Abstract
Objective:
We aimed to determine perceived stress levels among adults aged >20 years with type 2 diabetes mellitus (DM) in a tertiary care diabetes center, Chennai, Tamil Nadu, India, assess their association with sociodemographic and clinical characteristics and assess the possible risk factors for stress and coping strategies.
Methods:
A mixed-methods (triangulation design) study with quantitative methodology (survey) and qualitative methodology (interviews) was carried out. Stress levels were assessed among type 2 DM patients attending a diabetes clinic using a 5-point perceived stress scale-10. One-on-one interviews were carried out with 376 participants with DM having high/very high stress levels to understand the reasons for perceived stress and explore their coping mechanisms.
Results:
The prevalence of high/very high stress was 35% among DM patients. Age 30–40 years, working in professional jobs, and lack of physical activity were factors significantly associated with stress. The perceived major stress inducers were related to family, work, financial issues, and the disease itself.
Conclusions:
This study showed high levels of stress in more than one-third of DM patients. Potential solutions include regular, formal assessment of stress levels in the clinic, providing integrated counseling and psychological care for DM patients, and promoting physical activity.
Keywords: Diabetes mellitus, India, perceived stress score, physical activity
INTRODUCTION
Diabetes mellitus (DM) is one of the most common noncommunicable diseases in the world. According to the International Diabetes Federation estimates, around 415 million people had DM in 2015 and this number is expected to rise to 642 million by 2040.[1] Around 75% of participants with DM live in low- and middle-income countries.[1] In financial terms also the global burden of DM is enormous, with an estimated annual expenditure in 2015 of USD$ 673 billion dollars, which constituted 12% of global health spending for that year.[1]
India with 69.1 million people is estimated to have the second-highest number of cases of DM in the world after China in 2015.[1] The prevalence of DM in India ranges from 5% to 17%, with higher levels found in the Southern part of the country.[2,3,4] DM continues to increase as a result of rapid cultural and social changes, which include aging populations, increasing urbanization, dietary changes, reduced physical activity, and unhealthy behaviors.[3,5] Historically, a disease of the affluent, recent epidemiological evidence indicates a rising DM incidence and prevalence in urban India's middle class and working poor.[6]
Individuals with chronic illnesses such as DM are reported to have comorbid unrecognized mental health disorders.[7] DM patients in India have one of the lowest levels of psychological well-being, based on the World Health Organization (WHO) Well-being Index, with 41% reported as having poor psychological well-being, especially among the lower-income group.[8] The International Diabetes Federation has also stressed the importance of integrating psychological care in the management of DM.[9] Stress may lead to deterioration of glycemic control through its effects on the neuroendocrine system, and it may impact indirectly because of a change in health-related behavior.[10,11] There is a general lack of understanding regarding the levels of stress, their associated characteristics, and the reasons for stress among DM patients.
The present study was carried out to determine perceived stress levels among adult participants (aged >20 years) with type 2 DM at Chennai, Tamil Nadu, India, to assess their association with sociodemographic and clinical characteristics, glycemic control, and comorbidities and assess the possible risk factors for stress and the possible coping strategies to manage stress.
METHODS
Study design
This was a mixed methods study of triangulation design with a cross-sectional quantitative component (survey) and a descriptive qualitative component (interviews).
General setting
Chennai, along the coast of the Bay of Bengal, is the capital city of the state of Tamil Nadu. It is the biggest industrial and commercial center in South India, and a major cultural, economic, and educational center. It is the sixth largest city and the fourth most populous metropolitan area in the country with more than 8 million people. Large-scale studies have shown a higher prevalence of DM in South India, especially in urban pockets such as Chennai, when compared to the rest of the country.[3,4]
Study population and sample size
For the quantitative component of the study, the study population consisted of new or already registered patients with type 2 DM attending tertiary diabetes center in Chennai during a 4-month period from January to April 2016. DM patients who were waiting in the general outpatient hall were randomly selected and interviewed after getting informed consent, and on an average 5–10 participants were interviewed a day. Those with a known medically diagnosed psychiatric illness in the past (verified with medical records), with any form of cognitive impairment such as dementia or mental retardation, any female in the postpartum period, and participants unable to give consent were excluded from the study. For the qualitative component of the study, patients with DM recorded as having high levels of stress on the perceived stress scale (PSS) had one-on-one interviews.
Based on 80% power, a Type I error of 0.05, assuming a prevalence of stress among type 2 DM patients to be 13%.[12] An absolute precision of 3% and a nonresponse of 10%, a sample size of 400 participants with DM was calculated.
Data variables and collection
Phase 1: Quantitative data collection
Sociodemographic characteristics, anthropometric, clinical and biochemical parameters, and specified comorbidities were collected as exposure variables from the electronic patient record system maintained in the hospital. Current smoking was defined as one or more cigarettes smoked in the last month and current alcohol drinking as any alcohol taken at any time in the last month. Body mass index (BMI) was calculated using the formula, weight in kg/height in square meters. Blood test measurements were taken as the last recorded blood test in the patient case files: high serum cholesterol was defined as ≥200 mg/dl and uncontrolled DM as glycated hemoglobin (HbA1c) >7.0%.
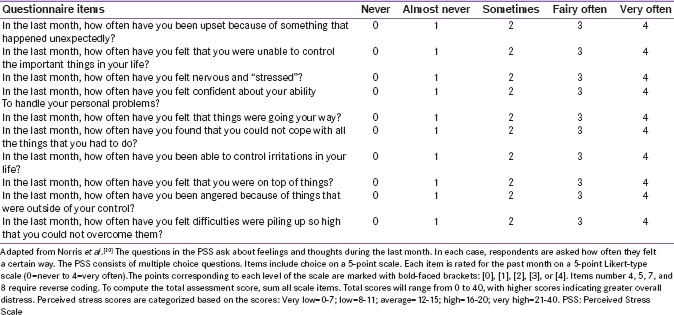
The outcome variable (perceived stress) was obtained using a 10-item PSS.[13] Respondents were asked questions about their feeling and thoughts during the last month, and they were also asked to indicate how often they felt these thoughts on a 5-point scale that ranged from 0 (never) to 4 (very often) [Box 1]. Participants with DM were then categorized into the following stress score levels: very low (score 0–7), low (score 8–11); average (score 12–15), high (score 16–20), and very high (score 21 up to 40).
Box 1.
Perceived stress scale-10
Phase 2: Qualitative data collection
Personal interviews were carried out on DM patients recorded as having high levels of stress (≥16 on the PSS) and willing to participate in the interviews to understand the possible risk factors for stress and explore their coping mechanisms. For the purpose of the study, coping was defined as the process of spending conscious effort and energy to minimize or tolerate stress and stressors that occur in everyday life.[14] Before each interview, the study details were explained to the participants. The interviews were conducted by an investigator who is well trained in qualitative research in the local language (Tamil). Each interview took 10–20 min. The participants were informed of the purpose of the study, and only the participant and the researcher were present during the interview. An interview guide with broad open-ended questions was used to conduct the interviews.
Analysis and statistics
Quantitative
Data were double-entered and validated in EpiData (version 3.1, EpiData Association, Odense, Denmark) and analyzed in EpiData analysis version 2.2.2.183. The Items numbers 4, 5, 7, and 8 were coded reversely in the PSS before analysis was done. The Chi-square test was used to study the association between sociodemographic and clinical variables and high or very high levels of perceived stress. Prevalence ratios (PRs) and their 95% confidence intervals were calculated to establish the strength of their association. Variables (age, occupation, and physical activity) showing associations at P ≤ 0.2 were then included in a multivariate regression model to calculate adjusted PRs. The level of significance was set at 5%.
Qualitative
The primary investigator noted down the proceedings of the interviews. Manual content analysis of the transcripts was done according to standardized guidance.[15,16] The participants’ responses were validated by the principal investigator. These were reviewed by a second investigator to reduce subjective interpretation. The findings were reported using “Consolidated Criteria for Reporting Qualitative Research (COREQ)” guidelines.[17]
Ethics
Permission for the study was obtained from the Institutional Ethics Committee of the Madras Diabetes Research Foundation (MDRF), Chennai and the Union Ethics Advisory Group, the International Union against Tuberculosis and Lung Disease, Paris, France. Informed consent was obtained from eligible DM patients and those consenting were interviewed.
RESULTS
Quantitative
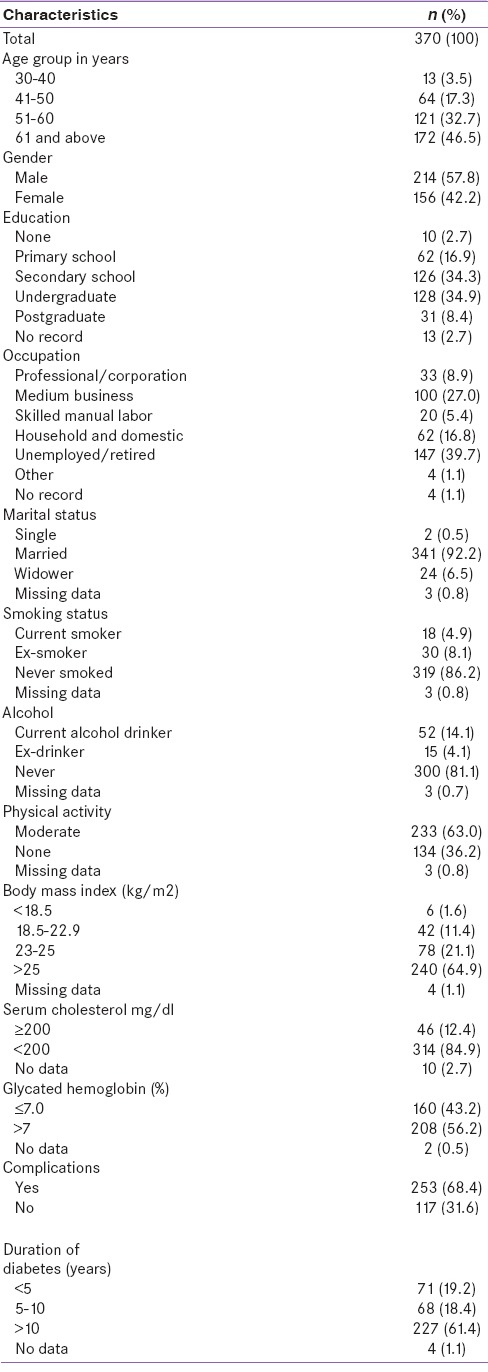
A total of 406 participants with DM were recruited and interviewed, but 36 were excluded due to some clinical information missing from the electronic data file. Patients with DM who were included in the study (The sociodemographic and clinical characteristics of the 367 participants) are shown in Table 1. Nearly half of the patients were aged 60 years and above, there were a higher proportion of males, 80% had been educated to secondary school level or above, 40% were unemployed/retired, and the majority was married. The majority of the participants had never smoked or drank alcohol and nearly two-thirds engaged in moderate exercise. Over 80% had normal cholesterol levels, over 50% had HbA1c concentrations >7.0%, over 60% had >25 BMI, and had more than 10 years of diabetes.
Table 1.
Sociodemographic and clinical characteristics of patients with diabetes mellitus attending a diabetes specialty hospital, Chennai, India: January to April 2016
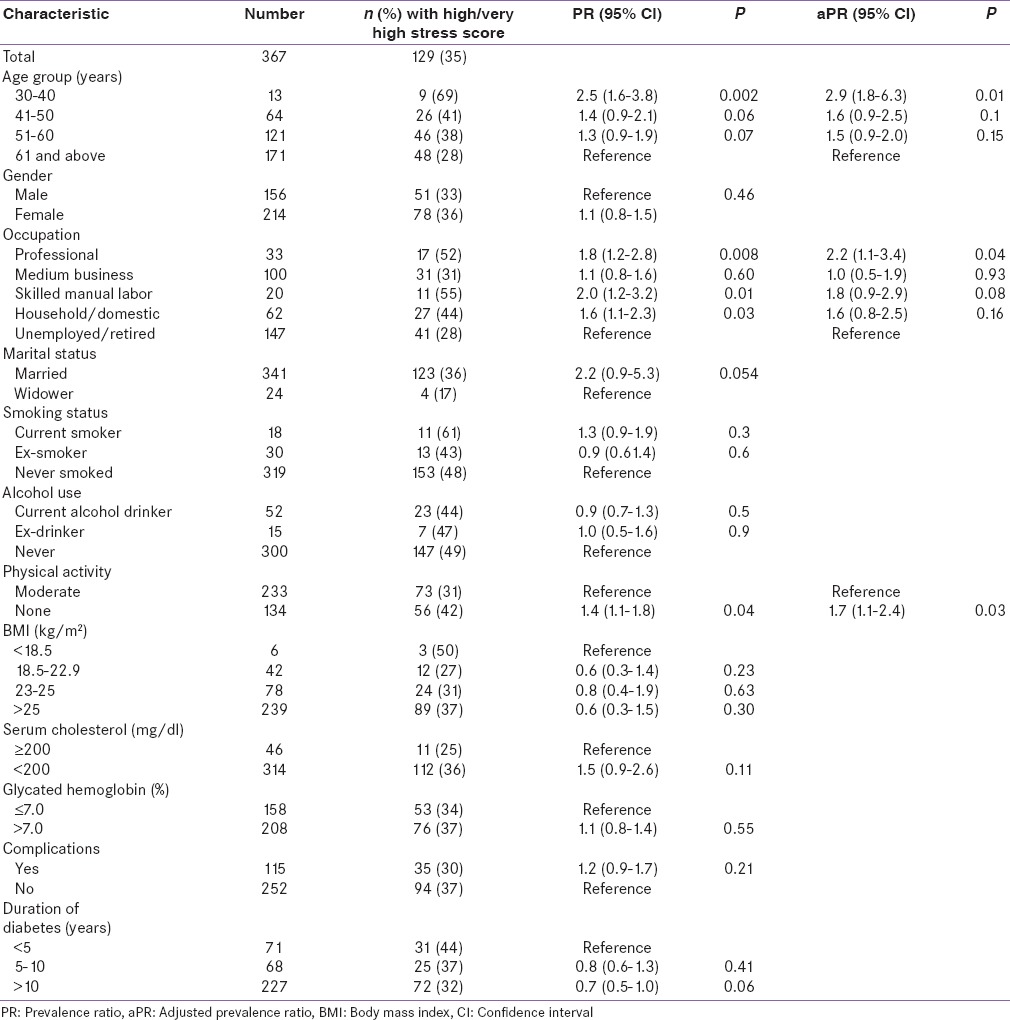
The distribution of perceived stress scores in the 367 participants with DM is shown in Figure 1. The scores ranged from 1 to 25. There were 118 participants (32%) with high scores and 11 (3%) with very high scores. Sociodemographic and clinical characteristics in association with high or very high stress scores are shown in Table 2. On univariate analysis, the factors significantly associated with high/very high stress were age 30–40 years, having a professional work, and lack of physical activity. After multivariate regression, age 30–40 years, working in a professional job, and lack of physical activity were still found to be significantly associated with high/very high stress.
Figure 1.
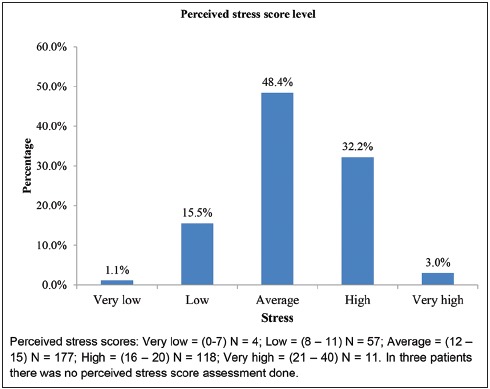
Perceived stress levels of persons with diabetes mellitus attending a diabetes specialty hospital, Chennai, Tamil Nadu, India: January to April 2016
Table 2.
Stratification of diabetes mellitus patients with stress based on various parameters
Qualitative
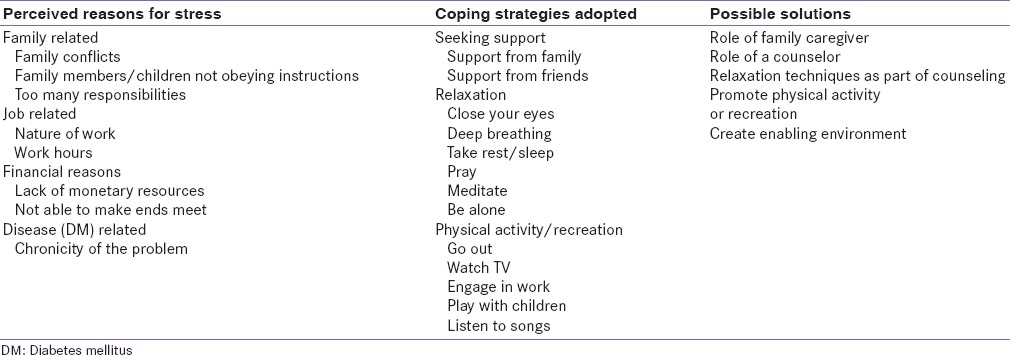
A total of 14 patients with DM were interviewed: Nine were males, and the mean age was 56 ± 14 years. Table 3 shows the major themes and reasons for stress and the coping strategies adopted during times of stress. Under perceived reasons for stress, the major themes were family-related (conflicts within the family, family members not obeying instructions, and too many responsibilities); job-related (nature of the work and working hours); financial (lack of monetary resources and not being able to make ends meet), and disease-related (chronicity of the illnesses). Four dominant ways of coping emerged: seeking support from family members and friends, various techniques of relaxation, physical activity, and recreation.
Table 3.
Major reasons for stress that emerged from the qualitative study and possible solutions
DISCUSSION
This study showed that 35% of DM patients seen in a tertiary diabetes care clinic in Chennai, Tamil Nadu, India report high to very high stress level. Being aged 30–40 years, working in professional jobs, and lack of physical activity were found to be significantly associated with stress in the study. These findings on the quantitative analysis were further confirmed through the one-to-one interviews where family conflict, workplace issues, financial concerns, and disease-related issues were noted to also contribute to high stress levels.
Earlier studies have shown the prevalence of stress among participants with DM to range from 12% to 23% although these studies have used different scales to measure stress levels.[12,18,19] These findings suggest that stress is a critical issue among participants with DM, and one that deserves to be identified and managed as part of comprehensive care.
Physical activity is known to promote feelings of well-being and reduce stress.[20] Several plausible mechanisms for how physical inactivity affects mental well-being have been proposed with the effects probably mediated through increased release of β-endorphins and brain neurotransmitters (e.g., serotonin, dopamine, and norepinephrine).[21] In our study, it was apparent that participants who indicated no physical activity were at risk of high levels of stress. This is in line with other studies showing positive associations between lack of physical activity and poor mental well-being such as stress, depression, and anxiety.[12,21,22,23] Physical activity and recreation were also reported as a coping strategy by patients with DM having stress.
In our study, participants engaged in professional jobs or business were found to have higher stress levels, similar to what has been found in other studies.[18,24,25] These findings were also verified through the one-on-one interviews during which job-related factors were recognized and acknowledged as one of the major reasons for stress.
Stress due to the disease itself, i.e., DM, was reported by some participants. This was found to be common, and providers generally recognized that patients were concerned about the chronic and potentially long-term complications of the disease and that these issues interfered with their self-management efforts.[8]
This study has several programmatic implications for a tertiary care clinic looking after patients with DM. First, given the prevalence of stress in the study population, all patients who attend the clinic should be formally and regularly assessed, maybe once a year, using simple instruments such as the perceived stress score system. This could help to identify those with high stress levels who need further attention. Second, special counseling services should be offered to those with high levels of stress, and these services could include advice about regular physical activity, teaching methods of relaxation, and further engaging the help of family and/or friends. Third, aggressive management of risk factors for cardiovascular or cerebrovascular disease would be of benefit to the whole clinic population, and one of these would be more attention given to help DM patients lose weight and engage in more exercise which may result in reducing disease-related comorbidity and mortality.[26,27]
The strengths of this study are that it is a mixed method methodology and the adherence to COREQ and Strengthening the Reporting of Observational Studies in Epidemiology guidelines in reporting of the study results.[17,28] There are, however, a few limitations. First, this being a cross-sectional design, causal pathways underlying the reported associations cannot be ascertained. Second, being a clinic-based study, referral bias could have affected the results. Finally, there was no control group, so we do not know whether the prevalence of stress levels is similar in the general population.
CONCLUSIONS
Nearly, one-third of the participants with DM seen at a tertiary diabetes clinic in Southern India had high stress levels. This underscores the need for psychological care and counseling at diabetes centers and people with diabetes in general.
Financial support and sponsorship
The training program and open access publications costs were funded by the Department for International Development (DFID), UK, The Union, MSF, and La Fondation Veuve Emile Metz-Tesch (Luxembourg). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the WHO/TDR. The model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union) and Medécins sans Frontières (MSF/Doctors Without Borders). The specific SORT IT programme which resulted in this publication was jointly developed and implemented by the Union South-East Asia Office, New Delhi, India; the Centre for Operational Research, The Union, Paris, France; the Operational Research Unit (LUXOR), MSF Brussels Operational Center, Luxembourg; Department of Preventive and Social Medicine, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India; Department of Community Medicine, Sri Manakula Vinayagar Medical College and Hospital, Puducherry, India; Department of Preventive and Social Medicine, Medical College, Baroda, Vadodara, Gujarat, India; and the National Institute for Research in Tuberculosis, Chennai, Tamil Nadu, India.
We thank the participants and the staff of Dr. Mohan's Diabetes Specialities Centre and the MDRF, Chennai, for their help with this study.
REFERENCES
- 1.International Diabetes Federation. IDF Diabetic Atlas. 7th ed. Brussels, Belgium: International Diabetes Federation; 2015. [Google Scholar]
- 2.Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125:217–30. [PubMed] [Google Scholar]
- 3.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 4.Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al. High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia. 2001;44:1094–101. doi: 10.1007/s001250100627. [DOI] [PubMed] [Google Scholar]
- 5.Ebrahim S, Kinra S, Bowen L, Andersen E, Ben-Shlomo Y, Lyngdoh T, et al. The effect of rural-to-urban migration on obesity and diabetes in India: A cross-sectional study. PLoS Med. 2010;7:e1000268. doi: 10.1371/journal.pmed.1000268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mendenhall E, Shivashankar R, Tandon N, Ali MK, Narayan KM, Prabhakaran D. Stress and diabetes in socioeconomic context: A qualitative study of urban Indians. Soc Sci Med. 2012;75:2522–9. doi: 10.1016/j.socscimed.2012.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ivbijaro GO. Mental health and chronic physical illnesses: The need for continued and integrated care. Vancouver: World Federation for Mental Health; 2010. [PMC free article] [PubMed] [Google Scholar]
- 8.Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychosocial problems and barriers to improved diabetes management: Results of the cross-national Diabetes Attitudes, Wishes and Needs (DAWN) study. Diabet Med. 2005;22:1379–85. doi: 10.1111/j.1464-5491.2005.01644.x. [DOI] [PubMed] [Google Scholar]
- 9.IDF Clinical Guidelines Task Force: Global Guideline for Type 2 Diabetes. Brussels: International Diabetes Federation; 2005. [Last accessed on 2016 Jul 22]. Available from: https://www.idf.org/sites/default/files/IDF%20T2DM%20Guideline.pdf . [Google Scholar]
- 10.Lloyd CE, Wing RR, Orchard TJ, Becker DJ. Psychosocial correlates of glycemic control: The Pittsburgh Epidemiology of Diabetes Complications (EDC) study. Diabetes Res Clin Pract. 1993;21:187–95. doi: 10.1016/0168-8227(93)90068-g. [DOI] [PubMed] [Google Scholar]
- 11.Surwit RS, van Tilburg MA, Zucker N, McCaskill CC, Parekh P, Feinglos MN, et al. Stress management improves long-term glycemic control in type 2 diabetes. Diabetes Care. 2002;25:30–4. doi: 10.2337/diacare.25.1.30. [DOI] [PubMed] [Google Scholar]
- 12.Kaur G, Tee GH, Ariaratnam S, Krishnapillai AS, China K. Depression, anxiety and stress symptoms among diabetics in Malaysia: A cross sectional study in an urban primary care setting. BMC Fam Pract. 2013;14:69. doi: 10.1186/1471-2296-14-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 14.Zeidner M, Endler NS, editors. Handbook of Coping: Theory, Research, Applications. New York: John Wiley; 1996. [Google Scholar]
- 15.Creswell J, Plano Clark V. Designing and Conducting Mixed Methods Research. London, United Kingdom: Sage Publications Ltd; 2007. pp. 142–5. [Google Scholar]
- 16.Kvale S. Doing Interviews. London, United Kingdom: Sage Publications; 2007. [Google Scholar]
- 17.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 18.Bhandary B, Rao S, Sanal TS. The effect of perceived stress and family functioning on people with type 2 diabetes mellitus. J Clin Diagn Res. 2013;7:2929–31. doi: 10.7860/JCDR/2013/7414.3689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdulbari B, Al-Hamaq AO, Dafeeah EE. High prevalence of depression, anxiety and stress symptoms among diabetes mellitus patients. Open Psychiatry J. 2011;5:5–12. [Google Scholar]
- 20.Norris R, Carroll D, Cochrane R. The effects of physical activity and exercise training on psychological stress and well-being in an adolescent population. J Psychosom Res. 1992;36:55–65. doi: 10.1016/0022-3999(92)90114-h. [DOI] [PubMed] [Google Scholar]
- 21.Craft LL, Perna FM. The benefits of exercise for the clinically depressed. Prim Care Companion J Clin Psychiatry. 2004;6:104–11. doi: 10.4088/pcc.v06n0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hong X, Li J, Xu F, Tse LA, Liang Y, Wang Z, et al. Physical activity inversely associated with the presence of depression among urban adolescents in regional China. BMC Public Health. 2009;9:148. doi: 10.1186/1471-2458-9-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khuwaja AK, Lalani S, Dhanani R, Azam IS, Rafique G, White F. Anxiety and depression among outpatients with type 2 diabetes: A multi-centre study of prevalence and associated factors. Diabetol Metab Syndr. 2010;2:72. doi: 10.1186/1758-5996-2-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rao JV, Chandraiah K. Occupational stress, mental health and coping among information technology professionals. Indian J Occup Environ Med. 2012;16:22–6. doi: 10.4103/0019-5278.99686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bolhari A, Rezaeian A, Bolhari J, Bairamzadeh S. Occupational stress level among information technology professionals in Iran. Int J Inf Electron Eng. 2012;2:682–5. [Google Scholar]
- 26.Snel M, Sleddering MA, Vd Peijl ID, Romijn JA, Pijl H, Meinders AE, et al. Quality of life in type 2 diabetes mellitus after a very low calorie diet and exercise. Eur J Intern Med. 2012;23:143–9. doi: 10.1016/j.ejim.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 27.Villareal DT, Chode S, Parimi N, Sinacore DR, Hilton T, Armamento-Villareal R, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364:1218–29. doi: 10.1056/NEJMoa1008234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med Public Libr Sci. 2007;4:e296. doi: 10.1371/journal.pmed.0040296. [DOI] [PMC free article] [PubMed] [Google Scholar]


