Abstract
The purpose of the article is to describe the various radiology consultation models in the Era of Precision Medicine. Since the inception of our specialty, radiologists have served as consultants to physicians of various disciplines. A variety of radiology consultation services have been described in the literature, including clinical decision support, patient-centric, subspecialty interpretation, and/or some combination of these. In oncology care in particular, case complexity often merits open dialogue with clinical providers. To explore the utility and impact of radiology consultation services in the academic setting, this article will further describe existing consultation models and the circumstances that precipitated their development. The hybrid model successful at our tertiary cancer center is discussed. In addition, the contributions of a consultant radiologist in breast cancer care are reviewed as the archetype of radiology consultation services provided to oncology practitioners.
Keywords: Radiology consultation, Radiology services, Precision medicine, Tertiary cancer center
INTRODUCTION
Since the inception of our specialty, radiologists have served as consultants to physicians of various disciplines, and we continue to diagnose, inform treatment decisions and guide management across the spectrum of medical disease. While the role of the radiologist in the multidisciplinary approach to care is little changed over time, our communication with ordering providers has evolved dramatically. Widely available technologies, including the picture archiving communication system (PACS), appropriateness criteria, and critical results communication systems, amongst others, have had the potential to decrease personalized, one-on-one interactions with referring providers. The means by which we fulfill our consultant role have changed, whereby information/result delivery is facilitated but free exchange of pertinent details is limited in any single clinical scenario.
A variety of radiology consultation services have been described in the literature, aimed at facilitating interactions between radiologists and clinical providers to optimize patient care. Consultation model types include clinical decision support, patient-centric, subspecialty interpretation, and/or some combination of these. In the clinical decision support model, radiologists are consulted by referring clinicians for assistance in radiologic procedure selection and planning. In the patient-centric model, patients are encouraged to interact directly with radiologists, for discussion of results or questions related to their imaging evaluation. The second opinion/subspecialty interpretation is generally sought out by referring clinicians or healthcare teams, but in some instances, is available directly to patients (in the latter instance, typically for a fee) (Table 1) (1).
Table 1. Consultation Models.
| Clinical | Patient | Subspecialty | Hybrid | |
|---|---|---|---|---|
| Who | Clinician | Clinician | Clinician | Clinician |
| Patient | Specialist | |||
| Aim | Guide imaging selection | Increase patient satisfaction | Expert interpretation | Multidisciplinary patient care |
| Increase radiologist visibility | Improved treatment planning | |||
| Outcome | Shared expertise and knowledge | Improved patient satisfaction | Better patient care | Improved productivity, patient care and research collaboration |
| More tailored exams | Improved treatment planning |
In oncology care in particular, case complexity often merits open dialogue with clinical providers. Nuanced, yet critical clinical details may not be readily available in study indications from electronic systems. In tumor board conferences and formal or informal consultation, radiologists play an integral role in multidisciplinary discussions centered on diagnosis, staging, approach to tissue sampling and definitive versus palliative management. At referral centers, outside imaging studies are reviewed in consultation to broaden the team's understanding of the prior workup, minimize duplication of services, and plan subsequent treatments. Imaging studies performed at the home institution are also re-examined to answer specific clinical questions, which may be related to patient symptomatology, underlying tumor genomics, targeted therapy selection, predicted treatment response and/or prognosis. Radiologists as consultants have both an opportunity and an obligation to demonstrate true added value to optimized treatment plans.
To explore the utility and impact of radiology consultation services in the academic setting, this article will further describe existing consultation models and the circumstances that precipitated their development. The hybrid model successful at our tertiary cancer center is discussed. In addition, the contributions of a consultant radiologist in breast cancer care are reviewed as the archetype of radiology consultation services provided to oncology practitioners.
The Clinical Decision Support Model
The concept of a radiology consultation service was first reported in 1979, when Shuman and Heilman (2) described their 2 year experience offering formal radiologic consults to clinicians anticipating complex radiologic work-ups. Referring clinicians would utilize the standard consultation form used for their services, which was then forwarded to the radiology resident assigned to consult that month. The resident would carefully review the patient's medical record, discuss issues with the appropriate services, and when indicated, perform a physical exam, and examine all prior pertinent imaging studies. A comprehensive radiologic evaluation plan was devised, discussed with the appropriate attending radiologist, and then conveyed to the requesting clinician.
The impetus for starting this service arose from the rising cost of healthcare, with often indiscriminate use of expensive imaging tests, and the simultaneous explosion of technological advances in radiology, as well as marked growth of interventional radiology procedures. The authors reasoned that radiologists are most knowledgeable about varied imaging modalities and their best utilization, as well as the capabilities of radiologic intervention, and should thus be consulted when making imaging decisions regarding complex cases. They describe the mixed responses of both the referring clinicians (some disliking the intrusion into their diagnostic arena), and the radiology residents and staff (some of whom were uneasy with the expansion of clinical interactions), but promoted the concept as deserving of further evaluation.
Several other academic radiology departments have instituted various forms of consultation, using the “clinical decision support model”, in some cases, mandating approval, and in others, offering it as an optional service and educational tool. Baker (3) analyzed several different scenarios where consult radiologists would provide guidance to clinicians in selecting appropriate radiologic studies and/or in planning imaging workups, and showed utility when compared to a control group without access to radiologic consultation. In a pilot study of patients presenting with biliary tract disease, non-emergent gastrointestinal bleeding or abdominal mass, they reported that actively structuring the diagnostic evaluation by a consultant radiologist resulted in a 64% reduction in time to diagnosis and 32% reduction in number of studies performed (3). By embedding a radiology consultant in daily medical rounds on an acute care medical ward, whereby all radiology requests were discussed daily, they reported significantly fewer radiologic examinations were performed, while house staff were educated on proper utilization of imaging tests, a potential means of cost containment (4). In a third study, on an acute care surgical ward, a consultant radiologist reviewed all radiographic studies performed, discussing their limitations, pertinence and cost, and future examination were discussed. Over the study period, the number of CT scans, ultrasound studies and barium studies decreased significantly, and the average length of patient stay decreased by 2.8 days (5).
Seltzer et al. (6) reported a study whereby all body CT scans required consultation with a radiologist prior to scheduling. They noted 95% cooperation by referring clinicians, and described benefits of obtaining more detailed clinical information, thus providing improved scanning protocols, fewer post-CT diagnostic tests, and improved rapport between the referring clinicians and radiologists.
With the ever present reminder of cost containment looming, the role of the radiologist as a consultant offering clinical decision support has been further investigated using several study designs, including optional vs. mandatory, assisting house staff vs. all referring clinicians, incorporated into rounds vs. a stand-alone service (7,8,9). In most institutions it was generally well received, but has had variable success in decreasing the number of studies ordered. Bree et al. (8) found that mandatory radiology precertification in an inpatient setting did not reduce radiology resource utilization. They noted that although participating physicians were supportive, internal medicine ward physicians did not reduce their test ordering, and radiologists, trained in the interpretation of exams, rather than assessment of appropriateness, were reluctant to perform precertification. The authors suggested that practice guidelines might help standardize the consultation process, and that financial incentives may motivate physicians to reduce ancillary tests.
With the advent of PACS, direct interactions with radiologists in reading rooms has declined, in one study, by 82% for general radiography, and 44% for cross sectional imaging studies, despite an increase in overall volume (10). As consultation has been shown to improve cost containment and allow for a more rapid diagnosis, improved communication between referring clinicians and radiologists is imperative. Tillack and Borgstede (11) looked at the impact of embedding radiology reading rooms in the clinic, noting a significantly greater number of visits by referring providers to embedded reading rooms (though the study was slightly confounded by comparing embedded versus non-embedded reading rooms of different specialties, with inherent differences in consultation patterns).
The present emphasis on value (over volume) in health imaging is strongly touted by the American College of Radiology (ACR), as noted in “Imaging 3.0”, which encourages radiologists to assist providers with clinical decision support, to discuss results and provide “actionable, meaningful reports” (12). It is felt that clinical decision support helps to eliminate unnecessary examinations and increases the radiologists' relevance, as well as provides radiologists with better detailed patient information, which allows for more directed protocols and accurate coding for billing.
The Patient-Centric Model
In 1966, Sherman (13) asked, “Is it not really the patient we are obligated to serve above all others?”, and suggested that patients (not their clinicians) are entitled to results of their exams. In 1990, the beginning of malpractice litigation that alleged failure of communication of radiologic results was brought to light in the American College of Radiology (ACR) Bulletin (14). Berlin noted that soon after the expansion of radiologist's duty to directly convey significant radiologic findings to the referring clinician, their role was further extended to include direct communication to patients, fueled by the judicial system, the federal government, the medical community and patients (15). He cites numerous lawsuits where radiologists were found to be negligent for not communicating significant results directly to patients. The United States government's involvement is evident in the Mammography Quality Standards Act, published in October 1992, mandating that all patients receive a summary of their mammographic findings, in layman's terms, within 30 days of their mammogram. Berlin further notes that both the American Medical Association and ACR have language in their bylaws and guidelines, describing the responsibility of the radiologist (and all consulting physicians) to communicate results directly to patients, and answer any questions they might have. However, he goes on to discuss the various difficulties that might arise, including selecting the format of transmissions, the affect on relationships with referring physicians, placing the radiologist in the unenviable position of being asked to advise on treatment options in which he/she is not involved and possibly less knowledgeable.
Several older studies that surveyed patients undergoing radiologic imaging reported patient preferences to hear imaging results from the radiologists interpreting their exams. A small study of 79 cancer patients undergoing CT imaging at a dedicated cancer center reported that 70% wanted the radiologist to disclose their results (16). In a survey of patient preferences of 261 consecutive patients undergoing radiologic evaluation in a large university hospital, the overwhelming majority (92% for normal findings, 87% for abnormal findings) also preferred to get results from the radiologist at the time of the procedure, rather than later, from their referring clinician (17). A follow-up survey of referring clinicians and radiologists concluded that radiologists and referring physicians both tended to support the proposition that, if asked by patients, radiologists should disclose the results of their imaging studies (18). However, given the uncertainties of many, direct patient radiologist communication has not become the standard of care in most general radiology practices.
Recently, the consultation radiologist role has resurfaced in the literature, as a means of increasing the radiologists' visibility to patients. In most scenarios, the ordering physician conveys results to the patient, who is often unaware that a radiologist has played any role in providing his or her care. Several institutions have revisited the exploration of patient preferences in receiving results of radiologic studies. A survey of 129 patients undergoing CT or MRI at an academic medical center outpatient facility revealed that speed of report delivery was the most important factor in patient satisfaction, without an overwhelming preference for which physician provided the results (19). In another study of 86 patients undergoing CT or ultrasound evaluation, patients preferred hearing results from both their referring clinicians and the interpreting radiologist, and found the latter consultation beneficial (20). However, at least 2 other studies noted that most patients preferred to hear from their referring clinicians. 642 responses to a survey of patients undergoing CT or MRI revealed that for both normal and abnormal results, the preferred mode of communication was a phone call from the referring physician (34.1% and 49.8%, respectively) (21). Patients also preferred detailed radiology reports, with some requesting access to key images. In a similar study of patients undergoing CT or MRI at an academic medical center (77%) or a county hospital (23%), among 617 surveys, 63% revealed preference for receiving results from their ordering providers; 64% desired access to their imaging report, and 85% wished to see their images (22).
Mangano et al. (23) have piloted a patient-centered radiology consultation area, where patients meet with a radiologist to discuss their imaging study results. The impetus in piloting this service was to increase the visibility of the radiologist, and increase awareness of the critical role imagers play in healthcare. This has been among the goals of several ACR outreach campaigns, including the Face of Radiology Campaign (24).
Another academic medical center created a unique consultation service, devised to address the ambiguous information legally mandated to be shared with patients following mammograms that reveal dense breast tissue. Following mammography, patients are presented with data regarding breast density and cancer, though without evidence-based guidelines for further evaluation. Sullivan et al. (25) report their experience in providing consultation services to these patients (and referring clinicians), by employing a Registered Radiology Assistant (RRA), who they define as a “mid-level provider who has received advanced education and clinical experience in radiology.” The RRA receives the requests, collects pertinent information and prepares the consultation, thus improving efficiency and optimizing the radiologist's time spent in direct consultation with the patient. Although the consultation service was only utilized by 138 of 7131 (2%) of their dense breast patient population (plus an additional 14 patients whom heard about the service from other sources), over 70% felt sure of their best choice for additional screening and over 78% felt they had gained enough information to make a decision regarding screening following their consultations. The authors concluded that their service provides education, and ultimately improves quality of care.
The Second Opinion/Subspecialty Interpretation Model
The subspecialty interpretation model is based on a general consensus that subspecialists provide better care in their area of expertise than generalists. Although a study evaluating interpretation of pediatric plain radiographs at a rural hospital did not show a statistically significant difference in interpretation between pediatric radiologists and generalists, the authors note that the subspecialists were more accurate (26). In another study, the detection of extracapsular extension of prostate cancer on MRI was significantly affected by the reader's subspecialty experience (27).
Several tertiary care centers have looked at the quantitative effect of radiology consultations on management of cancer patients. One center reported the addition of significant new information in 49% of patients reviewed at their Division of Oncology Radiology Conference, resulting in major changes in management in 37% (28). Two different centers specifically looked at reinterpretation of imaging studies in head and neck cancer patients. The first reported a change in interpretation of 41%, with statistically significant changes in TNM staging in 34% of patients, which altered treatment plans in 98% and affected prognosis in 95% (29). Changes were attributed to lack of subspecialization in head and neck imaging at the outside institution, and to often incomplete clinical information of the original interpreting radiologist. In a similar study, fellowship trained neuroradiologists provided formal second opinions on head and neck imaging studies, resulting in changes in stage in 56% and management changes in 38%, noting 93% accuracy based on pathologic staging as gold standard (30). A recent study at our cancer center evaluated the influence of a second opinion/subspecialty consultation on the surgical management of breast cancer patients (31). They reported changes in 11.7% of patients undergoing surgery for breast cancer. Given the variability in quality of outside studies and their interpretations, and the differences that a comprehensive evaluation may make in a patient's prognosis and treatment strategy, review of outside studies by a specialized oncologic imager is critically important.
Changes in patient care due to direct subspecialty radiology consultation have recently been reported in disciplines other than oncology. Chalian et al. (32) reviewed over 2000 second opinion subspecialty consultations in musculoskeletal radiology, and noted clinically important differences in interpretation in 26.2% overall, and discrepant interpretations in 36.3% of oncologic cases. Based on the final pathologic diagnosis, they reported that second opinion consultations were correct in 82.0% of cases where discrepancies were likely to change patient management. Dickerson et al. (33) also reported significant alterations in surgical decision making when acute care surgeons collaborated directly and in-person with radiologists. They reported that surgeons' diagnostic impressions and medical and/or surgical planning were altered in 43% of cases, and concluded that the in-person collaboration promoted “a shared mental model that facilitates the exchange of complex information.”
Of note, some departments have taken a different approach, choosing to issue a formal dictation of outside studies rather than a verbal consultation and bill for a second opinion read. Yousem (34) chose to upload outside neuroradiology studies to their electronic archive and provide an official dictation, noting the benefits to the referring clinicians including less hassle in bringing studies to radiologists, increased ease in making images available to operating rooms and conference rooms (via PACS), provision of subspecialty interpretations, access to the outside preoperative studies when evaluating for residual disease postoperatively, decreased interruption to workflow (as studies are now read from a PACS system work list), and monetary reimbursement. Given their success in neuroradiology, they have now initiated this approach throughout their department.
Hybrid Radiologic Consultation
At our tertiary care cancer center, imaging plays an integral role in optimizing patient care by guiding decisions regarding diagnosis, staging, tissue sampling, trial eligibility and treatment. Since PACS enables remote access to imaging studies, radiologists are commonly called upon to lend expertise in viewing both our own and outside imaging studies. A large study at our own institution over a decade ago looked at the volume and impact of second opinion consultations, noting an overall increase in daily workload of 18% (35). The impact on workflow, finances, and compensation in terms of relative value units were all considered. Based on the strict reimbursement requirements (which include a written report and documentation of medical necessity), as well as the variable quality of outside imaging studies and time needed to thoroughly review and redictate a study, it was deemed not cost effective to issue formal reports on outside consultation cases. However, referring clinicians strongly favored and valued this service, therefore institute administrators deemed it worthwhile to contract with the imaging department to provide consultation services by a radiologist located within the clinic. Our decision to participate was not only a matter of convenience, profit, and productivity, but one that has been shown to greatly benefit clinicians and patients alike. Monetary compensation for this dedicated radiologist allowed the hiring of an additional full time employee, allowing for fewer interruptions to the radiologists interpreting our home institution's studies, and incidentally increasing productivity overall. Although our survey only captured consultations on outside studies or on our studies that required further comparison, the consult radiologist is responsible for reviewing both on-site studies, as well as those from associated institutions, and is available to perform tumor measurements for clinical trial patients.
At our institution, the success of the consultation service and increasing patient volume has resulted in expanded general and subspecialty oncologic imaging consultation services. The consult radiologist provides several services, including (though not limited to) clinical decision support, interpretations, advice regarding biopsy or treatment planning, and determination of measurable disease to confirm trial eligibility. Given the ease of access and face-to-face interaction, we have noted increased dependence on our interpretation of all studies, including studies from both outside and inside the network, and also our daily services from within the institution. Most importantly, however, the interactions between imagers and oncologists, surgeons, radiation oncologists, nurses and physician assistants, have grown more collegial, and in fact have facilitated research opportunities/collaborative efforts. Thus, radiologists have become more integrated into the multidisciplinary approach which is so critical in caring for cancer patients (36). Van den Abbeele et al. (37) describe this integrated consultation service as only a part of their vision for the role of imaging in optimizing cancer care. They support the use of imaging in pre-clinical studies to facilitate translational research, and also note the importance of effective, specialized training programs for future oncologic imagers.
Case Study in Breast Cancer Consultation
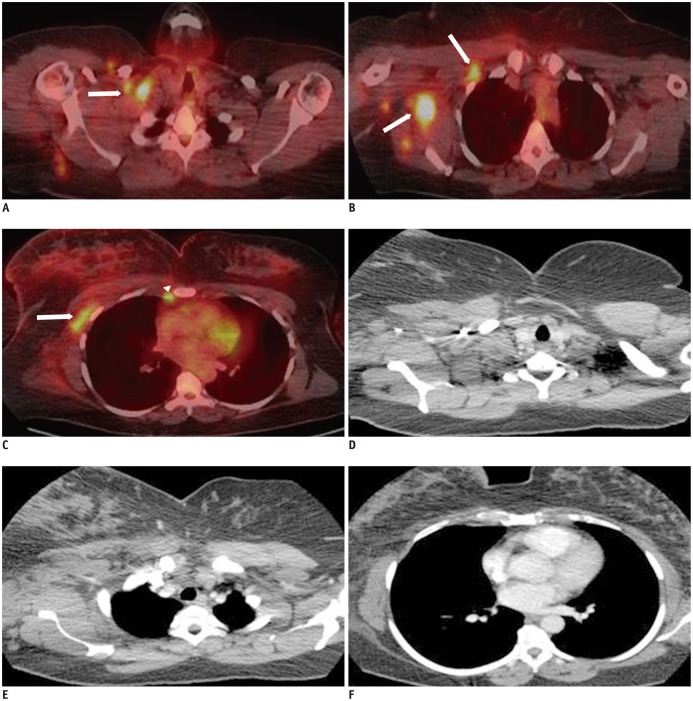
A brief evaluation of various treatment decisions in a breast cancer patient's medical journey elucidates the critical role that radiologists play as consultants to surgeons, radiation oncologists and medical oncologists. After a breast cancer diagnosis is made, a decision between breast conservation therapy and mastectomy must be made. Although a patient may opt for a lumpectomy versus mastectomy by personal choice, the radiologist, upon evaluation of the breast imaging studies, will assist the surgeon in determining whether breast conservation is feasible. Additional sites or wider extent of disease seen with mammography, ultrasound, or MRI, may preclude planned breast conservation surgery. The breast imager is not infrequently consulted by the radiation oncologist when planning radiation therapy for breast cancer patients. The presence of internal mammary lymphadenopathy may change the radiation field, and therefore the radiologist is sought out to provide an opinion regarding the presence of internal mammary lymph nodes and their exact location on MRI and CT, so that radiation treatment can be accurately planned. Patients with a diagnosis of inflammatory breast cancer undergo additional staging with PET-CT imaging, which in a small study at our institution altered the radiation treatment planning in 24% (Fig. 1) (38).
Fig. 1. 43-year-old woman with newly diagnosed inflammatory breast cancer.
A-C. Axial fused PET-CT images of supraclavicular region, upper and mid chest demonstrate focal tracer uptake at right supraclavicular region (white arrow, A), right subpectoral region, right axillary region (white arrows, B), within right anterior chest wall (white arrow, C) and right internal mammary node (white arrowhead, C). D-F. In contrast-enhanced axial CT images at same level, which was performed at outside institution 1 week earlier, lesions are not easily identified. PET-CT = positron emission tomography-computed tomography
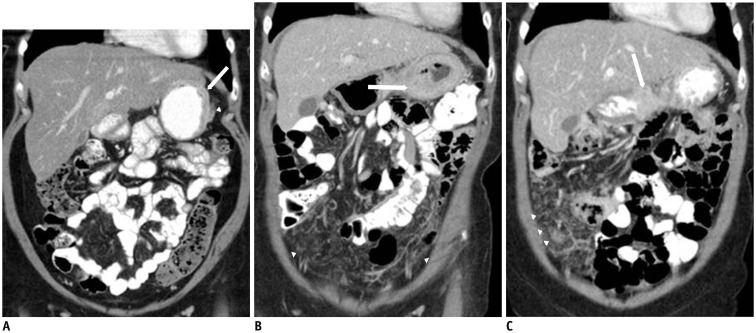
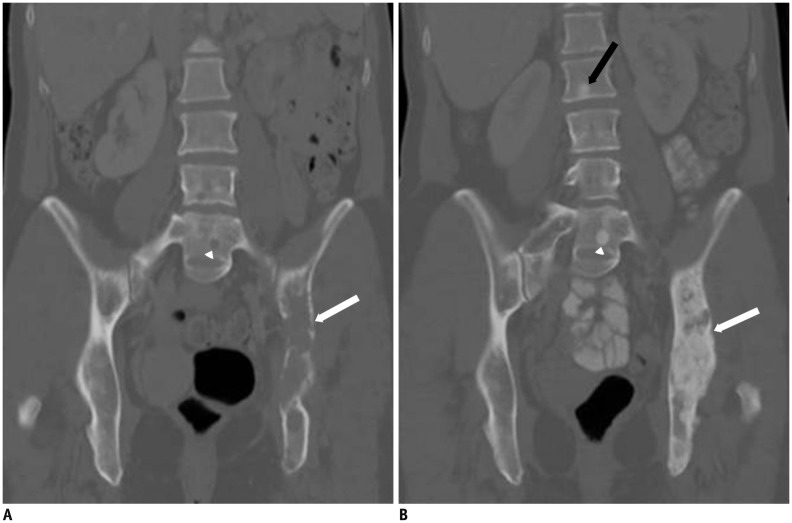
Knowledge of a patient's breast tumor pathology will also affect the consult radiologist's approach to disease evaluation and recommendations for future imaging. In cases of invasive lobular cancer, which are often mammographically occult, sonography or MRI may be important in better defining tumor margins. Given the knowledge of different patterns of metastatic disease spread with lobular breast cancer (versus invasive ductal cancer), a subspecialized oncologic radiologist is more attentive to subtle peritoneal thickening, bowel wall thickening or adnexal changes, that may herald early disease spread, thus suggesting biopsies or close follow-up (Fig. 2). In evaluation of treatment response, the radiologist is often consulted by the oncologist to evaluate changes, especially those not readily evaluated with standard response criteria (such as Response Evaluation Criteria In Solid Tumors [RECIST]). For example, the presence of increased sclerosis in a breast cancer patient with known osseous metastases at a site of previously radiologically occult disease may actually represent response, rather than disease progression as described in the University of Texas MD Anderson Cancer Center criteria (MDA criteria), and must be viewed in light of other changes (Fig. 3) (39). Many, increasing, radiologic response criteria are not necessarily known to many referring clinicians.
Fig. 2. 51-year-old woman with invasive lobular breast cancer.
A. Contrast-enhanced coronal CT image of abdomen reveal mild gastric wall thickening (white arrow, A) with minimal perigastric stranding (white arrowhead, A). B. Follow-up contrast-enhanced coronal CT image after 3 months demonstrates marked increase of gastric thickening (white arrow, B) and new peritoneal carcinomatosis (white arrowheads, B). C. Follow-up contrast-enhanced coronal CT image after 3 months demonstrates further interval increase of gastric thickening (white arrow, C) and worsening of measurable and non-measurable peritoneal disease (white arrowheads, C).
Fig. 3. 48-year-old woman with advanced breast cancer metastatic to bones.
A. Coronal CT image of the abdomen (bone window) reveal extensive lytic lesion involving left iliac bone (white arrow, A) and small lytic lesion within L5 vertebral body (white arrowhead, A). B. Follow-up coronal CT image of abdomen (bone window) shows marked increased sclerosis of left iliac lesion (white arrow, B), L5 vertebral body lesion (white arrowhead) and apparent new well-defined sclerotic lesion within L2 vertebral body (black arrow, B), which is consistent with treatment response.
The combination of imaging expertise, knowledge of disease presentation and patterns of spread, as well as responses to therapeutic options with their potential toxicities and complications make the consultant radiologist vitally important to patient care in the oncologic setting. It is often the radiologist who will first detect signs of drug toxicity or will note disease that will preclude the use of certain medications. As newer therapies have been developed, response criteria have changed to address the varied appearances of tumor response, and different patterns of drug toxicity have been noted. Therefore, it is critical that radiologists interact personally with oncologists and other members of the oncology care team to be made aware of the newest therapies. Together, care teams can learn about their resultant imaging findings, as well as their potential complications and toxicities. This relationship is mutually beneficial, affording imagers the ability to stay abreast of continuously changing therapeutic advances and the opportunity to acquire information about individual patients and their specific radiologic queries, as well as providing referring clinicians with radiologic expertise to help provide the best care to their patients.
CONCLUSION
In the last several years, there has been much focus on the value of imaging in healthcare, with campaigns sponsored by the ACR, and multiple publications urging radiologists to take a more active role in reaching out to clinicians and patients as a consultant (40,41,42). This report summarizes several different models of consultation services which address various end goals including optimization of interdisciplinary care foremost. At our tertiary center, a hybrid model has been incorporated to serve the specific needs of our patients and providers, aimed at cultivating these relationships and leveraging the strengths of our cancer imaging practice. In coming years, it will be important to quantify the added value of radiology consultation, as well as secure buy-in from the stakeholders on a broader scale.
References
- 1.Shaikh S, Bafana R, Halabi SS. Concierge and second-opinion radiology: review of current practices. Curr Probl Diagn Radiol. 2016;45:111–114. doi: 10.1067/j.cpradiol.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 2.Shuman WP, Heilman RS. The radiologist as a consultant. JAMA. 1979;242:1519–1520. [PubMed] [Google Scholar]
- 3.Baker SR. The operation of a radiology consultation service in an acute care hospital. JAMA. 1982;248:2152–2154. [PubMed] [Google Scholar]
- 4.Baker SR, Rosenberg ZS, Adel H. The operation of a ward-based radiology consultation service. Radiology. 1984;152:331–333. doi: 10.1148/radiology.152.2.6739794. [DOI] [PubMed] [Google Scholar]
- 5.Baker SR, Stein HD. Radiologic consultation: its application to an acute care surgical ward. AJR Am J Roentgenol. 1986;147:637–640. doi: 10.2214/ajr.147.3.637. [DOI] [PubMed] [Google Scholar]
- 6.Seltzer SE, Beard JO, Adams DF. Radiologist as consultant: direct contact between referring clinician and radiologist before CT examination. AJR Am J Roentgenol. 1985;144:661–664. doi: 10.2214/ajr.144.4.661. [DOI] [PubMed] [Google Scholar]
- 7.Khorasani R, Silverman SG, Meyer JE, Gibson M, Weissman BN, Seltzer SE. Design and implementation of a new radiology consultation service in a teaching hospital. AJR Am J Roentgenol. 1994;163:457–459. doi: 10.2214/ajr.163.2.8037049. [DOI] [PubMed] [Google Scholar]
- 8.Bree RL, Kazerooni EA, Katz SJ. Effect of mandatory radiology consultation on inpatient imaging use. A randomized controlled trial. JAMA. 1996;276:1595–1598. [PubMed] [Google Scholar]
- 9.Gottlieb RH, Hollenberg GM, Fultz PJ, Rubens DJ. Radiologic consultation: effect on inpatient diagnostic imaging evaluation in a teaching hospital. Acad Radiol. 1997;4:217–221. doi: 10.1016/s1076-6332(05)80294-6. [DOI] [PubMed] [Google Scholar]
- 10.Reiner B, Siegel E, Protopapas Z, Hooper F, Ghebrekidan H, Scanlon M. Impact of filmless radiology on frequency of clinician consultations with radiologists. AJR Am J Roentgenol. 1999;173:1169–1172. doi: 10.2214/ajr.173.5.10541082. [DOI] [PubMed] [Google Scholar]
- 11.Tillack AA, Borgstede JP. An evaluation of the impact of clinically embedded reading rooms on radiologist-referring clinician communication. J Am Coll Radiol. 2013;10:368–372. doi: 10.1016/j.jacr.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 12.American College of Radiology. Imaging 3.0™. [Accessed January 17, 2016]. http://www.acr.org/Advocacy/Economics-Health-Policy/Imaging-3.
- 13.Sherman RS. Whom do we serve? Radiology. 1966;87:147–148. [Google Scholar]
- 14.Liston SE. A new type of cancer lawsuit is emerging. ACR Bulletin. 1990;46:14. [Google Scholar]
- 15.Berlin L. Communicating results of all radiologic examinations directly to patients: has the time come? AJR Am J Roentgenol. 2007;189:1275–1282. doi: 10.2214/AJR.07.2740. [DOI] [PubMed] [Google Scholar]
- 16.Peteet JR, Stomper PC, Ross DM, Cotton V, Truesdell P, Moczynski W. Emotional support for patients with cancer who are undergoing CT: semistructured interviews of patients at a cancer institute. Radiology. 1992;182:99–102. doi: 10.1148/radiology.182.1.1727318. [DOI] [PubMed] [Google Scholar]
- 17.Schreiber MH, Leonard M, Jr, Rieniets CY. Disclosure of imaging findings to patients directly by radiologists: survey of patients' preferences. AJR Am J Roentgenol. 1995;165:467–469. doi: 10.2214/ajr.165.2.7618577. [DOI] [PubMed] [Google Scholar]
- 18.Schreiber MH. Direct disclosure by radiologists of imaging findings to patients: a survey of radiologists and medical staff members. AJR Am J Roentgenol. 1996;167:1091–1093. doi: 10.2214/ajr.167.5.8911156. [DOI] [PubMed] [Google Scholar]
- 19.Basu PA, Ruiz-Wibbelsmann JA, Spielman SB, Van Dalsem VF, 3rd, Rosenberg JK, Glazer GM. Creating a patient-centered imaging service: determining what patients want. AJR Am J Roentgenol. 2011;196:605–610. doi: 10.2214/AJR.10.5333. [DOI] [PubMed] [Google Scholar]
- 20.Pahade J, Couto C, Davis RB, Patel P, Siewert B, Rosen MP. Reviewing imaging examination results with a radiologist immediately after study completion: patient preferences and assessment of feasibility in an academic department. AJR Am J Roentgenol. 2012;199:844–851. doi: 10.2214/AJR.11.8064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mangano MD, Rahman A, Choy G, Sahani DV, Boland GW, Gunn AJ. Radiologists' role in the communication of imaging examination results to patients: perceptions and preferences of patients. AJR Am J Roentgenol. 2014;203:1034–1039. doi: 10.2214/AJR.14.12470. [DOI] [PubMed] [Google Scholar]
- 22.Cabarrus M, Naeger DM, Rybkin A, Qayyum A. Patients prefer results from the ordering provider and access to their radiology reports. J Am Coll Radiol. 2015;12:556–562. doi: 10.1016/j.jacr.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 23.Mangano MD, Bennett SE, Gunn AJ, Sahani DV, Choy G. Creating a patient-centered radiology practice through the establishment of a diagnostic radiology consultation clinic. AJR Am J Roentgenol. 2015;205:95–99. doi: 10.2214/AJR.14.14165. [DOI] [PubMed] [Google Scholar]
- 24.Neiman HL. Face of Radiology campaign. Acad Radiol. 2009;16:517–520. doi: 10.1016/j.acra.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 25.Sullivan CL, Pandya A, Min RJ, Drotman M, Hentel K. The development and implementation of a patient-centered radiology consultation service: a focus on breast density and additional screening options. Clin Imaging. 2015;39:731–734. doi: 10.1016/j.clinimag.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 26.Franken EA, Jr, Berbaum KS, Brandser EA, D'Alessandro MP, Schweiger GD, Smith WL. Pediatric radiology at a rural hospital: value of teleradiology and subspecialty consultation. AJR Am J Roentgenol. 1997;168:1349–1352. doi: 10.2214/ajr.168.5.9129442. [DOI] [PubMed] [Google Scholar]
- 27.Mullerad M, Hricak H, Wang L, Chen HN, Kattan MW, Scardino PT. Prostate cancer: detection of extracapsular extension by genitourinary and general body radiologists at MR imaging. Radiology. 2004;232:140–146. doi: 10.1148/radiol.2321031254. [DOI] [PubMed] [Google Scholar]
- 28.Brook OR, Hakmon T, Brook A, Dudnik E, Kuten A, Engel A. The effect of a Radiology Conference consultation on cancer patients management. Ann Oncol. 2011;22:1204–1208. doi: 10.1093/annonc/mdq581. [DOI] [PubMed] [Google Scholar]
- 29.Loevner LA, Sonners AI, Schulman BJ, Slawek K, Weber RS, Rosenthal DI, et al. Reinterpretation of cross-sectional images in patients with head and neck cancer in the setting of a multidisciplinary cancer center. AJNR Am J Neuroradiol. 2002;23:1622–1626. [PMC free article] [PubMed] [Google Scholar]
- 30.Lysack JT, Hoy M, Hudon ME, Nakoneshny SC, Chandarana SP, Matthews TW, et al. Impact of neuroradiologist second opinion on staging and management of head and neck cancer. J Otolaryngol Head Neck Surg. 2013;42:39. doi: 10.1186/1916-0216-42-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mallory MA, Losk K, Lin NU, Sagara Y, Birdwell RL, Cutone L, et al. The influence of radiology image consultation in the surgical management of breast cancer patients. Ann Surg Oncol. 2015;22:3383–3388. doi: 10.1245/s10434-015-4663-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chalian M, Del Grande F, Thakkar RS, Jalali SF, Chhabra A, Carrino JA. Second-opinion subspecialty consultations in musculoskeletal radiology. AJR Am J Roentgenol. 2016;206:1217–1221. doi: 10.2214/AJR.15.14540. [DOI] [PubMed] [Google Scholar]
- 33.Dickerson EC, Alam HB, Brown RK, Stojanovska J, Davenport MS Michigan Radiology Quality Collaborative. In-person communication between radiologists and acute care surgeons leads to significant alterations in surgical decision making. J Am Coll Radiol. 2016;13:943–949. doi: 10.1016/j.jacr.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 34.Yousem DM. Establishing an outside film reading service/dealing with turf issues: unintended consequences. J Am Coll Radiol. 2010;7:480–481. doi: 10.1016/j.jacr.2009.11.025. [DOI] [PubMed] [Google Scholar]
- 35.DiPiro PJ, vanSonnenberg E, Tumeh SS, Ros PR. Volume and impact of second-opinion consultations by radiologists at a tertiary care cancer center: data. Acad Radiol. 2002;9:1430–1433. doi: 10.1016/s1076-6332(03)80671-2. [DOI] [PubMed] [Google Scholar]
- 36.Fennell ML, Das IP, Clauser S, Petrelli N, Salner A. The organization of multidisciplinary care teams: modeling internal and external influences on cancer care quality. J Natl Cancer Inst Monogr. 2010;2010:72–80. doi: 10.1093/jncimonographs/lgq010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Van den Abbeele AD, Krajewski KM, Tirumani SH, Fennessy FM, DiPiro PJ, Nguyen QD, et al. Cancer imaging at the crossroads of precision medicine: perspective from an academic imaging department in a comprehensive cancer center. J Am Coll Radiol. 2016;13:365–371. doi: 10.1016/j.jacr.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 38.Jacene H, DiPiro P, Bellon J, Nakhlis F, Hirshfield-Bartek J, Yeh E, et al. Discrepancy between CT and FDG-PET/CT in the staging of patients with inflammatory breast cancer: implications for radiation therapy treatment planning. Cancer Res. 2012;72(24 Suppl) Abstract nr P5-02-01. [Google Scholar]
- 39.Hamaoka T, Madewell JE, Podoloff DA, Hortobagyi GN, Ueno NT. Bone imaging in metastatic breast cancer. J Clin Oncol. 2004;22:2942–2953. doi: 10.1200/JCO.2004.08.181. [DOI] [PubMed] [Google Scholar]
- 40.Norbash A, Bluth E, Lee CI, Francavilla M, Donner M, 3rd, Dutton SC, et al. Radiologist manpower considerations and Imaging 3.0: effort planning for value-based imaging. J Am Coll Radiol. 2014;11:953–958. doi: 10.1016/j.jacr.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 41.Duong PA, Bresnahan B, Pastel DA, Sadigh G, Ballard D, Sullivan JC, et al. Value of imaging part I: perspectives for the academic radiologist. Acad Radiol. 2016;23:18–22. doi: 10.1016/j.acra.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 42.Duong PA, Pastel DA, Sadigh G, Ballard D, Sullivan JC, Bresnahan B, et al. The value of imaging part II: value beyond Image interpretation. Acad Radiol. 2016;23:23–29. doi: 10.1016/j.acra.2015.09.017. [DOI] [PubMed] [Google Scholar]