% women, 31% non-Hispanic blacks, 39% Hispanics, and 22% whites. Asthma controller medications were currently used by 78.8% of the participants. One hundred fifty-five (36%) had limited health literacy. Those who had limited literacy were more likely to be minorities, older, poorer, with lower educational attainment, and to have been intubated in the past (P < .003 for all comparisons; Table I). There were no differences in sex or years with asthma between the 2 groups (P > .05 for all comparisons).
TABLE I.
Association of health literacy with patient characteristics
| Characteristic | All patients (N = 433) | Health literacy level
|
P value | |
|---|---|---|---|---|
| Adequate (n = 278) | Limited (n = 155) | |||
| Age (y) | ||||
|
| ||||
| 60–64 | 194 (45.0) | 141 (50.9) | 53 (34.4) | .003 |
|
| ||||
| 65–69 | 104 (24.1) | 63 (22.7) | 41 (26.6) | |
|
| ||||
| 70+ | 133 (30.9) | 73 (26.4) | 60 (39.0) | |
|
| ||||
| Sex: male | 70 (16.2) | 45 (16.2) | 25 (16.1) | .99 |
|
| ||||
| Race | ||||
|
| ||||
| Non-Hispanic white | 95 (21.9) | 90 (32.4) | 5 (3.2) | <.001 |
|
| ||||
| Non-Hispanic black | 132 (30.5) | 83 (29.9) | 49 (32.6) | |
|
| ||||
| Hispanic | 168 (38.8) | 76 (27.3) | 92 (59.4) | |
|
| ||||
| Other | 38 (8.8) | 29 (10.4) | 9 (5.8) | |
|
| ||||
| Income <$1350/mo | 229 (54.1) | 108 (39.7) | 121 (80.1) | <.001 |
|
| ||||
| Education | ||||
|
| ||||
| <12 y | 141 (32.6) | 37 (13.3) | 104 (67.5) | <.001 |
|
| ||||
| High school | 75 (17.4) | 50 (18.0) | 25 (16.2) | |
|
| ||||
| Some college | 89 (20.6) | 71 (25.5) | 18 (11.7) | |
|
| ||||
| College graduate | 127 (29.4) | 120 (43.2) | 7 (5.6) | |
|
| ||||
| Years with asthma, mean ± SD | 31.4 ± 20.8 | 31.0 ± 21.2 | 32.3 ± 20.0 | .54 |
|
| ||||
| Ever intubated | 38 (8.9) | 15 (5.5) | 23 (15.0) | .001 |
Values are n (%) unless indicated otherwise.
Unadjusted association of health literacy with illness and medication beliefs and cognition, and their association with adherence
Patients with limited health literacy had more negative illness and medication beliefs and scored lower on most of the cognitive abilities measured (Table II). Participants with limited health literacy were more likely to believe that asthma was temporary, present only when they were having symptoms, and could be cured (P < .001 for all comparisons). In addition, limited health literacy was associated with greater medication concerns (P < .001) and less belief in medication necessity (P = .02). Similarly, limited health literacy was also associated with poorer performance on all cognitive measures (Trails B, WMS-immediate, letter-number sequencing, and animal naming; P < .001 for all comparisons). All factors, including health literacy, illness and medication beliefs, and cognition, were significantly associated with adherence to asthma controller medications in the unadjusted analyses (Table III).
TABLE II.
Association of health literacy with asthma health beliefs and cognitive function
| Measure characteristics | Health literacy level
|
P value | |
|---|---|---|---|
| Adequate (n = 278) | Limited (n = 155) | ||
| Illness beliefs | |||
|
| |||
| B-IPQ, mean ± SD | 34.4 ± 12.8 | 39.6 ± 12.7 | <.001 |
|
| |||
| No symptoms no asthma, n (%) | 132 (47.8) | 100 (64.5) | <.001 |
|
| |||
| Will not always have asthma, n (%) | 61 (22.1) | 64 (41.3) | <.001 |
|
| |||
| Doctor can cure my asthma, n (%) | 38 (13.8) | 51 (32.9) | <.001 |
|
| |||
| BMQ scores, mean ± SD | |||
|
| |||
| Necessity score | 13.3 ± 4.6 | 12.1 ± 4.1 | .02 |
|
| |||
| Concern score | 12.9 ± 4.2 | 14.8 ± 4.2 | <.001 |
|
| |||
| Cognition | |||
|
| |||
| Memory | |||
|
| |||
| WMS-immediate, mean ± SD | 11.4 ± 4.0 | 7.2 ± 3.4 | <.001 |
|
| |||
| Executive function | |||
|
| |||
| Trails B, mean ± SD | 147.9 ± 82.5 | 271.6 ± 57.6 | <.001 |
|
| |||
| Word fluency | |||
|
| |||
| Animal naming test, mean ± SD | 17.4 ± 5.6 | 12.5 ± 4.1 | <.001 |
|
| |||
| Processing speed | |||
|
| |||
| Letter-numbers sequencing, mean ± SD | 8.0 ± 3.0 | 3.8 ± 2.7 | <.001 |
TABLE III.
Association of health literacy, beliefs, and cognition with medication adherence
| Adherence
|
P value | ||
|---|---|---|---|
| Good (n = 126) | Poor (n = 201) | ||
| Health literacy | |||
|
| |||
| Limited health literacy, n (%) | 25 (19.8) | 88 (43.8) | <.001 |
|
| |||
| Illness and medication beliefs | |||
|
| |||
| Illness beliefs | |||
|
| |||
| B-IPQ, mean ± SD | 33.8 ± 13.3 | 37.7 ± 12.1 | <.001 |
|
| |||
| No symptoms no asthma, n (%) | 44 (34.9) | 120 (59.7) | <.001 |
|
| |||
| Will not always have asthma, n (%) | 21 (16.7) | 75 (37.3) | <.001 |
|
| |||
| Doctor can cure my asthma, n (%) | 20 (15.9) | 43 (21.4) | .22 |
|
| |||
| BMQ scores, mean ± SD | |||
|
| |||
| Necessity score | 11.9 ± 4.3 | 13.5 ± 4.5 | .001 |
|
| |||
| Concern score | 12.0 ± 4.1 | 14.5 ± 4.2 | <.001 |
|
| |||
| Cognition | |||
|
| |||
| Memory | |||
|
| |||
| WMS-immediate, mean ± SD | 11.1 ± 4.1 | 9.3 ± 4.2 | <.001 |
|
| |||
| Executive function | |||
|
| |||
| Trails B, mean ± SD | 161.5 ± 94.0 | 203.7 ± 93.6 | <.001 |
|
| |||
| Word fluency | |||
|
| |||
| Animal naming test, mean ± SD | 17.1 ± 6.3 | 15.1 ± 5.1 | <.001 |
|
| |||
| Processing speed | |||
|
| |||
| Letter-numbers sequencing, mean ± SD | 7.6 ± 3.7 | 5.9 ± 3.3 | <.001 |
Mediation analysis
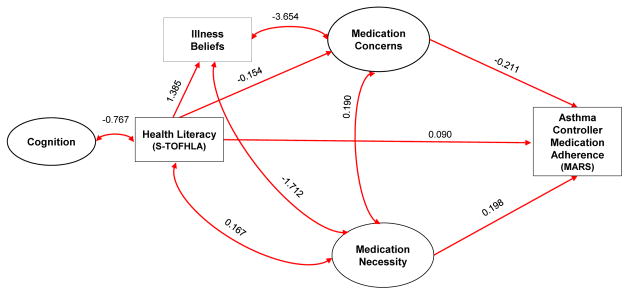
The best-fitting model demonstrated that medication concerns, a subscale of medication beliefs, was a partial mediator of the relationship between health literacy and medication adherence (root mean square error of approximation = 0.051 and comparative fit index = 0.931; Fig 1). Specifically, this model showed that greater concerns about medications was associated with lower health literacy (β = −0.154; P < .001) and lower medication adherence (β = −0.211; P <.004). The total indirect effect of this pathway was significant (β = 0.033; P =.002). Furthermore, health literacy was also directly associated with medication adherence (β = 0.090; P < .001). Comparing the sum total effect of health literacy on medication adherence (β = 0.123; P <.001) with the total indirect effect mediated by medication concerns (β = 0.033; P = .002) showed that approximately 27% of the effect of health literacy on adherence was mediated by medication concerns. Last, cognition and health literacy were associated (β = −0.767; P <.001), but cognition did not have a mediational role. Other models found that neither the path between health literacy and medication necessity (β = 0.044; P =.138) nor the path between illness beliefs and medication adherence (β = −0.007; P = .143) demonstrated meditational roles. Therefore, the final model demonstrates an association between health literacy and medication necessity (β = −0.155; P < .001) and no direct pathway between illness beliefs and medication adherence. All models controlled for age, sex, race/ethnicity, education, and English proficiency.
FIG 1.
Parameter estimates for model of medications concerns as a mediator of health literacy and medication adherence in older adults with asthma.
DISCUSSION
In this study, we used structural equation modeling to determine how health literacy, illness and medication beliefs, and cognition affect asthma controller medication adherence in older adults with asthma. We found 2 pathways by which health literacy impacts medication adherence. The first is that health literacy influences concerns about medications, which, in turn, influence medication adherence. Approximately one-quarter of the association of health literacy with adherence was attributable to this indirect pathway. We also found that health literacy has a direct impact on asthma controller medication. Our results suggest that limited health literacy leads to fears about asthma controller medications’ side effects and decreased adherence, identifying potentially valuable targets for educational interventions to improve adherence among older adults with asthma.
Our work is consistent with previous literature showing a connection between health literacy, medication concerns, and adherence. Older adults with limited health literacy are half as likely to be adherent to their asthma controller medications.37 Similarly, the odds of adherence to asthma controller medications is halved in patients with more concerns about medication side effect and addiction profiles.21 Although previous research has shown that patients with limited health literacy have greater concerns about their medications,29 this study is the first to show that low health literacy may lead to decreased adherence through contributing to misconceptions about asthma controller medications. In other words, patients with difficulty obtaining and processing medical information may misunderstand why and how medications work, develop fears about their medications, and be less likely to take them.
This pathway may be more pertinent to older adults because of the impact of cognitive function on health literacy. Although baseline literacy has been shown to affect cognition in late life,38,39 the increasing prevalence of dementia and delirium is likely to have a larger impact on health literacy as people age. As a result, it is possible that cognition did not have a mediational role in the model because health literacy and cognition are highly correlated in older adults. In previous studies, the odds of limited health literacy were 3 to 5 times higher in individuals with impairments in memory and verbal fluency than in those with normal cognition.40 In this way, the ability to self-manage asthma, including remembering clinician instructions, adhering to multidrug regimens, and complex problem-solving in the event of acute symptoms, may be improved not only by educational strategies that simplify vocabulary (a response to inadequate health literacy) but also by adopting techniques specific to the geriatric population.38,39
This knowledge of the importance of health literacy, medication beliefs, and cognition can lay the groundwork for a multipronged, geriatrics-specific approach to improving medication adherence in older adults with asthma, a group whose unique needs have been largely ignored.41 Our work has important practice implications for 3 reasons. First, the approach to older adults with asthma needs to be based on geriatrics principles of pharmacology and illness management.42 Many older adults are managing asthma medications and symptoms in the context of other comorbidities. As such, an effective intervention would need to include an individualized assessment of patients’ overall goals, symptom burden, a review of barriers to adherence, such as functional impairment, cost, or polypharmacy, and implementation of tailored solutions, such as simplifying regimens and enlisting pharmacists and other multidisciplinary team members.43–45
Second, information about asthma and asthma self-management should be delivered using limited health literacy techniques. Approximately one-third of English-speaking older adults and one-half of Spanish-speaking older adults have limited health literacy.46 Furthermore, worse health literacy is associated with increasing age and cognitive impairment, such that the frailest older adults are likely to be least adherent.47 To improve comprehension and subsequent adherence, techniques should be tailored to the patient and context and may include using familiar language and pictures, contextualizing facts and behaviors, limiting the amount of information provided, using teach-back techniques, or providing audio or print materials for patients to review the content on their own in the future.48
Third, practical interventions are needed to address patients’ concerns about their medications. In one survey, nearly half of all older adults with asthma and low literacy were concerned about the side effects of asthma controller medications or believed that these medications were addictive.21 Although patients may simultaneously believe that their medications are necessary, an implicit cost-benefit analysis weighs in favor of medication concerns and results in decreased adherence. To the authors’ knowledge, no studies have been done among older adults with asthma and low health literacy directly addressing this conflict. Future interventions among older adults with asthma may benefit from addressing erroneous medication beliefs.
There are limitations of our study. First, although the key strength of our study is the use of structural equation modeling to characterize associations between health literacy, illness and medication beliefs, and cognition with medication adherence, structural equation modeling cannot be used to prove a causal relationship between these factors and medication adherence. Second, individuals were recruited from 2 urban academic centers in the United States and findings may not be generalizable to younger patients or those residing outside urban areas. In addition, we relied on self-reported medication adherence, rather than measured adherence, which may not consistently reflect actual adherence.14 Finally, these results demonstrate the average affects in a cohort and, although they may be important in defining a group intervention, may not be applicable in approaching a given patient.
In summary, we found that the relationship between limited health literacy and low adherence to asthma controller medications among older adults with asthma is partially mediated by increased concerns about medications. This study suggests that interventions targeted at older adults with asthma may be most effective if they are sensitive to cognitive impairment, delivered using low health literacy techniques, and address patients’ medication concerns. Tailored interventional trials using the aforementioned strategies are needed to improve clinical outcomes among older adults with asthma.
Clinical implications.
Improving asthma controller medication adherence in older adults with low health literacy requires addressing medication concerns and using communication strategies appropriate for populations with limited health literacy and cognitive impairments.
Acknowledgments
This work was supported by a grant from the National Heart, Lung, and Blood Institute (grant no. 5R01HL096612-04), which played no role in the design or conduct of the study or the interpretation of its findings.
Abbreviations used
- B-IPQ
Brief Illness Perceptions Questionnaire
- BMQ
Beliefs about Medications Questionnaire
- MARS
Medication Adherence Rating Scale
- S-TOFHLA
Short Test of Functional Health Literacy in Adults
- WMS-immediate
Wechsler Memory Scale Story A
- Trails B
Trail Making Test Part B
Footnotes
Disclosure of Potential Conflict of Interest: J. L. Lin has received a grant from the National Cancer Institute. M. S. Wolf has received a grant from the National Heart, Lung, and Blood Institute, Merck, Eli Lilly, AbbVie, and United Healthcare and has consultant arrangements with Luto, Merck, Amgen, Adler Design, Imbev, Medlearning Group, CVS Caremark, and UAMS. R. O’Conor has received a grant from the National Heart, Lung, and Blood Institute. J. P. Wisnivesky has received a grant from the National Institutes of Health, Sanofi, and Quorum; is a board member for EHE International; and has consultant arrangements with Merck and Quintiles. A. D. Federman has received a grant from the National Institutes of Health. The rest of the authors declare that they have no relevant conflicts of interest.
References
- 1.Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. [Accessed September 1, 2015];Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. 2012 Available at: http://www.cdc.gov/nchs/data/databriefs/db94.htm. [PubMed]
- 2.American Lung Association. [Accessed September 1, 2015];Trends in asthma morbidity and mortality. 2012 Available at: http://www.lung.org/finding-cures/our-research/trend-reports/asthma-trend-report.pdf.
- 3.Quadrelli SA, Roncoroni A. Features of asthma in the elderly. J Asthma. 2001;38:377–89. doi: 10.1081/jas-100000259. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. [Accessed September 1, 2015];2013 National Health Interview Survey (NHIS) data. 2014 Available at: http://www.cdc.gov/asthma/nhis/2013/table3-1.htm.
- 5.Williams LK, Pladevall M, Xi H, Peterson EL, Joseph C, Lafata JE, et al. Relationship between adherence to inhaled corticosteroids and poor outcomes among adults with asthma. J Allergy Clin Immunol. 2004;114:1288–93. doi: 10.1016/j.jaci.2004.09.028. [DOI] [PubMed] [Google Scholar]
- 6.Williams LK, Peterson EL, Wells K, Ahmedani BK, Kumar R, Burchard EG, et al. Quantifying the proportion of severe asthma exacerbations attributable to inhaled corticosteroid nonadherence. J Allergy Clin Immunol. 2011;128:1185–91. e2. doi: 10.1016/j.jaci.2011.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Heart, Lung, and Blood Institute-National Asthma Education and Prevention Program. [Accessed September 1, 2015];Expert Panel Report 3: guidelines for the diagnosis and management of asthma: full report 2007. 2007 Available at: http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm#sthash.K0oQfp4l.dpuf.
- 8.Apter AJ, Wan F, Reisine S, Bender B, Rand C, Bogen DK, et al. The association of health literacy with adherence and outcomes in moderate-severe asthma. J Allergy Clin Immunol. 2013;132:321–7. doi: 10.1016/j.jaci.2013.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sofianou A, Martynenko M, Wolf MS, Wisnivesky JP, Krauskopf K, Wilson EA, et al. Asthma beliefs are associated with medication adherence in older asthmatics. J Gen Intern Med. 2013;28:67–73. doi: 10.1007/s11606-012-2160-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 11.Broers S, Smets E, Bindels P, Evertsz’ FB, Calff M, de Haes H. Training general practitioners in behavior change counseling to improve asthma medication adherence. Pat Educ Couns. 2005;58:279–87. doi: 10.1016/j.pec.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 12.Foster JM, Smith L, Usherwood T, Sawyer SM, Reddel HK. General practitioner-delivered adherence counseling in asthma: feasibility and usefulness of skills, training and support tools. J Asthma. 2016;53:311–20. doi: 10.3109/02770903.2015.1091473. [DOI] [PubMed] [Google Scholar]
- 13.Pelaez S, Lamontagne AJ, Collin J, Gauthier A, Grad RM, Blais L, et al. Patients’ perspective of barriers and facilitators to taking long-term controller medication for asthma: a novel taxonomy. BMC Pulm Med. 2015;15:42. doi: 10.1186/s12890-015-0044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barr R, Somers SC, Speizer FE, Camargo CA., Jr Patient factors and medication guideline adherence among older women with asthma. Arch Intern Med. 2002;162:1761–8. doi: 10.1001/archinte.162.15.1761. [DOI] [PubMed] [Google Scholar]
- 15.Bohlman-Nielsen L, Panzer A, Kindig D. Health literacy: a prescription to end confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 16.Dima AL, Hernandez G, Cunillera O, Ferrer M, de Bruin M group tA-L. Asthma inhaler adherence determinants in adults: systematic review of observational data. Eur Respir J. 2015;45:994–1018. doi: 10.1183/09031936.00172114. [DOI] [PubMed] [Google Scholar]
- 17.O’Conor R, Wolf MS, Smith SG, Martynenko M, Vicencio DP, Sano M, et al. Health literacy, cognitive function, proper use, and adherence to inhaled asthma controller medications among older adults with asthma. Chest. 2015;147:1307–15. doi: 10.1378/chest.14-0914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Halm EA, Mora P, Leventhal H. No symptoms, no asthma: the acute episodic disease belief is associated with poor self-management among inner-city adults with persistent asthma. Chest. 2006;129:573–80. doi: 10.1378/chest.129.3.573. [DOI] [PubMed] [Google Scholar]
- 19.Chambers CV, Markson L, Diamond JJ, Lasch L, Berger M. Health beliefs and compliance with inhaled corticosteroids by asthmatic patients in primary care practices. Respir Med. 1999;93:88–94. doi: 10.1016/s0954-6111(99)90296-2. [DOI] [PubMed] [Google Scholar]
- 20.Horne R. Patients’ beliefs about treatment: the hidden determinant of treatment outcome? J Psychosom Res. 1999;47:491–5. doi: 10.1016/s0022-3999(99)00058-6. [DOI] [PubMed] [Google Scholar]
- 21.Ponieman D, Wisnivesky JP, Leventhal H, Musumeci-Szabo TJ, Halm EA. Impact of positive and negative beliefs about inhaled corticosteroids on adherence in inner-city asthmatic patients. Ann Allergy Asthma Immunol. 2009;103:38–42. doi: 10.1016/S1081-1206(10)60141-X. [DOI] [PubMed] [Google Scholar]
- 22.Thai AL, George M. The effects of health literacy on asthma self-management. J Asthma Allergy Educ. 2010;1:50–5. [Google Scholar]
- 23.Rosas-Salazar C, Apter AJ, Canino G, Celedón JC. Health literacy and asthma. J Allergy Clin Immunol. 2012;129:935–42. doi: 10.1016/j.jaci.2012.01.040. [DOI] [PubMed] [Google Scholar]
- 24.Federman AD, Wolf MS, Sofianou A, O’Conor R, Martynenko M, Halm EA, et al. Asthma outcomes are poor among older adults with low health literacy. J Asthma. 2014;51:162–7. doi: 10.3109/02770903.2013.852202. [DOI] [PubMed] [Google Scholar]
- 25.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Pat Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 26.Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–7. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 27.Leventhal H, Leventhal EA, Contrada RJ. Self-regulation, health, and behavior: a perceptual-cognitive approach. Psychol Health. 1998;13:717–33. [Google Scholar]
- 28.Leventhal H, Safer MA, Panagis DM. The impact of communications on the self-regulation of health beliefs, decisions, and behavior. Health Educ Q. 1983;10:3–29. doi: 10.1177/109019818301000101. [DOI] [PubMed] [Google Scholar]
- 29.Federman AD, Wolf M, Sofianou A, Wilson EA, Martynenko M, Halm EA, et al. The association of health literacy with illness and medication beliefs among older adults with asthma. Pat Educ Couns. 2013;92:273–8. doi: 10.1016/j.pec.2013.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14:1–24. [Google Scholar]
- 31.Weintraub S, Salmon D, Mercaldo N, Ferris S, Graff-Radford NR, Chui H, et al. The Alzheimer’s Disease Centers’ Uniform Data Set (UDS): the neuropsychologic test battery. Alzheimer Dis Assoc Disord. 2009;23:91–101. doi: 10.1097/WAD.0b013e318191c7dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wechsler D. WMS-III: Wechsler Memory Scale administration and scoring manual. San Antonio, Texas: Psychological Corporation; 1997. [Google Scholar]
- 33.Spreen ES. A compendium of neuropsychological tests: administration, norms, and commentary. 2. New York, NY: Oxford University Press; 1998. [Google Scholar]
- 34.Cohen JL, Mann DM, Wisnivesky JP, Horne R, Leventhal H, Musumeci-Szabó TJ, et al. Assessing the validity of self-reported medication adherence among inner-city asthmatic adults: the Medication Adherence Report Scale for asthma. Ann Allergy Asthma Immunol. 2009;103:325–31. doi: 10.1016/s1081-1206(10)60532-7. [DOI] [PubMed] [Google Scholar]
- 35.Wisnivesky JP, Kattan M, Evans D, Leventhal H, Musumeci-Szabo TJ, McGinn T, et al. Assessing the relationship between language proficiency and asthma morbidity among inner-city asthmatics. Med Care. 2009;47:243–9. doi: 10.1097/MLR.0b013e3181847606. [DOI] [PubMed] [Google Scholar]
- 36.Wang J, Wang X. Structural equation modeling: applications using Mplus. United Kingdom: Wiley; 2012. [Google Scholar]
- 37.Federman AD, Wolf MS, Sofianou A, Martynenko M, O’Connor R, Halm EA, et al. Self-management behaviors in older adults with asthma: associations with health literacy. J Am Geriatr Soc. 2014;62:872–9. doi: 10.1111/jgs.12797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Manly JJ, Schupf N, Tang MX, Stern Y. Cognitive decline and literacy among ethnically diverse elders. J Geriatr Psych Neur. 2005;18:213–7. doi: 10.1177/0891988705281868. [DOI] [PubMed] [Google Scholar]
- 39.Manly JJ, Touradji P, Tang MX, Stern Y. Literacy and memory decline among ethnically diverse elders. J Clin Exp Neuropsycol. 2003;25:680–90. doi: 10.1076/jcen.25.5.680.14579. [DOI] [PubMed] [Google Scholar]
- 40.Federman AD, Sano M, Wolf MS, Siu AL, Halm EA. Health literacy and cognitive performance in older adults. J Am Geriatr Soc. 2009;57:1475–80. doi: 10.1111/j.1532-5415.2009.02347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hanania NA, King MJ, Braman SS, Saltoun C, Wise RA, Enright P, et al. Asthma in the elderly: current understanding and future research needs–a report of a National Institute on Aging (NIA) workshop. J Allergy Clin Immunol. 2011;128:S4–24. doi: 10.1016/j.jaci.2011.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hilmer SN, McLachlan AJ, Le Couteur DG. Clinical pharmacology in the geriatric patient. Fund Clin Pharmacol. 2007;21:217–30. doi: 10.1111/j.1472-8206.2007.00473.x. [DOI] [PubMed] [Google Scholar]
- 43.Steinman MA, Hanlon JT. Managing medications in clinically complex elders: “there’s got to be a happy medium”. J Am Med Assoc. 2010;304:1592–601. doi: 10.1001/jama.2010.1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44:213–8. doi: 10.1093/ageing/afu145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. J Am Med Assoc. 2005;294:716–24. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]
- 46.Gazmararian JA, Baker DW, Williams MV, Parker RM, Scott TL, Green DC, et al. Health literacy among Medicare enrollees in a managed care organization. J Am Med Assoc. 1999;281:545–51. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- 47.Levinthal BR, Morrow DG, Tu W, Wu J, Murray MD. Cognition and health literacy in patients with hypertension. J Gen Intern Med. 2008;23:1172–6. doi: 10.1007/s11606-008-0612-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mayer G, Villaire M. Health literacy in primary care: a clinician’s guide. New York: Springer Publishing Company; 2007. [Google Scholar]