Abstract
Traditionally tumors were classified based on anatomic location but now specific genetic mutations in cancers are leading to treatment of tumors with molecular targeted therapies. This has led to a paradigm shift in the classification and treatment of cancer. Tumors treated with molecular targeted therapies often show morphological changes rather than change in size and are associated with class specific and drug specific toxicities, different from those encountered with conventional chemotherapeutic agents. It is important for the radiologists to be familiar with the new cancer classification and the various treatment strategies employed, in order to effectively communicate and participate in the multi-disciplinary care. In this paper we will focus on lung cancer as a prototype of the new molecular classification.
Keywords: Lung cancer, NSCLC, Adenocarcinoma, EGFR mutation, ALK rearrangement
INTRODUCTION
Classification in medicine is central to establishing diagnosis, prognostication as well for selection of treatment strategies. Traditionally, tumors were classified based on anatomical location, for example lung cancer originating in the lung, and within each organ specific group, subgroups were based on the cell type and histopathological features. For example, the 2004 World Health Organization (WHO) classification divided lung cancer into two main subtypes; small cell lung cancer (SCLC) and non-SCLC (NSCLC), and further sub-classified NSCLC into adenocarcinoma and Squamous cell carcinoma (SCC) (1). This classification was sufficient as SCLC was treated with chemotherapy and/or radiation, and NSCLC was primarily treated with surgery, with chemotherapy and/or radiation reserved for unresectable or metastatic tumors. In the past, all advanced NSCLC were essentially treated with platinum based chemotherapy. The radiologist approach to staging and response assessment of tumors also mirrored this classification system. In patients undergoing conventional chemotherapy, response was seen primarily as change in size so size based criteria such as the WHO and Response Evaluation Criteria in Solid Tumours (RECIST) were developed to communicate results in universal fashion.
However, in recent years due to advances in molecular biology and gene sequencing, numerous genes have been identified across hematological and solid malignancies, that when mutated, promote tumorigenesis. Specific genetic mutations in cancers have the potential to be treated with molecular targeted therapies (MTT) such as epidermal growth factor receptor (EGFR) inhibitor Erlotinib in lung cancer, tyrosine kinase inhibitor (TKI) Imatinib in gastrointestinal stromal tumors and vascular endothelial growth factor (VEGF) inhibitor Sunitinib in renal cell carcinoma, leading to dramatic responses and significantly improved overall survival. This has led to a paradigm shift in the classification and treatment of cancer. The last decade saw a slew of newer cancer treatments focused on MTT obtain Food and Drug Administration (FDA)-approval, and treatment options have now exploded. Sub-classification of tumors based on their molecular characteristics allows for stratification of patients for optimal targeted therapy, the promise of precision medicine. Cancer genomics and personalized cancer treatment is the “new kid on the block” and is here to stay.
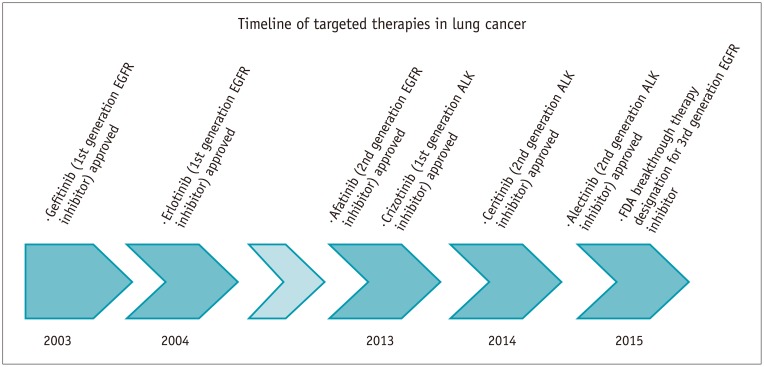
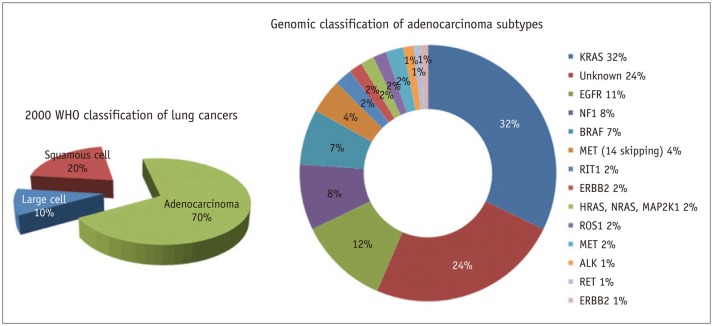
Lung cancer is the leading example of how transformative cancer classification and care has become in this era of precision medicine. Prior to 2004, the discovery of EGFR mutations in NSCLC and subsequent specific treatment with TKIs, gefitinib and erlotinib, paved the way for precision medicine in NSCLC (Fig. 1). This was quickly followed by the discovery of other driver genes such as echinoderm microtubule associated protein like 4-anaplastic lymphoma kinase 1 (EML4-ALK1) in 2007 and the ALK inhibitor crizotinib, which was granted accelerated FDA approval for treatment of ALK rearranged lung cancers (Fig. 1). EGFR mutations and ALK rearrangements currently account for 12% of all adenocarcinomas in the United States and EGFR accounts for up to 60% of lung adenocarcinomas in Korea and 55% of lung adenocarcinomas in Taiwan (2,3,4). The clinical success of targeted agents such as EGFR inhibitors and ALK inhibitors has fueled the research to identify additional genomic abnormalities and targetable agents. Other driver genes in lung cancer include receptor tyrosine kinase (ROS1), fibroblast growth factor receptor 1 and the landscape continues to evolve (Fig. 2). The WHO lung cancer classification was recently updated in 2015 to reflect these advances and testing for EGFR mutations and ALK rearrangements is currently the standard of care for patients with initial diagnosis of lung adenocarcinoma (5). Similar changes have been made to the classification of other cancers for example renal cell carcinoma, breast cancer and gastric cancer, to better reflect the molecular and genomic characteristics. This in turn allows the matching of the right gene with the right cancer agent and eventually improves the efficacy of therapy and patient outcomes.
Fig. 1. Timeline of events in lung cancer molecular targeted therapies.
ALK = anaplastic lymphoma kinase, EGFR = epidermal growth factor receptor, FDA = Food and Drug Administration
Fig. 2. Pie chart demonstrating percentage of driver alterations in lung adenocarcinoma.
Adapted from Sholl et al. J Thorac Oncol 2015;10:768-777 (2). ALK = anaplastic lymphoma kinase, EGFR = epidermal growth factor receptor
Imaging plays a central role in the assessment of response to treatment both in day-to-day practice as well as in the setting of clinical trials. Tumors treated with MTT often show morphological changes rather than change in size. Since conventional size based assessment such as WHO and RECIST may not be accurate in this scenario, alternate tumor response criteria such as Choi criteria, Morphology, Attenuation, Size and Structure (MASS) criteria, and Response Assessment in Neuro-Oncology (RANO) criteria have been developed, to capture these morphological changes. In addition, MTT are associated with class specific and drug specific toxicities, different from those encountered with conventional chemotherapeutic agents. A new class of agents that have emerged are the immune checkpoint inhibitors, which promote the body's intrinsic T-cell immune response to cancer cells, and have shown significant activity across multiple cell lines such as melanoma, lung cancer, renal cell carcinoma, bladder cancer and lymphoma. Tumors treated with immune checkpoint inhibitors respond in a different fashion, often demonstrating early increase in size and new lesions prior to dramatic tumor shrinkage, leading to new immune-related response criteria and are also associated with unique range of immune related adverse events. It is important for the radiologists to be familiar with the new cancer classification based on genomics and the various treatment strategies employed, in order to effectively communicate with the oncologists and participate in the multi-disciplinary care.
A review of the entire gamut of genomic alterations in cancer and the changes in classification of different tumors is beyond the scope of this article. Instead, in this paper, we will focus on lung cancer as a prototype of the new molecular classification system and review in detail the two most common targetable alterations in lung cancer. EGFR mutations and ALK rearrangements, and we will look at EGFR mutations and ALK rearrangements beyond lung cancer in different cell lines comparing the presentation and their targeted therapies.
Overview of Epidermal Growth Factor Receptor Mutations and ALK Rearrangements
Epidermal growth factor receptor is a tyrosine kinase receptor of the ErbB family, which is comprised of four related receptors: ErbB1 (EGFR/HER1), ErbB2 (HER2/neu), ErbB3 (HER3), and ErbB4 (HER4). Each receptor is composed of an extracellular ligand binding domain, a transmembrane domain and an intracellular domain (6). When epidermal growth factor binds to the extracellular ligand, a downstream signaling pathway is triggered that includes the Ras-Raf-MAP-kinase and the PI3K-Akt-mTOR pathway, linked to multiple responses promoting tumorigenesis including cell growth, proliferation, motility and survival (7). EGFR induces cancer by one of three mechanisms: mutational activation, amplification and overexpression of ligands. EGFR is overexpressed in multiple human tumors including lung, breast, colorectal, vulvar and head and neck cancers (8).
Anaplastic lymphoma kinase is a member of the insulin ROS1. Once activated it triggers downstream signaling on multiple pathways including RAS/MAPK, PI3K/AKT, JAK/STAT, and Cdc42/Rac (9).
A small inversion in chromosome 2p causes the formation of a fusion gene of the ALK and echinoderm microtubule-associated protein-like 4 (EML4). EML4-ALK rearrangements act as oncogenes and the EML4-ALK fusion protein has oncogenic potential with transforming activity, which is the most common fusion in NSCLC (10). ALK-rearranged cancers are oncogene-addicted with dependence on the oncogene mutation for sustaining proliferation and growth (10). Aberrant activation of ALK has been found in several cancers including NSCLC, anaplastic large cell lymphoma (ALCL), inflammatory myofibroblastic tumor and neuroblastoma (11).
Comparison of EGFR and ALK in NSCLC
EGFR in NSCLC
In NSCLC, EGFR mutations are more common in never smokers, females and patients of East Asian origin (12,13). A recent study looking at CT findings and EGFR mutation status, reported that EGFR-mutated adenocarcinoma had significantly higher frequencies of multiple bilateral lung tumors, convergence of surrounding structures, surrounding ground glass opacity, and notch sign at HRCT compared with the non-EGFR-mutated type (14,15). Cavitation and pleural effusions less frequent when compared to the non-mutated subtype (14,15).
It is important to understand that not all EGFR mutations are responsive to treatment. The two most common mutations of EGFR in NSCLC are deletions in exon 19 and L8585R point mutation in exon 21 (13). These mutations are associated with response to EGFR-TKI treatment and are considered sensitizing mutations, whereas tumors with other EGFR mutation such as exon 20 insertions are resistant to EGFR-TKI treatment. NSCLCs that contain these sensitizing EGFR mutations have been shown to be ‘addicted' to mutant EGFRs for proliferation and survival (16,17). Therefore drugs that bind to the EGFR tyrosine kinase and inhibit EGFR are highly effective in treating NSCLC with mutations. Erlotinib and gefitinib are first line EGFR TKIs that reversibly inhibit EGFR and afatinib is a second line EGFR TKI that irreversibly binds to EGFR. All three are administered orally and approved by the FDA as first line therapy in patients with EGFR mutation. Response to EGFR-TKI therapy is usually dramatic with response rates as high as 70%, and associated with early and significant tumor shrinkage (18). A third generation EGFR inhibitor (BI 1482694) got FDA breakthrough therapy designation in December 2015 for metastatic EGFR T790M mutation positive NSCLC (Fig. 1).
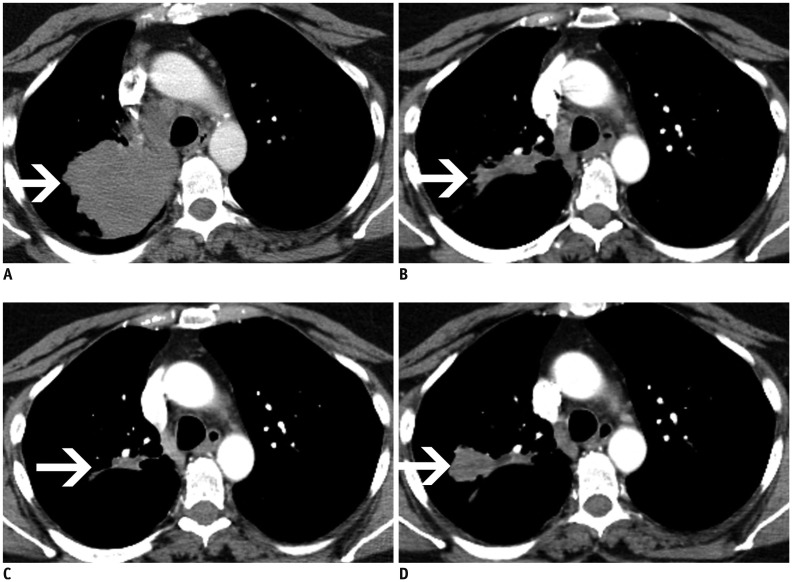
Patients with NSCLC that initially respond to EGFR inhibitors usually have disease progression after a median of 12 months due to the development of resistance (19). In approximately 50% of patients resistance is secondary to a second site mutation T790M at exon 20 (Fig. 3) (20). Afatinib has been shown to be effective against all forms of EGFR including wild type, exon 19, exon 21 L858R and T790M (20), and is currently used as first line treatment in EGFR mutated lung cancer or as second-line agents in patients who develop erlotinib resistance. In 20% of patients EGFR TKI resistance is caused by MET amplification that causing kinase switching triggering the erbB3 pathway instead of the erbB1 pathway (21). MET amplification can coexist with T790M or occur independently, and addition of MET-inhibitors to erlotinib has shown clinical benefit (20).
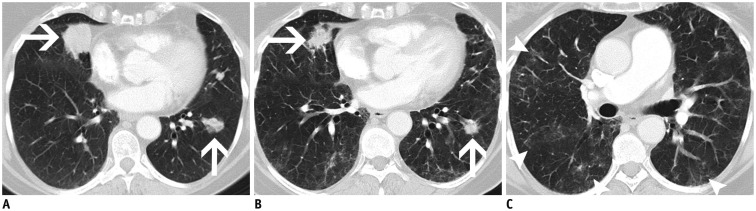
Fig. 3. Axial contrast enhanced CT on soft tissue windows at four different time points in 57-year-old woman with EGFR exon 19 deletion lung adenocarcinoma.
A. Initial image demonstrates large right upper lobe mass (arrow). B. Second image demonstrates response to first generation EGFR TKI (erlotinib) after 3 months with significant decrease in size of mass (arrow). C. Third image was performed 6 months later demonstrates further decrease in size of right upper lobe mass (arrow). D. Final image demonstrates gradual increase in size (arrow). Biopsy demonstrated T790M mutation that has known resistance to EGFR TKI (erlotinib) therapy. EGFR = epidermal growth factor receptor, TKI = tyrosine kinase inhibitor
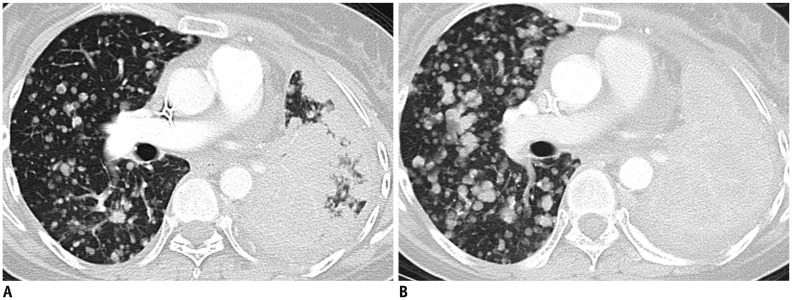
The use of RECIST to determine disease progression in patients on EGFR therapies is under debate. Patients treated with erlotinib may have an initial dramatic response to therapy followed by slow progression over several months suggesting some continued sensitivity to therapy. When erlotinib is discontinued due to disease progression, a flare phenomenon has been observed with dramatic increase in tumor burden, which promptly improves with re-administration of erlotinib (Fig. 4) (22). This ‘flare' phenomenon is not merely an imaging finding but can be associated with symptomatic disease worsening, resulting in hospitalization and in some cases even death (23). The current strategy at many centers is to continue erlotinib beyond RECIST defined progression and add conventional chemotherapy to EGFR inhibitor, or replace erlotinib with second-generation inhibitors such as afatinib.
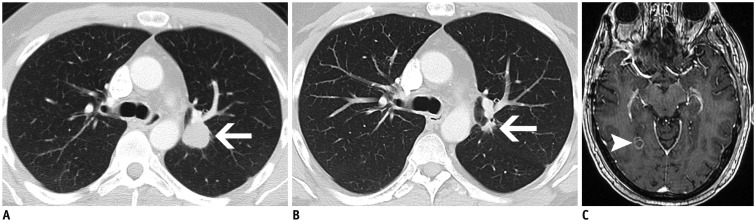
Fig. 4. Axial CECT on lung windows in 53-year-old woman with L8585R point mutation in exon 21 adenocarcinoma.
Patient had been treated with EGFR tyrosine kinase inhibitor (erlotinib) for 11 months but was progressing on serial CT studies. Initial CT (A) demonstrates multiple small right-sided pulmonary metastases and almost confluent opacification in left lung. Patient was taken off therapy and CT performed two weeks later due to patients dyspnea demonstrates now complete opacification in left hemithorax and interval increase in size in right sided pulmonary metastases, several had doubled in size (B). Appearances and clinical presentation were consistent with ‘flare’ phenomenon. CECT = contrast enhanced CT, EGFR = epidermal growth factor receptor
The most common toxicities that are seen with EGFR inhibitors include skin toxicity, colitis, and rare but potentially fatal pneumonitis. CT findings of pneumonitis include multifocal ground-glass opacities (Fig. 5) with or without interlobular septal thickening or diffuse ground glass changes with consolidation and traction bronchiectasis (24,25). Colitis may be manifest on imaging as fluid-filled colon, mural thickening, pericolonic fat stranding, and hyperemic mesenteric vessels. A rare but important toxicity is pneumatosis and pneumoperitoneum, the frequency of which increases with duration of drug treatment (26).
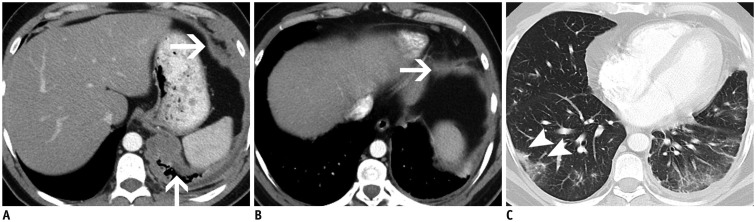
Fig. 5. Axial CECT on lung windows in 68-year-old woman with exon 19 EGFR mutant adenocarcinoma.
A. Patient had dominant masses in right and left lower lobes (arrows) on initial CT. Patient was treated with EGFR tyrosine kinase inhibitor (erlotinib) and follow up CT performed 2 months later (B) demonstrates decrease in size of lower lobe masses (arrows). C. Patient also had developed multifocal faint bilateral subpleural ground glass changes (arrowheads) consistent with pneumonitis. Patient was asymptomatic and remained on treatment with changes on pneumonitis resolving on follow up studies. CECT = contrast enhanced CT, EGFR = epidermal growth factor receptor
ALK Rearrangements in NSCLC
Anaplastic lymphoma kinase rearrangements occur in approximately 2–5% of all NSCLC and are more commonly seen in younger patients (median age early 50s) that are never smokers or former light smokers, adenocarcinoma histology, typically of signet ring cell subtype (27). Metastatic disease at presentation is common, with high propensity for pleuropericardial disease and central nervous system (CNS) metastases (Figs. 6, 7). A multi-institution trial performed for assessing the presence of an ALK molecular phenotype in primary NSCLC on CT found that a central tumor location, absence of a pleural tail and large pleural effusion in patients under 60 years were associated with ALK rearrangements (28). There are multiple ALK rearrangements in NSCLC, of which EML4-ALK is the most predominant (29). Without ALK targeted therapies, these tumors carry a poor prognosis with a median survival of approximately 20 months (30). Crizotinib is a first generation small molecule inhibitor with activity against ALK, MET and ROS1 (31). Crizotinib received accelerated approval from the FDA in 2011 and regular approval in 2013 for ALK rearranged NSCLC.
Fig. 6. Axial contrast enhanced CT of thorax on lung windows (A, B) and axial T1 post gadolinium contrast MRI of brain (C) in 40-year-old man with metastatic lung adenocarcinoma with ALK rearrangement.
On initial CT (A) patient has 2.5 × 2.3 cm mass in left upper lobe (arrow). Patient was treated with first generation ALK tyrosine kinase inhibitor (crizotinib) and had durable response in his lungs with second CT (B) post 5 year of treatment demonstrating small 1.2 × 0.6 cm ill-defined nodule at site of primary dominant mass (arrow). Patient unfortunately developed brain metastases due to poor blood brain barrier penetration with ALK inhibitor (crizotinib) and MRI (C) demonstrates ring enhancing 1.0 cm metastasis in right occipital lobe (arrowhead). ALK = anaplastic lymphoma kinase
Fig. 7. Axial contrast enhanced CT on soft tissue (A, B) and lung windows (C) in 38-year-old man lifelong non smoker with metastatic ALK rearranged lung adenocarcinoma.
A, B. Initial CT demonstrates extensive left pleural nodularity and circumferential thickening with example of pleural thickening in left lower lobe included (arrows). C. Follow up performed 8 weeks after treatment with alectinib (second generation ALK inhibitor) demonstrated decrease in left pleural metastatic disease but interval development of new right lower lobe ground glass changes (arrowheads) consistent with pneumonitis. Patient was not symptomatic and therapy was continued. ALK = anaplastic lymphoma kinase
Tumors treated with crizotinib or other ALK inhibitors often show an initial dramatic tumor shrinkage followed by slow progression on serial studies while the patient remains relatively asymptomatic through progression (32). Acquired resistance to crizotinib occurs secondary to development of mutations in the kinase domain of ALK such as the gatekeeper mutation of L1196M (33). Despite the development of resistance, tumors usually remain ALK-dependent, very similar to EGFR mutant lung cancer on EGFR-TKI therapy, and patients continue to be treated with the crizotinib despite evidence of radiological progression on CT by RECIST.
One of the most common sites of relapse is the CNS, which represents pharmacokinetic failure as crizotinib has poor blood brain barrier penetration (Fig. 6) (34). Surveillance MRI brain is recommended for patients on crizotinib every 6–9 months. Second generation ALK inhibitors developed include ceritinib and alectinib. Ceritinib is an oral small molecule inhibitor of ALK that does not inhibit MET but does inhibit ROS1 and was approved in 2014 by the FDA for patients with metastatic ALK NSCLC that progressed or was intolerant to crizotinib. Alectinib is a highly selective ALK inhibitor that has no activity against MET or ROS1 but does have activity against crizotinib mutations including L1196M and C1156Y and may have a better result in patients with brain metastases (35,36).
Side effects that may be seen with crizotinib include development of simple or complex renal cysts, fluid filled bowel loops, peripheral edema, osteopenia and more rarely pneumonitis (Fig. 8) (37,38). A peculiar finding is the include development of simple or complex renal cysts, not to be mistaken for cystic metastases or cystic renal cell carcinoma (37).
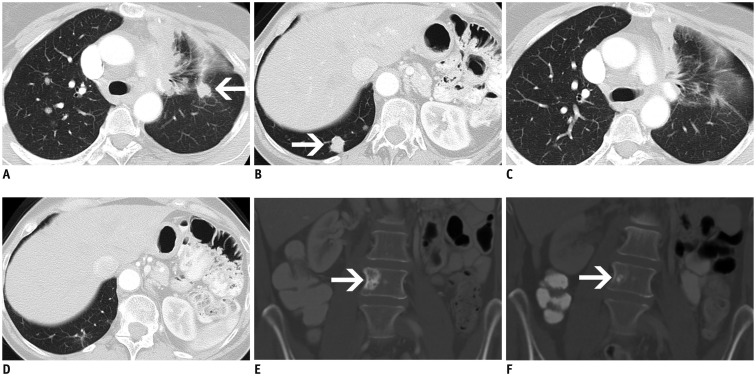
Fig. 8. Axial (A–D) and coronal enhanced (E, F) CT in 58-year-old woman with metastatic lung adenocarcinoma with ALK rearrangement.
A, B. Initial CT demonstrates post obstructive atelectasis in left upper lobe from left hilar lymphadenopathy (not shown) and bilateral lung metastases, largest in left upper lobe measuring 1.3 x 1.3 cm (arrow) and in right lower lobe (arrow) measuring 1.6 × 1.4 cm. Patient was treated with crizotinib and follow up CT performed after 8 weeks of therapy (C, D) demonstrates response with resolution of metastases with only mild ground glass changes at site of dominant masses. E, F. Coronal CT demonstrates complication of crizotinib therapy with development of osteopenia best seen on CT as decreased sclerosis after 2 years of therapy within blastic bone metastasis (arrow). ALK = anaplastic lymphoma kinase
EGFR Mutations in Non-Lung Cancers
EGFR in Breast Cancer
Between 12–30% of breast cancers have over-expression of ErbB2 (HER2/neu), typically affecting younger patients and have a clinically aggressive course (39). Patients with HER2 expression are more likely to have multifocal cancers, lymph nodal and liver metastases (40,41). Tumors that over-express HER2 was previously associated with a poor survival until the development of targeted therapy. Trastuzumab is a humanized monoclonal antibody that works on the extracellular domain of EGFR/HER2, and has shown to significantly improve overall survival in HER2 positive breast cancer (42). Other HER2 targeting agents are pertuzumab, trastuzumab-emtansine (T-DM1) and lapatinib. CNS metastases are more common in patients with HER2 positive breast cancers and subtypes of triple negative patients treated with trastuzumab, likely due to a combination of trastuzumab prolonging survival combined with the inability of trastuzumab to cross the blood brain barrier (42). Trastuzumab may be associated with cardiotoxicity, manifest on imaging as cardiomegaly, pleural effusions and interlobular septal thickening.
EGFR in Head and Neck Cancers
Over-expression of EGFR may be seen in SCCs of the head and neck (SCCHN) (Fig. 9), and correlates with poor prognosis and resistance to radiation therapy (43). Human papilloma virus (HPV) negative SCCHN is associated with EGFR mutations while HPV positive SCCHN is associated with a lack or low expression of EGFR expression (44). Cetuximab is a chimeric human: murine monoclonal antibody that binds to EGFR in the extracellular domain, and thereby prevents the binding and activation of downstream signaling pathways. Cetuximab can also recruit activated immune cells into tumor cells leading to tumor cell death. Cetuximab combined with radiotherapy has been shown to improve median survival in SCCHN (45). One of the common side effects of cetuximab therapy, acneiform skin rash, interestingly correlates with a greater response rate in SCCHN, and may be a surrogate marker of tumor response (45).
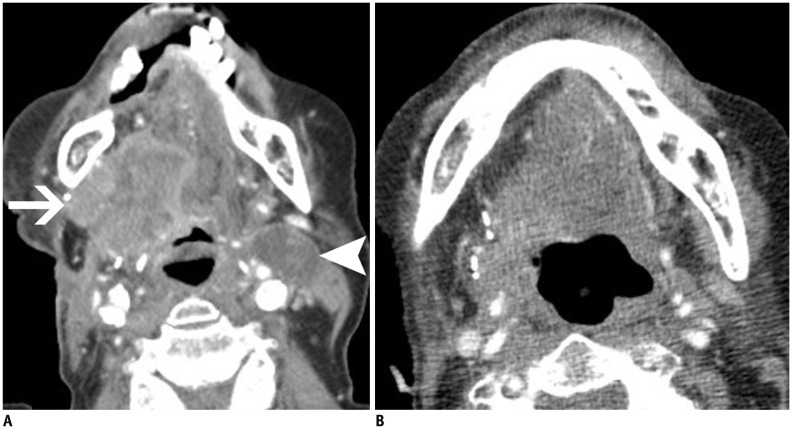
Fig. 9. Axial CECT at floor of mouth in 58-year-old man with EGFR mutant squamous cell carcinoma of tongue.
A. Patient had been treated with right sided hemiglossectomy but developed large enhancing mass in surgical site on right (arrow) and level IIa low density left cervical chain lymph node (arrowhead) on CT. B. Patient was treated with EGFR monoclonal antibody (cetuximab) and follow up CT performed 2 months later demonstrates resolution of mass on right and significant decrease in left cervical lymph node. CECT = contrast enhanced CT, EGFR = epidermal growth factor receptor
EGFR in Colon Cancer
The abnormal expression in EGFR has also been found in metastatic colorectal cancer. There are two anti-EGFR antibodies used in the treatment of colorectal cancer and head and neck squamous cell cancers: cetuximab and panitumab. Cetuximab was discussed previously. Panitumab is a fully human monoclonal antibody (IgG2) also given intravenously. As it does not contain any murine portion of IgG there is less hypersensitivity reactions and it has a longer half-life than cetuximab. Toxicities seen with the anti-EGFR monoclonal antibodies are skin rash, electrolyte abnormalities (hypokalemia, hypomagnesaemia) and an infusion reaction (46). The acneiform skin rash seen with cetuximab as with SCCHN also in colon cancer correlates with a greater response rate in treatment (47). Imaging findings in panitumab toxicities include colitis which may appear as fluid filled colon, mural thickening, pericolonic fat stranding and hyperemia of mesenteric vessels and deranged liver function tests may be associated with periportal edema, gallbladder wall thickening and ascites (25).
EGFR in Vulvar Cancers
Squamous cell carcinoma of the vulva, similar to head and neck cancers can be HPV associated or HPV-independent but the pathogenesis and classification is currently controversial. HPV-associated neoplasms present in younger women with vulvar intraepithelial neoplasm and expression of p16, a cell cycle protein, compared to HPV-independent vulvar SCC occurring in older women with TP53 mutations (48,49,50). A number of mutations have been identified in HPV-independent vulvar SCC including activation of EGFR (51). A study found EGFR amplification in 12% of invasive vulvar SCC and another study found a negative correlation with p16 expression and positive association with p53 raising the possibility of synergism between TP53 and EGFR in the tumorigenesis of HPV-independent vulvar SCC (48,51). Studies have also shown EGFR expression in vulvar SCC with advanced stage and lymph node metastases and an association with decrease in survival (51,52). While HPV-associated neoplasm in head and neck cancers have shown a better prognosis and therapeutic response, the results are conflicting in vulvar SCC but the presence of EGFR amplification does represent a possible target for therapy with EGFR inhibitors (53).
ALK Rearrangements in Non-Lung Cancer
ALK Rearrangements in Anaplastic Large Cell Lymphoma
Anaplastic large cell lymphoma accounts for 10–15% of pediatric non-Hodgkins lymphoma (NHL) and 1–2% of adult NHL. ALCL more recently has been subdivided into ALK positive and ALK negative subclasses with approximately 90% of pediatric tumors and 40–50% of adult tumors being ALK positive (54,55). Most patients present at a late stage with B symptoms with intra-abdominal or mediastinal lymph node involvement and extranodal spread to lung, liver, soft tissue, bone and skin (55). ALK positive ALCL is extremely chemosensitive in front line and relapse with high response rates to traditional NHL chemotherapy regimes (Fig. 10). ALK inhibitors have shown promise in treating relapsed ALK positive ALCL in small phase one trials (56).
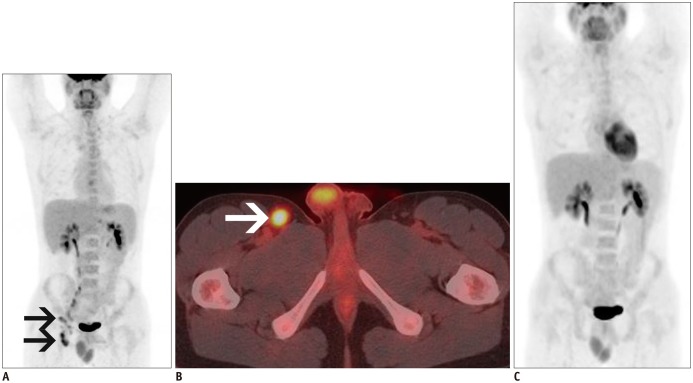
Fig. 10. MIP (A, C) and axial non contrast fused 18F-FDG PET/CT (B) in 20-year-old man with ALK positive anaplastic large cell lymphoma.
A. Patient had been diagnosed one year earlier and treated with brentuximab but had relapsed 6 months after completing treatment. New baseline PET/CT demonstrated residual lymphadenopathy in right external iliac and inguinal lymph nodes (arrows). B. Axial fused PET/CT demonstrates FDG avid right inguinal lymph node (arrow) with SUVmax 5.5. C. Patient was treated with salvage chemotherapy (gemcitabine, vinorelbine and doxil) with response to treatment and resolution of right pelvic lymphadenopathy on PET/CT performed 8 weeks later. ALK = anaplastic lymphoma kinase, MIP = maximum intensity projection, PET = positron emission tomography
ALK Rearrangements in Inflammatory Myofibroblastic Tumors
Inflammatory myofibroblastic tumors (IMT) are mesenchymal neoplasms that occur most commonly in the lung, abdomen and bladder in children and young adults (57). IMT has a wide spectrum ranging from a clinically benign inflammatory pseudotumor to an aggressive sarcomatous neoplasm and surgical resection is the principal treatment. Most cases have a benign clinical course but IMT can recur locally and rarely metastasize (58). Approximately 50% of IMT have ALK rearrangements involving multiple fusion partners (59). ALK expression and rearrangement has been described as a good prognostic marker in IMT with positive cases showing a better outcome compared to a more aggressive course in ALK-negative IMT (58,60).
ALK Rearrangements in Neuroblastoma
Neuroblastoma is the most common extracranial tumor in children and is responsible for approximately 12% of pediatric cancer deaths (61). ALK mutations are found in the majority of familial neuroblastoma cases and up to 10% cases of sporadic neuroblastoma (61,62). Somatic mutations in ALK have been associated with decrease in overall survival and can occur simultaneously with another genetic aberration that is associated with a poor prognosis (amplification of MYCN) (63).
CONCLUSION
The utility of classification systems ultimately rests on the ability to provide prognostic data and if possible offer specific therapies. In the past, histological classification had little impact on treatment protocol as seen with lung cancer, where almost all patients with advanced NSCLC received platinum-based chemotherapy. In the current era of precision medicine, tumor specimens are tested for targetable mutations and tumors are classified accordingly, in order to match the right patient with the right treatment. As cancer genomics and genomically driven therapies evolve, pure histological classification may become irrelevant in the coming years. As pathologists and oncologists are moving away from the traditional classification systems, as part of multidisciplinary patient management team it is important for radiologist to “adapt” to the evolving changes and “adopt” the new wave of genomic medicine and personalized cancer treatment.
Acknowledgments
The authors wish to thank Erin Foley, Cancer Imaging Program Coordinator/Administrative Assistant for her help in creating Figures 1 and 2 in this paper.
References
- 1.Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC. Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC; 2004. [Google Scholar]
- 2.Sholl LM, Aisner DL, Varella-Garcia M, Berry LD, Dias-Santagata D, Wistuba II, et al. Multi-institutional oncogenic driver mutation analysis in lung adenocarcinoma: the lung cancer mutation consortium experience. J Thorac Oncol. 2015;10:768–777. doi: 10.1097/JTO.0000000000000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ha SY, Choi SJ, Cho JH, Choi HJ, Lee J, Jung K, et al. Lung cancer in never-smoker asian females is driven by oncogenic mutations, most often involving EGFR. Oncotarget. 2015;6:5465–5474. doi: 10.18632/oncotarget.2925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hsu KH, Ho CC, Hsia TC, Tseng JS, Su KY, Wu MF, et al. Identification of five driver gene mutations in patients with treatment-naïve lung adenocarcinoma in Taiwan. PLoS One. 2015;10:e0120852. doi: 10.1371/journal.pone.0120852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JH, Beasley MB, et al. The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015;10:1243–1260. doi: 10.1097/JTO.0000000000000630. [DOI] [PubMed] [Google Scholar]
- 6.Schlessinger J. Ligand-induced, receptor-mediated dimerization and activation of EGF receptor. Cell. 2002;110:669–672. doi: 10.1016/s0092-8674(02)00966-2. [DOI] [PubMed] [Google Scholar]
- 7.Vivanco I, Sawyers CL. The phosphatidylinositol 3-Kinase AKT pathway in human cancer. Nat Rev Cancer. 2002;2:489–501. doi: 10.1038/nrc839. [DOI] [PubMed] [Google Scholar]
- 8.Salomon DS, Brandt R, Ciardiello F, Normanno N. Epidermal growth factor-related peptides and their receptors in human malignancies. Crit Rev Oncol Hematol. 1995;19:183–232. doi: 10.1016/1040-8428(94)00144-i. [DOI] [PubMed] [Google Scholar]
- 9.Mologni L. Inhibitors of the anaplastic lymphoma kinase. Expert Opin Investig Drugs. 2012;21:985–994. doi: 10.1517/13543784.2012.690031. [DOI] [PubMed] [Google Scholar]
- 10.Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y, Ishikawa S, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007;448:561–566. doi: 10.1038/nature05945. [DOI] [PubMed] [Google Scholar]
- 11.Mologni L. Current and future treatment of anaplastic lymphoma kinase-rearranged cancer. World J Clin Oncol. 2015;6:104–108. doi: 10.5306/wjco.v6.i5.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pao W, Miller V, Zakowski M, Doherty J, Politi K, Sarkaria I, et al. EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci U S A. 2004;101:13306–13311. doi: 10.1073/pnas.0405220101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shigematsu H, Lin L, Takahashi T, Nomura M, Suzuki M, Wistuba II, et al. Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst. 2005;97:339–346. doi: 10.1093/jnci/dji055. [DOI] [PubMed] [Google Scholar]
- 14.Hasegawa M, Sakai F, Ishikawa R, Kimura F, Ishida H, Kobayashi K. CT Features of epidermal growth factor receptor-mutated adenocarcinoma of the lung: comparison with nonmutated adenocarcinoma. J Thorac Oncol. 2016;11:819–826. doi: 10.1016/j.jtho.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 15.Liu Y, Kim J, Qu F, Liu S, Wang H, Balagurunathan Y, et al. CT features associated with epidermal growth factor receptor mutation status in patients with lung adenocarcinoma. Radiology. 2016;280:271–280. doi: 10.1148/radiol.2016151455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sordella R, Bell DW, Haber DA, Settleman J. Gefitinib-sensitizing EGFR mutations in lung cancer activate anti-apoptotic pathways. Science. 2004;305:1163–1167. doi: 10.1126/science.1101637. [DOI] [PubMed] [Google Scholar]
- 17.Tracy S, Mukohara T, Hansen M, Meyerson M, Johnson BE, Jänne PA. Gefitinib induces apoptosis in the EGFRL858R non-small-cell lung cancer cell line H3255. Cancer Res. 2004;64:7241–7244. doi: 10.1158/0008-5472.CAN-04-1905. [DOI] [PubMed] [Google Scholar]
- 18.Sharma SV, Bell DW, Settleman J, Haber DA. Epidermal growth factor receptor mutations in lung cancer. Nat Rev Cancer. 2007;7:169–181. doi: 10.1038/nrc2088. [DOI] [PubMed] [Google Scholar]
- 19.Zhou C, Wu YL, Chen G, Feng J, Liu XQ, Wang C, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12:735–742. doi: 10.1016/S1470-2045(11)70184-X. [DOI] [PubMed] [Google Scholar]
- 20.Yu HA, Arcila ME, Rekhtman N, Sima CS, Zakowski MF, Pao W, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res. 2013;19:2240–2247. doi: 10.1158/1078-0432.CCR-12-2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, Park JO, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316:1039–1043. doi: 10.1126/science.1141478. [DOI] [PubMed] [Google Scholar]
- 22.Riely GJ, Kris MG, Zhao B, Akhurst T, Milton DT, Moore E, et al. Prospective assessment of discontinuation and reinitiation of erlotinib or gefitinib in patients with acquired resistance to erlotinib or gefitinib followed by the addition of everolimus. Clin Cancer Res. 2007;13:5150–5155. doi: 10.1158/1078-0432.CCR-07-0560. [DOI] [PubMed] [Google Scholar]
- 23.Chaft JE, Oxnard GR, Sima CS, Kris MG, Miller VA, Riely GJ. Disease flare after tyrosine kinase inhibitor discontinuation in patients with EGFR-mutant lung cancer and acquired resistance to erlotinib or gefitinib: implications for clinical trial design. Clin Cancer Res. 2011;17:6298–6303. doi: 10.1158/1078-0432.CCR-11-1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hughes B, Mileshkin L, Townley P, Gitlitz B, Eaton K, Mitchell P, et al. Pertuzumab and erlotinib in patients with relapsed non-small cell lung cancer: a phase II study using 18F-fluorodeoxyglucose positron emission tomography/computed tomography imaging. Oncologist. 2014;19:175–176. doi: 10.1634/theoncologist.2013-0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Howard SA, Rosenthal MH, Jagannathan JP, Krajewski KM, Shinagare AB, Ramaiya NH, et al. Beyond the vascular endothelial growth factor axis: update on role of imaging in nonantiangiogenic molecular targeted therapies in oncology. AJR Am J Roentgenol. 2015;204:919–932. doi: 10.2214/AJR.14.12876. [DOI] [PubMed] [Google Scholar]
- 26.Thornton E, Howard SA, Jagannathan J, Krajewski KM, Shinagare AB, O'Regan K, et al. Imaging features of bowel toxicities in the setting of molecular targeted therapies in cancer patients. Br J Radiol. 2012;85:1420–1426. doi: 10.1259/bjr/19815818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shaw AT, Yeap BY, Mino-Kenudson M, Digumarthy SR, Costa DB, Heist RS, et al. Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4-ALK. J Clin Oncol. 2009;27:4247–4253. doi: 10.1200/JCO.2009.22.6993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yamamoto S, Korn RL, Oklu R, Migdal C, Gotway MB, Weiss GJ, et al. ALK molecular phenotype in non-small cell lung cancer: CT radiogenomic characterization. Radiology. 2014;272:568–576. doi: 10.1148/radiol.14140789. [DOI] [PubMed] [Google Scholar]
- 29.Ou SH, Bartlett CH, Mino-Kenudson M, Cui J, Iafrate AJ. Crizotinib for the treatment of ALK-rearranged non-small cell lung cancer: a success story to usher in the second decade of molecular targeted therapy in oncology. Oncologist. 2012;17:1351–1375. doi: 10.1634/theoncologist.2012-0311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shaw AT, Kim DW, Nakagawa K, Seto T, Crinó L, Ahn MJ, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. 2013;368:2385–2394. doi: 10.1056/NEJMoa1214886. [DOI] [PubMed] [Google Scholar]
- 31.Ou SH, Bazhenova L, Camidge DR, Solomon BJ, Herman J, Kain T, et al. Rapid and dramatic radiographic and clinical response to an ALK inhibitor (crizotinib, PF02341066) in an ALK translocation-positive patient with non-small cell lung cancer. J Thorac Oncol. 2010;5:2044–2046. doi: 10.1097/JTO.0b013e318200f9ff. [DOI] [PubMed] [Google Scholar]
- 32.Nishino M, Hatabu H, Johnson BE, McLoud TC. State of the art: response assessment in lung cancer in the era of genomic medicine. Radiology. 2014;271:6–27. doi: 10.1148/radiol.14122524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Choi YL, Soda M, Yamashita Y, Ueno T, Takashima J, Nakajima T, et al. EML4-ALK mutations in lung cancer that confer resistance to ALK inhibitors. N Engl J Med. 2010;363:1734–1739. doi: 10.1056/NEJMoa1007478. [DOI] [PubMed] [Google Scholar]
- 34.Costa DB, Shaw AT, Ou SH, Solomon BJ, Riely GJ, Ahn MJ, et al. Clinical experience with crizotinib in patients with advanced ALK-rearranged non-small-cell lung cancer and brain metastases. J Clin Oncol. 2015;33:1881–1888. doi: 10.1200/JCO.2014.59.0539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kinoshita K, Asoh K, Furuichi N, Ito T, Kawada H, Hara S, et al. Design and synthesis of a highly selective, orally active and potent anaplastic lymphoma kinase inhibitor (CH5424802) Bioorg Med Chem. 2012;20:1271–1280. doi: 10.1016/j.bmc.2011.12.021. [DOI] [PubMed] [Google Scholar]
- 36.Gadgeel SM, Gandhi L, Riely GJ, Chiappori AA, West HL, Azada MC, et al. Safety and activity of alectinib against systemic disease and brain metastases in patients with crizotinib-resistant ALK-rearranged non-small-cell lung cancer (AF-002JG): results from the dose-finding portion of a phase 1/2 study. Lancet Oncol. 2014;15:1119–1128. doi: 10.1016/S1470-2045(14)70362-6. [DOI] [PubMed] [Google Scholar]
- 37.Schnell P, Bartlett CH, Solomon BJ, Tassell V, Shaw AT, de Pas T, et al. Complex renal cysts associated with crizotinib treatment. Cancer Med. 2015;4:887–896. doi: 10.1002/cam4.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weickhardt AJ, Rothman MS, Salian-Mehta S, Kiseljak-Vassiliades K, Oton AB, Doebele RC, et al. Rapid-onset hypogonadism secondary to crizotinib use in men with metastatic nonsmall cell lung cancer. Cancer. 2012;118:5302–5309. doi: 10.1002/cncr.27450. [DOI] [PubMed] [Google Scholar]
- 39.Cadoo KA, Fornier MN, Morris PG. Biological subtypes of breast cancer: current concepts and implications for recurrence patterns. Q J Nucl Med Mol Imaging. 2013;57:312–321. [PubMed] [Google Scholar]
- 40.Morrow M. Personalizing extent of breast cancer surgery according to molecular subtypes. Breast. 2013;22(Suppl 2):S106–S109. doi: 10.1016/j.breast.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 41.Kennecke H, Yerushalmi R, Woods R, Cheang MC, Voduc D, Speers CH, et al. Metastatic behavior of breast cancer subtypes. J Clin Oncol. 2010;28:3271–3277. doi: 10.1200/JCO.2009.25.9820. [DOI] [PubMed] [Google Scholar]
- 42.Bria E, Cuppone F, Fornier M, Nisticò C, Carlini P, Milella M, et al. Cardiotoxicity and incidence of brain metastases after adjuvant trastuzumab for early breast cancer: the dark side of the moon? A meta-analysis of the randomized trials. Breast Cancer Res Treat. 2008;109:231–223. doi: 10.1007/s10549-007-9663-z. [DOI] [PubMed] [Google Scholar]
- 43.Ang KK, Berkey BA, Tu X, Zhang HZ, Katz R, Hammond EH, et al. Impact of epidermal growth factor receptor expression on survival and pattern of relapse in patients with advanced head and neck carcinoma. Cancer Res. 2002;62:7350–7356. [PubMed] [Google Scholar]
- 44.Seiwert TY, Zuo Z, Keck MK, Khattri A, Pedamallu CS, Stricker T, et al. Integrative and comparative genomic analysis of HPV-positive and HPV-negative head and neck squamous cell carcinomas. Clin Cancer Res. 2015;21:632–641. doi: 10.1158/1078-0432.CCR-13-3310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bonner JA, Harari PM, Giralt J, Cohen RB, Jones CU, Sur RK, et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol. 2010;11:21–28. doi: 10.1016/S1470-2045(09)70311-0. [DOI] [PubMed] [Google Scholar]
- 46.Yazdi MH, Faramarzi MA, Nikfar S, Abdollahi M. A comprehensive review of clinical trials on EGFR inhibitors such as cetuximab and panitumumab as monotherapy and in combination for treatment of metastatic colorectal cancer. Avicenna J Med Biotechnol. 2015;7:134–144. [PMC free article] [PubMed] [Google Scholar]
- 47.Saltz LB, Meropol NJ, Loehrer PJ, Sr, Needle MN, Kopit J, Mayer RJ. Phase II trial of cetuximab in patients with refractory colorectal cancer that expresses the epidermal growth factor receptor. J Clin Oncol. 2004;22:1201–1218. doi: 10.1200/JCO.2004.10.182. [DOI] [PubMed] [Google Scholar]
- 48.Dong F, Kojiro S, Borger DR, Growdon WB, Oliva E. Squamous cell carcinoma of the vulva: a subclassification of 97 cases by clinicopathologic, immunohistochemical, and molecular features (p16, p53, and EGFR) Am J Surg Pathol. 2015;39:1045–1053. doi: 10.1097/PAS.0000000000000454. [DOI] [PubMed] [Google Scholar]
- 49.Santos M, Landolfi S, Olivella A, Lloveras B, Klaustermeier J, Suárez H, et al. p16 overexpression identifies HPV-positive vulvar squamous cell carcinomas. Am J Surg Pathol. 2006;30:1347–1356. doi: 10.1097/01.pas.0000213251.82940.bf. [DOI] [PubMed] [Google Scholar]
- 50.Scheistrøen M, Tropé C, Pettersen EO, Nesland JM. p53 protein expression in squamous cell carcinoma of the vulva. Cancer. 1999;85:1133–1138. doi: 10.1002/(SICI)1097-0142(19990301)85:5<1133::AID-CNCR17>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 51.Growdon WB, Boisvert SL, Akhavanfard S, Oliva E, Dias-Santagata DC, Kojiro S, et al. Decreased survival in EGFR gene amplified vulvar carcinoma. Gynecol Oncol. 2008;111:289–297. doi: 10.1016/j.ygyno.2008.07.038. [DOI] [PubMed] [Google Scholar]
- 52.Johnson GA, Mannel R, Khalifa M, Walker JL, Wren M, Min KW, et al. Epidermal growth factor receptor in vulvar malignancies and its relationship to metastasis and patient survival. Gynecol Oncol. 1997;65:425–429. doi: 10.1006/gyno.1997.4660. [DOI] [PubMed] [Google Scholar]
- 53.Horowitz NS, Olawaiye AB, Borger DR, Growdon WB, Krasner CN, Matulonis UA, et al. Phase II trial of erlotinib in women with squamous cell carcinoma of the vulva. Gynecol Oncol. 2012;127:141–146. doi: 10.1016/j.ygyno.2012.06.028. [DOI] [PubMed] [Google Scholar]
- 54.Brugières L, Pacquement H, Le Deley MC, Leverger G, Lutz P, Paillard C, et al. Single-drug vinblastine as salvage treatment for refractory or relapsed anaplastic large-cell lymphoma: a report from the French Society of Pediatric Oncology. J Clin Oncol. 2009;27:5056–5061. doi: 10.1200/JCO.2008.20.1764. [DOI] [PubMed] [Google Scholar]
- 55.Sibon D, Fournier M, Brière J, Lamant L, Haioun C, Coiffier B, et al. Long-term outcome of adults with systemic anaplastic large-cell lymphoma treated within the Groupe d'Etude des Lymphomes de l'Adulte trials. J Clin Oncol. 2012;30:3939–3946. doi: 10.1200/JCO.2012.42.2345. [DOI] [PubMed] [Google Scholar]
- 56.Mossé YP, Lim MS, Voss SD, Wilner K, Ruffner K, Laliberte J, et al. Safety and activity of crizotinib for paediatric patients with refractory solid tumours or anaplastic large-cell lymphoma: a Children's Oncology Group phase 1 consortium study. Lancet Oncol. 2013;14:472–480. doi: 10.1016/S1470-2045(13)70095-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Coffin CM, Watterson J, Priest JR, Dehner LP. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol. 1995;19:859–872. doi: 10.1097/00000478-199508000-00001. [DOI] [PubMed] [Google Scholar]
- 58.Coffin CM, Hornick JL, Fletcher CD. Inflammatory myofibroblastic tumor: comparison of clinicopathologic, histologic, and immunohistochemical features including ALK expression in atypical and aggressive cases. Am J Surg Pathol. 2007;31:509–520. doi: 10.1097/01.pas.0000213393.57322.c7. [DOI] [PubMed] [Google Scholar]
- 59.Antonescu CR, Suurmeijer AJ, Zhang L, Sung YS, Jungbluth AA, Travis WD, et al. Molecular characterization of inflammatory myofibroblastic tumors with frequent ALK and ROS1 gene fusions and rare novel RET rearrangement. Am J Surg Pathol. 2015;39:957–967. doi: 10.1097/PAS.0000000000000404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chan JK, Cheuk W, Shimizu M. Anaplastic lymphoma kinase expression in inflammatory pseudotumors. Am J Surg Pathol. 2001;25:761–768. doi: 10.1097/00000478-200106000-00007. [DOI] [PubMed] [Google Scholar]
- 61.Pugh TJ, Morozova O, Attiyeh EF, Asgharzadeh S, Wei JS, Auclair D, et al. The genetic landscape of high-risk neuroblastoma. Nat Genet. 2013;45:279–284. doi: 10.1038/ng.2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mossé YP, Laudenslager M, Longo L, Cole KA, Wood A, Attiyeh EF, et al. Identification of ALK as a major familial neuroblastoma predisposition gene. Nature. 2008;455:930–935. doi: 10.1038/nature07261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.De Brouwer S, De Preter K, Kumps C, Zabrocki P, Porcu M, Westerhout EM, et al. Meta-analysis of neuroblastomas reveals a skewed ALK mutation spectrum in tumors with MYCN amplification. Clin Cancer Res. 2010;16:4353–4362. doi: 10.1158/1078-0432.CCR-09-2660. [DOI] [PubMed] [Google Scholar]