Abstract
Background:
Total thyroidectomy (TT) is a commonly performed surgery and postoperative hypocalcemia is a major detriment to early discharge. The aim of this randomized controlled trial was to ascertain the usefulness of routine pre- and post-operative calcium and Vitamin D supplementation in prevention of hypocalcemia after TT.
Materials and Methods:
Sixty consecutive patients who underwent total or near TT from February 2013 to August 2014 were included in the study. They were randomly divided into two groups - Group 1 received oral calcium (500 mg every 6 h) and Vitamin D (calcitriol 0.25 mcg every 6 h) 7 days before and 7 days after the surgery; and Group 2 did not receive supplementation. Symptoms and signs of hypocalcemia were monitored. Calcium profile was measured pre- and post-operatively at 6, 12, 24, 48, 72 h, and on 30th day. Hypocalcemia after surgery was either symptomatic or laboratory documented. Serum calcium level ≤ 8.5 mg/dl was considered as laboratory hypocalcemia.
Results:
Twelve patients from Group 2, and 3 patients from Group 1 developed symptomatic hypocalcemia (P < 0.01). Laboratory hypocalcemia within postoperative 24 h was comparable between two groups, but more patients of Group 2 compared to Group 1 developed hypocalcemia at 48 h (6 and 13, respectively; P = 0.04) and at 72 h after surgery (5 and 14, respectively; P = 0.01). Twenty-four hours postoperative serum calcium level was significantly associated with grade of goiter, preoperative calcium, and nature of thyroid disease (benign or malignant). On multiple linear regression analysis, preoperative serum calcium was only independent variable significantly associated with development of 24 h post-TT hypocalcemia.
Conclusion:
Routine pre- and post-TT calcium and Vitamin D supplementation can significantly reduce postoperative hypocalcemia.
Keywords: Calcium supplementation, postoperative hypocalcemia, thyroidectomy, Vitamin D supplementation
INTRODUCTION
Total thyroidectomy (TT) is a commonly performed surgery worldwide.[1] It is the definitive management option for thyroid malignancies and also for benign diseases such as multinodular goiter symptomatic of compression.[2] In the hands of an experienced surgeon, it is a safe procedure. Main postoperative complications include bleeding, recurrent laryngeal nerve injury, and hypocalcemia depending on the extent of surgery and experience of the surgeon. The incidence of transient hypocalcemia, defined as hypocalcemia occurring within 6 months of surgery, has been variedly reported to be 13%–38%.[3,4] It occurs because of transient hypoparathyroidism due to parathyroid gland manipulation or impairment of its blood supply. The development of postoperative hypocalcemia after TT is unfavorable not only since it is a cause of morbidity but also because it occurs 24–72 h postoperatively and hence necessitates repeated biochemical testing and prolonged in-hospital stay. Many risk factors have been identified for postoperative hypocalcemia including age >50 years, female gender, thyroid malignancy, Grave's disease, lymph node dissection, nonidentification of parathyroid glands intraoperatively, reoperation, and Vitamin D deficiency.[5,6,7] The prediction of patients who can be discharged early or those who would require close monitoring and postoperative calcium and Vitamin D supplementation is difficult. Although 1-h and 4-h postoperative intact parathormone (iPTH) testing has been shown to stratify patients into high- and low-risk for hypocalcemia and expedite an early discharge after TT,[8,9,10] rapid iPTH measurement facility is not routinely available in many resource-poor settings and is hence not feasible.
A high prevalence of Vitamin D deficiency has been demonstrated in some North Indian states,[11] and is a known risk factor for postoperative hypocalcemia after TT.[5,6,7] To prevent postoperative hypocalcemia, routine Vitamin D supplementation as a standard protocol merits consideration. Although routine postoperative oral calcium and Vitamin D supplementation has been shown to prevent the development of hypocalcemia after TT and facilitate an early discharge,[12,13] the role of preoperative supplementation has seldom been tested.[14] We hypothesize that a 1-week preoperative Vitamin D and calcium supplementation to a cohort of patients belonging to an area endemic to Vitamin D deficiency, continued 1 week into postoperative period, would reduce the rates of hypocalcemia and associated morbidity. The aim of the present randomized controlled trial was to ascertain the usefulness of pre- and post-operative calcium and Vitamin D supplementation in prevention of hypocalcemia after TT.
MATERIALS AND METHODS
This prospective randomized controlled study was performed, from February 2013 to August 2014, on sixty consecutive patients who underwent total or near TT in the department of General and Minimal Invasive Surgery in collaboration with Endocrinology Department. Prior Ethical Committee approval was sought and each patient gave an informed written consent before being enrolled in the study. The included patients had no history of prior thyroid or neck surgery. Those patients who underwent lobectomy or sub-TT were excluded from the study. All the patients had normal renal function before surgery. Preoperatively, patients were randomly divided into two groups, Group 1 received oral calcium and Vitamin D and Group 2 did not receive supplementation. Randomization was done by alternatively assigning consecutive patients to Group 1 or 2. Patients in the supplemented group were given oral calcium 500 mg every 6 h and calcitriol 0.25 µg every 6 h (Shelcal CT, Elder Pharma., Mumbai India) starting 7 days before surgery and continued for 7 days postoperatively. Patients who did not receive any supplement were given therapy only when symptomatic hypocalcemia developed. The symptoms and signs of hypocalcemia that were monitored included paresthesia of fingertips and perioral area, tetany, neuropsychiatric manifestations, Chvostek and Trousseau signs, and electrocardiogram evidence of prolonged corrected QT interval by Bazett's formula. This monitoring was done by the surgical team. If severe hypocalcemia symptoms developed, intravenous calcium gluconate was given.
Identical surgical techniques were used for thyroidectomy for all patients. TT was performed by experienced surgeons who were blinded as to which group the patients belonged. This was done so as to avoid bias in reporting and treating symptomatic hypocalcemia. During the surgical procedure, the recurrent laryngeal nerves and all parathyroid glands were routinely identified. If all four parathyroid glands could not be observed during surgery, then the TT specimen was postoperatively examined for the missing gland. Four patients in whom vascularity of parathyroid glands was compromised, parathyroid autotransplantation was done in the sternocleidomastoid muscles. Segment of fascia lying over the sternocleidomastoid muscle was dissected away. The parathyroid glands were cleaned off all fat, sliced into pieces of size 1 mm × 3 mm, placed in saline, and finally implanted into the muscle pockets. Three to four slices of parathyroid tissue were grafted into single pocket and closed with a silk suture.
Serum calcium, magnesium, phosphate, albumin, creatinine were measured pre- and post-operatively at 6, 12, 24, 48, 72 h and then on follow-up on 30th day. All these biochemical measurements were done by Beckman Coulter AU680 laboratory analyzer by standardized technique. The reference range for serum calcium was 8.5–10.5 mg/dl. Hypocalcemia after surgery was either symptomatic or laboratory hypocalcemia. Serum calcium level ≤ 8.5 mg/dl was considered as laboratory hypocalcemia. This study needed minimum 3 days of hospitalization of patients to perform required tests. After being discharged from the hospital, patients were followed at day 30th of surgery at which time serum calcium and phosphate levels were again measured.
Statistical analysis
Results are reported as the median (range) or mean ± standard deviation. The primary outcome measure was the presence of postoperative hypocalcemia. Paired t-test was used for comparison of paired samples, the Student's t-test was used for comparison of continuous variables between different groups, and Chi-square test was used for categorical data analysis. P value was calculated as two-tailed and value <0.05 was considered as statistically significant. In another analysis, Pearson's correlation coefficients were calculated between serum calcium at 24 h postoperatively and age, sex, weight, body mass index, grade of goiter, type of thyroid disease, and preoperative serum calcium level. Of those variables found to be significantly associated with 24 h postoperative serum calcium, a multiple linear regression model was constructed and independently associated variables were ascertained. All analyses were performed by Statistical Package for Social Sciences statistical software version 20 (IBM SPSS Statistics for Windows, Version 20 Armonk, NY: IBM Corp).
RESULTS
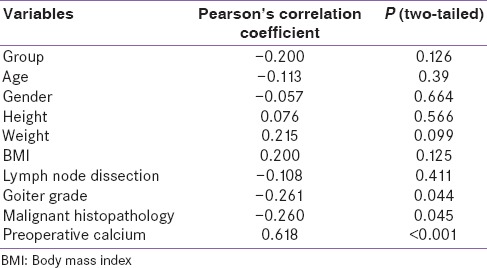
During the study period, sixty consecutive patients referred for TT were recruited. They were randomly assigned to Group 1 or 2. Baseline characteristics of patients belonging to the two groups are shown in Table 1. The mean age, sex ratio, type of thyroid disease, surgical procedure performed, and preoperative calcium profiles were comparable between the two groups. Twelve patients from Group 2, and 3 patients from Group 1 [Table 2] developed symptomatic hypocalcemia (P < 0.01). Laboratory hypocalcemia within postoperative 24 h was comparable between two groups, but more patients of Group 2 compared to Group 1 developed hypocalcemia at 48 h (6 and 13 respectively; P = 0.04) and at 72 h after surgery (5 and 14 respectively; P = 0.01) [Figure 1]. Intravenous calcium was given to four patients who developed tetany and all these belonged to Group 2. Hypercalcemia or other side effects did not develop in any of the patients’ receiving oral calcium and Vitamin D. Total calcium levels were lower in the group who did not receive any supplement than in the supplemented group [Table 2]. In another analysis, we found that 24 h postoperative serum calcium level was significantly associated with grade of goiter, preoperative calcium level, and nature of thyroid disease (benign or malignant). The association was negative for grade of goiter and malignant disease while it was positive for preoperative calcium. The Pearson's correlation coefficients and two-tailed P values are depicted in Table 3. On multiple linear regression analysis, preoperative serum calcium was the only independent significant variable in the development of 24 h post-TT hypocalcemia (standard coefficient β =0.62; P < 0.001) while grade of goiter approached significance (β = −0.226; P = 0.056). The risk of 24 h post-TT hypocalcemia was increased 2.78-fold for patients who had a preoperative calcium <9.00 mg/dl (odds ratio 8.14; 95% confidence interval 1.47–45.18).
Table 1.
Baseline characteristics of supplemented (Group 1) and not supplemented (Group 2)
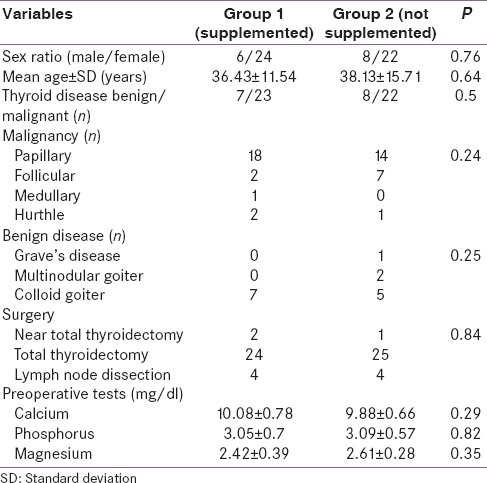
Table 2.
Postoperative calcium levels and hypocalcemia in supplemented (Group 1) and not supplemented (Group 2)
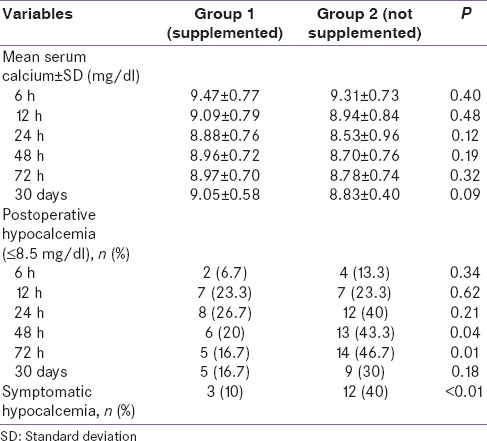
Figure 1.
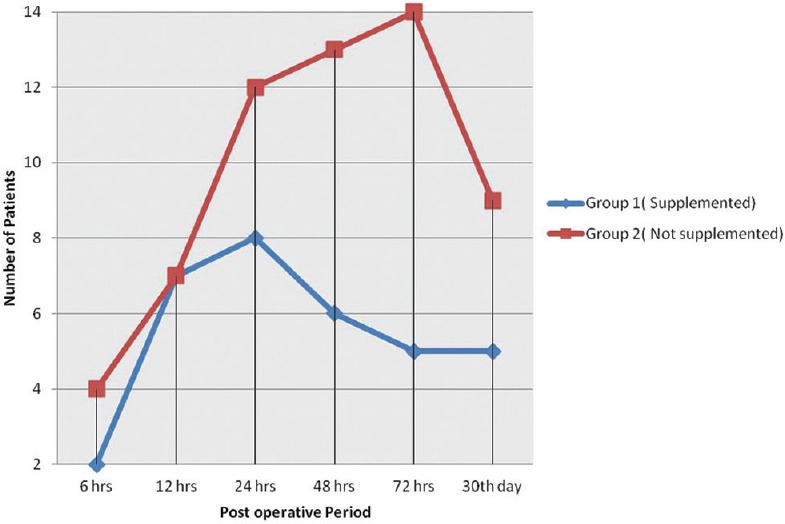
Number of patients developing hypocalcemia in the two groups
Table 3.
Correlation between 24 h postoperative calcium and other parameters
DISCUSSION
In this randomized controlled study, we have shown that 7 day preoperative oral calcium and Vitamin D supplementation continued into the postoperative period after TT significantly reduced laboratory and symptomatic hypocalcemia. Moreover, the need for intravenous calcium administration due to carpopedal spasm was completely eliminated in the supplemented group while four patients of the control group required the same. Although the improvement in calcemia at all tested post-TT time points was modest, it did not reach statistical significance. This may be explained by the small sample size and it would be constructive to include more patients in each group to elicit statistically significant results. Hence, our study suggests the role of routine pre- and post-operative oral calcium and Vitamin D supplements in decreasing the incidence and severity of hypocalcemia after TT although it does not completely eliminate the occurrence of postoperative hypocalcemia.
The literature is replete with studies evaluating the effect of post-TT calcium and Vitamin D supplementation on hypocalcemia. Moore[12] administered calcium at a dosage of 5 g/day to patients after bilateral thyroid resection and found that only 4 of 124 patients developed hypocalcemia and one required administration of intravenous calcium. Hence, he recommended prophylactic use of oral calcium to reduce the risk of hypocalcemic crisis and increase the likelihood of early hospital discharge. Bellantone et al.[15] conducted a prospective control study and reported that only 3 of 26 patients (11%) receiving oral calcium supplement (3 g/day) had symptoms related to hypocalcemia after TT, whereas 11 of 27 patients (40%) not receiving calcium supplement had symptoms. They also showed that the addition of Vitamin D to oral calcium supplements was associated with significantly higher serum calcium concentrations on postoperative day 2 and 3, with a lower incidence of hypocalcemia. Therefore, they recommended the early use of Vitamin D in addition to calcium supplement in patients undergoing TT. These studies suggest that hypocalcemia after thyroidectomy can be prevented by routine administration of calcium supplements. A systematic review and meta analysis on nine such studies also showed a significant decrease in postoperative hypocalcemia in patients who received routine supplementation of oral calcium or Vitamin D.[16] The incidence decreased even more with the combined administration of both supplements. However, the effect of preoperative calcium and Vitamin D has seldom been tested. Docimo et al.[14] supplemented fifty consecutive patients undergoing TT with pre- and post-operative calcium and Vitamin D. They found the incidence of symptomatic hypocalcemia to be 6% and that of laboratory hypocalcemia to be 10%. No permanent hypocalcemia developed. This study was poorly conceived in that no control group was included in it. In another prospective study, patients with Graves’ disease managed over a 9-month period took 1 g of calcium carbonate three times a day for 2 weeks before TT.[17] Postoperatively, patients with untreated Graves’ disease had lower serum calcium levels than pretreated patients or control subjects without Graves’ disease. This study had a disadvantage that population was limited to patients with Graves’ disease only. Given these limitations, we designed the current study, whereby a control group with comparable attributes to the study group was chosen, patients had different indications of undergoing thyroidectomy, and the study group was supplemented with 7 day pre-TT calcium and Vitamin D.
The dosage and duration of calcium and Vitamin D intake are also of concern. In the study by Moore,[12] patients were given oral calcium on an empirical basis as 5 g/day for 2 weeks. On this dose, one elderly patient became lethargic and developed hypercalcemia. In the trial conducted by Bellantone et al.,[15] the dosage of calcium was 3 g/day and Vitamin D was 1 µg/day for 7 days after surgery and it did not lead to any complication. In our study, oral calcium 2 g/day and calcitriol 2 µg/day were given preoperatively for 1 week and continued 1 week postoperatively. Hypercalcemia and other side effects were not observed in any patient. We found that 24 h postoperative serum calcium level was significantly associated with grade of goiter, preoperative calcium level, and nature of thyroid disease (benign or malignant). However, pre-TT serum calcium was the only independent association of 24 h post-TT hypocalcemia. It is likely that low normal calcium levels were the result of Vitamin D deficiency, which itself has been shown to be one of the factors associated with post-TT hypocalcemia.[18] The idea central to the inception and implementation of this study was the simplicity of its design and thus its applicability to resource-poor settings where iPTH and 25-hydroxy Vitamin D tests are not routinely available. Although iPTH testing has been shown to stratify patients into high- and low-risk for hypocalcemia and expedite an early discharge after TT,[8,9,10] its role in prevention of hypocalcemia is not clear. We consider iPTH measurement to be of limited utility in evaluating the efficacy of routine perioperative calcium and Vitamin D supplementation for prevention of hypocalcemia. We also did not measure Vitamin D in our patients given the fact that the prevalence of its deficiency is reported to be as high as 83% in our population.[11] We intended to test the protocol of its routine perioperative supplementation and its side effects if any.
CONCLUSION
The results of this study indicate that routine pre and post TT calcium and Vitamin D supplementation can significantly reduce post operative hypocalcemia. We, therefore, suggest the same in the prevention of post TT hypocalcemia, which ultimately can also decrease prolonged hospitalization of patients and costs associated with multiple blood sampling.
Limitations
Although the cause of hypocalcemia after TT is hypoparathyroidism, we did not test for PTH to document it. Moreover, role of Vitamin D deficiency in causation of hypocalcemia after surgery is not clear from the present study as we did not measure Vitamin D levels either.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Karamanakos SN, Markou KB, Panagopoulos K, Karavias D, Vagianos CE, Scopa CD, et al. Complications and risk factors related to the extent of surgery in thyroidectomy. Results from 2,043 procedures. Hormones (Athens) 2010;9:318–25. doi: 10.14310/horm.2002.1283. [DOI] [PubMed] [Google Scholar]
- 2.Ho TW, Shaheen AA, Dixon E, Harvey A. Utilization of thyroidectomy for benign disease in the United States: A 15-year population-based study. Am J Surg. 2011;201:570–4. doi: 10.1016/j.amjsurg.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 3.de Roy van Zuidewijn DB, Songun I, Kievit J, van de Velde CJ. Complications of thyroid surgery. Ann Surg Oncol. 1995;2:56–60. doi: 10.1007/BF02303703. [DOI] [PubMed] [Google Scholar]
- 4.Chia SH, Weisman RA, Tieu D, Kelly C, Dillmann WH, Orloff LA. Prospective study of perioperative factors predicting hypocalcemia after thyroid and parathyroid surgery. Arch Otolaryngol Head Neck Surg. 2006;132:41–5. doi: 10.1001/archotol.132.1.41. [DOI] [PubMed] [Google Scholar]
- 5.Puzziello A, Rosato L, Innaro N, Orlando G, Avenia N, Perigli G, et al. Hypocalcemia following thyroid surgery: Incidence and risk factors. A longitudinal multicenter study comprising 2,631 patients. Endocrine. 2014;47:537–42. doi: 10.1007/s12020-014-0209-y. [DOI] [PubMed] [Google Scholar]
- 6.Thomusch O, Machens A, Sekulla C, Ukkat J, Lippert H, Gastinger I, et al. Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: Prospective multicenter study in Germany. World J Surg. 2000;24:1335–41. doi: 10.1007/s002680010221. [DOI] [PubMed] [Google Scholar]
- 7.Thomusch O, Machens A, Sekulla C, Ukkat J, Brauckhoff M, Dralle H. The impact of surgical technique on postoperative hypoparathyroidism in bilateral thyroid surgery: A multivariate analysis of 5846 consecutive patients. Surgery. 2003;133:180–5. doi: 10.1067/msy.2003.61. [DOI] [PubMed] [Google Scholar]
- 8.AlQahtani A, Parsyan A, Payne R, Tabah R. Parathyroid hormone levels 1 hour after thyroidectomy: An early predictor of postoperative hypocalcemia. Can J Surg. 2014;57:237–40. doi: 10.1503/cjs.008013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Le TN, Kerr PD, Sutherland DE, Lambert P. Validation of 1-hour post-thyroidectomy parathyroid hormone level in predicting hypocalcemia. J Otolaryngol Head Neck Surg. 2014;43:5. doi: 10.1186/1916-0216-43-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grodski S, Lundgren CI, Sidhu S, Sywak M, Delbridge L. Postoperative PTH measurement facilitates day 1 discharge after total thyroidectomy. Clin Endocrinol (Oxf) 2009;70:322–5. doi: 10.1111/j.1365-2265.2008.03317.x. [DOI] [PubMed] [Google Scholar]
- 11.Zargar AH, Ahmad S, Masoodi SR, Wani AI, Bashir MI, Laway BA, et al. Vitamin D status in apparently healthy adults in Kashmir Valley of Indian subcontinent. Postgrad Med J. 2007;83:713–6. doi: 10.1136/pgmj.2007.059113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moore FD., Jr Oral calcium supplements to enhance early hospital discharge after bilateral surgical treatment of the thyroid gland or exploration of the parathyroid glands. J Am Coll Surg. 1994;178:11–6. [PubMed] [Google Scholar]
- 13.Genser L, Trésallet C, Godiris-Petit G, Li Sun Fui S, Salepcioglu H, Royer C, et al. Randomized controlled trial of alfacalcidol supplementation for the reduction of hypocalcemia after total thyroidectomy. Am J Surg. 2014;207:39–45. doi: 10.1016/j.amjsurg.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 14.Docimo G, Tolone S, Pasquali D, Conzo G, D’Alessandro A, Casalino G, et al. Role of pre and post-operative oral calcium and Vitamin D supplements in prevention of hypocalcemia after total thyroidectomy. G Chir. 2012;33:374–8. [PubMed] [Google Scholar]
- 15.Bellantone R, Lombardi CP, Raffaelli M, Boscherini M, Alesina PF, De Crea C, et al. Is routine supplementation therapy (calcium and Vitamin D) useful after total thyroidectomy? Surgery. 2002;132:1109–12. doi: 10.1067/msy.2002.128617. [DOI] [PubMed] [Google Scholar]
- 16.Alhefdhi A, Mazeh H, Chen H. Role of postoperative Vitamin D and/or calcium routine supplementation in preventing hypocalcemia after thyroidectomy: A systematic review and meta-analysis. Oncologist. 2013;18:533–42. doi: 10.1634/theoncologist.2012-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oltmann SC, Brekke AV, Schneider DF, Schaefer SC, Chen H, Sippel RS. Preventing postoperative hypocalcemia in patients with Graves disease: A prospective study. Ann Surg Oncol. 2015;22:952–8. doi: 10.1245/s10434-014-4077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tripathi M, Karwasra RK, Parshad S. Effect of preoperative Vitamin D deficiency on postoperative hypocalcemia after thyroid surgery. Thyroid Res. 2014;7:8. doi: 10.1186/1756-6614-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


