Abstract
Historically, intersectionality has been an underutilized framework in sociological research on racial/ethnic and gender inequalities in health. To demonstrate its utility and importance, we conduct an intersectional analysis of the social stratification of health using the exemplar of hypertension—a health condition in which racial/ethnic and gender differences have been well-documented. Previous research has tended to examine these differences separately and ignore how the interaction of social status dimensions may influence health over time. Using seven waves of data from the Health and Retirement Study and multilevel logistic regression models, we found a multiplicative effect of race/ethnicity and gender on hypertension risk trajectories, consistent with both an intersectionality perspective and persistent inequality hypothesis. Group differences in past and contemporaneous socioeconomic and behavioral factors did not explain this effect.
Keywords: Race, Gender, Health inequalities, Intersectionality, Life course
Highlights
-
•
Race/ethnicity and gender have multiplicative impacts on hypertension risk.
-
•
Results are largely consistent with intersectionality hypotheses.
-
•
Additive approaches obscure substantively and theoretically important findings.
-
•
Multiplicative impacts of race/ethnicity and gender are stable across age.
-
•
Findings underscore the utility of intersectionality and life course approaches.
Introduction
Stratification scholars widely acknowledge that social status dimensions, such as race/ethnicity, gender, and socioeconomic status (SES), structure lived experience by constraining or bolstering resources, opportunities, and life chances. If we view health as a life chance (Haas, 2006), then it becomes clear that these dimensions also structure susceptibility and resilience to illness. As a result, racial/ethnic, gender, and socioeconomic disparities in health have been increasingly recognized as both consequences of and contributors to social stratification processes across the life course (Haas, 2006, House et al., 1994). What is less well acknowledged is the need for a multidimensional—or intersectional—approach to understanding social stratification generally and the social stratification of health in particular. Instead, it is more common for race/ethnicity, gender, and other dimensions of inequality to be treated as separate categories of analysis or, when examined together, viewed as additive rather than mutually reinforcing and inseparable. Likewise, considering the inextricable linkages among social status dimensions is an uncommonly pursued approach to health disparities research. This neglect may obscure the social processes underlying these disparities.
To demonstrate the utility and importance of an intersectional approach to longitudinal research on health disparities, we use the exemplar of hypertension. In the U.S., hypertension is the leading cause of cardiovascular disease and a major contributor to high medical and work productivity loss costs, home productivity loss, and consequent family financial and caregiving burdens (Druss et al., 2001, Heidenreich et al., 2011, Kessler et al., 2003, Merikangas et al., 2007). Racial/ethnic and gender disparities in hypertension prevalence have been well-documented, suggesting that it is a key contributor to inequalities in life chances. Although many studies have been conducted to identify determinants of hypertension, our understanding of the determinants of hypertension disparities remains incomplete (Flack et al., 2003, Minor et al., 2008, Rieker et al., 2010). Not only have previous studies frequently considered race/ethnicity and gender as separate (rather than intersecting) categories of analysis (see the Canadian study by Veenstra (2013) for an exception), but they also have focused primarily on contemporaneous risk factors rather than risk histories. Moreover, much of what we know about gender and racial/ethnic differences in hypertension—and their age patterns—comes from cross-sectional data (e.g., Cutler et al., 2008; Geronimus, Bound, Keene, & Hicken, 2007), which are not well-suited for testing hypotheses about group differences in intra-individual change with age.
Thus, we extended previous research by using panel data and integrating intersectionality and life course perspectives to examine how race/ethnicity, gender, and age combine to shape hypertension risk trajectories between mid- and late-life among Black, White, and Mexican Americans. Specifically, we sought to determine whether and how racial/ethnic disparities in hypertension trajectories are (en)gendered. Using seven waves of data from the Health and Retirement Study (1992–2004) and multilevel logistic regression models, we investigated whether race/ethnicity and gender combine in a multiplicative fashion—i.e., the intersectionality hypothesis—to produce disparate trajectories of hypertension risk net of early life and contemporaneous social, economic, and behavioral factors. We also tested the alternate hypothesis—i.e., the double jeopardy hypothesis—that the relationships among race/ethnicity and gender are additive. In addition, we tested whether group differences in hypertension risk trajectories are consistent with cumulative advantage/disadvantage, aging-as-leveler, or persistent inequality hypotheses.
Racial/ethnic, gender, and age disparities in hypertension prevalence
Racial/ethnic disparities in hypertension prevalence in the U.S. are well-documented. Non-Hispanic Blacks have had consistently higher rates of hypertension than Whites (Minor et al., 2008, Ong et al., 2007). Conversely, although the prevalence of hypertension has been rising among Mexican Americans (Ghatrif et al., 2011), they typically have rates of hypertension similar to or lower than those of Whites (Gillespie & Hurvitz, 2013). Age-related increases in hypertension prevalence also differ by race/ethnicity, as well as gender. Blacks have an earlier average age of hypertension onset than Whites (Minor et al., 2008, Ong et al., 2007). Moreover, the Black–White gap in hypertension is wider at older ages, particularly among women (Cutler et al., 2008). In fact, using cross-sectional data, Geronimus et al. (2007) identified both an earlier age of onset and more pronounced increase in hypertension prevalence with increasing age among Black women compared to other racial/ethnic-gender groups.
Known risk factors for hypertension do not fully explain hypertension disparities (Flack et al., 2003, Minor et al., 2008, Rieker et al., 2010). In addition, our understanding of the age patterns of hypertension disparities is incomplete due to a dearth of longitudinal studies. Unlike the cross-sectional studies of hypertension that have been conducted to date (e.g., Cutler et al., 2008; Geronimus et al., 2007), longitudinal studies would enable testing hypotheses about group differences in intra-individual change with age and including risk histories instead of limiting potential explanations for disparities to contemporaneous risk factors. Research on hypertension disparities in the U.S. also has not considered race/ethnicity and gender as intersecting (rather than separate) categories of analysis.
Intersectionality as a key mechanism in the social stratification of health
Intersectionality, a concept coined by legal scholar Kimberle Crenshaw (1989), suggests that dimensions of social inequality—such as race/ethnicity and gender—vary as a function of each other, are interconnected or interlocked, and are mutually reinforcing/constitutive. As a result, these “interlocking systems of oppression” (Ore, 2003) simultaneously create unique social locations and structure the lived experience and life chances of the people who occupy them (Collins, 2000). With regard to Black women, for example, intersectionality refers to this group’s simultaneous positioning at the disadvantaged ends of both race/ethnicity and gender hierarchies, and consequently class hierarchies (Collins, 2000, Davis, 1981). Intersectionality, therefore, predicts that Black women are more likely to experience disadvantage than other race/ethnicity-gender groups—a prediction that runs counter to popular notions about the low social status of Black men. Indeed, Black women experience the greatest disadvantages of all racial/ethnic-gender groups across multiple indicators of life chances, including poverty rates (Elemelech & Lu, 2004), income (U.S. Census Bureau 2012), wealth (Chang, 2006), and marriage (Warner & Brown, 2011). This relative disadvantage is posited to result from Black women’s experiences of “a double [or triple] load of discrimination” (Borrell, Kiefe, Williams, Diez-Roux, & Gordon-Larsen, 2006), and/or “gendered racism” (Essed, 1991), as well as additional burdens stemming from the plight of their male counterparts, who suffer disproportionate incarceration, unemployment, and premature mortality (U.S. Department of Labor & U.S. Bureau of Labor Statistics, 2011; Guerino, Harrison, & Sabol, 2011; Xu, Kochanek, Murphy & Tejada-Vera, 2010) (Mullings & Wali, 2001).
These chronic stressors, together with Black women’s perpetual and often unsuccessful attempts to cope with them, could precipitate poor health (Geronimus, 1992, Mullings and Wali, 2001, Thomas et al., 2008). In fact, studies have found that Black women experience multiple chronic stress-related morbidities at a higher rate than other racial/ethnic-gender groups, including Black males (e.g., Bird et al., 2010; Brown & Hargrove, 2013; Geronimus et al., 2007; Geronimus, Hicken, Keene & Bound, 2006b; Read & Gorman, 2006; Warner & Brown 2011). Thus, while Black men live shorter lives than their female counterparts on average, Black women have the shortest healthy life expectancy of all racial/ethnic gender groups.
While there is growing interest in bringing intersectionality to bear on health disparities research (Schulz & Mullings, 2006), few empirical studies have adopted this approach. The vast majority of studies on intersectionality and health have been within-group qualitative studies and/or considered health outcomes other than hypertension (e.g., Haldeman, 2005; Mullings & Wali, 2001). Fewer quantitative studies of health disparities have explicitly applied intersectionality (e.g., Ailshire & House, 2011; Veenstra, 2013; Hinze, Lin & Andersson, 2012; Brown & Hargrove, 2013). Among them, however, are at least two studies that found support for intersectionality, revealing a potential need for more frequent use of this framework. Using cross-sectional data from the National Social Life, Health and Aging Project (2005–2006), Hinze et al. (2012) showed the overlapping and simultaneous impacts of race, gender, and education on self-rated health among Black and White older adults. They found that Black women with less than a high school education had the lowest self-rated health compared to other race–gender–education groups. Using longitudinal data instead, Ailshire and House (2011) found interactive effects of gender, race, SES, and age on body mass index (BMI) trajectories among 25–84 year old Blacks and Whites in the American’s Changing Lives study (1986–2001/2002). Specifically, they found that low-educated and low-income Black women experienced the greatest increase in BMI with age compared to other race–gender–SES groups.
The latter study foreshadows the need for an intersectionality approach to research on hypertension, given that BMI (particularly at levels indicative of obesity) lies along the pathway to hypertension. Racial/ethnic and gender patterns of hypertension prevalence also suggest the need for this approach. Yet when both race/ethnicity and gender have been included in previous quantitative research on hypertension (and other health) disparities, researchers have frequently examined gender effects while stratifying by race (or vice versa); used a “configurational” approach (Alon, 2007)—i.e., one that compares gender-race/ethnicity combinations to one reference group, usually white men (as Ailshire and House did); or, more often, assumed an additive relationship between race/ethnicity and gender.
Intersectionality, however, suggests that the simultaneity of social status dimensions is a multiplicative—not additive—relationship (Crenshaw, 1994, King, 1988). According to additive (also known as “double jeopardy” (King, 1988)) explanatory models, the disadvantages incurred by Black women are the sum of those associated with being Black and those associated with being female. Thus, as Spelman (1988: 125) argues, additive models fail “to note important differences between the contexts in which black women and white women experience sexism” and erroneously assume “that a woman’s racial identity can be ‘subtracted’ from her combined sexual and racial identity.” Instead, the multiplicative relationship between race/ethnicity and gender posited by intersectionality theorists means that treating them as separate dimensions in research is inappropriate (Weber & Fore, 2007) and producing explanations based on their sum is inadequate. Other prevailing approaches to examining racial/ethnic-gender disparities (e.g., the aforementioned configurational approach) also leave open the question of whether the relationship is multiplicative or additive, or do not allow for the formal testing of the interaction as required by an intersectionality analytic approach (Dubrow, 2008, Landry, 2007). In contrast, the aforementioned studies by Hinze et al. (2012) and Ailshire and House (2011) showed that explicitly testing the overlapping and simultaneous impacts of social statuses on health produces a more nuanced understanding of disparities. To date, however, the only study of hypertension disparities to explicitly apply an intersectionality approach relied on cross-sectional data from a non-U.S.-based sample (Veenstra, 2013).
Life course perspectives on the social stratification of health
Life course perspectives on health often are premised on the idea that risk factors may combine cross-sectionally and accumulate or interact with each other longitudinally to impact health trajectories (Kuh & Ben-Schlomo, 2004). A life course perspective on the social stratification of health might then suggest that exposures to risk factors over the life course will vary between social status groups, and that resulting differences in exposure trajectories underlie social inequalities in health trajectories (Hertzman, 2004). Perhaps the most popular life course theory in recent research on the social stratification of health is cumulative advantage/disadvantage (hereafter referred to as “cumulative dis/advantage”). Cumulative dis/advantage refers to the systematic growth of inequality over time due to the social structuring of risks, resources, opportunities, and resultant differences (Dannefer, 1987, O'Rand, 1996). A corollary of this proposition is that early life disadvantages lead to subsequent disadvantages and risk exposures, thereby shaping social, health, and developmental trajectories (O'Rand & Hamil-Luker, 2005). Thus, according to cumulative dis/advantage theory, racial/ethnic and gender disparities in health should increase with increasing age.
Indeed several studies have demonstrated a pattern of racial/ethnic disparities in health that is consistent with cumulative dis/advantage (Ferraro et al., 1997, Kelley-Moore and Kenneth, 2004, Willson et al., 2007). However, relatively few studies have focused on racial/ethnic disparities in adult health trajectories and, of those studies, most focused on Black–White disparities in self-rated health and disability (Ferraro et al., 1997, Kelley-Moore and Kenneth, 2004, Shuey and Andrea, 2008, Taylor, 2008, Willson et al., 2007, Yao and Robert, 2008). The aforementioned intersectional study of hypertension in Canada used cross-sectional data and controlled for age, thereby removing the possibility of examining long-term hypertension patterns (Veenstra, 2013). Indeed, few studies have examined racial/ethnic-gender differences in hypertension trajectories, although analyses of cross-sectional prevalence data suggest there may be a shift in the scaling of age among Blacks, especially Black women, that seems consistent with cumulative dis/advantage (see Geronimus et al., 2007). However, studies that rely on cross-sectional data are incapable of producing valid tests of life course hypotheses (Lynch, 2008) because such data only allow for the examination of average population change across the separate time points. Using panel data instead, as we do in the present study, allows for analysis of trajectories of change within individuals and the testing of cumulative dis/advantage processes.
Combining intersectionality and life course perspectives in research on hypertension disparities
As Collins (2003) writes, “each of us carries around the cumulative effect of our lives within multiple structures of oppression” (p. 598). This assertion, combined with what we know about racial/ethnic, gender, and age patterns of hypertension prevalence, suggest the need for both intersectionality and life course approaches in research on hypertension risk trajectories. Yet, another shortcoming of health disparities research to date is its tendency to ignore how the intersection of race/ethnicity and gender may disadvantage or advantage certain groups over time. As we previously noted, studies that have examined racial/ethnic and gender disparities in health, including hypertension, often relied on data that cannot be used to validly test such life course hypotheses, did not use statistical techniques that allow for the detection of an interaction between race/ethnicity and gender, and/or only focused on Blacks and Whites.
We, therefore, sought to fill these gaps by using panel data on a diverse sample that includes non-Hispanic Blacks, non-Hispanic Whites, and Mexican Americans, and by combining intersectionality and life course perspectives, to test hypotheses (and competing hypotheses) associated with three main research questions:
Do race/ethnicity and gender combine in a multiplicative way to produce disparities in hypertension risk trajectories?
We assumed intersectionality to be present if the hypertension risk trajectories varied across the race/ethnicity-gender groups, and if the gap in hypertension was the largest between individuals with intersecting disadvantages (e.g., Black×female) and those without them (i.e., white×male). Statistical significance of the race/ethnicity×gender interaction term was considered to be the strongest support for intersectionality. We also tested an alternative to this multiplicative relationship—i.e., an additive one consistent with a double jeopardy hypothesis (King, 1988). This alternate hypothesis suggests that the consequences of race/ethnicity and gender are independent of one another (King, 1988) and that the race/ethnicity×gender interaction term will be non-significant (Greenman & Xie, 2008).
Does age amplify the effects of race/ethnicity and gender on hypertension risk trajectories in a way that is consistent with a cumulative dis/advantage hypothesis?
Cumulative dis/advantage is assumed to be present if racial/ethnic and gender disparities in hypertension risk trajectories increase with increasing age. We also tested two alternate hypotheses, i.e., aging-as-leveler and persistent inequality. The aging-as-leveler hypothesis suggests that aging involves negative health consequences for both advantaged and disadvantaged populations, so that hypertension disparities will attenuate with age (Dowd & Bengtson, 1978). The persistent inequality hypothesis suggests that the racial/ethnic-gender disparity in hypertension will persist and remain stable with age (Henretta & Campbell, 1976).
Do differences in social and behavioral factors over the life course mediate racial/ethnic, gender, and racial/ethnic-gender disparities in trajectories of hypertension risk?
Social, economic, and behavioral factors associated with blood pressure or cardiovascular disease, including SES, marriage, smoking, physical inactivity, alcohol consumption, and BMI (Bell et al., 2002, Brummett et al., 2011, Hamil-Luker and Angela M., 2007, James et al., 2006, Marin et al., 2008, Ong et al., 2007, Richardson et al., 2011, Wang and Wang, 2004) are known to leave a substantial portion of variability in hypertension unexplained (Flack et al., 2003). They also do not fully capture the phenomena implicit in intersectionality theory. Thus, we hypothesized that adding these factors to our models would result in only partial attenuation of racial/ethnic-gender disparities in hypertension risk trajectories. This addition remains informative, however, because the previous intersectional study of hypertension (Veenstra, 2013) did not include these variables, thereby limiting their explanatory power and the study’s conclusion validity.
Methods
Data
This study used data from Waves 1 to 7 of the Health and Retirement Study (HRS), which were collected biennially between 1992 and 2004. The target population for the HRS included all English or Spanish-speaking adults in the contiguous United States, aged 51-61 in 1992 (spouses of respondents were interviewed regardless of age-eligibility), who resided in households. Blacks and Hispanics were oversampled to allow for independent analysis of racial groups. Respondents remained in the study if they were institutionalized between 1992 and 2004; only a small proportion of individuals were institutionalized at the target ages of this study. Analyses were based on 1,641 non-Hispanic Blacks, 516 Mexican Americans, and 6,854 non-Hispanic Whites aged 51–61 in 1992. Due to small sample sizes, other racial/ethnic groups and Hispanic subgroups (n=304) were not included in the study. We also excluded the latter because of differences in health profiles among them (e.g., Hummer, Rogers, Amir, Forbes & Frisbie, 2000; Henry-Sanchez & Geronimus, 2013). In other words, we excluded the other Hispanic subgroups because they were too diverse to lump together but too small when considered separately.
Measures
Our outcome of interest was hypertension. Hypertensive status was determined based on respondents answers to the question, “Has a doctor ever told you that you have (had) high blood pressure or hypertension?”, at each wave of the survey. The response was coded 1=yes, 0=no.
The focal predictors in this study were race/ethnicity, gender, and age. Three dummy variables index race/ethnicity: non-Hispanic White (omitted), non-Hispanic Black, and Mexican American. Respondents were considered non-Hispanic White if they reported being White but did not report Hispanic/Latino ethnicity; similarly, individuals were classified as being non-Hispanic Black if they reported being Black but not Hispanic/Latino. Respondents were classified as Mexican American if they reported being Hispanic/Latino, and indicated that they were of Mexican origin. Gender was measured by a dummy variable (1=female; 0=male) and age was measured in years.
The key covariates in this study were early life and contemporaneous socioeconomic resources and health behaviors. Measures of early life socioeconomic resources were indicators of: whether the family was poor (1=poor; 0=not poor), and parents’ educational attainment (1=greater than or equal to high school; 0=otherwise). Measures of contemporaneous social and economic resources included: respondents’ educational attainment measured in years of schooling (0–17); household earnings measured in dollars; Social Security income measured in dollars; current participation in the labor force (1=yes; 0=no); net worth (total assets – total liabilities); lack of health insurance coverage (1=uninsured; 0=insured) ; and marital status (1=unmarried; 0=otherwise). The income and wealth measures included resources from both spouses (for married respondents) and were logged. Prior to logging them, a constant of 1 was added to the raw wealth variable for respondents with values of 0, given that values of 0 cannot be logged and the natural logarithm of 1 is 0 (Wilmoth & Koso, 2002). In cases where respondents had negative values for net worth, the absolute value of the wealth measure was logged and the resulting value was then multiplied by −1 (Haas and Rohlfsen, 2010, Zagorsky, 2005). We also included four indicators of respondents’ health behaviors in our models: whether they were obese (i.e., BMI ≥30), based on self-reported height and weight (1= yes; 0=no); whether they ever smoked (1=yes; 0=no); whether they currently smoke (1=yes; 0=no); and whether they were heavy drinkers, i.e., drink three or more drinks per day (1=yes; 0=no).
We controlled for nativity (i.e., foreign- vs. U.S.-born) because of the potential for bias resulting from the healthy immigrant effect or return migration (Palloni & Arias, 2004), and because previous studies have found that: (1) levels of acculturation—indexed in part by nativity—may have different health implications for male and female Mexican Americans (Gorman, Read & Krueger, 2010); and (2) hypertension prevalence differs between foreign-born and U.S.-born Blacks (Hicks, Fairchild, Cook, & Ayanian, 2003). To minimize the risk of underestimating rates of hypertension among respondents with limited access to care, we also controlled for whether respondents visited a doctor’s office (1=yes) or hospital (1=yes) in the past 12 months. At ages 65 and older, underreporting of hypertensive status may be less likely because individuals are eligible for Medicare benefits. Finally, to account for differential rates of dropout and death attrition, we controlled for the number of measurement occasions (i.e., number of waves interviewed (1–7)) and whether the respondent died during the observation (1=yes; 0=no). Other researchers have shown this approach to be efficient and effective in minimizing biases associated with sample attrition (e.g., Thomas, 2011; Warner & Brown, 2011).
Analytic strategy
Consistent with prior studies that have estimated trajectories of disease onset among HRS participants (Hamil-Luker and Angela M., 2007, O'Rand and Hamil-Luker, 2005), we modeled age-trajectories of hypertension onset risk. We utilized time-varying measures of hypertension diagnoses to estimate population-average trajectories of hypertension risk, which indicate the proportion of the population that has been diagnosed with hypertension by age. We used multilevel logistic regression to investigate disparities in these hypertension risk trajectories because it is well-suited for the assessment of interindividual differences in intraindividual stability and change in health risks with age (Gelman and Hill, 2007, Raudenbush and Bryck, 2002). Specifically, we estimated the impact of race/ethnicity and gender on hypertension risk trajectories using the following equation:
where i and t index the individual and assessment levels, respectively. HYP is the binary response variable indicating the presence of hypertension. β0i is the random intercept, which varies by i with mean = µβ0 and variance = σβ0. Similarly, β1i is the random age coefficient, which varies by i with mean = µβ1 and variance = σβ1. β2 - β9 are fixed effects of primary substantive interest and model age variation in the effects of race/ethnicity and gender on hypertension risk; they may be interpreted as ordinary logistic regression coefficients. βk represents a vector of fixed effects for control variables, which vary across models. No assessment level residual term is estimated in multilevel logistic regression due to identification constraints (Gelman & Hill, 2007).
Thus, the analyses generated individual trajectories based on estimates of person-specific intercepts (initial value) and slopes (rate of change) that describe intra-individual patterns of change in hypertension risk as a function of age. To facilitate parameter interpretation, we rescaled age, making age 51 the intercept; covariates were mean-centered to facilitate model interpretation. A model with random intercepts and random linear age slopes provided the best fit, based on comparisons of nested likelihood ratio tests of various shapes of health trajectories (e.g. linear, quadratic or cubic models). To estimate the effects of the social locations on the trajectory slope, we included interactions among race/ethnicity, gender, and age. For the sake of parsimony and to minimize the problem of collinearity, interactions between covariates and age were included only when they were statistically significant or improved model fit (see Warner & Brown, 2011; Yang & Lee, 2009). Given the complexities associated with interpreting interaction effects in logistic regression, we conducted several sensitivity analyses including using a configurational approach as well as stratified models where we tested for gender differences in the coefficients for race/ethnicity (see Landry, 2007). Notably, these approaches produced similar results that were consistent with the intersectional effects presented here. In light of the robustness of our findings, we present findings from the interaction models because they are the most parsimonious and explicit tests of intercategorical intersectional hypotheses (McCall, 2005, Brown and Hargrove, 2013, Landry, 2007).
The multilevel logistic regression models were fit in R version 2.13.0. (R Development Core Team, Vienna, Austria). Multilevel logistic regression is a subclass of generalized linear mixed models, using a logit as the canonical link function. In these models, the likelihood does not have a closed form; thus, optimization requires approximate methods (Gelman and Hill, 2007, Rabe-Hesketh and Skrondal, 2008). Specifically, the model employs a penalized iteratively reweighted least squares (PIRLS) estimation algorithm, which relies on adaptive Gauss–Hermite quadrature approximation at every iteration of likelihood estimation (Bates, 2011, Bates and DebRoy, 2004, Rabe-Hesketh and Skrondal, 2008). Models were fit varying the number of points in the quadrature approximation to ensure that parameter estimates were stable and unbiased (Rabe-Hesketh & Skrondal, 2008).
Preliminary analyses revealed that measurement occasions (i.e., the number of waves respondents were interviewed) and mortality rates varied along racial/ethnic and gender lines (see Table 1). Moreover, respondents with fewer measurement occasions and those who died were more likely to have hypertension. In light of these findings, we included all respondents who had been observed at least once (including those who died or attrited for other reasons) in the sample to avoid the biases that complete-case analysis would introduce. As previously discussed, we also controlled for differential rates of dropout and death attrition by including indicators of the number of measurement occasions and whether respondents died.
Table 1.
| White |
Black |
Mexican American |
||||
|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | |
| Hypertension | .32 | .29⁎,† | .50⁎ | .56⁎,† | .25⁎ | .33† |
| Age | 55.73 | 55.73 | 55.75 | 55.70 | 55.28⁎ | 55.20⁎ |
| Early life social origins | ||||||
| Family was poor | .24 | .23 | .32⁎ | .32⁎ | .37⁎ | .38⁎ |
| Mother had≥H.S. education | .45 | .40⁎,† | .21⁎ | .18⁎ | .09⁎ | .05⁎ |
| Father had ≥ H.S. education | .39 | .35⁎,† | .18⁎ | .15⁎ | .06⁎ | .07⁎ |
| Adult Socioeconomic Status | ||||||
| Years of education | 12.91 | 12.56⁎,† | 11.03⁎ | 11.52⁎,† | 7.93⁎ | 7.31⁎ |
| Earnings | $29,245 | $22,606⁎,† | $18,031⁎ | $12,599⁎,† | $12,670⁎ | $9,110⁎,† |
| Social security income | $469 | $975⁎,† | $686⁎ | $886⁎,† | $503 | $824⁎,† |
| In the labor force | .81 | .62⁎,† | .65⁎ | .61⁎,† | .69⁎ | .40⁎,† |
| Net worth | $198,718 | $189,844 | $55,957⁎ | $44,095⁎,† | $42,384⁎ | $49,575⁎,† |
| Uninsured | .11 | .15⁎,† | .21⁎ | .21⁎ | .43⁎ | .48⁎ |
| Unmarried | .18 | .25⁎,† | .41⁎ | .59⁎,† | .25 | .35⁎,† |
| Health-related behaviors | ||||||
| Obese (BMI≥30) | .20 | .21 | .24⁎ | .41⁎,† | .25 | .33⁎,† |
| Ever smoked | .74 | .56⁎,† | .73 | .56⁎,† | .79 | .43⁎,† |
| Currently smokes | .27 | .26 | .39⁎ | .24⁎,† | .30 | .21⁎,† |
| Heavy drinker (3+drinks/day) | .09 | .02⁎,† | .11⁎ | .01⁎,† | .11 | .01⁎,† |
| Controls | ||||||
| Foreign-born | .05 | .05 | .05 | .05 | .41⁎ | .43⁎ |
| Been to a doctor | .75 | .83⁎,† | .77⁎ | .86⁎,† | .58⁎ | .69† |
| Been to the hospital | .11 | .09⁎,† | .16⁎ | .15⁎ | .12 | .09 |
| Measurement occasions | 5.75 | 5.99⁎,† | 5.19⁎ | 5.71† | 5.58 | 5.79 |
| Died during observation | .16 | .10⁎,† | .28⁎ | .17† | .13 | .13 |
| N | 3344 | 3510 | 697 | 944 | 254 | 262 |
p<.05 for comparison between men and women within racial/ethnic groups.
Means for dummy variables can be interpreted as the proportion of the sample coded 1 on that indicator.
Welch-Satterthwaite t-tests computed for difference in means with unequal variances.
p<.05 for comparison of racial/ethnic/gender group to White men.
Results
Descriptive statistics
Table 1 presents descriptive statistics and results of t-tests comparing means for all variables in the study by race/ethnicity and gender, i.e., for non-Hispanic White, non-Hispanic Black, and Mexican American men and women in the sample. Compared to White men, the prevalence of hypertension was greater among Black men and women while it was lower among Mexican American men and White women. Among Blacks and Mexican Americans, women had higher prevalence of hypertension than men. Moreover, as predicted by intersectionality, Black women had the highest hypertension prevalence of all race/ethnicity-gender groups.
Compared to White men, women and men in all other race/ethnicity-gender groups were more disadvantaged according to most indicators of early life and contemporaneous SES. Specifically, they were less likely than White men to have had mothers and fathers with at least a high school education, to be insured, and to be in the labor force. On average, they also had lower educational attainment and lower household earnings than White men. With the exception of White women, these groups also were more likely than White men to report having been from a family that was poor.
Compared to their male counterparts of the same race/ethnicity, Mexican American and Black women had less household earnings and more social security income on average; were less likely to be in the labor force and to be married; and more likely to be obese, although less likely to engage in other risk behaviors. Mexican American women were the only group of females to have a higher average net worth than their same-race male counterparts, and Black women were the only group of women to have higher educational attainment than same-race males, despite being more disadvantaged on other SES indicators.
Additive vs. multiplicative hypertension risk trajectory models
Table 2 presents estimates of trajectories of hypertension prevalence between ages 51 and 73 derived from multilevel logistic regression models. Model 1 is a conventional additive model that assumes the consequences of race/ethnicity and gender are independent of each other. Thus, it includes only the main effects of race/ethnicity and gender on the hypertension intercept and linear slope, controlling for immigrant status, death and dropout attrition, and whether respondents have been to the doctor’s office or hospital in the last year. This additive model indicates that only race/ethnicity shapes hypertension risk. Specifically, compared to Whites, Blacks are 1.6 times more likely to have hypertension at age 51 than Whites [OR=2.61, p<.001]. The non-significant odds ratio for the effect of being female on the hypertension intercept suggests that gender does not influence hypertension prevalence. In sum, the effect of race and the absence of a gender effect are assumed to be universal in this additive model.
Table 2.
Impact of race/ethnicity and gender on hypertension trajectories: multilevel logistic regression models (odds ratios; N=9011).
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Fixed Effects | |||
| Intercept | .519⁎⁎⁎ | .552⁎⁎⁎ | .729⁎⁎⁎ |
| Black | 2.614⁎⁎⁎ | 2.088⁎⁎⁎ | 1.790⁎⁎⁎ |
| Mexican American | 1.185 | .913 | .739⁎ |
| Female | .904 | .806⁎⁎⁎ | .769⁎⁎⁎ |
| Black×Female | 1.486⁎⁎⁎ | 1.372⁎⁎⁎ | |
| Mexican American×Female | 1.608⁎⁎⁎ | 1.467⁎⁎ | |
| Linear Slope (Age) | 1.069⁎⁎⁎ | 1.069⁎⁎⁎ | 1.061⁎⁎⁎ |
| Black | .653 | .996 | .997 |
| Mexican American | 1.011 | 1.013 | 1.009 |
| Female | 1.007 | 1.009 | 1.010⁎ |
| Early Life Social Origins | |||
| Family was Poor | .959 | ||
| Mother had ≥ H.S. Education | .940 | ||
| Father had ≥ H.S. Education | 1.071 | ||
| Adult Socioeconomic Status | |||
| Years of Education | .977⁎⁎⁎ | ||
| Earnings (Ln) | .998 | ||
| Social Security Income (Ln) | 1.012⁎⁎ | ||
| In the Labor Force | .815⁎⁎⁎ | ||
| Net Worth (Ln) | .970⁎⁎⁎ | ||
| Uninsured | .949 | ||
| Unmarried | 1.027 | ||
| Health-Related Behaviors | |||
| Obese (BMI ≥ 30) | 2.199⁎⁎⁎ | ||
| Ever Smoked | 1.074⁎ | ||
| Currently Smokes | .754⁎⁎⁎ | ||
| Heavy Drinker (3+ Drinks/Day) | 1.387⁎⁎⁎ | ||
| Controls | |||
| Foreign-Born | .832⁎⁎ | .830⁎⁎ | .804⁎⁎⁎ |
| Been to a Doctor | .502⁎⁎⁎ | .503⁎⁎⁎ | .50⁎⁎⁎ |
| Been to the Hospital | .733⁎⁎⁎ | .731⁎⁎⁎ | .820⁎⁎⁎ |
| Measurement Occasions | .948⁎⁎⁎ | .946⁎⁎⁎ | .946⁎⁎⁎ |
| Died during Observation | 1.331⁎⁎⁎ | 1.326⁎⁎⁎ | 1.237⁎⁎⁎ |
| Random Effects | |||
| Level 2 Intercept | 1.587⁎⁎⁎ | 1.589⁎⁎⁎ | 1.592⁎⁎⁎ |
| Level 2 Age | 1.443⁎⁎⁎ | 1.443⁎⁎⁎ | 1.445⁎⁎⁎ |
p<.05.
p<.01.
p<.001.
To test whether the effects of race and gender are instead contingent upon each other in a multiplicative fashion, i.e., the intersectionality hypothesis, Model 2 (Table 2) adds race/ethnicity×gender interaction terms. As hypothesized, the Black×female and Mexican American×female odds ratios are statistically significant, suggesting that race/ethnicity and gender effects are multiplicative. The combination of a higher odds of hypertension for Blacks compared to whites (OR=2.09, p<.001), a lower odds of hypertension for females compared to males (OR=.81, p<.001), and a higher odds for Black×female compared to other race/ethnicity-gender groups (OR=1.49, p<.001) indicates that the impact of gender on hypertension is racialized: White women have lower odds of hypertension than their White male counterparts while Black women fare worse than Black men. In addition, the Black-White gap in hypertension odds at age 51 is larger among women. Thus, for Black women, racial/ethnic and gender disadvantages are amplified by each other. Mexican American women also are disadvantaged: whereas White women have lower odds of hypertension than White men, Mexican American women have higher odds of hypertension than their Mexican American male counterparts, as evidenced by the non-significant odds ratio for Mexican American, a statistically significant odds ratio less than 1 for female (OR=.81, p<.001) and a statistically significant odds ratio greater than 1 for Mexican American×female (OR=1.61, p<.01). In sum, being a non-Hispanic Black or Mexican American woman increases the odds of hypertension beyond the main effects of race/ethnicity and gender coefficients.
Cumulative dis/advantage vs. other life course hypotheses
The coefficient for the linear slope (1.06, p<.001) in Table 2 indicates that hypertension prevalence increases with age, though there is considerable variability both within and between racial/ethnic-gender groups. The remainder of the findings presented in Table 2 and ancillary analyses (not shown) suggest that there are no interactive influences of race/ethnicity × gender on hypertension risk slopes (i.e., the three-way interaction between race/ethnicity, gender, and age was non-significant). Thus, the multiplicative effects of race/ethnicity and gender on hypertension levels, as evidenced by the significant interaction effects on hypertension intercepts, are carried forward. That is, the effects neither increase nor decrease with age, consistent with the persistent inequality hypothesis.
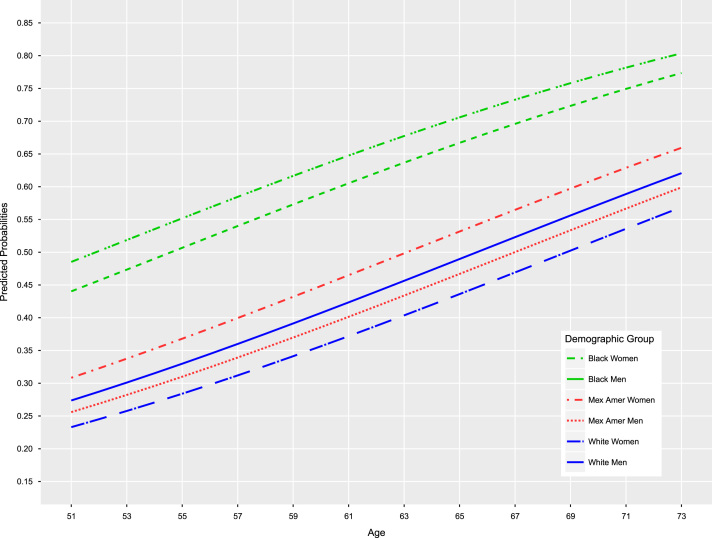
Fig. 1 presents model-implied group-specific hypertension prevalence trajectories, illustrating their magnitude and shape, net of controls. At age 51, Black women have the highest hypertension prevalence (48%), followed (in descending order of prevalence) by Black men (44%), Mexican American women (31%), Mexican American and White men (27%), and White women (23%). This race/ethnicity-gender hierarchy of hypertension prevalence is stable across all ages. It should be noted, however, that Black women’s rate of hypertension at age 51 is not reached until ages 54, 62, 65 and 68 for Black men, Mexican American women, Mexican American and White men, and White women, respectively. Taken together, these patterns suggest an earlier age of onset among Black women but, contrary to our hypothesis, no widening with increasing age (i.e., no cumulative dis/advantage).
Fig. 1.
Predicted hypertension trajectories by race/ethnicity, gender, and age.
Mediators of the hypertension risk trajectory model
To determine what factors underlie the large disparities in hypertension trajectories, Model 3 (Table 2) adds indicators of early life socioeconomic factors, social and economic resources, and health behaviors. We find that the magnitudes of the odds ratios for race/ethnicity (e.g., Black), female, and race/ethnicity×female across Models 2 and 3 are only slightly attenuated and remain statistically significant. Thus, controlling for group differences in these factors fails to fully explain the elevated odds of hypertension faced by non-White females. Specifically, being a non-Hispanic Black or Mexican American woman is associated with 37 and 47% greater odds, respectively, of hypertension than other racial/ethnic-gender groups net of all other variables included in the study.
Discussion
In this study of racial/ethnic and gender disparities in hypertension risk trajectories, we had three primary aims. First, we sought to determine whether race/ethnicity and gender combine to produce disparities in hypertension risk trajectories, and whether the combination was consistent with intersectionality (multiplicative) or double jeopardy (additive) hypotheses. We found that race/ethnicity and gender effects are multiplicative rather than additive. Being a non-Hispanic Black or Mexican American female increased the odds of hypertension beyond the risk imposed by race/ethnicity and gender separately. When we tested the alternate hypothesis of an additive effect of race/ethnicity and gender on hypertension risk trajectories, we found that race/ethnicity—but not gender—shaped hypertension risk. The additive approach, therefore, obscured a substantively and theoretically important finding: among Whites, being a female was protective against hypertension, while it was associated with greater odds of hypertension among non-Hispanic Blacks and Mexican Americans. The fact that simplistic, additive approaches can mask this important heterogeneity underscores the utility of intersectionality perspectives and methods.
Our finding for Black women is consistent with the findings of other studies that demonstrate their health disadvantage compared to other race/ethnicity-gender groups (e.g., Ailshire & House, 2011; Bird et al., 2010; Geronimus, Hicken, Keene, & Bound, 2006a; Hinze et al., 2012; Read & Gorman, 2006; Warner & Brown, 2011), although our analytic approach differed. Our finding that the multiplicative consequences of race/ethnicity and gender are also damaging for Mexican American women is novel and warrants further exploration. Typically, Mexican Americans are omitted from the discourse on hypertension disparities and largely neglected in studies of health disparities that apply an intersectional framework (Zambrana & Dill, 2006). They are, however, one of the fastest growing racial/ethnic groups in the U.S. (Day, 1996) that is projected to occupy an increasing proportion of the aged population (Angel & Whitfield, 2007) and among whom hypertension prevalence has been rising (Ghatrif et al., 2011). Thus, they should be included in life course and intersectionality studies of health.
Our second aim was to understand the nature of the disparities in hypertension risk trajectories and whether and how the pattern was consistent with cumulative dis/advantage or, alternatively, aging-as-leveler or persistent inequality hypotheses. In other words, we examined whether age functioned in combination with race/ethnicity and gender to structure hypertension risk. We found that Black women experience elevated rates of hypertension earlier in the life course than other groups, consistent with findings from cross-sectional research on age patterns of hypertension prevalence (e.g., Geronimus et al., 2007). Yet the pattern of disparities in hypertension risk trajectories was suggestive of persistent inequality: the multiplicative effects of race/ethnicity and gender on hypertension levels were stable across age. Nonetheless, by extending the typical focus of intersectionality and health scholarship on the race–class–gender trifecta (e.g., Schulz & Mullings, 2006) to include age as a dimension of stratification, our findings still make clear that the story of racial/ethnic disparities in hypertension risk trajectories is not complete without concomitant attention to the roles of gender and age. To date, the only other study to examine the effects of intersectional inequality on hypertension controlled for age rather than treating it as a focal variable in the analysis (Veenstra, 2013).
The fact that we did not find evidence of cumulative dis/advantage, and a three-way interaction between race/ethnicity, gender, and age, could be because the accumulation occurs earlier in the life course than the period captured by the HRS. Indeed, evidence from studies of other health outcomes has suggested that the effects of cumulative dis/advantage begin to appear as early as the late teens and early 20s and extend at least into the early 40s (e.g., Rich-Edwards, Buka, Brennan, & Earls, 2003). Moreover, recent research suggests that patterns of disparities in health trajectories may shift from cumulative dis/advantage to persistent inequality between mid- to later-life (House et al., 2005, Shuey and Andrea, 2008). Future research should use other longitudinal datasets with longer and earlier timeframes than the HRS to assess these possibilities—i.e., whether disparities in hypertension risk trajectories across early- to late-adulthood demonstrate a pattern consistent with persistent inequality (as we found) or cumulative dis/advantage (as cross-sectional hypertension prevalence patterns from late adolescence through late adulthood suggest).
Our third aim was to examine whether past and contemporaneous social, economic, and behavioral factors accounted for the observed disparities in hypertension risk trajectories. We included a much wider set of control variables, spanning multiple stages of the life course, than previous studies of hypertension and its health correlates (e.g., Ailshire & House, 2011; Geronimus et al., 2007; Veenstra, 2013). This set included factors that are associated with blood pressure or cardiovascular risk—namely, early life socioeconomic status (Hamil-Luker and Angela M., 2007, Marin et al., 2008), contemporaneous socioeconomic position (James et al., 2006), marriage (Brummett et al., 2011), several health behaviors, including alcohol consumption, smoking, and physical inactivity (Ong et al., 2007, Wang and Wang, 2004), and body mass index (BMI) (Bell et al., 2002, Richardson et al., 2011). However, these factors are known to leave a substantial portion of variability in hypertension unexplained (Flack et al., 2003); they also do not fully capture the phenomena implicit in intersectionality theory. Thus, consistent with our expectation, we found that group differences in these factors explained less than 10% of the elevated hypertension risks experienced by non-Hispanic Black and Mexican American females. This finding suggests (as intersectionality theory also does) that other unmeasured factors could be more important.
A good candidate is chronic stress, given its known vascular effects (Bruner and Marmot, 2001, McEwen and Seeman, 1999). Social scientists have argued that differential exposure to stressful experiences over time (due to the social structuring of exposure) is a key way that racial/ethnic disparities in health trajectories are produced (Thoits, 2010). The “weathering hypothesis,” for example, suggests that Black women experience early health decline due to chronic stressful life circumstances (Geronimus, 1992). It is also well known that groups who encounter the most stressors are the least likely to have the coping and social resources to offset them (Thoits, 2010). Although we included marital status in our analysis, research has found pronounced differences in other buffering social resources (e.g., strong social networks and social ties) across racial groups (Williams, 1992) and racial/ethnic-gender groups (Mair, 2010) that may help explain hypertension disparities (Bell, Thorpe, & LaVeist, 2010). Moreover, prolonged, high-effort coping with chronic stress may add to the physiological wear and tear, and be responsible for the increased prevalence of hypertension among Black women, especially if they have few socioeconomic resources (Etherington, 2015, James and Thomas, 2000).
One of the limitations of this study, however, is the absence of longitudinal measures of stress, social support, and coping—especially measures that capture differences in what is deemed stressful across racial/ethnic groups (Griffith, Ellis, & Allen, 2013) or what is most harmful to specific racial/ethnic-gender groups (Spruill, 2010). This is not unique to the HRS, however. Efforts to identify the unique stressors (other than discrimination) experienced by Black and Mexican American women have primarily been qualitative and they have not been incorporated into major social surveys.
Another key limitation of this study, likely shared by most quantitative intersectionality studies, is the absence of more appropriate measures of race/ethnicity and gender vis-à-vis intersectionality theory. Consistent with an “intercategorical” approach to intersectionality research (McCall, 2005), we made provisional use of existing categories of race/ethnicity and gender to analyze and understand patterns of hypertension disparities. From an intersectionality perspective, however, race/ethnicity and gender should be viewed as socially constructed and historically contingent power relationships—not just attributes or differences in the distributions of attributes (Collins, 2000, Weber and Fore, 2007). This perspective should shift our analytic focus from race to racism and from gender to gender inequality (Mullings, 2006), and ideally to “gendered racism” (Essed, 1991). However, it poses a challenge for life course research on health because available datasets, including the HRS, are not equipped to measure these phenomena. The absence of gendered racism measures, in particular, precludes us from considering what ties race/ethnicity and gender together and produces their multiplicative effect on health (Thomas et al., 2008).
A final limitation of the study pertains to our use of self-reported diagnosis of hypertension—the only measure of hypertensive status consistently available in each wave of the HRS. Although widely used, this measure could have succumbed to errors in physician diagnosis, errors in respondent recall, or racial/ethnic differences in awareness and diagnosis of hypertension (Ostchega, Yoon, Hughes, & Louis, 2008). While we controlled for whether respondents have visited a doctor or hospital in the past year and whether they have health insurance, other studies showing discordance between self-reported and observed measures of hypertension (e.g., Nguyen et al., 2011) suggest that the likelihood of underestimating rates of hypertension by using self-reported receipt of a diagnosis to measure it may remain. Nevertheless, this means our findings may be conservative.
Despite its limitations, this study demonstrates the utility of combining intersectionality and life course perspectives and methods in research on health disparities. It also suggests the need for a reframing of interventions and policies to address these disparities. If race/ethnicity, gender, and age operate together to increase hypertension risk, it is essential that policies and interventions to address this increase are grounded in intersectionality. Failing to do so and focusing instead on racial/ethnic disparities in hypertension without regard for how they are gendered could reduce the benefits of behavioral and clinical interventions to the racial/ethnic-gender groups that are at highest risk. The results of our study, for example, reveal the need for hypertension risk reduction interventions and screening efforts that are targeted toward and tailored specifically for younger African American women. Taken together, these activities will lend substantive support to current interest in intersectionality and health, strengthen its connections to sociological scholarship on the social stratification of health and aging, and, ultimately, help us better understand and address the factors that compromise the health of certain racial/ethnic-gender groups relative to others.
Acknowledgements
This research was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; grant number R01-HD057073), the National Institute on Aging (RCMAR grant number P30AG043073), and the Robert Wood Johnson Foundation Center for Health Policy at Meharry Medical College (RWJF grant number 64300). This research also received support from the Population Research Infrastructure Program awarded to the Carolina Population Center (grant number P2C HD050924) by NICHD.
Contributor Information
Liana J. Richardson, Email: liana_richardson@unc.edu.
Tyson H. Brown, Email: tyson.brown@duke.edu.
References
- Ailshire J.A., House J.S. The unequal burden of weight gain: An intersectional approach to understanding social disparities in BMI trajectories from 1986 to 2001/2002. Social Forces. 2011;90(2):397–423. doi: 10.1093/sf/sor001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alon S. Overlapping disadvantages and the racial/ethnic graduation gap among students attending selective institutions. Social Science Research. 2007;36(4):1475–1499. [Google Scholar]
- Angel J.L., Whitfield K.E. Springer; New York: 2007. The health of aging hispanics: The Mexican-origin population. [Google Scholar]
- Bates, D. (2011). Linear mixed model implementation in lme4. 〈http://cran.r-project.org/web/packages/lme4/vignettes/Implementation.pdf〉.
- Bates D., DebRoy S. Linear mixed models and penalized least squares. Journal of Multivariate Analysis. 2004;91(1):1–17. [Google Scholar]
- Bell A.C., Adair L.S., Popkin B.M. Ethnic differences in the association between body mass index and hypertension. American Journal of Epidemiology. 2002;155(4):346–353. doi: 10.1093/aje/155.4.346. [DOI] [PubMed] [Google Scholar]
- Bell C.N., Thorpe R.J., LaVeist T.A. Race/ethnicity and hypertension: The role of social support. American Journal of Hypertension. 2010;23(5):534–540. doi: 10.1038/ajh.2010.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird C.E., Seeman T., Escarce J.J., Basurto-Davila R., Finch B.K., Dubowitz T., Heron M., Hale Lauren, Merkin Sharon Stein, Weden Margaret, Lurie N. Neighbourhood socioeconomic status and biological 'wear and tear' in a nationally representative sample of U.S. adults. Journal of Epidemiology and Community Health. 2010;64:860–865. doi: 10.1136/jech.2008.084814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrell L.N., Kiefe C.I., Williams D.R., Diez-Roux A.V., Gordon-Larsen P. Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Social Science and Medicine. 2006;63:1415–1427. doi: 10.1016/j.socscimed.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Brown T.H., Hargrove T. Multidimensional approaches to examining gender and racial/ethnic stratification in health. Women, Gender, and Families of Color. 2013;1(2):180–206. [Google Scholar]
- Brummett B.H., Babyak M.A., Siegler I.C., Shanahan M., Harris K.M., Elder G.H., Williams R.B. Systolic blood pressure, socioeconomic status, and biobehavioral risk factors in a nationally representative U.S. young adult sample. Hypertension. 2011;58:161–166. doi: 10.1161/HYPERTENSIONAHA.111.171272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruner E., Marmot M. Social organization, stress, and health. In: Marmot M., Wilkinson R.G., editors. Social determinants of health. Oxford University Press; Oxford: 2001. p. 41. [Google Scholar]
- Chang M.L. Women and wealth. In: Nembhard J.G., Chitej N., editors. Wealth accumulation and communities of color: Current issues. University of Michigan Press; Ann Arbor, MI: 2006. pp. 112–132. [Google Scholar]
- Collins P.H. Routledge; New York: 2000. Black feminist thought: Knowledge, consciousness, and the politics of empowerment. [Google Scholar]
- Collins P.H. Toward a new vision: Race, class, and gender as categories of analysis and connection. In: Ore T.E., editor. The social construction of difference and inequality: race, class, gender, and sexuality. McGraw Hill; Boston, MA: 2003. pp. 591–605. [Google Scholar]
- Crenshaw K. Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum. 1989;1989(1):139–167. [Google Scholar]
- Crenshaw K.W. Mapping the margins: Intersectionality, identity politics, and violence against women of color. In: Fineman M.A., Mykitiuk R., editors. The public nature of private violence. Routledge; New York: 1994. pp. 93–118. [Google Scholar]
- Cutler J.A., Sorlie P.D., Wolz M., Thom T., Fields L.E., Roccella E.J. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- Dannefer D. Aging as intrachohort differentiation: Accentuation, the Matthew effect, and the life course. Sociological Forum. 1987;2(2):211–236. [Google Scholar]
- Davis A.Y. Random House; New York: 1981. Women, race, and class. [Google Scholar]
- Day J.C. U.S. Government Printing Office; Washington, DC: 1996. Population projections of the United States by age, sex, race, and Hispanic origin: 1995 to 2050, U.S. Bureau of the Census, Current population reports. [Google Scholar]
- Dowd J.J., Bengtson V.L. Aging in minority populations: A test of the double jeopardy hypothesis. Journal of Gerontology. 1978;33:427–436. doi: 10.1093/geronj/33.3.427. [DOI] [PubMed] [Google Scholar]
- Druss B.G., Marcus S.C., Olfson M., Tanielian T., Elinson L., Pincus H.A. Comparing the national economic burden of five chronic conditions. Health Affiars. 2001;20(6):233–241. doi: 10.1377/hlthaff.20.6.233. [DOI] [PubMed] [Google Scholar]
- Dubrow J.K. How can we account for intersectionality in quantitative analysis of survey data? Empirical illustration for Central and Eastern Europe. ASK. Research and Methods. 2008;17:85–100. [Google Scholar]
- Elemelech Y., Lu H. Race, ethnicity, and the gender poverty gap. Social Science Research. 2004;33:158–182. [Google Scholar]
- Essed P. Sage; Newbury Park, CA: 1991. Understanding everyday racism: An interdisciplinary theory. [Google Scholar]
- Etherington N. Race, gender, and the resources that matter: An investigation of intersectionality and health. Women and Health. 2015;55(7):754–777. doi: 10.1080/03630242.2015.1050544. [DOI] [PubMed] [Google Scholar]
- Ferraro K.F., Farmer M.M., Wybraniec J.A. Health trajectories: Long-term dynamics among Black and White adults. Journal of Health and Social Behavior. 1997;38:38–54. [PubMed] [Google Scholar]
- Flack J.M., Ferdinand K.C., Nasser S.A. Epidemiology of hypertension and cardiovascular disease in African Americans. Journal of Clinical Hypertension. 2003;5(1 Suppl. 1):S5–S11. doi: 10.1111/j.1524-6175.2003.02152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelman A., Hill J. Cambridge University Press; Cambridge: 2007. Data analysis using regression and multilevel/hierarchical models. [Google Scholar]
- Geronimus A.T. The weathering hypothesis and the health of African-American women and infants: Evidence and speculations. Ethnicity and Disease. 1992;2(3):207–221. [PubMed] [Google Scholar]
- Geronimus A.T., Bound J., Keene D., Hicken M. Black–White differences in age trajectories of hypertension prevalence among adult women and men, 1999–2002. Ethnicity and Disease. 2007;17:40–48. [PubMed] [Google Scholar]
- Geronimus A.T., Hicken M., Keene D., Bound J. Geronimus et al. respond to Thomas' What's missing from the weathering hypothesis? American Journal of Public Health. 2006;96(6):955–956. doi: 10.2105/AJPH.2006.085514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus A.T., Hicken M., Keene D., Bound J. Weathering and age patterns of allostatic load scores among Blacks and Whites in the United States. American Journal of Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghatrif M.A., Yong-fang K., Snih S.A., Raji M.A., Ray L.A., Markides K.S. Trends in hypertension prevalence, awareness, treatment and control in older Mexican Americans, 1993–2005. Annals of Epidemiology. 2011;21:15–25. doi: 10.1016/j.annepidem.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie C.D., Hurvitz K.A. Prevalence of hypertension and controlled hypertension — United States, 2007–2010. MMWR Supplement. 2013;62(3):144–148. [PubMed] [Google Scholar]
- Gorman B.K., Read J.G., Krueger P.M. Gender, acculturation, and health among Mexican Americans. Journal of Health and Social Behavior. 2010;51(4):440–457. doi: 10.1177/0022146510386792. [DOI] [PubMed] [Google Scholar]
- Greenman E., Xie Y. Double jeopardy? The interaction of gender and race on earnings in the United States. Social Forces. 2008;86(3):1217–1244. doi: 10.1353/sof.0.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith D.M., Ellis K.R., Allen J.O. An intersectioanl approach to social determinants of stress for African American Men: Men's and women's perspectives. American Journal of Men's Health. 2013;7(4 Suppl):19S–30S. doi: 10.1177/1557988313480227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerino P., Harrison P.M., Sabol W.J. In: Prisoners in 2010. Bureau of Justice Statistics U.S., editor. Department of Justice; Washington, DC: 2011. [Google Scholar]
- Haas S.A. Health selection and the process of social stratification: The effect of childhood health on socioeconomic attainment. Journal of Health and Social Behavior. 2006;47(4):339–354. doi: 10.1177/002214650604700403. [DOI] [PubMed] [Google Scholar]
- Haas S.A., Rohlfsen L. Life course determinants of racial and ethnic disparities in functional health trajectories. Social Science and Medicine. 2010;70(2):240–250. doi: 10.1016/j.socscimed.2009.10.003. [DOI] [PubMed] [Google Scholar]
- Haldeman K.M. University of North Carolina at Chapel Hill; 2005. Expectant fears and racialized reproduction: African American women's lived experiences of pregnancy and motherhood [Unpublished dissertation] [Google Scholar]
- Hamil-Luker J., O'Rand A.M. Gender differences in the link between childhood socioeconomic conditions and heart attack risk in adulthood. Demography. 2007;44(1):137–158. doi: 10.1353/dem.2007.0004. [DOI] [PubMed] [Google Scholar]
- Heidenreich, Paul A., Justin G. Trogdon, Olga A. Khavjou, Javed Butler, Kathleen Dracup, Michael D. Ezekowitz, Eric A. Finkelstein, Yuling Hong, S. Claiborne Johnston, Amit Khera, Donald M. Lloyd-Jones, Sue A. Nelson, Graham Nichol, Diane Orenstein, Peter W.F. Wilson, and Y. Joseph Woo. 2011. "Forecasting the future of cardiovascular disease in the United States: a policystatement from the American Heart Association." Circulation 123:933-44. [DOI] [PubMed]
- Henretta J.C., Campbell R.T. Status attainment and status maintenance: A study of stratifcation in old age. American Sociological Review. 1976;41:981–992. [Google Scholar]
- Henry-Sanchez B.L., Geronimus A.T. Racial/ethnic disparities in infant mortality among U.S. Latinos: A test of the segmented racialization hypothesis. DuBois Review. 2013;10(1):205–231. [Google Scholar]
- Hertzman C. The life-course contribution to ethnic disparities in health. In: Norman B., Anderson R.A., Bulatao B.C., editors. Critical perspectives on racial and ethnic differences in health in late life. The National Academies Press; Washington, DC: 2004. pp. 145–170. [PubMed] [Google Scholar]
- Hicks L.S., Fairchild D.G., Cook E.F., Ayanian J.Z. Association of region of residence and immigrant status with hypertension, renal failure, cardiovascular disease, and stroke, among African-American participants in the third National Health and Nutrition Examination Survey (NHANES III) Ethnicity and Disease. 2003;13:316–323. [PubMed] [Google Scholar]
- Hinze S.W., Lin J., Andersson T.E. Can we capture the intersections? Older Black women, education, and health. Women's Health Issues. 2012;22(1):e91–e98. doi: 10.1016/j.whi.2011.08.002. [DOI] [PubMed] [Google Scholar]
- House J.S., Lantz P.M., Herd P. Continuity and change in the social stratification of aging and health over the life course: Evidence from a nationally representative longitudinal study from 1986 to 2001/2002 (Americans' Changing Lives Study) Journals of Gerontology: Series B. 2005;60B(special issue 2):15–26. doi: 10.1093/geronb/60.special_issue_2.s15. [DOI] [PubMed] [Google Scholar]
- House J.S., Lepkowski J.M., Kinney A.M., Mero R.P., Kessler R.C., Herzog A..R. The social stratification of aging and health. Journal of Health and Social Behavior. 1994;35(3):213–234. [PubMed] [Google Scholar]
- Hummer R., Rogers R.G., Amir S.H., Forbes D., Frisbie W.P. Adult mortality differentials among Hispanic subgroups and non-Hispanic whites. Social Science Quarterly. 2000;81(1):459–476. [PubMed] [Google Scholar]
- James S.A., Thomas P.E. John Henryism and blood pressure in Black populations: A review of the evidence. African American Research Perspectives. 2000;6(3):1–10. [Google Scholar]
- James S.A., Hoewyk J.V., Belli R.F., Strogatz D.S., Williams D.R., Raghunathan T.E. Life-course socioeconomic position and hypertension in African American men: The Pitt County Study. American Journal of Public Health. 2006;96(5):812–817. doi: 10.2105/AJPH.2005.076158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley-Moore J.A., Ferraro K.F. The Black/White disability gap: Persistent inequality in later life? Journal of Gerontology: Social Sciences. 2004;59B:S34–S43. doi: 10.1093/geronb/59.1.s34. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Ormel J., Demier O., Stang P.E. Comorbid mental disorders account for the role impairment of commonly occurring chronic physical disorders: Results from the National Comorbidity Study. Journal of Occupational and Environmental Medicine. 2003;45:1257–1266. doi: 10.1097/01.jom.0000100000.70011.bb. [DOI] [PubMed] [Google Scholar]
- King D.K. Multiple jeopardy, multiple consciousness: The context of Black Feminist ideology. Signs. 1988;14(1):42–72. [Google Scholar]
- Kuh D., Ben-Schlomo Y. Introduction. In: Kuh D., Ben-Schlomo Y., editors. A life course approach to chronic disease epidemiology. Oxford University Press; Oxford: 2004. pp. 3–14. [Google Scholar]
- Landry B. Pearson Prentice Hall; Upper Saddle River, NJ: 2007. Race, gender, and class: Theory and methods of analysis. [Google Scholar]
- Lynch S.M. Race, socioeconomic status, and health in life-course perspective. Research on Aging. 2008;30(2):127–136. [Google Scholar]
- Mair C.A. Social ties and depression: An intersectional examination of Black and White community-dwelling older adults. Journal of Applied Gerontology. 2010;29(6):667–696. [Google Scholar]
- Marin T.J., Chen E., Miller G.E. What do trajectories of childhood socioeconomic status tell us about markers of cardiovascular health in adolescence? Psychosomatic Medicine. 2008;70:152–159. doi: 10.1097/PSY.0b013e3181647d16. [DOI] [PubMed] [Google Scholar]
- McCall L. The complexity of intersectionality. Signs. 2005;30(3):1771–1800. [Google Scholar]
- McEwen B.S., Seeman T. Protective and damaging effects of mediators of stress: Elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Science. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- Merikangas K.R., Ames M., Cui L., Stang P.E., Ustun T.B., Von Korff M., Kessler R.C. The impact of comorbidity of mental and physical conditions on role disability in the U.S. adult household population. Archives of General Psychiatry. 2007;64(10):1180–1188. doi: 10.1001/archpsyc.64.10.1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minor D.S., Wofford M.R., Jones D.W. Racial and ethnic differences in hypertension. Current Ahterosclerosis Reports. 2008;10:121–127. doi: 10.1007/s11883-008-0018-y. [DOI] [PubMed] [Google Scholar]
- Mullings L. Resistance and resilience: The Sojourner Syndrome and the social context of reproduction in Central Harlem. In: Schulz A.J., Mullings L., editors. Gender, race, class, and health: Intersectional approaches. Jossey-Bass; San Francisco: 2006. pp. 345–370. [Google Scholar]
- Mullings L., Wali A. Kluwer Academic/Plenum Publishers; New York: 2001. Stress and resilience: The social context of reproduction in Harlem. [Google Scholar]
- Nguyen Q.C., Tabor J.W., Entzel P.P., Lau Y., Suchindran C., Hussey J.M., Halpern C.T., Harris K.M., Whitsel E.A. Discordance in national estimates of hypertension among young adults. Epidemiology. 2011;22(4):532–541. doi: 10.1097/EDE.0b013e31821c79d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Rand A., Hamil-Luker J. Processes of cumulative adversity: Childhood disadvantage and increased risk of heart attack across the life course [special issue] Journal of Gerontology: Social Sciences. 2005;60B:117–124. doi: 10.1093/geronb/60.special_issue_2.s117. [DOI] [PubMed] [Google Scholar]
- O'Rand A.M. The precious and the precocious: Understanding cumulative disadvantage and cumulative advantage over the life course. Gerontologist. 1996;36(2):230–238. doi: 10.1093/geront/36.2.230. [DOI] [PubMed] [Google Scholar]
- Ong K.L., Cheung B.M.Y., Man Y.B., Lau C.P., Lam K.S.L. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- Ore T.E. Constructing differences. In: Tracy E.O., editor. The social construction of difference and inequality: Race, class, gender, and sexuality. 2nd ed. McGraw Hill; Boston: 2003. pp. 11–17. [Google Scholar]
- Ostchega Y., Yoon S.S., Hughes J., Louis T. NCHS data brief. National Center for Health Statistics; Hyattsville, MD: 2008. Hypertension awareness, treatment, and control—Continued disparities in adults: United States, 2005–2006. [PubMed] [Google Scholar]
- Palloni A., Arias E. Paradox lost: Explaining the Hispanic adult mortality advantage. Demography. 2004;41(3):385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- Rabe-Hesketh S., Skrondal A. second edition. Stata Press; College Station, TX: 2008. Multilevel and longitudinal modeling using Stata. [Google Scholar]
- Raudenbush S.W., Bryck A.S. Sage; Thousand Oaks, CA: 2002. Hierarchical linear models: Applications and data analysis methods. [Google Scholar]
- Read J.G., Gorman B.K. Gender inequalities in U.S. adult health: The interplay of race and ethnicity. Social Science and Medicine. 2006;62:1045–1065. doi: 10.1016/j.socscimed.2005.07.009. [DOI] [PubMed] [Google Scholar]
- Rich-Edwards J.W., Buka S.L., Brennan R.T., Earls F. Diverging associations of maternal age with low birthweight for black and white mothers. International Journal of Epidemiology. 2003;32(1):83–90. doi: 10.1093/ije/dyg008. [DOI] [PubMed] [Google Scholar]
- Richardson L.J., Hussey J.M., Strutz K.L. Origins of disparities in cardiovascular disease: Birth weight, body mass index, and young adult systolic blood pressure in the National Longitudinal Study of Adolescent Health. Annals of Epidemiology. 2011;21:598–607. doi: 10.1016/j.annepidem.2011.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rieker P.P., Bird C.E., Lang M.E. Understanding gender and health: Old patterns, new trends, and future directions. In: Bird C.E., Conrad P., Fremont A.M., Timmermans S., editors. Handbook of medical sociology. 6th ed. Vanderbilt University Press; Nashville: 2010. pp. 52–74. [Google Scholar]
- Schulz A.J., Mullings L. Jossey-Bass; San Francisco: 2006. Gender, race, class, and health: Intersectional approaches. [Google Scholar]
- Shuey K.M., Willson A.E. Cumulative disadvantage and Black–White disparities in life-course health trajectories. Research on Aging. 2008;30(2):200–225. [Google Scholar]
- Spelman E.V. Beacon Press; Boston: 1988. Inessential woman. [Google Scholar]
- Spruill T.M. Chronic psychosocial stress and hypertension. Current Hypertension Reports. 2010;12:10–16. doi: 10.1007/s11906-009-0084-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor M.G. Timing, accumulation, and the Black/White disability gap in later life: A test of weathering. Research on Aging. 2008;30:226–250. [Google Scholar]
- Thoits P.A. Stress and health: Major findings and policy implications. Journal of Health and Social Behavior. 2010;51(S):S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Thomas A.J., Witherspoon K.M., Speight S.L. Gendered racism, psychological distress, and coping styles of African American women. Cultural Diversity and Ethnic Minority Psychology. 2008;14(4):307–314. doi: 10.1037/1099-9809.14.4.307. [DOI] [PubMed] [Google Scholar]
- Thomas P.A. Gender, social engagement, and limitations in late life. Social Science and Medicine. 2011;73:1428–1435. doi: 10.1016/j.socscimed.2011.07.035. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Labor & U.S. Bureau of Labor and Statistics (Eds.) (2011). Labor force characteristics by race and ethnicity, 2010. Washington, DC.
- Veenstra G. Race, gender, class, sexuality (RGCS) and hypertension. Social Science and Medicine. 2013;89:16–24. doi: 10.1016/j.socscimed.2013.04.014. [DOI] [PubMed] [Google Scholar]
- Wang Y., Wang Q.J. The prevalence of prehypertension and hypertension among U.S. adults according to the New Joint National Committee Guidelines: New challenges of the old problem. Archives of Internal Medicine. 2004;164:2126–2134. doi: 10.1001/archinte.164.19.2126. [DOI] [PubMed] [Google Scholar]
- Warner D.F., Brown T.H. Understanding how race/ethnicity and gender impact age-trajectories of disability: An intersectionality approach. Social Science and Medicine. 2011;72(8):1236–1248. doi: 10.1016/j.socscimed.2011.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber L., Fore M.E. Race, ethnicity, and health: An intersectional approach. In: Vera H., Feagin J.R., editors. Handbook of the sociology of racial and ethnic relations. Springer; New York, NY: 2007. pp. 191–218. [Google Scholar]
- Williams D.R. Black–White differences in blood pressure: the role of social factors. Ethnicity and Disease. 1992;2:126–141. [PubMed] [Google Scholar]
- Willson A.E., Shuey K.M., Elder G.E., Jr. Cumulative advantage processes as mechanisms of inequality in life course health. American Journal of Sociology. 2007;112(6):1886–1924. [Google Scholar]
- Wilmoth J., Koso G. Does marital history matter? Marital status and wealth outcomes among preretirement adults. Journal of Marriage and Family. 2002;64(1):254–268. [Google Scholar]
- Xu J., Kochanek K.D., Murphy S.L., Tejada-Vera B. Deaths: Final data for 2007. National Vital Statistics Reports. 2010;58(19) [PubMed] [Google Scholar]
- Yang Y., Lee L.C. Sex and race disparities in health: Cohort variations in life course patterns. Social Forces. 2009;87:2093–2124. [Google Scholar]
- Yao L., Robert S. The contributions of race, individual socioeconomic status, and neighborhood socioeconomic context on the self-rated health trajectories and mortality of older adults. Research on Aging. 2008;30(2):251–273. [Google Scholar]
- Zagorsky J.L. Marriage and divorce's impact on wealth. Journal of Sociology. 2005;41:406–424. [Google Scholar]
- Zambrana R.E., Dill B.T. Disparities in Latina health: An intersectional analysis. In: Schulz A.J., Mullings L., editors. (pp. 192–227. Jossey-Bass; San Francisco: 2006. (Gender, race, class, & health: Intersectional approaches). [Google Scholar]