Abstract
Navratri is one of the most common religious fasts observed among Hindus. A large number of people with diabetes follow Navratris fast irrespective of its health implications, often without proper education and medical advice. The quest for the scientific research on dietary advices for Hindu fasts including Navratris shows paucity of literature comparative to the dietary advices advocated during Ramadan. The eating and physical activity patterns during different fasts vary a lot depending up on social and cultural factors. Even eating pattern is not uniform among all persons following Navratris and is modified as per their region, local culture, and religious beliefs. Dietary advice during Navratris depends upon pattern of fasting, religious beliefs, and local sociocultural factors. In this review, efforts are made to provide pragmatic dietary advice for people with diabetes, modifications in the menus and cooking practices, and timings of the meals for successful blood glucose management during Navratris. This review will also help plan diet and physical activity advice for persons observing other fasts as well.
Keywords: Diabetes mellitus, diet, fasting, Hinduism, India, Navratris
INTRODUCTION
India has a vast variety of cultures and religions following vast number of festivals and rituals. In India, numerous festivals are celebrated irrespective of their caste, creed, age, and status with different rituals.[1] Fasting or abstinence from certain foods and feasting are observed among most of the people at such occasions and religions. Navratris among Hindus and Ramadan among Muslims are one of the most common fasts being observed in India. Hindu religion constitutes the world's third largest religion comprising over 80% of the population of Nepal and India, and over 5% of the population in at least another 15 countries. Many types of fasts are observed by Hindus for cultural and religious issues such as annual KarvaChauth, Guru Purnima, Ahoi Ashtami, and Navratris.[2]
Navaratri is one of the widely celebrated festivals among them all over India and Nepal according to regional traditions. It is a 9 day festival devoted to the worship of goddess Durga. In general, Navaratri comes 5 times a year but is usually celebrated twice a year in the months of March–April (ending on the 9th and final day which is celebrated as Ram Navami) and September–October (ending on the 10th day celebrated as Vijayadashmi also called Dussehra), the exact dates being fixed according to the Hindu lunar calendar. It is celebrated in different parts of the world wherever Hindu societies exist. The people observe fasts, worship goddess (north India), perform garba and dandiya-raas dance (western India) and follow unique tradition-bound activities in different states with different cultural beliefs.[3]
CHALLENGES OF DIABETES MANAGEMENT IN INDIA
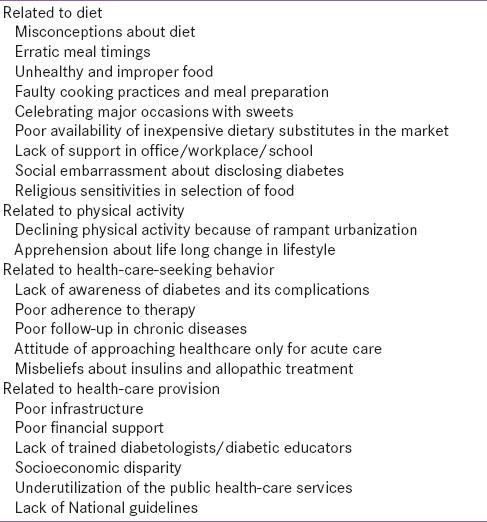
There are numerous challenges of diabetes management in India related to diet, physical activity pattern, health care-seeking behavior, and health-care provision [Table 1]. Studies show poor glycemic control and higher incidence of acute and chronic complications in Indian patients. In addition, there is lack of awareness and misconceptions about their concepts and attitudes toward diabetes, its complications, diet, exercise, drug therapy, understanding about insulin, and treatment among patients and as well their family members.[4]
Table 1.
Challenges of diabetes management in India
CHALLENGES OF DIABETES MANAGEMENT DURING FASTING
It is an important consideration that health cannot be ignored whether it is a fasting or a feasting occasion. Maintenance of a balance between “health” and “celebrations” is a tight rope walk, especially for those with compromised health status. Fasting or feasting is both a diplomatic situation and a challenge for diabetics.
Since the persons with diabetes should eat at regular intervals to maintain optimum blood glucose levels,[5] management of diabetes is challenging for the physician during such fasting periods when people abstain from certain food items and opt to survive on others observing a long time fasting, usually eating once or twice in a whole day.[6] Erratic meal patterns are evidenced by consumption of either only fruits or consumption of single meal throughout all the fasting days.[3] In addition, in the festive mood and social gathering, people with diabetes may be served unhealthy and improper food such as high fat, calorie-rich foods with improper timings.
A sudden change in dietary habits can have harmful and unmanageable impacts on blood glucose levels. On one hand, it leads to episodes of hypoglycemia and on the other hand, it results in postprandial hyperglycemia, ketoacidosis, metabolic complications consequently leading to renal dysfunction and major comorbidities.[7,8] Abstinence of water and fluids during hot weather can result in dehydration, electrolyte imbalance, and hypotension while hyperglycemia can lead to loss of body fluids and electrolytes through excessive urination.[2]
Fasting may throw off the delicate balance of food, water, and blood glucose levels in potentially harmful ways.[9] Abstinence from food lowers the circulating glucose levels, decreasing secretion of insulin, raising the levels of glucagon and catecholamines and stimulating the breakdown of glycogen. Prolonged fasting may deplete glycogen stores, increasing the production and oxidation of fatty acids from adipocytes leading to ketoacidosis.[8,10] Contraction of the intravascular space and dehydration may increase the tendency of thrombosis during fasting.[5,10] The quality and quantity of food consumption and changes in weight during fasting days can impact serum lipids levels also.[11]
There are limited studies pertaining to the impact of fasts on glycemic control, hypoglycemia, and other health outcomes in diabetics. Furthermore, most of such data are available in context of Ramadan fasting in Muslims. There is gross paucity of data about Hindu fasting including Navratris in people with diabetes. Available data indicate that diabetics often ignore their nutrition/health during fasting. A study published in 2013 revealed significantly increased calorie consumption during Ramadan fasting with increased consumption of carbohydrates, protein and fats independent of the socioeconomic strata and educational status. On the contrary, beneficial effects had been observed for the diabetic people consuming diets which were high in rich complex carbohydrates, dietary fiber, and relatively low in fat.[12]
PREFAST ASSESSMENT
Patients may visit their primary care physicians asking if they can observe fast and precautions they need to follow if they observe fast. In addition, during routine visits, health-care physicians should take the advantage of taking history regarding fasting pattern observed by the patients taking care of their religious beliefs. However, discussion about fasting should be carried out prior to the fast. Health-care physician needs to discuss potential risks of fasting. Furthermore, it is important to understand exact perspective of fasting, including duration of fast, allowance for liquids and snacks during the day, acceptance of sublingual foods and freedom to break the fast in case of significant discomfort must be clarified. Pre-fast assessment comprises comprehensive history-taking, physical examination, and investigations aimed at identifying stigmata of target-organ damage, so that strategies can be made to optimize health during fasts. Factors that may increase the risk of hypoglycemia, hypoglycemia unawareness, and dehydration must be noted.
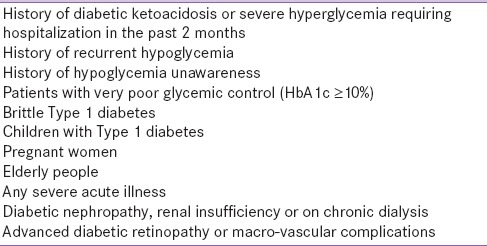
Although fasting may improve health-related outcomes such as blood pressure, lipids, insulin sensitivity, and biomarkers of oxidative stress in general population,[13] it should not be the part of many diabetic patients specifically harmful among those with severe hypoglycemic incidents, poor glycemic control, noncompliant, poorly controlled, pregnant diabetics, and diabetic patients with renal disease.[7,8,10,11] Fasting should be strongly discouraged in the presence of life-threatening, or organ-/limb-threatening situations [Table 2].
Table 2.
Diabetic patients for whom fasting is not advisable
MEDICAL NUTRITION THERAPY DURING FASTING
In the management of diabetes, the importance of medical nutrition therapy (MNT) cannot be ignored at any time including fasts to ensure adequate glycemic control and to prevent both short- and long-term complications.[9] The American Diabetes Association (ADA) guidelines regards MNT as mandatory part of an overall treatment plan and considered it to be followed during fasting days as well for achievement of dietary goals.[14,15] The dietary advice is a broad term to include the knowledge about eating patterns, meal planning, food selection, food preparation, dinning out, portion control, as well as appropriate responses to eating challenges.[16] The patients need to be educated about timings of meals, wise selection of food items, dietary modifications, healthful recipes, and nutritional requirements.[17] The dietary advice should also ensure caring individualized needs depending upon other associated complications such as hypertension, nephropathy, and cardiac disease. Besides that, knowledge about lifestyle activity, glucose monitoring, medications, and insulin regimens are also considered necessary for successful blood glucose management, medical care, caretakers, and patient self-management education.[18,19]
Prefast meal
To prepare for fasting period, the prefast meal (usually a day or two before fasting) should comprise “slow-release” calories by including complex and nondigestive carbohydrates with low glycemic index, proteins, and moderate amount of fats. It should be balanced diet providing unprocessed and unrefined cereals, pulses and lentils, vegetables, fruits, limited oil, and nuts to reduce its glycemic index and retain energy availability for a longer period. Water and fluids should be adequately included to prevent dehydration usually if water intake is also restricted during fasting. Meal supplements/replacements can prove to be beneficial as well for good glycemic control and health.[2]
Meal during fasting
Meal pattern
For a meal planning during fast, the dietician/diabetic educator/health-care physician first needs to understand about the pattern of fast being observed, and kind of food items being eaten during fasts as per their religious and cultural patterns. In Navratris, the eating patterns and beliefs have no fixed rule and vary from community to community, allowing different kinds of foods, different cooking practices with different frequencies and timings, some people eating only one or two major meals while others eating particular kinds of foods particularly fruits, vegetables, and dairy products at more frequent intervals.
Meal composition
The plate model during Navratri should include all the food groups with a wisely and timely distribution of carbohydrates throughout the day. Complex carbohydrates and low caloric fluids and beverages have a low glycemic index than simple carbohydrates and concentrated beverages and hence should be preferred. Adequate fluid intake will help hydrate the body and prevent dehydration. Optimum physical activity during nonfasting periods and 15–20 min walk followed by major meal (at the end of fast) is beneficial.
Carbohydrate
An optimally required serving of cereals, the food group which majorly contributes to the carbohydrates, should be included in plate from the grains which are permitted in the fasts to provide adequate glucose and energy for the vital organs to work. It is metabolically essential to provide approximately 50%–60% of the total kilocalories per day from carbohydrates.[20] Foods with higher glycemic index would adversely affect the body weight besides increasing blood sugar levels, production of free fatty acids in the late postprandial state and insulin resistance.[21] During fasting preparations, cereals should be combined with other food groups including more of vegetables, dietary fiber and lesser amount of oils to reduce the glycemic load of the meals.[22] However, the common dishes prepared at home or available as special Navratri thalis at hotels and restaurants comprise fried or oily preparations made of Makhane or any other dry fruit vegetable, sawan special rice, curd potato, sweet potato chaat, banana chips, cereal preparations of sabudana/singhara/kuttu.[1,3] The preferable methods of cooking are grilling, boiling, steaming, toasting, baking, etc. over oily preparations.[2]
Protein
Approximately 15%–20% of the total energy should be met from the protein to meet the daily dietary allowances (varies from person to person).[23,24,25] The guidelines for protein recommendation changes for individuals with diabetic ketoacidosis where it is restricted to some amount depending on glomerular filtration rate. Along with the avoidance of specific grains, onion and garlic, an important food group of pulses and legumes and other nonvegetarian sources of protein are often abstained during fasts and religious occasions. These are believed to extinguish the surrounding negative energies.[3] Selection of low-fat dairy products such as milk, curd, paneer and preparations such as sugar-free shakes, naturally flavored milk including Indian spices, lassi, chaach, mattha, vegetable raita, and paneer preparations and serving of nuts should be included as a good protein source in the diet of Hindus during fasting.
Fat
There should be a total contribution of ≤30% of calories from fat per day.[26] The studies support the idea of significant reduction of glycated hemoglobin (HbA1c) with lower-fat, moderate-carbohydrate and higher-fiber diet in adults with poor glycemic control, Therefore it is advised to include the similar composition of meals during fasting.[20] In addition, the specific fatty acid or fatty acid composition of the oils and fats plays an important role in the diets of diabetic people. It is preferred to include <10% saturated fats and cholesterol to <300 mg/day.[20,26] Further scientific research work may declare that lowering saturated fatty acids or increasing monounsaturated fatty acids may increase glucagon-like peptide-1 activity, thereby reducing postprandial transglucosidase. Furthermore, omega-3 fatty acids (good sources being flaxseeds, generally allowed during fasting) have been associated with reduction in cardiovascular disease risk biomarkers in type 2 diabetes. Nuts can serve as an optimum meal during fasting being good source of protein, micronutrients, unsaturated fatty acids and its substitution with starch has shown improve HbA1c and serum lipids.[27]
Vitamins and minerals
Inclusion of fruits and vegetables increases concentration of plasma carotenoids and Vitamin C to provide antioxidants and phytochemicals.[28,29] Combining fibrous vegetables with high carbohydrate and fat rich meals may help lower the glycemic load and thereby postprandial glucose.[20] Whole fruits with pulp, fresh vegetables and fiber should be chosen instead of concentrated juices.[10] Whole fruits and specifically green leafy vegetables are low in energy density, low glycemic load, higher fiber and micronutrient content showing beneficial effects on serum total and LDL cholesterol concentrations.[30,31] Fruit chaat, salads, custards, ice creams, shakes, and vegetable lassi containing natural fruit sweetness and vegetables are better options of frequent in-between minor meals than juices and sugary preparations.
Fiber
A desirable intake of about 25 g/1000 kcal or 30–40 g fiber per day should also be maintained in the days of fasting and feasting when the diet pattern and meals bear most of the modifications for adequate blood glucose control.[32]
Water and fluids
It is beneficial to include low-calorie beverages and drinks such as lemon water, green tea, lassi, chacch, mattha, pudina water, jal-jeera, etc., to quench thirst, especially during summer season. The sugary preparations if done during fasting should be included on the basis of calorie consumption as cultural practices may restrict other usual sources of carbohydrates specifically cereals.[9]
Herbs and spices
Herbal medicine is a rapidly growing field in both developing as well as developed countries, but scientific data are yet controversial about its health impact. India has been called as Botanical garden of the world with about 2500 species from India out of 21,000 herbal plants being listed by the World Health Organization. Because of their natural origin, antioxidant effects and medicinal properties, such herbs and spices are often added in different recipes during Navratri to improve the flavor, taste and beneficial effects on blood glucose levels. They can be added in tea, milk and milk preparations, and other beverages and recipes instead of sugars and other sweeteners to improve palatability of meals. There is literature supporting that many such herbs may have role in stimulation of insulin secretion from beta cells of islets or/and inhibition of insulin degradative processes, reduction in insulin resistance, stimulation of glycogenesis and hepatic glycolysis, improvement in digestion along with reduction in blood glucose and urea, prevention of pathological conversion of starch to glucose, inhibition of β-galactocidase and α–glucocidase, and also cortisol-lowering activities.[33,34] Oral administration of the fruits of bitter gourd (momordicacharantia) and ivy gourd (cocciniaindica) has shown insulin secretagogue effect and is influential on the enzymes involved in glucose metabolism.[35]
Meal quantity
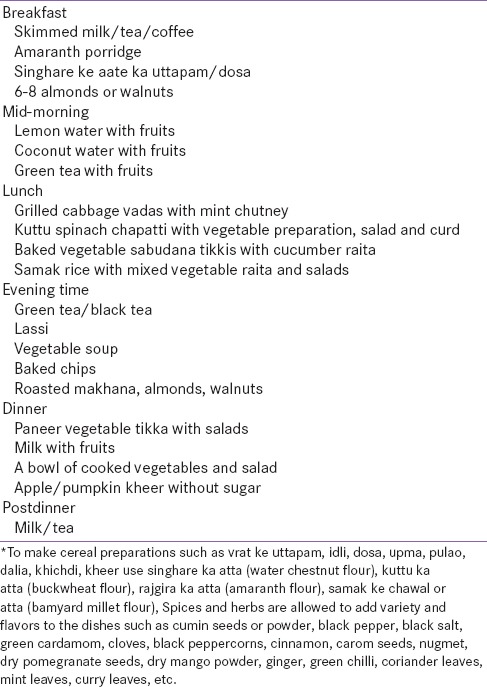
Patients are advised to eat small frequent meals at the intervals of approximately 3 h choosing healthier options among the foods allowed during fasting instead of the large meals usually taken at the end of fasting often containing high carbohydrates, fats, sugars and calorie-rich foods including fizzy drinks and fruit juices which can lead to hyperglycemia and faulty fluctuations in blood glucose levels.[2,36,37] Patients are advised to limit simple sugars and products containing so. Standardized calorie-level meal pattern with a specified percentage of carbohydrate, protein and fat based on exchange lists and food stuffs allowed to be eaten during fasting can be helpful to plan complete balanced meals on individual basis.[15] The planning of menus for such days is a laborious task for people with diabetes and hence a sample menu can be an exemplar for planning nutritious meals [Table 3].
Table 3.
Sample menu options for diabetics during Navratris
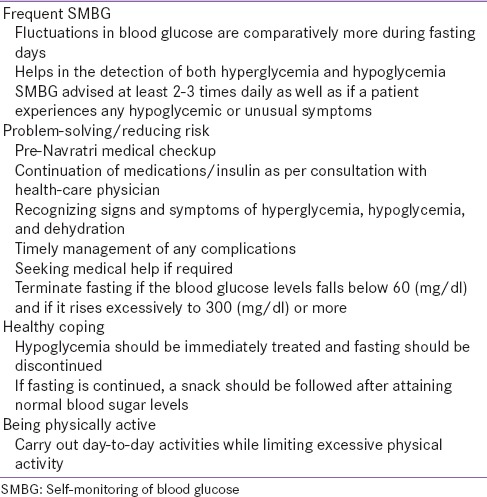
Educational counseling
The need for intensive education before fasting, clear and universal guidelines was felt necessary in Dhahira region, Oman, during Ramadan.[26] Patients and family members must receive the necessary education concerning self-care, including signs and symptoms of hyper and hypoglycemia, blood glucose monitoring, meal planning, physical activity, medication administration, and management of acute complications. The usual pattern of breaking the fast with one major meal should be replaced with small frequent meals, snacks, or beverages prepared from the food products allowed during fasting.[5] Importance of adequate nutrition and hydration should be well emphasized. A very important part of education is ability of the patients and family members to identify and treat hypoglycemia, even if it is mild. In addition, they should be prepared to break the fasts in case of any medical complications including hypoglycemia and seek medical care if required. Few simple measures for successful fasting during Navratris are summarized in Table 4.
Table 4.
Suggested measures for successful fasting during Navratri for diabetic people
CONCLUSION
No religion makes it mandatory for the vulnerable group to fast. However, for persons with well controlled diabetes, who do not wish for exemption from the religious and cultural values of the society, fasts can be managed with the proper dietary advice and adequate lifestyle practices. The team of physician, dietician, and diabetic educator should collectively be consulted before fasting to prevent medical complications and improve glycemic management. The nutritional plans should be individually modified according to the recommendations and daily dietary allowances for such occasions with inclusion of type of foods allowed to be taken during fasting, individual perspectives, religious and cultural food beliefs, dietary preferences and cooking practices, and suitability to meal timings. In addition, awareness should be facilitated among family members, community, and society for the effective management of diabetes in the cultural and religious occasions. Furthermore, healthy diets should be promoted for everyone including family members to reduce social exclusion of diabetic people for dietary reasons.
The quest for the scientific researche on dietary advice for Hindu fasts including Navratris shows the paucity of literature comparative to the dietary advices advocated during Ramadan. The scientific evidence about dietary advice and practices during Navratri is always promoted for Hindu culture. This review is based more on our clinical experience and extrapolation of data rather than robust scientific data. There is need for research in this social field, pertaining to the impact of fasting in Hinduism on metabolic and glycemic health, which in turn will create evidence based approaches to help manage this clinical challenge.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Akbani MF, Saleem M, Gadit WU, Ahmed M, Basit A, Malik RA. Fasting and feasting safely during Ramadan in the patient with diabetes. Pract Diabetes Int. 2005;22:100–4. [Google Scholar]
- 2.Kalra S, Bajaj S, Gupta Y, Agarwal P, Singh SK, Julka S, et al. Fasts, feasts and festivals in diabetes-1: Glycemic management during Hindu fasts. Indian J Endocrinol Metab. 2015;19:198–203. doi: 10.4103/2230-8210.149314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birdie AK. Impact of Navratras festival on the subjective wellbeing of vegetarian customers in hospitality sector. Int J Soc Sci Manage. 2015;2:333–8. [Google Scholar]
- 4.Sircar AR, Sircar S, Sircar J, Misra S. Patients’ concepts and attitudes about diabetes. J Diabetes Complications. 2010;24:398–403. doi: 10.1016/j.jdiacomp.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 5.Almalki MH, Alshahrani F. Options for controlling type 2 diabetes during Ramadan. Front Endocrinol (Lausanne) 2016;7:32. doi: 10.3389/fendo.2016.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Arouj M, Assaad-Khalil S, Buse J, Fahdil I, Fahmy M, Hafez S, et al. Recommendations for management of diabetes during Ramadan: Update 2010. Diabetes Care. 2010;33:1895–902. doi: 10.2337/dc10-0896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elhadd TA, Al-Amoudi AA. Recommendations for management of diabetes during Ramadan. Diabetes Care. 2006;29:744–5. doi: 10.2337/diacare.29.03.06.dc05-2102. [DOI] [PubMed] [Google Scholar]
- 8. [Last accessed on 2015 Aug 15]. Available from: http://www.mcb.org.uk/wp-content/uploads/2014/06/Ramadan-and-diabetes-A-guide-for-patients-2013.pdf .
- 9.Kelley DE. Sugars and starch in the nutritional management of diabetes mellitus. Am J Clin Nutr. 2003;78:858S–64S. doi: 10.1093/ajcn/78.4.858S. [DOI] [PubMed] [Google Scholar]
- 10.Jaleel MA, Raza SA, Fathima FN, Jaleel BN. Ramadan and diabetes: As-Saum (The fasting) Indian J Endocrinol Metab. 2011;15:268–73. doi: 10.4103/2230-8210.85578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azizi F. Islamic fasting and health. Ann Nutr Metab. 2010;56:273–82. doi: 10.1159/000295848. [DOI] [PubMed] [Google Scholar]
- 12.Vasan SK, Karol R, Mahendri NV, Arulappan N, Jacob JJ, Thomas N. A prospective assessment of dietary patterns in Muslim subjects with type 2 diabetes who undertake fasting during Ramadan. Indian J Endocrinol Metab. 2012;16:552–7. doi: 10.4103/2230-8210.98009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trepanowski JF, Bloomer RJ. The impact of religious fasting on human health. Nutr J. 2010;9:57. doi: 10.1186/1475-2891-9-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Diabetes Association. Standards of medical care in diabetes-2016 abridged for primary care providers. Clin Diabetes. 2016;34:3–21. doi: 10.2337/diaclin.34.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schafer RG, Bohannon B, Franz MJ, Freeman J, Holmes A, McLaughlin S, et al. Translation of the diabetes nutrition recommendations for health care institutions. Diabetes Care. 2003;26(Suppl 1):S70–2. doi: 10.2337/diacare.26.2007.s70. [DOI] [PubMed] [Google Scholar]
- 16.Yannakoulia M. Eating behavior among type 2 diabetic patients: A poorly recognized aspect in a poorly controlled disease. Rev Diabet Stud. 2006;3:11–6. doi: 10.1900/RDS.2006.3.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bravis V, Hui E, Salih S, Mehar S, Hassanein M, Devendra D. Ramadan Education and Awareness in Diabetes (READ) programme for Muslims with type 2 diabetes who fast during Ramadan. Diabet Med. 2010;27:327–31. doi: 10.1111/j.1464-5491.2010.02948.x. [DOI] [PubMed] [Google Scholar]
- 18.Vaibhav A, Singh OP, Tripathi AK. The prevalence of diabetes mellitus its current treatment trends. Indian J Res. 2012;6:10–6. [Google Scholar]
- 19.Wangnoo SK, Maji D, Das AK, Rao PV, Moses A, Sethi B, et al. Barriers and solutions to diabetes management: An Indian perspective. Indian J Endocrinol Metab. 2013;17:594–601. doi: 10.4103/2230-8210.113749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wheeler ML, Dunbar SA, Jaacks LM, Karmally W, Mayer-Davis EJ, Wylie-Rosett J, et al. Macronutrients, food groups, and eating patterns in the management of diabetes: A systematic review of the literature, 2010. Diabetes Care. 2012;35:434–45. doi: 10.2337/dc11-2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Willett W, Manson J, Liu S. Glycemic index, glycemic load, and risk of type 2 diabetes. Am J Clin Nutr. 2002;76:274S–80S. doi: 10.1093/ajcn/76/1.274S. [DOI] [PubMed] [Google Scholar]
- 22.Kiehm TG, Anderson JW, Ward K. Beneficial effects of a high carbohydrate, high fiber diet on hyperglycemic diabetic men. Am J Clin Nutr. 1976;29:895–9. doi: 10.1093/ajcn/29.8.895. [DOI] [PubMed] [Google Scholar]
- 23.Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2003;26(Suppl 1):S51–61. doi: 10.2337/diacare.26.2007.s51. [DOI] [PubMed] [Google Scholar]
- 24.Franz MZ, Evert AB. Medical nutrition therapy for diabetes & hypoglycemia of nondiabetic origin. In: Krause's Food & the Nutrition Care Process. 13th ed. US: Elsevier Health Sciences; 2016. [Google Scholar]
- 25.Mann JI, De Leeuw I, Hermansen K, Karamanos B, Karlström B, Katsilambros N, et al. Evidence-based nutritional approaches to the treatment and prevention of diabetes mellitus. Nutr Metab Cardiovasc Dis. 2004;14:373–94. doi: 10.1016/s0939-4753(04)80028-0. [DOI] [PubMed] [Google Scholar]
- 26.Patel P, Mirakhur A, El-Magd KM, El-Matty AN, Al-Ghafri D. Type 2 diabetes and its characteristics during Ramadan in Dhahira Region, Oman. Oman Med J. 2007;22:16–23. [PMC free article] [PubMed] [Google Scholar]
- 27.Jenkins DJ, Kendall CW, Banach MS, Srichaikul K, Vidgen E, Mitchell S, et al. Nuts as a replacement for carbohydrates in the diabetic diet. Diabetes Care. 2011;34:1706–11. doi: 10.2337/dc11-0338. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 28.Carter P, Gray LJ, Troughton J, Khunti K, Davies MJ. Fruit and vegetable intake and incidence of type 2 diabetes mellitus: Systematic review and meta-analysis. BMJ. 2010;341:c4229. doi: 10.1136/bmj.c4229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamer M, Chida Y. Intake of fruit, vegetables, and antioxidants and risk of type 2 diabetes: Systematic review and meta-analysis. J Hypertens. 2007;25:2361–9. doi: 10.1097/HJH.0b013e3282efc214. [DOI] [PubMed] [Google Scholar]
- 30.Bazzano LA, Li TY, Joshipura KJ, Hu FB. Intake of fruit, vegetables, and fruit juices and risk of diabetes in women. Diabetes Care. 2008;31:1311–7. doi: 10.2337/dc08-0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nuttall FQ. Dietary fiber in the management of diabetes. Diabetes. 1993;42:503–8. doi: 10.2337/diab.42.4.503. [DOI] [PubMed] [Google Scholar]
- 32.Sahay BK. Dietary carbohydrate content in Indian diabetic patients. Med Update. 2012;22:235–9. [Google Scholar]
- 33.Modak M, Dixit P, Londhe J, Ghaskadbi S, Devasagayam TP. Indian herbs and herbal drugs used for the treatment of diabetes. J Clin Biochem Nutr. 2007;40:163–73. doi: 10.3164/jcbn.40.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dwivedi C, Daspaul S. Antidiabetic herbal drugs and polyherbal formulation used for diabetes: A review. J Phytopharmacol. 2013;2:44–51. [Google Scholar]
- 35.Platel K, Srinivasan K. Plant foods in the management of diabetes mellitus: Vegetables as potential hypoglycaemic agents. Nahrung. 1997;41:68–74. doi: 10.1002/food.19970410203. [DOI] [PubMed] [Google Scholar]
- 36.Dutta D, Biswas K, Sharma M, Maskey R, Baruah MP, Amin MF. Managing diabetes during Navratris with special focus on Durga pujas. J Soc Health Diabetes. 2015;3:84–8. [Google Scholar]
- 37.Sahay RK, Nagesh VS. Type 1 diabetes and fasting during Ramzan. J Soc Health Diabetes. 2016;4:11–6. [Google Scholar]


