Abstract
Background:
Stress hyperglycemia is common in patients presenting at the emergency medical ward and is associated with poor prognosis and increased risk of mortality.
Aims and Objective:
To study and determine the prevalence and factors associated with stress hyperglycemia.
Materials and Methods:
A cross-sectional observational study was performed on 536 nondiabetic patients presented to the Intensive Care Unit (ICU) at Gandhi Medical College and allied Hamidia Hospital, Bhopal, between March 31, 2015, and May 28, 2015. A detailed history including demographic profile, presence of chronic disease, history of hospitalization and ICU admission, surgical status, and major reason for ICU admission (i.e., predominant diagnostic category) was collected. Hematological and other parameters based on profile of study population were also analyzed.
Results:
Out of 536 patients, 109 (20.33%) had stress hyperglycemia. Out of 109 patients with stress hyperglycemia, 87 (16.23%) patients had glycated hemoglobin (HbA1c) <5.7% and 22 (4.10%) patients had HbA1c between 5.7% and 6.4%. Mean age of the study population was 40.27 ± 1.44 years, with male dominance. Mean random blood glucose level was 181.46 ± 3.80 mg/dl. Frequency of stress hyperglycemia was 24.13% in stroke, 19.54% in multiple organ dysfunction syndrome (MODS), 17.24% in chronic kidney disease (CKD), 12.64% in central nervous system (CNS) infection, 8.05% in chronic liver disease (CLD), and 8.05% in seizure patients. Association between stroke and stress hyperglycemia was significant (P = 0.036). Association between hospital stay more than 7 days and stress hyperglycemia was significant in stroke patients (P = 0.0029), CKD patients (P = 0.0036), CLD (P = 0.0099), and MODS patients (P = 0.0328).
Conclusions:
The factors associated with stress hyperglycemia were stroke, MODS, CKD, CNS infection, CLD, seizure patients, with prolonged hospital stay and expected proportion.
Keywords: Chronic kidney disease, Intensive Care Unit admission, stress hyperglycemia, stroke
INTRODUCTION
The American Diabetes Association and American Association of Clinical Endocrinologists[1] consensus on inpatient hyperglycemia defined stress hyperglycemia or hospital-related hyperglycemia as any blood glucose concentration >7.8 mmol/l (140 mg/dl) without evidence of previous diabetes.[1]
Stress hyperglycemia typically resolves as the acute illness or surgical stress abates.[2] More recently, the use of glycated hemoglobin (HbA1c) has been recommended over oral glucose tolerance test as the preferred diagnostic testing in hospitalized patients with hyperglycemia.[3] Measurement of an HbA1c during periods of hospitalization provides the opportunity to differentiate patients with stress hyperglycemia from those with diabetes who were previously undiagnosed.[4]
Stress hyperglycemia is very common among critically ill patients. DiNardo et al. claimed in their review that one-third of patients in tertiary care facilities were hyperglycemic.[4] Observational studies have reported a prevalence of hyperglycemia ranging from 32% to 38% in community hospitals, 16% of which had no previous history of diabetes mellitus.[5] Hyperglycemia is even more evident in critically ill patients where 31% of the population will have at least one blood glucose reading of 11.1 mmol/l (200 mg/dl) and nearly 100% will have a blood glucose >6.1 mmol/l (110 mg/dl) during Intensive Care Unit (ICU).[5]
Greci et al. showed that nearly one in five adult patients with “stress” hyperglycemia has probably unrecognized diabetes.[6] An association between stress-related hyperglycemia and adverse outcome was described in various patient groups: patients with myocardial infarction,[7,8] stroke,[9] cardiovascular surgery, pneumonia, sepsis,[10] pediatrics,[11] and chronic obstructive pulmonary disease.[12]
Stress hyperglycemia in other way defined as a transient increase in blood glucose during an acute physiological stress in the absence of diabetes. Mechanick reported a review of the mechanisms of stress hyperglycemia that a “stressor” is an event that constitutes a threat to homeostasis.[13] Stress or injury alters normal glucose metabolism because of changes in endocrine secretions and peripheral insulin resistance, resulting in stress hyperglycemia.[13] In the past, this response to stress or injury was believed to be beneficial during critical illness.[14] It has recently recognized to be associated with increased mortality and morbidity. Some studies show that insulin therapy results in reduced hospital and ICU length of stay, decreased need for antibiotics, fewer blood transfusion, reduced organ failure, and other benefits in critically ill patients.[15,16]
The landmark study of hyperglycemia in ICU patients by van den Berghe et al. in 2001 brought new light to the seriousness of hyperglycemia and had elicited the need for further research. Hence, the present study was performed to study clinical and epidemiological and factors associated with stress hyperglycemia.
MATERIALS AND METHODS
A cross-sectional observational study was performed on 536 nondiabetic patients presented to 24-bedded multidisciplinary Medical ICU at Gandhi Medical College and allied Hamidia Hospital, Bhopal, for 2 months from March 31, 2015, to May 28, 2015.
The study protocol was approved by the Ethics Committee of the Institute and written informed consent was obtained from each patient.
Diabetic patients on oral hypoglycemic agents and insulin therapy and undiagnosed diabetic (HbA1c >6.5%) patients were excluded from the study. Patients with severe anemia with hemoglobin <7 g% (reported to alter HbA1c level) and patients who had taken first aid from referral center with unknown status (alter random blood glucose level) were also excluded from the study.
A detailed history of patients including demographic profile (age and sex), presence of chronic disease, history of hospitalization and ICU admission, surgical status, major reason for ICU admission (i.e., predominant diagnostic category) were recorded from each patient. Hematological and other parameters based on profile of study population were also analyzed.
All the statistical analyses were performed using IBM Corporation, SPSS version 20. Mean and standard deviations were calculated for time-varying variables, and percentages were calculated for categorical variables. P <0.05 was considered statistically significant.
RESULTS
Out of 536 nondiabetic patients, 427 (79.66%) had normoglycemia and 109 (20.33%) had stress hyperglycemia; among them, 87 (16.23%) had HbA1c <5.7% whereas 22 (4.10%) patients had HbA1c between 5.7% and 6.4%.
The most common age group affected by stress hyperglycemic was 41–60 years (47 [43.12%]), followed by 40 (36.70%) patients with age group of 21–40 years. Stress hyperglycemia was mostly observed in male population (73 [66.97%]) as compared to female population (36 [33.03%]).
Distribution of patients according to random blood glucose sugar (random blood sugar [RBS] revealed that 78 (71.56%) patients had RBS between 141 and 180 mg/dl, 15 (13.76%) had between 181 and 220 mg/dl, 8 (7.34%) had between 221 and 260 mg/dl, and 5 (4.59%) patients had between 261 and 300 mg/dl; only 3 (2.76%) patients were recorded RBS more than 300 mg/dl [Tables 1 and 2].
Table 1.
Existing comorbidities in stress hyperglycemic and normoglycemic patients
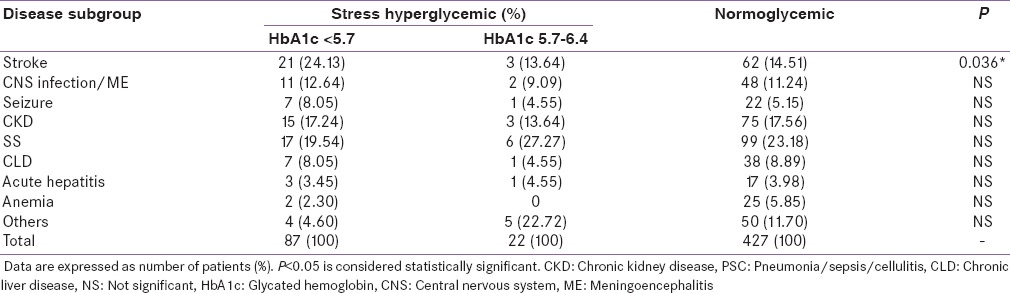
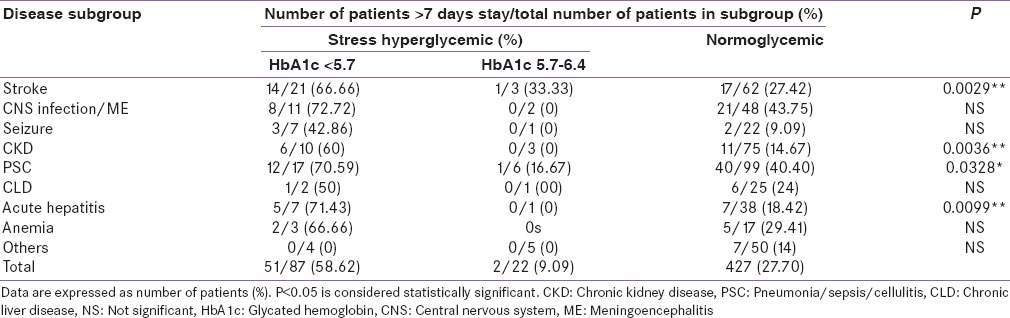
Table 2.
Proportion of patients with stress hyperglycemia and normoglycemia admitted for >7 days with existing comorbidities
DISCUSSION
In the present study, frequency of stress hyperglycemia in the medical ICU was 20.33%. This is lower than what was reported by DiNardo et al.[4] that one-third (33.33%) of patients in tertiary care facilities were nondiabetic hyperglycemic and Corstjens et al.[5] that 23% of nondiabetic patients had blood glucose levels above 11.1 mmol/L (200 mg/dl) upon admission.
The fact that most of the patients in the present study were not very sick, with less stress of illness, and they were more likely to have lesser sugar levels than very sick patients as in Corstjens et al.[5] We took lower limit of blood glucose 200 mg/dl and cardiac patients are not included because of separate department; hence, a lower proportion of stress hyperglycemia is recorded in our study.
Age group of the patients ranged from 13 years to 70 years with maximum patients in the age group of 41–60 years (43.12%), and mean age of the patients in our study was 40.27 ± 1.44 year. This finding was in sharp contrast to the studies by NICE-SUGAR[17] and LEUVEN trial,[14] in which the mean age was around 60 ± 12 years and 59 ± 3.7 years, respectively. This implies that patients in developing countries are much younger than developed nations.
There was male (66.97%) predominance in the present study. Finding was higher to study done by Krinsley,[15] Egi et al.,[18] and LEUVEN trial,[14] in whom there were 61%, 59%, and 63% male patients, respectively. It may be due to higher proportion of male hospitalization.
RBS in the present study was 140 mg/dl to 310 mg/dl. The mean glucose level in our study was 181.46 ± 3.80 mg/dl with maximum 71.56% patients having RBS 141–180 mg/dl. This finding was not comparable to a study by Egi et al. (139 ± 16.2 mg/dl) because their study included multiple blood glucose value in predefined interval.[18]
Frequency of stress hyperglycemia in the present study in existing comorbidities was 24.13% in stroke (higher prevalence as compared to Matz et al., 16%),[19] 19.54% in multiple organ dysfunction syndrome (MODS) (sepsis, pneumonia, cellulitis patients lower frequency as compared with Rattanataweeboon et al., 42.3%),[10] 17.24% in chronic kidney disease (CKD), 12.64% in central nervous system (CNS) infection, 8.05% in chronic liver disease (CLD), and 8.05% in seizure patients. Association between stroke and stress hyperglycemia was statistically significant. Our study differs from the previous study because of small number of patients.[10,19]
Significant association was observed between hospital stay more than 7 days and stress hyperglycemia for stroke, CKD, and CLD and significant in (MODS) pneumonia, sepsis, and cellulitis. Bochicchio et al. found that hyperglycemic trauma patients also had significantly longer ICU and hospital lengths of stay even when adjusted for age and injury severity score.16]
The present study had few limitations such as cardiac patients were not included because of separate department. Hence, a lower frequency of stress hyperglycemia was recorded. Family history of diabetes in stress hyperglycemic patients was not correlated because patient and their relatives were less educated, less aware of diabetes in developing country as compared to developed country.
The present study recommends that clinicians should have high index of suspicion of stress hyperglycemia in critically ill patients, especially when considering administration of intravenous or oral glucose in sick patients. This would lead to avoidance of unnecessary glucose infusions in these patients. Further studies should evaluate the pattern of subsequent blood sugar measurements in sick patients with stress hyperglycemia and its effects on the prognosis of sick patients and correlate stress hyperglycemia with severity of illness by established scoring systems for critically ill patients. Stress hyperglycemic patient may be prone to develop diabetes in future life, so they should advise for RBS and HbA1c monitoring.
CONCLUSIONS
Expected proportion of stress hyperglycemia was observed among patients admitted to the medical ICU. The factors associated with stress hyperglycemia in critically ill patients of are stroke, (MODS) sepsis, pneumonia, CKD, CNS infection, CLD, seizure patients. Stress hyperglycemic patients are associated with the prolonged hospital stay as compared with normoglycemic patients. Thus, it is now known that patients with stress hyperglycemia suffer from various diseases. Blood glucose value offers a simple, sensitive, noninvasive, easily available, bedside, consistent means of assessing the status of patients and identifies the high-risk patients even among those who have similar disease. Hence, all critically ill patients should be subjected to blood glucose monitoring and given appropriate management at the earliest.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Farrokhi F, Smiley D, Umpierrez GE. Glycemic control in non-diabetic critically ill patients. Best Pract Res Clin Endocrinol Metab. 2011;25:813–24. doi: 10.1016/j.beem.2011.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garber AJ, Moghissi ES, Bransome ED, Jr, Clark NG, Clement S, Cobin RH, et al. American college of endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract. 2004;10(Suppl 2):4–9. doi: 10.4158/EP.10.S2.4. [DOI] [PubMed] [Google Scholar]
- 3.Mazurek JA, Hailpern SM, Goring T, Nordin C. Prevalence of hemoglobin A1c greater than 6.5% and 7.0% among hospitalized patients without known diagnosis of diabetes at an urban inner city hospital. J Clin Endocrinol Metab. 2010;95:1344–8. doi: 10.1210/jc.2009-1151. [DOI] [PubMed] [Google Scholar]
- 4.DiNardo MM, Korytkowski MT, Siminerio LS. The importance of normoglycemia in critically ill patients. Crit Care Nurs Q. 2004;27:126–34. doi: 10.1097/00002727-200404000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Corstjens AM, van der Horst IC, Zijlstra JG, Groeneveld AB, Zijlstra F, Tulleken JE, et al. Hyperglycaemia in critically ill patients: Marker or mediator of mortality? Crit Care. 2006;10:216. doi: 10.1186/cc4957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greci LS, Kailasam M, Malkani S, Katz DL, Hulinsky I, Ahmadi R, et al. Utility of HbA1c levels for diabetes case finding in hospitalized patients with hyperglycemia. Diabetes Care. 2003;26:1064–8. doi: 10.2337/diacare.26.4.1064. [DOI] [PubMed] [Google Scholar]
- 7.Lerario AC, Coretti FM, Oliveira SF, Betti RT, Bastos Mdo S, Ferri Lde A, et al. The prevalence of diabetes and stress hyperglycemia in the acute myocardial infarction patients. Arq Bras Endocrinol Metabol. 2008;52:465–72. doi: 10.1590/s0004-27302008000300006. [DOI] [PubMed] [Google Scholar]
- 8.Ishihara M. Acute hyperglycemia in patients with acute myocardial infarction. Circ J. 2012;76:563–71. doi: 10.1253/circj.cj-11-1376. [DOI] [PubMed] [Google Scholar]
- 9.Kernan WN, Viscoli CM, Inzucchi SE, Brass LM, Bravata DM, Shulman GI, et al. Prevalence of abnormal glucose tolerance following a transient ischemic attack or ischemic stroke. Arch Intern Med. 2005;165:227–33. doi: 10.1001/archinte.165.2.227. [DOI] [PubMed] [Google Scholar]
- 10.Rattanataweeboon P, Vilaichone W, Vannasaeng S. Stress hyperglycemia in patients with sepsis. J Med Assoc Thai. 2009;92(Suppl 2):S88–94. [PubMed] [Google Scholar]
- 11.Klein GW, Hojsak JM, Schmeidler J, Rapaport R. Hyperglycemia and outcome in the pediatric intensive care unit. J Pediatr. 2008;153:379–84. doi: 10.1016/j.jpeds.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 12.Baker EH, Janaway CH, Philips BJ, Brennan AL, Baines DL, Wood DM, et al. Hyperglycaemia is associated with poor outcomes in patients admitted to hospital with acute exacerbations of chronic obstructive pulmonary disease. Thorax. 2006;61:284–9. doi: 10.1136/thx.2005.051029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mechanick JI. Metabolic mechanisms of stress hyperglycemia. JPEN J Parenter Enteral Nutr. 2006;30:157–63. doi: 10.1177/0148607106030002157. [DOI] [PubMed] [Google Scholar]
- 14.van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–67. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- 15.Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc. 2003;78:1471–8. doi: 10.4065/78.12.1471. [DOI] [PubMed] [Google Scholar]
- 16.Bochicchio GV, Salzano L, Joshi M, Bochicchio K, Scalea TM. Admission preoperative glucose is predictive of morbidity and mortality in trauma patients who require immediate operative intervention. Am Surg. 2005;71:171–4. doi: 10.1177/000313480507100215. [DOI] [PubMed] [Google Scholar]
- 17.Finfer S, Chittock DR, Su SY, Blair D, Foster D, et al. NICE-SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283–97. doi: 10.1056/NEJMoa0810625. [DOI] [PubMed] [Google Scholar]
- 18.Egi M, Bellomo R, Stachowski E, French CJ, Hart G. Variability of blood glucose concentration and short-term mortality in critically ill patients. Anesthesiology. 2006;105:244–52. doi: 10.1097/00000542-200608000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Matz K, Keresztes K, Tatschl C, Nowotny M, Dachenhausen A, Brainin M, et al. Disorders of glucose metabolism in acute stroke patients: An underrecognized problem. Diabetes Care. 2006;29:792–7. doi: 10.2337/diacare.29.04.06.dc05-1818. [DOI] [PubMed] [Google Scholar]


