Abstract
Background:
This study aimed to document practices in managing hypothyroidism among doctors in New Delhi, with special focus on subclinical hypothyroidism, pregnancy, and old age, and to compare it with global practices.
Methods:
During an academic program attended by 394 doctors, all participants were given a questionnaire designed based on thyroid practices survey done by Burch et al. to evaluate the practice patterns. Questions were based on evaluating doctor's preferred choices in diagnosis, therapy, and follow-up of hypothyroidism in different scenarios.
Results:
Responses from 308 questionnaires (general physicians [n = 204], obstetricians [n = 51], pediatricians [n = 27], surgeons [n = 12], endocrinologists [n = 10], and others [n = 4]) were analyzed. In the evaluation of 52-year-old female patient with primary hypothyroidism, 52% doctors would prefer thyroid ultrasonography, comparable to global rates. Nearly 96.1% doctors would have initiated levothyroxine, with a large majority of doctors (83.77%) preferred using branded levothyroxine. About 58.74% doctors preferred gradual restoration of euthyroidism. Levothyroxine dose of 25 mcg was the most preferred increment dose (46.07%) during follow-up, with 6 weekly being the most frequent dose adjustment frequency (41.57%). Most preferred target thyroid-stimulating hormone (TSH) in the 52-year-old female patient was 2.5–4.99 mU/L (63.96%), 25-year-old female patient was 1–2.49 mU/L (53.90%), and in 85-year-old female was 2.5–4.99 mU/L (45.45%). Only 68% of doctors in our study preferred keeping TSH <2.5 mU/L during the first trimester of pregnancy, in contrast to global trends of 95% (P < 0.001).
Conclusion:
There was a disproportionately high use of ultrasonography in hypothyroidism management, near exclusive preference for branded levothyroxine, widespread use of age-specific TSH targets, and low threshold for treating mild thyroid failure, a highly variable approach to both rates and means of restoring euthyroidism for overt primary hypothyroidism. There is a need for spreading awareness regarding TSH targets in pregnancy.
Keywords: Clinical practice, guidelines, hypothyroidism, pattern, trends
INTRODUCTION
Hypothyroidism is one of the most common diagnoses seen in clinical practice, across different specialties ranging from family and general physicians, obstetricians, infertility specialists, surgical specialties during the preoperative workup of patients, and last but not the least by the endocrinologists.[1,2,3] In two large studies from India, the prevalence of anti-thyroid peroxidase (anti-TPO) positivity, overt hypothyroidism, and subclinical hypothyroidism has been reported to be 13.3%–21.8%, 3.5%–4.2%, and 8.02%–19.3%, respectively.[4,5,6] In spite of available different clinical practice guidelines (CPGs)/recommendations for the management of hypothyroidism, a lot of heterogeneity with regard to treatment practices is seen in hypothyroidism. Controversies exist, especially with regard to treatment threshold for mild subclinical hypothyroidism, treatment targets especially during pregnancy and old age, and screening in the general population, during prepregnancy and presurgical investigative work up of an individual.[7,8,9,10,11]
This study aimed to document the current clinical practices in managing hypothyroidism among doctors of different specialties in New Delhi, with special focus on subclinical hypothyroidism, pregnancy, and old age. This study also aimed to compare the current clinical practices in India with the clinical practices in the US, using the 2012 American Association of Clinical Endocrinology (AACE)/American Thyroid Association (ATA) hypothyroidism guidelines as the reference standard.[1,11] This guideline was used as the reference guideline as this is one of the most commonly referred guidelines in the management of hypothyroidism and has already been previously used in the US to evaluate the clinical practices of the doctors there and other parts of the globe.[11]
METHODS
The society for the promotion of education in endocrinology and diabetes conducted a one-day current medical education (CME) program on the management of thyroid disorders on February 21, 2016, which was attended by 394 doctors from different specialties including family and general physicians, obstetricians, pediatricians, surgeons, and endocrinologists. At the beginning of the CME, all the doctors were given a questionnaire including 30 multiple choice questions with the scope of marking more than 1 choice as the preferred answer. A time of 15 min was allocated for filling the questionnaire based on a pilot study done in 15 doctors before the event. The questionnaire was designed based on the survey done by Burch et al. in 2013 to evaluate the clinical practice patterns for managing hypothyroidism in the US (after taking approval from Burch to use their questionnaire).[11] Questions in the questionnaire were primarily based on evaluating the doctor's preferred choices in diagnostic evaluation, choice of therapy, and follow-up for an index case (vide infra) of primary hypothyroidism followed by three clinical variants including a patient with persistent symptoms of hypothyroidism despite having achieved biochemical euthyroidism, a patient planning for pregnancy, and a patient with subclinical hypothyroidism.[11]
Questionnaire
A 52-year-old female patient reported with 9-month history of fatigue, cold intolerance, poor concentration, constipation, and she was otherwise healthy, had no significant medication history, and had no addictions. She had a blood pressure of 135/90 mmHg, pulse rate of 55 beats per minute, and weighed 60 kg. She had a firm goiter, approximately twice normal size. Serum thyroid-stimulating hormone (TSH) was 20 mU/L (normal 0.4–4.5 mU/L), and free T4 was 0.7 ng/dL (normal 0.8–1.8 ng/dL). Questions 1–16 were based on the above-mentioned index case. Questions 17–24 were related to the management of hypothyroidism in the soon to be pregnant or a currently pregnant patient. The details of the patient used in the questionnaire were that of a 25-year-old female with recently diagnosed primary hypothyroidism who wished to become pregnant. History was significant for one prior spontaneous miscarriage. She had a small firm goiter, pulse rate of 55 beats per minute, and normal deep tendon reflexes. At diagnosis 3 months earlier, she was placed on levothyroxine, and currently, her serum TSH was 3.5 mU/L (normal 0.4–4.5 mU/L). Anti-TPOs were strongly positive. Questions 25 and 26 were on the management of subclinical hypothyroidism. It was based on the clinical history of a 52-year-old female with a family history of thyroid dysfunction, who was found to have a serum TSH of 7.8 mU/L. She was asymptomatic and otherwise healthy, not taking any medication, and had no addictions. She had a blood pressure of 125/80 mmHg, a pulse rate of 75 beats per minute, and weight of 60 kg. She had a firm goiter, approximately twice normal size. Repeat serum TSH is 7.9 mU/L, and free T4 was in the mid-normal range. Question 27 was on the volume of newly diagnosed hypothyroidism patients managed by the doctor. Question 28 was on the clinical specialty of the doctor; question 29 on the year of graduation from the medical school and question 30 was on the gender of the doctor. The detailed questionnaire has been elaborated at the end of the manuscript.
Study participants
Study participants were a diverse group of practicing doctors ranging from family physicians/general practitioners, obstetricians, internal medicine specialists, surgeons, and endocrinologists practicing in New Delhi, who voluntarily chose to attend the CME. The venue, timing, and the program content of the CME were advertised in the local newspapers, radio, and all major hospitals of New Delhi for the prior 1 month to the actual event. There were no registration fees for the event, and any doctor was free to attend the event.
Statistical analysis
Summary statistics were prepared for responses to each question. Because not every participant answered all questions, the percentage of respondents providing a given answer was calculated individually for each question, using the number of respondents to that question as the denominator. The analysis was performed using the Statistical Package for the Social Sciences (SPSS) (Chicago, Illinois, USA) version-20 software.
RESULTS
A total of 394 doctors participated in the CME program, of which 339 doctors returned the questionnaires. Responses from 308 questionnaires were analyzed. Thirty-one questionnaires with <50% of the questions answered were excluded from the analysis. A majority of the attending doctors were family/general physicians (n = 204), followed by obstetricians (n = 51), pediatricians (n = 27), surgeons (n = 12), endocrinologists (n = 10), and others (n = 4). The median (25–75th percentile) year of graduation (MBBS) of the attending doctors was 1984 (1976–1995). Two hundred and ten doctors were males, 96 females, and 2 did not disclose their gender. The number of new hypothyroidism cases seen on a monthly basis was < 10 for 186 participants (60.38%), 10–30 for 84 participants (27.27%), 30–60 for six participants (1.94%), and >60 for four participants (1.30%). Twenty-eight participants (9.1%) reported that they see zero patients per month with newly diagnosed hypothyroidism.
Diagnostic evaluation of the index patient
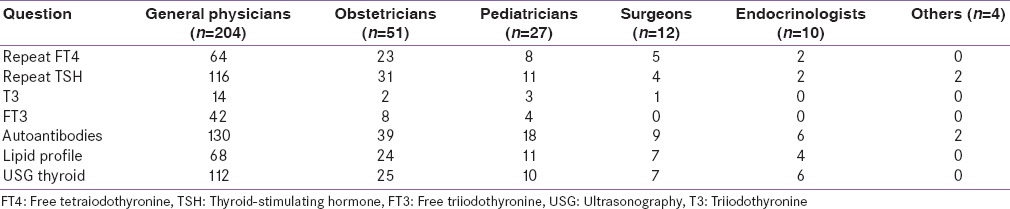
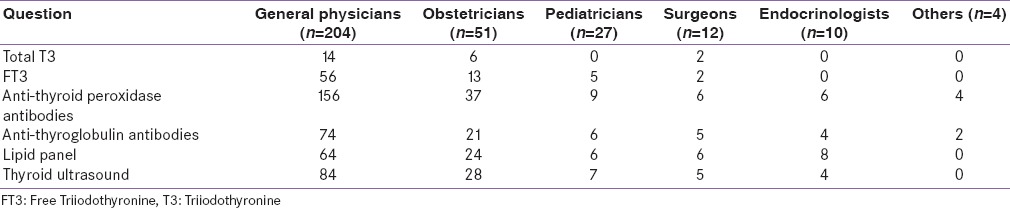
Question 1 dealt with the diagnostic evaluation of the index patient. Repeat free T4, TSH, total T3, and free T3 evaluation were requested by 102 (33.12%), 166 (53.89%), 20 (6.49%), and 54 (17.53%) participants, respectively. Two-hundred and four doctors (66.23%) needed thyroid autoantibodies evaluation, whereas 114 (37.01%) and 160 (51.95%) doctors requested lipid profile and thyroid ultrasonography evaluation, respectively. The difference in prescription patterns for investigations sought among doctors from different specialties is shown in Table 1.
Table 1.
Analysis of question 1
Treatment decisions
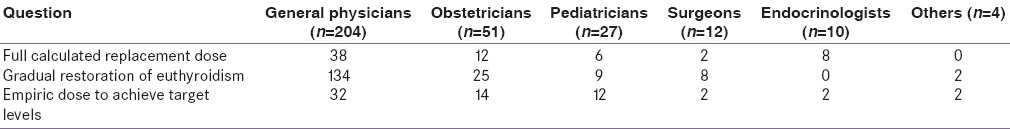
About 96.1% (296 out of 308) doctors would have initiated levothyroxine supplementation in the index patient with overt hypothyroidism. All the 12 doctors who decided against levothyroxine supplementation were general physicians. Among the preferred techniques for correcting hypothyroidism, 21.42% doctors (n = 66) would start with full-calculated levothyroxine replacement dose as the initial treatment option, 58.74% doctors (n = 178) would gradually restore euthyroidism starting with a low dose of levothyroxine and gradually building up the dose over weeks to months, and 20.78% doctors (n = 64) would select an empiric dose to achieve target TSH levels [Table 2]. For the 178 doctors who preferring a gradual restoration of euthyroidism, most (46.07%; n = 82) would increase the levothyroxine doses in increments of 25 mcg, followed by 37.08% doctors (n = 66) by 12.5 mcg, 13.48% doctors (n = 24) preferred increments of 50 mcg, and 6 doctors (3.37%) preferred increase in levothyroxine dose by 100 cmg. The most commonly preferred frequency of incremental increases in levothyroxine dose in doctors who preferred a gradual restoration of euthyroidism (n = 178) was 6 weeks (41.57%; n = 74), followed by 4 weeks (33.71%; n = 60), 3 months (11.24%; n = 20), and 2 months (8.98%; n = 16), and 8 doctors (4.49%) preferred 2 weekly increment in levothyroxine dose. Gender of the doctor had no impact on the choice of correction technique. Doctors who preferred a gradual increase in levothyroxine dose had a later year of graduation (median [25–75th percentile]) from MBBS (1986 [1977–1997]) as compared to those who preferred use of full-calculated levothyroxine dose/empirical dose (1984 [1975–1992]) to start treatment (P = 0.082).
Table 2.
Strategy for correcting hypothyroidism in 52-year-old female with primary hypothyroidism (index case)
Preferred thyroid hormone preparation for therapy, frequency of follow-up, and treatment targets
Among the 308 respondents, a large majority of doctors (83.77%; n = 258) preferred using a specific brand of levothyroxine for therapy. Only 13.63% (n = 42) doctors used generic levothyroxine for therapy. The use of levothyroxine plus liothyronine combination of thyroid extract was extremely uncommon reported by 7 (2.27%) and 1 (0.32%) doctors, respectively. The use of specific brand of levothyroxine was significantly higher among obstetricians (92.16%) and surgeons (91.67%) as compared to general physicians (81.37%), pediatricians (81.5%), and endocrinologists (80%) (P < 0.001). Nearly half of the surveyed doctors (46.75%; n = 144) preferred repeat thyroid function testing and dose adjustment following 6 weeks of follow-up. A quarter of the doctors (26.62%; n = 82) needed repeat thyroid function assessment at 4 weeks of follow-up. Thirty-four doctors (11.04%) each preferred repeat biochemical assessment at 2 and 3 months of follow-up.
Among the 308 respondents, the most preferred target TSH in the 52-year-old female (index case) was 2.5–4.99 mU/L (63.96%; n = 197), followed by 1–2.49 mU/L (26.95%; n = 83). Twenty-two respondents (7.14%) preferred a higher TSH target of 5–8 mU/L. When asked about the preferred TSH target in a younger 25-year-old patient, there was a shift toward lower TSH values. One hundred and sixty-six respondents (53.90%) now preferred a TSH target of 1–2.49 mU/L, followed by 124 respondents (40.26%) preferring a TSH target of 2.5–4.99 mU/L. Conversely, when asked about the preferred treatment TSH target in an 85-year-old female, 140 respondents (45.45%) preferred a TSH of 2.5–4.99 mU/L, followed by 108 respondents (35.1%) opting for a TSH of 5–8 mU/L. Thirty-four respondents (11.03%) preferred a TSH target of 8–10 mU/L. The comparison of TSH targets in the three different discussed patients of different age groups is shown in Figure 1 (181.8KB, pdf) .
Questionnaire used for the survey
Long-term follow-up
After achieving stable target TSH values, when the respondents were asked how often they would repeat thyroid laboratory testing, the most preferred follow-up thyroid function testing duration was 6 months (49.35%; n = 152), followed by 3 months (34.74%; n = 107). Thirty-six respondents (11.69%) preferred doing an annual thyroid function testing in a stable euthyroid patient. The most preferred method of follow-up of asymptomatic patients at target TSH values was laboratory evaluation of thyroid function along with office visits in 162 respondents (52.60%), followed by return to the primary care physician by 43.51% (n = 134), or laboratory studies plus a phone call by 3.89% (n = 12) of respondents.
Managing persistent hypothyroid symptoms with biochemical euthyroidism
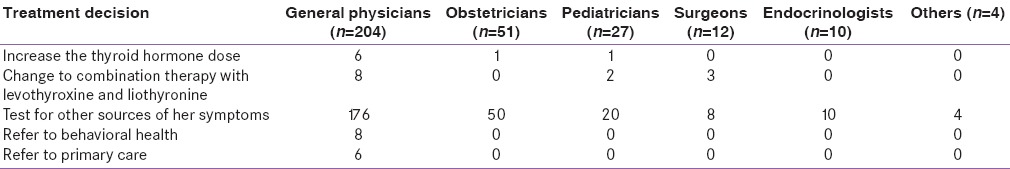
We queried respondents about their response to a patient who despite achieving target TSH values on levothyroxine therapy still has persistent symptoms suggestive of hypothyroidism. An overwhelming 87.01% (n = 268) respondents preferred evaluation for other sources of the patient's symptoms. Eight respondents (2.5%) each would consider increasing the dose of levothyroxine or seek referral for the behavioral health evaluation. Only 6 doctors (1.94%) considered referring the patient back to their primary care physician for further evaluation as the optimal decision [Table 3].
Table 3.
Preferred treatment response to a patient who despite achieving target thyroid-stimulating hormone on levothyroxine still has persistent hypothyroid symptoms
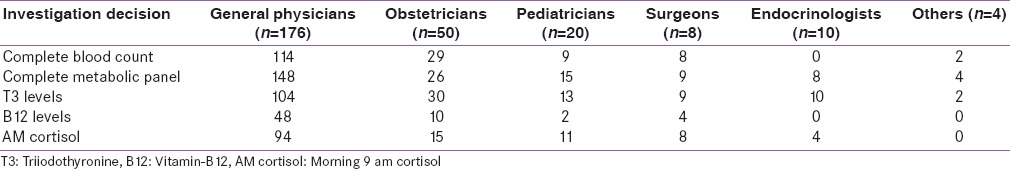
Among the respondents who preferred evaluation for other sources of patient's symptoms (n = 268), the most commonly sought evaluation was complete metabolic panel (81.34%; n = 218), followed by T3 levels (62.68%; n = 168), complete blood count (60.44%; n = 162), morning cortisol (49.25%; n = 132), and serum Vitamin B12 levels (23.88%; n = 64) [Table 4].
Table 4.
Preferred investigations among doctors evaluating for other sources of persistent symptoms of hypothyroidism with biochemical euthyroidism (n=268)
Hypothyroidism management in a patient planning pregnancy
The doctors were asked for their opinion regarding management of a 25-year-old woman with recently diagnosed primary hypothyroidism (details in the questionnaire, vide infra) on levothyroxine having TSH of 3.5 mU/L, who wishes to become pregnant (history of 1 spontaneous miscarriage). For this patient, the most preferred prepregnancy TSH target was 1–2.49 mU/L (68.50%; n = 211), followed by 2.5–4.5 mU/L (19.48%; n = 60). 9.09% (n = 28) and 2.92% (n = 9) respondents selected TSH <0.1 mU/L and 5–8 mU/L as their preferred TSH target, respectively. Four-weekly intervals was the most preferred frequency of thyroid function monitoring during pregnancy (71.10%; n = 219), followed by 8.44%, 9.41%, and 10.39% for 2 weeks, 8 weeks, and 12 weeks monitoring.
Subclinical hypothyroidism management
In the case of 52-year-old woman with subclinical hypothyroidism (details in the questionnaire, vide infra), the most preferred investigation to decide on further management was serum anti-TPO antibody titer (70.78%; n = 218), followed by thyroid ultrasonography (41.56%; n = 128), anti-thyroglobulin titer (36.36%; n = 112), lipid profile (35.06%; n = 108), serum free T3 (24.67%; n = 76), and total T3 (7.14%; n = 22) [Table 5].
Table 5.
Preferred investigation in a 52-year-old female with subclinical hypothyroidism
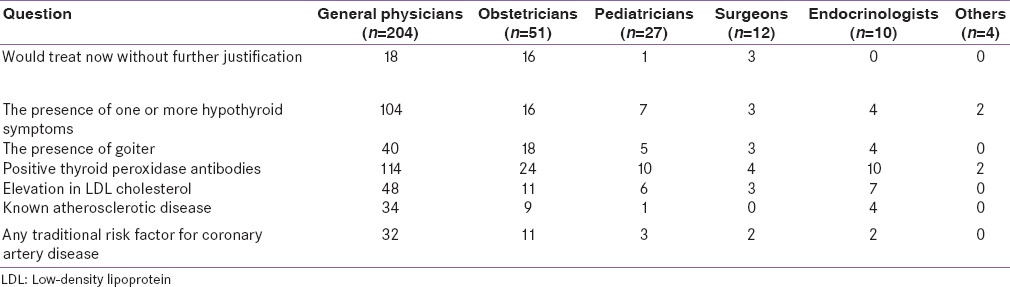
The most common factor that would influence the decision to start levothyroxine therapy for subclinical hypothyroidism was the presence of anti-TPO antibody positivity (53.24%; n = 164), followed by the presence of one or more hypothyroidism symptoms (44.15%; n = 136), elevated LDL cholesterol (24.35%; n = 75), and presence of goiter (22.73%; n = 70). About 12.33% doctors (n = 38) would prefer treatment of subclinical hypothyroidism on diagnosis itself without any further investigation. 15.58% (n = 48) and 16.23% (n = 50) doctors would treat subclinical hypothyroidism in the presence of atherosclerotic disease and patients having one of more traditional risk factors for coronary artery disease [Table 6].
Table 6.
Factor that would influence the decision to start levothyroxine in subclinical hypothyroidism
DISCUSSION
In this age of globalization and standardization, especially in the field of medicine, it is important to periodically evaluate the current practices of care in a particular geographical area. In this regard, this study evaluated the current clinical practice patterns of doctors in New Delhi with regard to the management of hypothyroidism in different clinical scenarios and compared it with the global management patterns. Burch et al. previously evaluated the clinical practice patterns in hypothyroidism in 880 respondents from different parts of the globe (North America [67.5%], United States [65.0%], Canada [2.5%], Latin America [9.7%], Europe [9.2%], Asia and Oceania [8.1%], and the Middle East and Africa [5.5%]).[11] We have used the same questionnaire they had used, to enable us to compare the results from our study.
In the evaluation of the index case of a 52-year-old female with clinical features suggestive of hypothyroidism with biochemical report confirming primary hypothyroidism, 52% of the doctors in our study would prefer thyroid ultrasonography, which is comparable to the rates seen in Latin America (58.0%), Europe (58.8%), Asia-Oceania (58.2%), and Middle East-Africa (56.3%), but significantly higher than North America where only 37.9% doctors would prefer thyroid ultrasonography (P < 0.001).[11] It is important to highlight that a majority of the doctors needed evaluation for thyroid autoantibodies (66.23%) to analyze the underlying etiology for this hypothyroidism, and 37% doctors needed to rule out any associated dyslipidemia, which is common in hypothyroidism. Thyroid ultrasonography is not recommended routinely in the hypothyroid patient in the ATA/AACE guidelines, but 52% of respondents in our study (40% of respondents in the study by Burch et al.) would obtain this study.[11] This may be reflective of the general practice of seeking structural evaluation of thyroid using ultrasonography and to rule out the presence of thyroid nodules. Thyroid ultrasonography would also help in the diagnosis of Hashimoto's thyroiditis. The current CPGs recommended against the use of T3 measurement in making the diagnosis of hypothyroidism, and accordingly both in New Delhi as well as globally, only a minority of doctors in the survey requested for T3 evaluation.
Nearly 96.1% doctors would have initiated levothyroxine supplementation in the index patient with overt hypothyroidism, which is comparable to the globally observed rate of 98.9%.[11] The use of T4 monotherapy was recommended in the CPG, and nearly 100% of respondents agreed. In spite of India being the global capital of generic medicine manufacturing, an overwhelming 83.77% doctors in our study preferred using a specific brand of levothyroxine for therapy. This is significantly higher than the global preferences (P < 0.001). North America had the lowest rate of use of specific brand of levothyroxine for therapy (37.9%), followed by Latin America (58.0%), Asia-Oceania (58.2%), Middle East-Africa (56.3%), and Europe (58.8%).[11] The reasons for this near-exclusive preference for branded levothyroxine in New Delhi may be multifactorial. Generic levothyroxine is not commonly available in the market. It is primarily available in the big hospitals and institutes. Levothyroxine is a medication which comes under the price control list of medications by the Government of India. Hence, the price is not much different between branded and generic levothyroxine in India. A majority of patients do out-of-pocket expenditure while buying medicines in India and may choose to buy a branded preparation. Generic and brand name LT4 preparations are mostly bioequivalent, but altered bioavailability has been reported due to changes in the formulation of preparations. Hence, it is advisable to stick to one brand during long-term therapy.[12]
The majority of doctors from New Delhi (58.74%) preferred a gradual restoration of euthyroidism starting with a low dose of levothyroxine and gradually building up the dose over weeks to months in the index 52-year-old female with primary hypothyroidism, which is similar to rates reported from Latin America (60.5%), Europe (55.8%), Asia-Oceania (55.1%), and Middle East-Africa (46.8%), but significantly higher as compared to North America (30.5%; P < 0.001).
Increments of 25 mcg followed by 12.5 mcg were the most preferred increment dose among doctors (46.05% and 37.08%, respectively; 83.13%) preferring a gradual restoration of euthyroidism in our study. In contrast globally, 61.1% would increase in increments of 25 mcg, followed by 50 mcg by 26.9% doctors. This is in accordance with current guidelines, which recommends a gradual correction of hypothyroidism for all patients over 50–60 years of age.[11] Repeat thyroid function testing and dose adjustment following 6 weeks of follow-up was the most favored time-window by doctors in our study (46.75%), which is similar to the global patterns where 49.2% doctors would recheck thyroid hormone levels 6 weeks after starting thyroid hormone therapy.[11]
In our study, the most preferred TSH target in the 52-year-old index patient was 2.5–4.99 mU/L (63.96%), which is higher than the globally preferred target of 1.0–1.9 mU/L in 47.7% respondents.[11] Similar to the global trends, there was a shift to a lower TSH target when the age of the patient was considered to be 25 years, and a higher target when the age of the considered patient was increased to 85 years. This is important as overtreatment in the elderly population may increase the risk of iatrogenic hyperthyroidism and the associated osteoporosis and atrial fibrillation.[13,14] After achieving euthyroidism, the most preferred follow-up thyroid function testing duration was 6 months (49.35%), followed by 3 months (34.74%). In the study by Burch et al., 55.5% doctors would obtain laboratory studies at 6-month intervals, followed by 12 months in 34.0%. Only 9.3% doctors would do thyroid function assessment 3 monthly. About 43.51% doctors would refer their patients to the primary care physician in New Delhi, which is higher than in North America (23.8%), but lower that in Europe (54.5%) (P < 0.001).[11]
For patients having persistent hypothyroidism symptoms despite achieving biochemical euthyroidism, 87.01% doctors in our study preferred evaluation for other sources of the patient's symptoms, which is comparable to the global trends of 84.3% doctors testing for other sources of the patient's symptoms. The most commonly sought investigations in these patients were complete metabolic panel (81.34%), followed by T3 levels (62.68%), complete blood count (60.44%), morning cortisol (49.25%), and Vitamin-B12 levels (23.88%) in our study. In contrast, the global trends for the most sought investigations were complete cell count (90.3%), complete metabolic panel (82.4%), morning cortisol level (58.5%), B-12 levels (57.4%), and T3 levels (21.9%).
In a young female planning for pregnancy, the most preferred prepregnancy TSH target was 1–2.49 mU/L (68.50%), which was significantly lower than that of global trends where 95.1% doctors would prefer a TSH value <2.5 mU/L (P < 0.001).[8] Nearly 71.1% doctors would monitor thyroid function during pregnancy at a 4-week interval, which is similar to the global trends of 67.7% doctors preferring a 4-week monitoring.[11]
Patients with subclinical hypothyroidism and TSH values between 5 and 10-mU/L represent a subset in which treatment with thyroid hormone is of unproven benefit.[11,15] In an asymptomatic 52-year-old female with subclinical hypothyroidism, the most preferred investigation to decide on further management was serum anti-TPO antibody titer (70.78%), followed by thyroid ultrasonography (41.56%), anti-thyroglobulin titer (36.36%), and lipid profile (35.06%). In contrast, globally, 91.9% doctors would perform TPO Ab testing, 50.6% would obtain a lipid panel, 50.4% would do a thyroid ultrasound, and 41.5% doctors would obtain antithyroglobulin Ab titer.[11] Only a small fraction of doctors would prefer T3 testing (serum free T3 [24.67%] and total T3 [7.14%] in our study; 19.7% would order either a free T3 or total T3 testing globally). The most common factor that would influence the decision to start levothyroxine therapy for subclinical hypothyroidism was the presence of anti-TPO antibody positivity (53.24%), followed by the presence of one or more hypothyroidism symptoms (44.15%), elevated LDL cholesterol (24.35%), and presence of goiter (22.73%), which is similar to the global trends. Only 12.33% doctors in New Delhi would prefer treatment of subclinical hypothyroidism on diagnosis itself without any further investigation, which is much lower than in North America (24.7%), but comparable to that in Latin America (10.8%), Europe (14.3%), or Asia-Oceania (9.3%).[11]
Due to concerns regarding adverse neurodevelopmental impact and on intelligence quotient associated with maternal hypothyroidism during early pregnancy, lower trimester-specific TSH targets are recommended in pregnancy (<2.5 mU/L in the first trimester; <3.0 mU/L in the second and third trimester).[16,17] However, in spite of this, only 68% of doctors in our study would prefer to keep TSH <2.5 mU/L during the first trimester in pregnancy in contrast to global trends of 95%. Hence, there is a need to increase the awareness among doctors in New Delhi regarding the pregnancy-specific TSH targets. It must however be highlighted that management of subclinical hypothyroidism in pregnancy is still an area of active research with changes in guidelines expected in the recent future, with the availability of more clinical evidence. As of today, universal screening of thyroid function is not recommended in pregnancy by any of the guidelines. The Endocrine Society of USA recommends levothyroxine in all women with subclinical hypothyroidism whereas the ATA guidelines recommend levothyroxine therapy only in women with subclinical hypothyroidism, who are anti-TPO antibody-positive, or TSH >10 mIU/L.[18]
The current guidelines provide specific referral criteria, implying that only a few hypothyroid patients do require specialty care and a majority of the patients can be easily followed up under the care of a family physician. However, both in our study and Burch et al.'s study, only a small minority of the evaluated doctors referred the patients to their family physicians for long-term follow-up after achieving euthyroidism.
Limitations of this study include the lack of equal representation of doctors from different specialties, the doctors evaluated may not be representative of all doctors of the state of New Delhi, as they were recruited from the participants of an academic event, and it is likely that doctors who had an interest in managing hypothyroidism were more likely to have attended this event. Nevertheless, this study generates vital data, provides better understanding of the doctors’ psyche with regard to managing hypothyroidism, and highlights potential areas where treatment approaches can be further improved. To summarize, the key observation of this study was a nearly exclusive preference for levothyroxine alone as initial therapy for hypothyroidism, widespread use of age-specific TSH treatment targets, a low threshold for treating mild thyroid failure, a need for spreading awareness regarding TSH targets in pregnancy, a nearly exclusive use of branded levothyroxine for therapy, a disproportionately high use of ultrasonography in hypothyroidism management, which is not evidence based and a highly variable approach to both the rate and means of restoring euthyroidism for overt primary hypothyroidism. A lot of interesting similarities as well as difference with international global trends in managing hypothyroidism were also highlighted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Garber JR, Cobin RH, Gharib H, Hennessey JV, Klein I, Mechanick JI, et al. Clinical practice guidelines for hypothyroidism in adults: Cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid. 2012;22:1200–35. doi: 10.1089/thy.2012.0205. [DOI] [PubMed] [Google Scholar]
- 2.Sharma N, Sharma LK, Dutta D, Gadpayle AK, Anand A, Gaurav K, et al. Prevalence and predictors of thyroid dysfunction in patients with HIV infection and acquired immunodeficiency syndrome: An Indian perspective. J Thyroid Res 2015. 2015:517173. doi: 10.1155/2015/517173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Basu N, Dutta D, Maisnam I, Basu S, Ghosh S, Chowdhury S, et al. Percutaneous ethanol ablation in managing predominantly cystic thyroid nodules: An Eastern India perspective. Indian J Endocrinol Metab. 2014;18:662–8. doi: 10.4103/2230-8210.139229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Unnikrishnan AG, Kalra S, Sahay RK, Bantwal G, John M, Tewari N. Prevalence of hypothyroidism in adults: An epidemiological study in eight cities of India. Indian J Endocrinol Metab. 2013;17:647–52. doi: 10.4103/2230-8210.113755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marwaha RK, Tandon N, Ganie MA, Kanwar R, Sastry A, Garg MK, et al. Status of thyroid function in Indian adults: Two decades after universal salt iodization. J Assoc Physicians India. 2012;60:32–6. [PubMed] [Google Scholar]
- 6.Kalra S, Kumar A, Jarhyan P, Unnikrishnan AG. Indices of thyroid epidemiology. Indian J Endocrinol Metab. 2015;19:844–7. doi: 10.4103/2230-8210.167543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooper DS, Biondi B. Subclinical thyroid disease. Lancet. 2012;379:1142–54. doi: 10.1016/S0140-6736(11)60276-6. [DOI] [PubMed] [Google Scholar]
- 8.Vadiveloo T, Donnan PT, Murphy MJ, Leese GP. Age- and gender-specific TSH reference intervals in people with no obvious thyroid disease in Tayside, Scotland: The Thyroid Epidemiology, Audit, and Research Study (TEARS) J Clin Endocrinol Metab. 2013;98:1147–53. doi: 10.1210/jc.2012-3191. [DOI] [PubMed] [Google Scholar]
- 9.Haddow JE. Maternal thyroxine and fetal brain development: The latest chapter, a look back, and considerations for the future. J Clin Endocrinol Metab. 2013;98:1388–90. doi: 10.1210/jc.2013-1646. [DOI] [PubMed] [Google Scholar]
- 10.Brent GA. The debate over thyroid-function screening in pregnancy. N Engl J Med. 2012;366:562–3. doi: 10.1056/NEJMe1112591. [DOI] [PubMed] [Google Scholar]
- 11.Burch HB, Burman KD, Cooper DS, Hennessey JV. A 2013 survey of clinical practice patterns in the management of primary hypothyroidism. J Clin Endocrinol Metab. 2014;99:2077–85. doi: 10.1210/jc.2014-1046. [DOI] [PubMed] [Google Scholar]
- 12.Khandelwal D, Tandon N. Overt and subclinical hypothyroidism: Who to treat and how. Drugs. 2012;72:17–33. doi: 10.2165/11598070-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 13.Dutta D, Dharmshaktu P, Aggarwal A, Gaurav K, Bansal R, Devru N, et al. Severity and pattern of bone mineral loss in endocrine causes of osteoporosis as compared to age-related bone mineral loss. J Postgrad Med. 2016;62:162–9. doi: 10.4103/0022-3859.183170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Biswas D, Dutta D, Maisnam I, Mukhopadhyay S, Chowdhury S. Occurrence of osteoporosis and factors determining bone mineral loss in young adults with Graves’ disease. Indian J Med Res. 2015;141:322–9. doi: 10.4103/0971-5916.156620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma LK, Sharma N, Gadpayle AK, Dutta D. Prevalence and predictors of hyperprolactinemia in subclinical hypothyroidism. Eur J Intern Med. 2016 doi: 10.1016/j.ejim.2016.07.012. pii: S0953-620530219-9. [DOI] [PubMed] [Google Scholar]
- 16.Haddow JE, Palomaki GE, Allan WC, Williams JR, Knight GJ, Gagnon J, et al. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Engl J Med. 1999;341:549–55. doi: 10.1056/NEJM199908193410801. [DOI] [PubMed] [Google Scholar]
- 17.Finken MJ, van Eijsden M, Loomans EM, Vrijkotte TG, Rotteveel J. Maternal hypothyroxinemia in early pregnancy predicts reduced performance in reaction time tests in 5- to 6-year-old offspring. J Clin Endocrinol Metab. 2013;98:1417–26. doi: 10.1210/jc.2012-3389. [DOI] [PubMed] [Google Scholar]
- 18.Amouzegar A, Mehran L, Sarvghadi F, Delshad H, Azizi F, Lazarus JH. Comparison of the American Thyroid Association with the Endocrine Society practice guidelines for the screening and treatment of hypothyroidism during pregnancy. Hormones (Athens) 2014;13:307–13. doi: 10.14310/horm.2002.1486. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Questionnaire used for the survey


