Abstract
Background
It is unclear whether health related quality of life (HRQL) may have a predictive value for mortality in idiopathic pulmonary fibrosis (IPF).
We investigated the relationship between HRQL assessed using the St. George’s Respiratory Questionnaire (SGRQ) and survival time in patients with IPF, and tried to determine a clinical meaningful cut off value to predict poorer survival rates.
Methods
We retrospectively analyzed consecutive patients with IPF who underwent an initial evaluation from May 2007 to December 2012. The diagnosis of IPF was made according to the 2011 international consensus guidelines. We used Cox proportional hazard models to identify independent predictors for mortality rate in patients with IPF.
Results
We examined 182 eligible cases, average age was 66 years old, and 86% were male. Mean levels of percent predicted FVC, DLco, six-minute-walk test distance, and the SGRQ total score were around 80%, 58%, 580 m, and 34 points. On multivariate analysis, the SGRQ total score (hazard ratio [HR], 1.012; 95% confidence interval [CI] 1.001–1.023; P = .029) and percent predicted FVC (HR, 0.957; 95% CI 0.944–0.971, P < .001) were independent predictors for mortality rate. Moreover, a score higher than 30 points in the SGRQ total score showed higher mortality rate (HR, 2.047; 95% CI, 1.329–3.153; P = .001).
Conclusions
The SGRQ total score was one of independent prognostic factors in patients with IPF. Total scores higher than 30 points were associated with higher mortality rates.
Trial registration
This study was retrospective, observational study, so it is not applicable.
Electronic supplementary material
The online version of this article (doi:10.1186/s12931-017-0503-3) contains supplementary material, which is available to authorized users.
Keywords: Health related QoL, Idiopathic pulmonary fibrosis, Prognostic factors, The St. George’s Respiratory Questionnaire
Background
Idiopathic pulmonary fibrosis (IPF) is a fatal lung disease characterized by chronic, progressive fibrosing interstitial pneumonia of unknown etiology [1]. As the disease condition progresses, dyspnoea on exertion becomes severe and health-related quality of life (HRQL) seriously deteriorates [2].
HRQL is a subjective and multidimensional appraisal that focuses on the impact of illness and treatment on physical, emotional, and social well-being [3]. HRQL tools can thus capture various information that physiologic or radiologic measures cannot. Therefore, it has been considered to be one of the most important endpoints in pharmacological trials and rehabilitation for IPF [4, 5].
The St. George’s Respiratory Questionnaire (SGRQ) is the most frequently used tool to measure HRQL. It was developed as a standardized, self-administered, disease-specific health status evaluation scale for patients with chronic obstructive disease [6]. The questionnaire consists of 50 items with 76 weighted responses that produce scores in three domains and one total score. The domains are symptoms (breathlessness, cough, and wheeze), activities (that are limited by the symptoms), and impacts (social and psychologic effect of the respiratory diseases). The score for each domain is calculated from 0 to 100, with higher scores corresponding to worse HRQL.
In patients with COPD, the SGRQ was shown to be a significant predictor of mortality [7, 8]. However, in patients with IPF, the relationship between HRQL assessed using the SGRQ and mortality has not fully been studied.
The aim of the present study was to investigate whether the SGRQ has a predictive value for mortality in IPF, including various dimensional clinical factors previously reported as prognostic factors, namely MMRC [9], % predicted FVC, % predicted DLco [1, 10–15], 6MWD, desaturation during 6MWT [13, 16–18], and BMI [19]. We also sought a clinically meaningful cut off value to predict poorer mortality rate.
Methods
Study subjects
Two-hundred and five consecutive patients with IPF, who underwent systemic initial evaluation from May 2007 to December 2012 at a center for respiratory diseases (Aichi, Japan), were identified from their medical records. The diagnosis of IPF was made according to the 2011 international consensus guidelines, and since 2011 the accuracy of the diagnosis has been confirmed by multidisciplinary discussion (MDD); however, some of the patients who initially presented before 2010 had been diagnosed based on different guidelines. The diagnosis for these patients was therefore confirmed according to the 2011 guidelines and MDD before May 2015 [1]. A thoracic radiologist with 27 years of experience re-read the chest high-resolution CT (HRCT) that had been obtained at the initial evaluation. This thoracic radiologist was blind to the clinical course and examination data for each patient.
Patients were excluded from the present study if there was clinical evidence of other known conditions, such as connective tissue disease, left heart failure, an occupational or environmental exposure that may result in interstitial lung disease, or a history of ingestion of an agent known to cause interstitial lung disease. Moreover, patients who had been prescribed medication for IPF (i.e. anti-fibrotic drug, corticosteroid, immunosuppressant), or who had undergone long-term oxygen therapy before initial evaluation at a center for respiratory diseases (Aichi, Japan) were also excluded. Finally, we examined 182 patients with IPF who were newly diagnosed. Of them, 55 patients who were in a clinical trial were enrolled. The present study was approved by a local institutional review board (IRB No. 509).
Data collection
Clinical data were retrospectively collected from a medical chart review. The eligible patients had undergone all of the tests and assessments that were physical examination and assessment of physiological function, dyspnoea (modified Medical Research Council (MMRC) scale and Baseline Dyspnoea Index (BDI) score), exercise capacity (6-minute-walk test (6MWT) and desaturation during 6MWT), and HRQL, which was assessed using the SGRQ [6] at the initial evaluation. The Japanese version of the SGRQ has been previously validated [20].
All patients completed pulmonary function tests (PFTs) by spirometry (CHESTAC-55 V; Chest, Tokyo, Japan), according to the ATS/ERS criteria [21]. Diffusion capacity for carbon monoxide (DLco) was also measured (CHESTAC-55 V). The values for forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and DLco were measured according to the American Thoracic Society/European Respiratory Society recommendation [22]. The 6MWT was performed according to the ATS/ERS criteria [23]. The duration from initial evaluation to the last attendance or death was recorded. We analyzed censored cases by calling them to confirm their life-or-death status.
Statistical analysis
We performed all analyses by using SPSS (version 22; Chicago, IL, USA). Clinical variables were used as continuous variables, except that the categorical variables of gender, smoking status, and a history of surgical lung biopsy were coded as one or zero for the analyses. Continuous variables were presented as mean ± standard deviation unless otherwise stated. Categorical variables were reported as counts and percentages. The survival time was calculated with the life table method. We performed univariate and multivariate Cox proportional hazards analyses to investigate the relationships between clinical variables and mortality rate with adjustment for age and gender. Results of Cox proportional hazards analyses were presented in terms of estimated hazard ratios (HRs) with corresponding 95% confidence intervals (CI); p values of less than 0.05 were considered to be statistically significant. In order to select final prognostic predictors in multivariate analysis, all candidate predictors for which the p-value was < 0.1 on univariate analysis were included in a forward selection method, with a p-value of 0.05 used for final entry or removal. To avoid multicollinearity, some of the highly correlated variables were excluded on multivariate analysis if they had Pearson’s correlation coefficients higher than 0.7. We performed a receiver operating characteristic (ROC) curve analysis to find an optimized cutoff value for 3-year survival prediction. Survival curves were estimated using the Kaplan–Meier method, and compared using the log-rank test across the higher and lower groups of the SGRQ total score.
Results
Patient characteristics
The characteristics of the study population are shown in Table 1. Average age was 65.6 years old, and 85.2% of the patients were male. Surgical lung biopsy was performed to diagnose IPF in 97 patients (53.3%). Median follow-up time was 36.1 months (interquartile range, 19.3 to 48.6 months), 12 cases were lost to follow-up, and 94 patients (51.6%) died within the follow-up times. MST was 48.3 months (95% CI, 43.5 to 53.1 months).
Table 1.
Baseline characteristics of study populationa (N = 182)
| Characteristic | |
|---|---|
| Age, y | 65.6 ± 8.0 |
| Male gender, N (%) | 155 (85.2) |
| BMI, kg/m2 | 24.0 ± 3.4 |
| Ever smoking, N (%) | 147 (81.9) |
| Surgical Lung Biopsy, N (%) | 97 (53.3) |
| Arterial blood gas analysis | |
| PaO2, mmHg | 82.0 ± 11.6 |
| Pulmonary function | |
| FVC, % predicted | 79.7 ± 19.1 |
| FEV1 / FVC | 85.2 ± 7.5 |
| DLco, % predicted (N = 179) | 58.2 ± 20.1 |
| Dyspnoea index | |
| MMRC (0/1/2/3/4) | 51 / 74 / 41 / 15 / 1 |
| BDI (N = 180) | 8.9 ± 2.4 |
| 6MWT (N = 181) | |
| 6MWD, m | 580 ± 136 |
| SpO2 nadir, % | 82.8 ± 9.1 |
| SGRQ score | |
| Symptom | 44.2 ± 22.6 |
| Activity | 40.0 ± 26.1 |
| Impact | 27.7 ± 19.8 |
| Total | 34.5 ± 20.2 |
BMI body mass index, FVC % predicted percent predicted forced vital capacity; FEV 1 forced expiratory volume in the first second, DL CO % predicted percent predicted diffusion capacity for carbon monoxide, PaO 2 partial pressure for oxygen, 6MWD 6-min walk distance, SpO 2 oxygen saturation by pulse oximetry
aPlus–minus values are means ± SD
Baseline levels of clinical indices
Table 1 shows all variables we collected in the present study: mean levels of PaO2, the pulmonary function test, exercise capacity, dyspnoea scale and HRQL score. Mean percent predicted FVC was 79.7%, mean percent predicted DLco was 58.2%. Mean score on the SGRQ total domain was 34.5 points and its distribution is shown in Fig. 1. The relationship between SGRQ and baseline physiological measures is shown in Additional file 1: Table S1. Comorbidities, especially diabetes and orthopedic disease, were related to SGRQ total score. However, they did not have predictive value for mortality with adjustment for age and gender (HR, 1.449; 95% CI 0.901–2.332, P = 0.13, HR, 0.748; 95% CI 0.325–1.720, P = 0.49, respectively) (Additional file 1: Table S2).
Fig. 1.
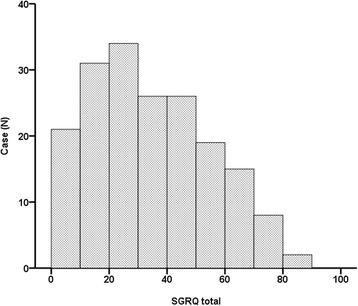
The distribution histogram for SGRQ
Correlation between baseline levels of clinical indices and mortality
On univariate analysis, all domain scores of the SGRQ showed significant predictive value for mortality (Table 2). Moreover, symptom, impact, and total domain showed significant predictive value for mortality with adjustment for age, gender, and %FVC model (Additional file 1: Table S3). Because the SGRQ total score included all domain scores of the SGRQ and there were high correlations between the total score and each domain score, we only used the SGRQ total score in multivariate analysis. Moreover, BDI was excluded from multivariate analysis because of its high correlation with MMRC. In multivariate analysis using a forward selection method, the SGRQ total score was an independent predictor for mortality (HR, 1.012; 95% CI, 1.001–1.023; P = .029), along with percent predicted FVC (HR, 0.957; 95% CI, 0.944–0.971; P <.001) (Table 3).
Table 2.
Univariate Cox proportional-hazard analysis
| Variables | Adjusted HRs (95% CI)a | p value |
|---|---|---|
| Age, y | 1.005 (0.979–1.031) | 0.72 |
| Male gender | 0.725 (0.394–1.334) | 0.30 |
| BMI, kg/m2 | 0.882 (0.826–0.942) | <0.001 |
| PaO2, mmHg | 0.978 (0.961–0.996) | 0.014 |
| FVC, % predicted | 0.954 (0.941–0.967) | <0.001 |
| DLco, % predicted | 0.976 (0.964–0.989) | <0.001 |
| MMRC | 1.413 (1.14–1.753) | 0.002 |
| BDI | 0.830 (0.764–0.903) | <0.001 |
| 6MWD, m | 0.996 (0.994–0.998) | <0.001 |
| SpO2 nadir, % | 0.962 (0.944–0.98) | <0.001 |
| SGRQ | ||
| Symptom | 1.019 (1.01–1.029) | <0.001 |
| Activity | 1.014 (1.006–1.022) | 0.001 |
| Impact | 1.019 (1.009–1.029) | <0.001 |
| Total | 1.021 (1.011–1.032) | <0.001 |
a; age, gender adjusted
Table 3.
Multivariate Cox proportional-hazard analysis
| Variables | Adjusted HRs (95% CI)a | p value |
|---|---|---|
| FVC, % predicted | 0.957 (0.944–0.971) | <0.001 |
| SGRQ total | 1.012 (1.001–1.023) | 0.029 |
a; age, gender adjusted
The ROC curve analysis for the 3-year mortality rate demonstrated that the most accurate and optimal cutoff value for the SGRQ total score was 30 points (area under the curve, 71.1%; 95% CI 62.8–79.4%; P < .001) (Fig. 2). MST was significantly shorter in patients with SGRQ total scores of over 30 points than in patients with scores under 30 points (MST, 37.7 vs 54.7 months. HR, 2.047; 95% CI, 1.329–3.153; P = .001) (Fig. 3).
Fig. 2.
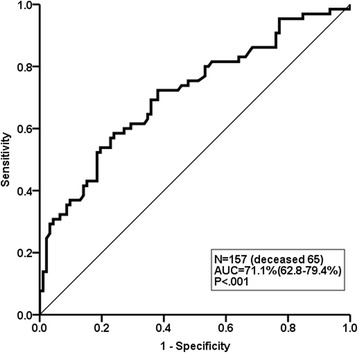
The ROC curve for SGRQ models in predicting 3-year mortality
Fig. 3.
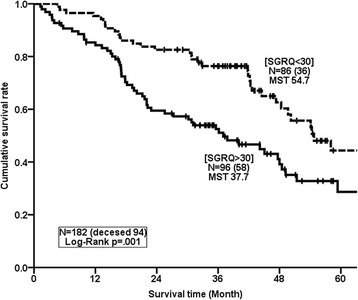
The Kaplan-Meier Curve for SGRQ models
Discussion
This is the first report to show that health status assessed using the SGRQ total score is an independent predictor of mortality in patients with IPF. Moreover, IPF patients with a SGRQ total score higher than 30 points had a higher mortality rate.
The SGRQ is widely used as an assessment tool for HRQL and is applied as one of the key endpoints in clinical trials in patients with IPF [24–29] and COPD [30–32]. However, the impact of HRQL (assessed using the SGRQ) on survival rate has not been fully studied in patients with IPF.
In the univariate analysis in this study, the SGRQ as well as various dimensional clinical factors previously reported as prognostic factors were significant predictors for mortality rate. However, the multivariate analyses showed that both the SGRQ as a patient-reported outcome and percent predicted FVC as a physiological indicator had superior capabilities as independent predictors of mortality than other widely known predictors. Baseline FVC has been reported to be a robust prognostic factor [12], and was recently included in a prognostic model [12]. The present study also shows that baseline FVC remains an important prognostic factor, and the SGRQ total score is an equally independent prognostic meaningful factor. This may be because the SGRQ is derived from multidimensional viewpoints of disease severity, and so may capture more comprehensive information than individual predictive variables.
However, there has been no study on an appropriate cut off value for the SGRQ total score in predicting mortality in patients with IPF. We showed that patients with SGRQ total scores higher than 30 points had a remarkably higher mortality, with a hazard ratio of 2.047. In contrast to the present results, SGRQ was not a significant predictive value for mortality in a previously reported multivariate analysis [33]. The authors of that study examined a smaller sample size and made diagnoses from 2000 to 2005 based on 2000 guidelines that were different from the 2011 ones with a formal multidisciplinary discussion (MDD) used in the present study.
The mean value of the SGRQ total score was reported by Swigris and colleagues to be around 45 points with 56.9–73.1% in FVC from a literature review [5], versus 34.5 points with 79.7% in FVC in the present study. Interestingly, the latest rigorous clinical trial of INPULSIS showed a SGRQ total score (39.6 points) and FVC (79.6%) closer to our findings. Considering the grave prognosis with a score higher than 30 points, these scores should be explicitly considered in the administration of anti-fibrotic drugs, even though FVC may be preserved.
Recently the importance of comorbidities in IPF was reported, however, the relationship between HRQL and comorbidity in IPF has not been fully examined. The present study showed that comorbidities, especially diabetes and orthopedic disease, were related to total score, however, they didn’t have predictive value in age and gender adjusted models.
The present study had some limitations. First, this is a retrospective, single-centered study, and so there may be selection bias. Further large prospective studies will be needed to assess the relationship between the SGRQ and mortality rate. Next, because we examined mild to moderate cases, results may differ in a different cohort. Lastly, all the patients in the present study were Japanese, and it is unclear whether the findings will apply to people of different ethnicities.
Conclusion
The SGRQ total score was found to be an independent prognostic factor in patients with IPF, along with percent predicted FVC. Total scores higher than 30 points were associated with a higher mortality rate.
Acknowledgements
This study was partially supported by a grant to the Diffuse Lung Disease Research Group from the Ministry of Health, Labor and Welfare, Japan and the NPO Respiratory Disease Conference.
Funding
There is no source of funding for the research.
Authors’ contributions
HT is the guarantor of the paper and takes responsibility for the integrity of the work as a whole. YK, KK, ON, KS, and YH contributed to the study design, the analysis and interpretation of the data, and the writing of the paper. MA contributed to the analysis of the data and the writing of the paper. TJ and JF contributed to the diagnosis of IPF as a radiologist and a pathologist respectively, the analysis and interpretation of the data, and the writing of the paper. All authors gave final approval for publication.
Competing interests
The authors have reported to the following conflicts of interest: Furukawa T, Ando M, Kataoka K, Johkoh T, Fukuoka J, and Sakamoto K have nothing to disclose; Taniguchi H reports personal fees from Shionogi & Co., Ltd., Nippon Boehringer Ingelheim, Asahi Kasei Pharma Corp., Bayer in Japan, Chugai Pharmaceutical Co., Ltd., GlaxoSmithKline plc., Ono Pharmaceutical Co., Ltd., TEIJIN PHARMA LIMITED, AstraZeneca K.K, DAIICHI SANKYO COMPANY, LIMITED, Eli Lilly Japan K.K., Novartis Pharma K.K., Fukuda Denshi Co., Ltd., TERUMO CORPORATION, TAIHO Phamaceutical Co., Ltd., KYORIN Pharmaceutical Co., Ltd., Meiji Seika Pharma Co., Ltd., Philips Respironics GK, Pfizer Japan Inc., ABBOTT JAPAN CO., LTD, NIPPON SHINYAKU CO.,LTD, Eisai Co., Ltd., MSD K.K., outside the submitted work.; Kondoh Y reports personal fees from Shionogi & Co., Ltd., KYORIN Pharmaceutical Co., Ltd., Takeda Phamaceutical Co., Ltd., Nippon Boehringer Ingelheim, TEIJIN PHARMA LIMITED, Novartis Pharma K.K., Eisai Co., Ltd., outside the submitted work.; Nishiyama O reports personal fees from Boehringer Ingelheim, Shionogi &Co., LTD., outside the submitted work.; Hasegawa Y reports grants and personal fees from Shionogi & Co., Ltd., Boehringer Ingelheim Japan, and Astellas Pharma Inc, outside the submitted work. These sponsors had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The present study was approved by a local institutional review board of Tosei General Hospital without the consent because of retrospective study (IRB No. 509).
Abbreviations
- 6MWD
6-min walk distance
- 6MWT
6-minute-walk test
- BDI
Baseline Dyspnoea Index
- CI
Confidence interval
- DLco
Diffusion capacity for carbon monoxide
- FEV1
Forced expiratory volume in 1 second
- FVC
Forced vital capacity
- HR
Hazard ratio
- HRQL
Health-related quality of life
- IPF
Idiopathic pulmonary fibrosis
- MMRC
Modified Medical Research Council
- MST
Median survival time
- ROC
Receiver operating characteristic
- SGRQ
St. George’s Respiratory Questionnaire
Additional file
Spearman’s correlation coefficients between SGRQ and baseline physiological measures. Table S2. The relationship between SGRQ and comorbidities. Table S3. SGRQ domain as predictors for mortality. (DOCX 29 kb)
Contributor Information
Taiki Furukawa, Email: yxjry228@ybb.ne.jp.
Hiroyuki Taniguchi, Email: taniguchi@tosei.or.jp.
Masahiko Ando, Email: mando.tsuru@gmail.com.
Yasuhiro Kondoh, Email: konyasu2003@yahoo.co.jp.
Kensuke Kataoka, Email: kataoka@tosei.or.jp.
Osamu Nishiyama, Email: nishiyama_o@yahoo.co.jp.
Takeshi Johkoh, Email: johkoht@kich.itami.hyogo.jp.
Junya Fukuoka, Email: junfkoka@gmail.com.
Koji Sakamoto, Email: sakakoji@med.nagoya-u.ac.jp.
Yoshinori Hasegawa, Email: yhasega@med.nagoya-u.ac.jp.
References
- 1.Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier JF, Flaherty KR, Lasky JA, Lynch DA, Ryu JH, Swigris JJ, Wells AU, Ancochea J, Bouros D, Carvalho C, Costabel U, Ebina M, Hansell DM, Johkoh T, Kim DS, King TE, Jr, Kondoh Y, Myers J, Müller NL, Nicholson AG, Richeldi L, Selman M, Dudden RF, Griss BS, Protzko SL, Schünemann HJ, ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183(6):788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Swigris JJ, Brown KK, Behr J, du Bois RM, King TE, Raghu G, Wamboldt FS. The SF-36 and SGRQ: validity and first look at minimum important differences in IPF. Respir Med. 2010;104(2):296–304. doi: 10.1016/j.rmed.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cella DF. Measuring quality of life in palliative care. Semin Oncol. 1995;22:73–81. [PubMed] [Google Scholar]
- 4.Nishiyama O, Kondoh Y, Kimura T, Kato K, Kataoka K, Ogawa T, Watanabe F, Arizono S, Nishimura K, Taniguchi H. Effects of pulmonary rehabilitation in patients with idiopathic pulmonary fibrosis. Respirology. 2008;13(3):394–399. doi: 10.1111/j.1440-1843.2007.01205.x. [DOI] [PubMed] [Google Scholar]
- 5.Swigris JJ, Esser D, Conoscenti CS, Brown KK. The psychometric properties of the St George’s Respiratory Questionnaire (SGRQ) in patients with idiopathic pulmonary fibrosis: a literature review. Health Qual Life Outcomes. 2014;12:124. doi: 10.1186/s12955-014-0124-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. Am Rev Respir Dis. 1992;145(6):1321–1327. doi: 10.1164/ajrccm/145.6.1321. [DOI] [PubMed] [Google Scholar]
- 7.Domingo-Salvany A, Lamarca R, Ferrer M, Garcia-Aymerich J, Alonso J, Félez M, Khalaf A, Marrades RM, Monsó E, Serra-Batlles J, Antó JM. Health-related quality of life and mortality in male patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166(5):680–685. doi: 10.1164/rccm.2112043. [DOI] [PubMed] [Google Scholar]
- 8.Oga T, Nishimura K, Tsukino M, Sato S, Hajiro T. Analysis of the factors related to mortality in chronic obstructive pulmonary disease: role of exercise capacity and health status. Am J Respir Crit Care Med. 2003;167(4):544–549. doi: 10.1164/rccm.200206-583OC. [DOI] [PubMed] [Google Scholar]
- 9.Nishiyama O, Taniguchi H, Kondoh Y, Kimura T, Kato K, Kataoka K, Ogawa T, Watanabe F, Arizono S. A simple assessment of dyspnoea as a prognostic indicator in idiopathic pulmonary fibrosis. Eur Respir J. 2010;36(5):1067–1072. doi: 10.1183/09031936.00152609. [DOI] [PubMed] [Google Scholar]
- 10.King TE, Jr, Tooze JA, Schwarz MI, Brown KR, Cherniack RM. Predicting survival in idiopathic pulmonary fibrosis: scoring system and survival model. Am J Respir Crit Care Med. 2001;164(7):1171–1181. doi: 10.1164/ajrccm.164.7.2003140. [DOI] [PubMed] [Google Scholar]
- 11.du Bois RM, Weycker D, Albera C, Bradford WZ, Costabel U, Kartashov A, Lancaster L, Noble PW, Raghu G, Sahn SA, Szwarcberg J, Thomeer M, Valeyre D, King TE., Jr Ascertainment of individual risk of mortality for patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011;184(4):459–466. doi: 10.1164/rccm.201011-1790OC. [DOI] [PubMed] [Google Scholar]
- 12.Ley B, Ryerson CJ, Vittinghoff E, Ryu JH, Tomassetti S, Lee JS, Poletti V, Buccioli M, Elicker BM, Jones KD, King TE, Jr, Collard HR. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Intern Med. 2012;156(10):684–691. doi: 10.7326/0003-4819-156-10-201205150-00004. [DOI] [PubMed] [Google Scholar]
- 13.Lederer DJ, Arcasoy SM, Wilt JS, D’Ovidio F, Sonett JR, Kawut SM. Six-minute-walk distance predicts waiting list survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2006;174(6):659–664. doi: 10.1164/rccm.200604-520OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Collard HR, King TE, Jr, Bartelson BB, Vourlekis JS, Schwarz MI, Brown KK. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2003;168(5):538–42. doi: 10.1164/rccm.200211-1311OC. [DOI] [PubMed] [Google Scholar]
- 15.Best AC, Meng J, Lynch AM, Bozic CM, Miller D, Grunwald GK, Lynch DA. Idiopathic pulmonary fibrosis: physiologic tests, quantitative CT indexes, and CT visual scores as predictors of mortality. Radiology. 2008;246(3):935–940. doi: 10.1148/radiol.2463062200. [DOI] [PubMed] [Google Scholar]
- 16.du Bois RM, Albera C, Bradford WZ, Costabel U, Leff JA, Noble PW, Sahn SA, Valeyre D, Weycker D, King TE., Jr 6-Minute walk distance is an independent predictor of mortality in patients with idiopathic pulmonary fibrosis. Eur Respir J. 2014;43(5):1421–1429. doi: 10.1183/09031936.00131813. [DOI] [PubMed] [Google Scholar]
- 17.Caminati A, Bianchi A, Cassandro R, Mirenda MR, Harari S. Walking distance on 6-MWT is a prognostic factor in idiopathic pulmonary fibrosis. Respir Med. 2009;103(1):117–123. doi: 10.1016/j.rmed.2008.07.022. [DOI] [PubMed] [Google Scholar]
- 18.Lama VN, Flaherty KR, Toews GB, Colby TV, Travis WD, Long Q, Murray S, Kazerooni EA, Gross BH, Lynch JP, 3rd, Martinez FJ. Prognostic value of desaturation during a 6-minute walk test in idiopathic interstitial pneumonia. Am J Respir Crit Care Med. 2003;168(9):1084–1090. doi: 10.1164/rccm.200302-219OC. [DOI] [PubMed] [Google Scholar]
- 19.Alakhras M, Decker PA, Nadrous HF, Collazo-Clavell M, Ryu JH. Body mass index and mortality in patients with idiopathic pulmonary fibrosis. Chest. 2007;131(5):1448–1453. doi: 10.1378/chest.06-2784. [DOI] [PubMed] [Google Scholar]
- 20.Hajiro T, Nishimura K, Tsukino M, Ikeda A, Koyama H, Izumi T. Comparison of discriminative properties among disease-specific questionnaires for measuring health-related quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157:785–790. doi: 10.1164/ajrccm.157.3.9703055. [DOI] [PubMed] [Google Scholar]
- 21.Laszlo G. Standardisation of lung function testing: helpful guidance from the ATS/ERS Task Force. Thorax. 2006;61(9):744–746. doi: 10.1136/thx.2006.061648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Macintyre N, Crapo RO, Viegi G, Johnson DC, van der Grinten CP, Brusasco V, Burgos F, Casaburi R, Coates A, Enright P, Gustafsson P, Hankinson J, Jensen R, McKay R, Miller MR, Navajas D, Pedersen OF, Pellegrino R, Wanger J. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 2005;26:720–35. doi: 10.1183/09031936.05.00034905. [DOI] [PubMed] [Google Scholar]
- 23.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 24.Richeldi L, Costabel U, Selman M, Kim DS, Hansell DM, Nicholson AG, Brown KK, Flaherty KR, Noble PW, Raghu G, Brun M, Gupta A, Juhel N, Klüglich M, du Bois RM. Efficacy of a tyrosine kinase inhibitor in idiopathic pulmonary fibrosis. N Engl J Med. 2011;365(12):1079–1087. doi: 10.1056/NEJMoa1103690. [DOI] [PubMed] [Google Scholar]
- 25.Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, Cottin V, Flaherty KR, Hansell DM, Inoue Y, Kim DS, Kolb M, Nicholson AG, Noble PW, Selman M, Taniguchi H, Brun M, Le Maulf F, Girard M, Stowasser S, Schlenker-Herceg R, Disse B, Collard HR, INPULSIS Trial Investigators Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2071–2082. doi: 10.1056/NEJMoa1402584. [DOI] [PubMed] [Google Scholar]
- 26.Raghu G, King TE, Jr, Behr J, Brown KK, du Bois RM, Leconte I, Roux S, Swigris J. Quality of life and dyspnoea in patients treated with bosentan for idiopathic pulmonary fibrosis (BUILD-1) Eur Respir J. 2010;35(1):118–123. doi: 10.1183/09031936.00188108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raghu G, Brown KK, Bradford WZ, Starko K, Noble PW, Schwartz DA, King TE., Jr A placebo-controlled trial of interferon gamma-1b in patients with idiopathic pulmonary fibrosis. Idiopathic Pulmonary Fibrosis Study Group. N Engl J Med. 2004;350(2):125–133. doi: 10.1056/NEJMoa030511. [DOI] [PubMed] [Google Scholar]
- 28.Han MK, Bach DS, Hagan PG, Yow E, Flaherty KR, Toews GB, Anstrom KJ, Martinez FJ, IPFnet Investigators Sildenafil preserves exercise capacity in patients with idiopathic pulmonary fibrosis and right-sided ventricular dysfunction. Chest. 2013;143(6):1699–1708. doi: 10.1378/chest.12-1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Horton MR, Santopietro V, Mathew L, Horton KM, Polito AJ, Liu MC, Danoff SK, Lechtzin N. Thalidomide for the treatment of cough in idiopathic pulmonary fibrosis: a randomized trial. Ann Intern Med. 2012;157(6):398–406. doi: 10.7326/0003-4819-157-6-201209180-00003. [DOI] [PubMed] [Google Scholar]
- 30.Chapman KR, Rennard SI, Dogra A, Owen R, Lassen C, Kramer B, INDORSE Study Investigators Long-term safety and efficacy of indacaterol, a long-acting β2-agonist, in subjects with COPD: a randomized, placebo-controlled study. Chest. 2011;140(1):68–75. doi: 10.1378/chest.10-1830. [DOI] [PubMed] [Google Scholar]
- 31.Tashkin DP, Celli B, Senn S, Burkhart D, Kesten S, Menjoge S, Decramer M, UPLIFT Study Investigators A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359(15):1543–1554. doi: 10.1056/NEJMoa0805800. [DOI] [PubMed] [Google Scholar]
- 32.Wedzicha JA, Calverley PM, Seemungal TA, Hagan G, Ansari Z, Stockley RA, INSPIRE Investigators The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med. 2008;177(1):19–26. doi: 10.1164/rccm.200707-973OC. [DOI] [PubMed] [Google Scholar]
- 33.Nishiyama O, Taniguchi H, Kondoh Y, Kimura T, Kataoka K, Nishimura K, Ogawa T, Watanabe F, Arizono S, Tohda Y. Health-related quality of life does not predict mortality in idiopathic pulmonary fibrosis. Sarcoidosis Vasc Diffuse Lung Dis. 2012;29(2):113–118. [PubMed] [Google Scholar]


