Abstract
T cell avidity is critical to viral clearance, but mechanisms of CD8+ T cell avidity maturation are poorly understood. Here, we find that IL-15 mediates two mechanisms of avidity maturation. (i) By selection at the population level, IL-15 promotes greater survival of high- compared with low-avidity cytotoxic T lymphocytes (CTLs). High-avidity CTLs express higher levels of IL-15Rα and persist longer by homeostatic proliferation. (ii) At the individual cell level, IL-15 induces higher levels of surface coreceptor CD8αβ, increasing functional avidity. IL-15 during priming selects or induces higher-avidity CTLs. Conversely, high-avidity CTLs are diminished in IL-15Rα knockout mice. These results provide an explanation of CD8+ T cell avidity maturation and may contribute to the design of novel vaccines.
Cytotoxic T lymphocyte (CTL) avidity is a critical factor in clearing virus infections and in killing tumor cells (1-5). In contrast to the maturation of antibody affinity, dependent on somatic mutation, avidity maturation of T cells has long been an enigma. Antigen-specific CD8+ T cells undergo avidity maturation during viral infections, but T cell receptors (TCRs) do not undergo somatic mutation. Some selection of T cell repertoire by competition for antigens must play a role. However, T cells may compete for factors other than antigens.
Both in vivo and in vitro, high-avidity CD8+ CTLs could be selectively expanded in response to limited levels of antigens (1, 6, 7). We previously showed that increased costimulatory signals resulted in the selective induction of high-avidity CD8+ CTLs (8), consistent with a dependence of functional avidity of CD8+ CTLs on the signal transduction machinery (6). Moreover, boosting resulted in a higher proportion of high-avidity CD8+ CTLs (7-9). Thus, signals through both the TCR and costimulatory molecules contribute to CTL avidity.
IL-15 is a key cytokine for homeostatic proliferation and maintenance of memory CD8+ T cells (10-12) and has been used as a vaccine adjuvant to enhance CTL responses (13, 14). Recently, in examining the ability of IL-15 expressed by a vaccine vector to influence the response induced, we found that the presence of IL-15 during the immune induction phase resulted in long-lasting CD8+ memory T cells, due to increased expression of IL-15Rα (14). Thus, the quality of CD8+ T cells, not only for expansion and differentiation but also for longevity, is determined when T cells first encounter antigen (14), consistent with other recent studies (15-17). We have now asked whether IL-15-dependent survival might influence T cell avidity maturation.
Here, we have identified two mechanisms for CD8+ CTL avidity maturation. (i) Selection by competition for IL-15 results in greater homeostatic proliferation and persistence of high-avidity CD8+ CTLs, which are more responsive to endogenous IL-15 because they express higher levels of IL-15Rα. Thus, the population average avidity is increased over time. (ii) Instructionally, at the individual cell level, IL-15 up-regulates the CD8 coreceptor, resulting in enhanced functional avidity. In addition to providing a mechanism to explain the enigma of CTL avidity maturation, the finding that the quality of CD8+ CTLs is determined in the induction phase of the immune response, and is strongly influenced by IL-15, may contribute to the design of novel vaccines.
Materials and Methods
Viruses, Animals, and Immunization. Recombinant vaccinia viruses vPE16 and vPE16/IL-15 were described (14, 18). Vaccinia virus expressing ovalbumin was provided by J. Yewdell (National Institute of Allergy and Infectious Diseases, National Institutes of Health). Female ΒΑLΒ/c mice (Animal Production Colonies, Frederick Cancer Research Facility, National Institutes of Health, Frederick, MD) were used at 6-8 weeks of age. Both IL-15Rα (-/-) and control mice (The Jackson Laboratory) were used at 6-10 weeks of age. Animal procedures were carried out under institutionally approved protocols. Mice were immunized s.c. in the tail base with 2-4 × 106 plaque-forming units of the recombinant vaccinia viruses and boosted after 3 weeks where indicated.
Antibodies, Tetramer, and Flow Cytometry. Fluorescent or biotin-labeled anti-mouse CD3 (17A2), CD8α (53-6.7), CD8β (53.5.8), CD44 (IM-7), CD62L (MEL-14), CD69 (H1.2F3), CD25 (IL-2Rα), CD122 (IL-2Rβ), CD127 (IL-7Rα), TCRβ (H57-597), anti-Bcl-2, annexin V, anti-goat IgG, and all control antibodies were purchased from Pharmingen. Goat anti-human IL15Rα was from R & D Systems, and specificity for mouse IL-15Rα was confirmed by using IL-15Rα (-/-) mice (The Jackson Laboratory) as a negative control (Fig. 6, which is published as supporting information on the PNAS web site). H-2Dd-P18-I10 tetramer was provided by the National Institutes of Health Tetramer Core Facility (Atlanta). H-2Kb-SIINFEKL tetramer was purchased from Beckman Coulter. Cells stained with appropriate antibodies were analyzed on a FACSCalibur (Becton Dickinson). Background staining was assessed by using an isotype control antibody (Pharmingen). For tetramer staining of the cells, anti-CD8 and tetramer were first diluted (2-3 μl of anti-CD8 and 1 μl of tetramer in 200 μl) in the fluorescence-activated cell sorter buffer and added into the tubes containing 106 cells. Cells were incubated for 30 min on ice before washing. An Epics Elite ESP sorter (Beckman Coulter) was used for preparative sorting of CD8 and tetramer-positive T cells. For intracellular IFN-γ staining, cells were stained following the manufacturer's protocol (Pharmingen).
Peptides, Media, Cells, and Lines. P18-I10 (RGPGRAFVTI) and ovalbumin epitope (SIINFEKL) peptides were commercially synthesized (Multiple Peptide Systems, San Diego). P815 cells were maintained in RPMI medium 1640 complete medium supplemented with 10% FCS/2 mM L-glutamine/100 units/ml penicillin/100 μg/ml streptomycin/5 × 10-5 M 2-mercaptoethanol. P18-I10-specific CD8+ CTL lines were established by continuous in vitro restimulation with peptide-pulsed splenocytes and characterized by P18-I10-H-2Dd tetramer staining and lytic activity over a range of peptide concentrations.
Proliferation and CTL Assays. For the proliferation assay in Fig. 1a, the positively purified (Miltenyi Biotec, Auburn, CA) spleen CD8+ T cells were stimulated with peptide-pulsed splenocytes, and [3H]thymidine uptake was measured as described (8). The proliferation of preparatively sorted cells (Fig. 2b) was also measured similarly. For an in vivo proliferation assay (Fig. 2d), carboxy fluorescein (diacetate) succinimidyl ester (CFSE)-labeled CD8+ T cells (1 × 107 cells per mouse) were transferred to naïve recipients i.v. Antigen-specific lytic activity of CD8+ CTLs from the immunized animals was measured by a 5-h 51Cr release assay as described (8).
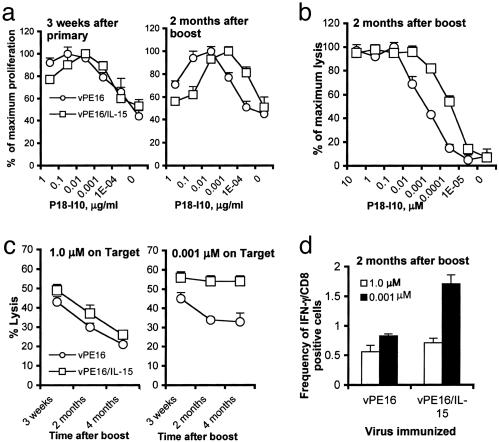
Fig. 1.
IL-15 during priming results in the long-lasting high-avidity CD8+ CTLs. (a) Spleen cells from three to four mice in each group were pooled, CD8+ T cells were positively purified and stimulated with splenocytes loaded with different concentrations of P18-I10, and proliferation was measured as described in Materials and Methods. Data are representative of three repeated experiments with consistent results. Each data point indicates mean ± SEM of triplicate assay. (b and c) Spleen CD8+ T cells from three to four mice in each group were pooled and stimulated with 1.0 (c Left) or 0.001 μM(b and c Right) P18-I10-pulsed splenocytes for 1 week. Lytic activity of CD8+ CTLs against P815 cells pulsed with different concentrations of the peptide was measured. Data represent mean ± SEM of triplicate assay at an effector-to-target cell ratio of 20:1. Similar kinetics of response were observed at all effector-to-target cell ratios tested, 80:1, 40:1, 20:1, and 10:1 (data not shown) in three repeat experiments. Data presented in b were normalized to the maximum lysis to compare avidity independent of magnitude of lysis and show mean ± SEM of triplicate assays. (d) Spleen CD8+ T cells from mice immunized as indicated were restimulated with 1.0 or 0.001 μM soluble P18-I10 overnight in the presence of brefeldin A. Cells were stained for intracellular IFN-γ by the manufacturer's protocol.
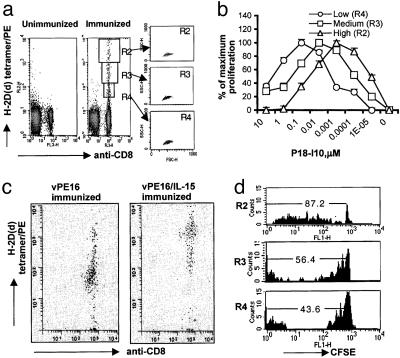
Fig. 2.
In vivo proliferation and persistence of antigen-specific CD8+ T cells depend on CD8+ T cell avidity. (a) Two to 3 months after boosting, splenocytes were stained with anti-CD8 and P18-I10 tetramer concurrently, as described in Materials and Methods. Cells at Left were from unimmunized animals. The three graphs at Right show the distribution of cells from gate R2, R3, and R4 in forward and side scatter plots. (b) Cells were gated, based on the brightness of tetramer staining, and sorted, left in the media for 6 h, and stimulated with P18-I10-pulsed splenocytes. Proliferation was measured as in Fig. 1. (c) Four months after boosting, spleen CD8+ T cells from mice immunized with vPE16 (Left) or vPE16/IL-15 (Right) were stained with anti-CD8 and P18-I10 tetramer, and then double-positive cells were sorted and reanalyzed by flow cytometry. (d) Two to 3 months after the boost, spleen CD8+ T cells from the immunized mice were labeled with CFSE and transferred to naïve animals. Four to 5 weeks after the transfer, spleen cells in the recipients were stained with anti-CD8 and tetramer, gated as in a, and analyzed to measure homeostatic proliferation. The numbers in histograms are mean ± SEM of at least four individual recipients in each experiment. Three repeated experiments showed consistent results.
Cytokine ELISA. T cell lines, 5 × 104 cells per well, were stimulated with 1 × 105 cells per well of irradiated (3,000 rads; 1 rad = 0.01 Gy) syngeneic splenocytes pulsed with different concentrations of P18-I10 in a 96-well flat-bottomed microtiter plate (Costar). On day 2, culture supernatants were analyzed for IFN-γ by ELISA by using Dynatech Immunolon I plates (Dynatech, Chantilly, VA) and antibodies purchased from Pharmingen.
Results
In Vivo Priming with IL-15 Results in Long-Lasting High-Avidity CD8+ CTLs. Priming CD8+ T cells results in a broad range of avidities of antigen-specific CD8+ CTLs (1), and these cells undergo further avidity maturation over time (6). We now examined whether IL-15 contributes to the avidity maturation of antigen-specific CD8+ CTLs.
Animals were immunized with either vPE16, a recombinant vaccinia virus expressing HIV-1 IIIB gp160 (18), or vPE16/IL-15. The avidity of CD8+ CTLs specific for the dominant epitope P18-I10 was determined from the responsiveness of CD8+ CTLs to different concentrations of P18-I10-pulsed splenocytes ex vivo, as described (8, 19). Data in Fig. 1a were normalized to maximal response to show the shift in dose response independent of the absolute magnitude of response. CD8+ T cells in the two groups of animals had a similar avidity at 3 weeks. However, the average avidity of CD8+ T cells in the two groups increased over time, and CD8+ T cells induced with IL-15 showed increased proliferation at low doses of peptide (an ≈10-fold shift in peptide concentration) after 2 months (Fig. 1a). We confirmed this difference by a different method, by using CFSE dilution in immune spleen cells ex vivo as an indicator of cell division (Fig. 7, which is published as supporting information on the PNAS web site). Consistent with Fig. 1a, the lytic dose response of bulk CD8+ CTLs from mice immunized with vPE16/IL-15 was shifted 10-fold from that of mice immunized with vPE16 alone (Fig. 1b), showing higher avidity by an independent method.
To examine the kinetics of high- and low-avidity CD8+ CTLs by measuring their lytic activity against target cells presenting different densities of peptide, CD8+ T cells from the two groups were restimulated once with either a high (1.0 μM) or low (0.001 μM) concentration of peptide. The frequency of low-avidity CD8+ CTLs in both groups of animals decreased over time, as did the high-avidity CTLs in mice immunized without IL-15 (Fig. 1c). However, high-avidity CD8+ CTLs from mice immunized with vPE16/IL-15 were quite stable over 4 months, resulting in a higher proportion of high-avidity T cells at later times as measured by lytic activity, confirming the differences seen by proliferation. To confirm the ex vivo data in Fig. 1a by yet a third measure of functional activity, the frequency of peptide-specific CD8+ CTLs was measured by intracellular IFN-γ staining (Fig. 1d). At 2 months after the boost, the ratio of specific CD8+ CTLs of high avidity (responding to 0.001 μM peptide) vs. low avidity (responding to 1.0 μM) was higher in the group immunized with the IL-15-expressing vector. Thus, by several independent measures, expression of IL-15 by the vaccine vector led to avidity maturation over months, with better preservation of high-avidity CTLs at later time points, even though the vector expressing IL-15 and antigen is cleared within 10 days.
CD8+ CTLs Undergo Avidity Maturation in the Absence of Antigen. To study ex vivo why the low-avidity CD8+ CTLs disappeared earlier than high-avidity CD8+ CTLs, we stained bulk spleen cells from immunized mice directly ex vivo with P18-I10 tetramer and anti-CD8 concurrently, and we then stratified gated double-positive cells based on the brightness of tetramer staining (Fig. 2a). With some exceptions and caveats (20, 21, 37), the magnitude of tetramer binding was correlated with the avidity of CD8+ CTLs in our own unpublished and other published studies (4, 22). To get enhanced resolution of avidity, we stained cells with a concurrent staining method based on the fact that the interaction between CD8 molecules and the α3 domains of tetramer alters the binding affinity of the class I MHC tetramer to the TCR (23-26). This tetramer stains very brightly, and competition with anti-CD8 broadens the spread of tetramer fluorescence intensity. Similar spreads in tetramer brightness have been observed (4). Scattergrams in Fig. 2a show that the size and autofluorescence of the cells in different gates are similar, so the brightness difference is not just a difference in cell size. Also, differences in tetramer staining were not simply due to differences in TCRαβ levels, which did not differ between high- and low-avidity CD8+ CTLs (see Fig. 4a below). Tetramer staining was specific because it could not be detected on cells from unimmunized mice (Fig. 2a). To confirm that the brightness of tetramer staining correlates with T cell avidity, we preparatively sorted cells based on the tetramer brightness and examined the proliferative response over a range of peptide concentrations (Fig. 2b) and the functional lytic activity against target cells pulsed with a low concentration of peptide (Fig. 8, which is published as supporting information on the PNAS web site). The brightest tetramer-staining population clearly responded by proliferation at a 100-fold lower concentration than the least bright population, whereas those with intermediate staining were intermediate (Fig. 2b). They also showed higher lytic activity on targets expressing low levels of antigen as a measure of high-avidity CTLs (Fig. 8). Thus, by multiple criteria, the distribution of tetramer staining faithfully reflects differences in functional CTL avidity, not cell size or TCR density.
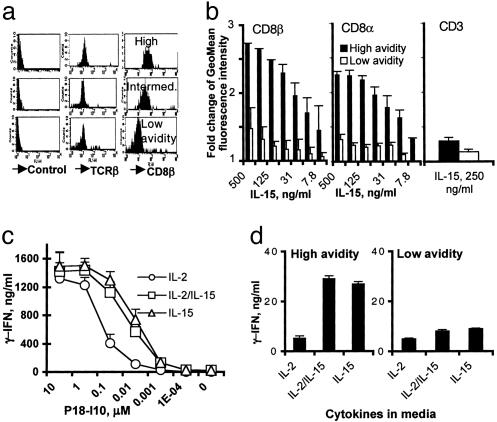
Fig. 4.
High-avidity CD8+ CTLs express higher levels of CD8αβ and IL-15 up-regulates the expression level of CD8αβ, resulting in enhanced functional activity. (a) Cells from the immunized mice were stained with anti-CD8 and P18-I10 tetramer, gated on the brightness of tetramer staining as in Fig. 2, and assessed for CD8β and TCRβ levels. (Top, Middle, and Bottom) High-, intermediate-, and low-avidity gates, respectively. Data are representative of three experiments with consistent results. (b) High- and low-avidity CD8+ CTL lines were incubated in media containing different concentrations of IL-15, and the expression levels of CD8β (Left) and CD8α (Center) were measured at 36 h of incubation. As a control, the levels of CD3 in both high- and low-avidity CTL lines were also measured (Right) when lines were incubated in the media containing 250 ng/ml IL-15. Data are mean ± SEM of three experiments. The fold increase of geometric mean fluorescence intensity (MFI) was calculated by (MFI with IL-15)/(MFI without IL-15). (c) The high-avidity CTL line, grown with 0.001 μM peptide, was stimulated with splenocytes pulsed with different concentrations of P18-I10 in the presence of IL-2 50 units/ml, IL-15 20 ng/ml, or both for 36 h, and the amount of IFN-γ produced was measured by ELISA. (d) The high- and low-avidity CD8+ T cell lines were depleted of presenting cells by positive selection with anti-CD8 beads and cultured without antigen or other cells in the presence of IL-2 50 units/ml, IL-15 20 ng/ml, or both for 36 h, and the amount of IFN-γ produced was measured by ELISA.
The results of concurrent staining of CD8+ CTL from the animals immunized with vPE16 or vPE16/IL-15 are compared in Fig. 2c. The observed difference in average population tetramer brightness again confirms by yet a fourth criterion, in addition to the functional assays in Fig. 1, that immunization with vPE16/IL-15 results in higher-avidity CTLs.
To assess homeostatic proliferation, 2-3 months after the boost, purified CD8+ T cells from the animals immunized with vPE16 were labeled with CFSE and adoptively transferred into naïve animals. Four weeks later, homeostatic proliferation of P18-I10-specific CD8+ CTLs was measured based on the CFSE intensity, gating on CD8+ tetramer+ cells in different gates of tetramer fluorescence intensity as an estimate of avidity. High-avidity CD8+ CTLs (R2 gate) proliferated more than lower-avidity CTLs (R3 and R4 gates; Fig. 2d), suggesting that homeostatic proliferation parallels avidity, even in the absence of antigen. Although the cells in the R4 gate proliferated nearly as well as the cells in the R3 gate, almost 65% of the cells in the R4 gate were positive for annexin V staining, suggesting that these are more fragile for handling and probably in the early stage of apoptosis (data not shown). Cells with low CFSE at left in the R3 and R4 gates in Fig. 2d are likely to be apoptotic. Consistently, more brightly tetramer-staining cells expressed higher levels of antiapoptotic protein, Bcl-2 (data not shown). Thus, the gradual shift in population avidity seen in Fig. 1 could be explained by both increased rates of homeostatic proliferation and greater survival.
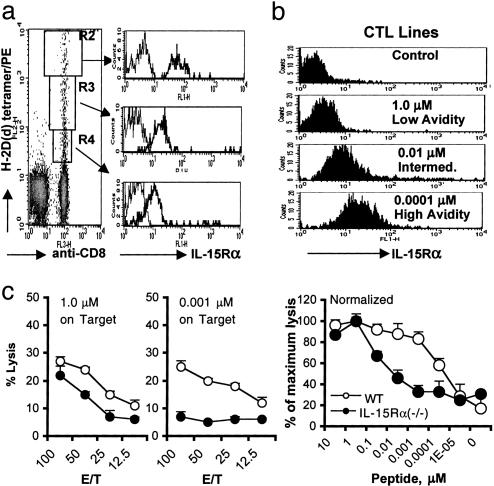
CD8+ CTL Avidity Maturation and Homeostasis of Memory CD8+ T Cells Depend on the Levels of IL-15Rα. Maintenance of antigen-specific memory CD8+ T cells requires IL-15 (12, 27). To explore the mechanism by which high-avidity CD8+ CTLs persist longer than low-avidity CTLs in vivo, we first examined IL-15 receptor levels. Bulk high-avidity CD8+ CTLs studied directly ex vivo among spleen cells of immunized mice expressed higher levels of IL-15Rα, in parallel with relative avidity (Fig. 3a). In contrast, however, no differences in levels of IL-7Rα and IL-2Rβ were detectable among the cells from the different gates although CD8+ CTL in all three gates expressed both IL-7Rα and IL-2Rβ (data not shown). Similar observations were made on CD8+ CTL lines selected by growth on different concentrations of peptide and showing different degrees of tetramer staining (a >4-fold range of tetramer staining intensity, data not shown). Rested high-avidity CD8+ CTL lines (grown with lower peptide concentration) constitutively expressed higher levels of IL-15Rα than the low-avidity CD8+ CTLs (Fig. 3b). Similar higher levels of IL-15Rα were confirmed independently with a different antibody, goat anti-mouse IL-15Rα from R & D Systems (data not shown). All CTL lines expressed similar levels of IL-7Rα, suggesting that IL-7/IL-7Rα may not contribute to the avidity maturation of CD8+ CTLs, in contrast to its role in their memory (ref. 28 and data not shown). The homeostatic proliferation of high-avidity CD8+ CTL lines in response to 20 ng/ml IL-15 is shown in Fig. 9, which is published as supporting information on the PNAS web site. Thus, the functional response to IL-15 confirms the difference based on staining for IL-15Rα, supporting the conclusion that high-avidity CTLs express higher levels of IL-15Rα, allowing the enhanced homeostatic proliferation by more efficiently capturing low levels of endogenous IL-15 in naïve animals.
Fig. 3.
High-avidity CD8+ CTLs express higher levels of IL-15Rα, resulting in long-lasting memory CTLs. (a) Cells from the pooled spleens of three to four mice immunized with vPE16/IL-15 were stained with anti-CD8 and P18-I10 tetramer. IL-15Rα expression levels were measured for CD8+ T cells gated by the brightness of tetramer staining. Thin lines represent isotype control antibody. Three repeated experiments showed consistent data. (b) CD8+ T cell lines were raised by in vitro stimulation with different concentrations of P18-I10 in the media containing 50 units/ml IL-2. Cells grown in 0.0001, 0.01, and 1.0 μM peptide are designated as high-, intermediate-, and low-avidity CTL lines, respectively. The levels of IL-15Rα in CTL lines were measured 6-8 days after restimulation. Four repeated experiments showed consistent data. Data in Fig. 9 indicate that a high-avidity CTL line shows enhanced proliferative responsiveness to IL-15. (c) On day 17 after the immunization with vaccinia expressing ovalbumin, CD8+ T cells from the pooled spleens of three mice per group [B6 or IL-15Rα (-/-)] were restimulated with 1.0 or 0.001 μM of the dominant epitope SIINFEKL peptide for 1 week. (Left) Functional activity of CD8+ CTLs against target cells pulsed with 1.0 or 0.001 μM of the peptide was measured by 5h 51Cr-release assay. (Right) CD8+ T cells were stimulated with 0.01 μM peptide, and lytic activities against target cells pulsed with different concentrations of peptide were measured. Data presented at Right were normalized to the maximum lysis to compare avidity independent of magnitude of lysis and show mean ± SEM of triplicate assays. Data were consistent in two repeat experiments. E/T, effector-to-target cell ratio.
The prediction from these results is that mice lacking IL-15Rα should have a relative deficit in high-avidity CTLs. To test this hypothesis, we compared the avidity of bulk splenic CTLs with the immunodominant ovalbumin epitope in wild-type C57BL/6 mice and IL-15Rα (-/-) mice on the same background (Fig. 3c). IL-15Rα (-/-) animals did not maintain high-avidity CD8+ CTLs compared with wild-type mice, whereas activity of low-avidity CTLs was similar. Thus, the prediction was confirmed that IL-15Rα-deficient mice have a relatively greater deficit in high-avidity CTLs, and the conclusions were verified in an independent system.
CD8+ CTL Avidity Is Determined by a Coreceptor Regulated by IL-15. We sought a molecular mechanism to explain the association of higher levels of IL-15Rα with higher functional avidity for antigen.
The CD8 molecule plays a role as a coreceptor for the ligation of the TCR and MHC/peptide complex. The cytoplasmic domain of CD8β constitutively associates with the TCR, resulting in high affinity for MHC/peptide complexes (29). Both CD8αα and CD8αβ can bind Lck, but only CD8αβ can be localized into lipid rafts (30, 31). Expression of CD8β has been shown to contribute to functional CTL avidity (31). Therefore, we examined the levels of CDαβ on bulk high- and low-avidity CD8+ CTLs ex vivo from immunized mice gated by the concurrent staining method used in Fig. 2a, and found that high-avidity CD8+ T cells express significantly higher levels of CD8αβ (Fig. 4a). The brighter tetramer-staining cells in the bulk spleen population ex vivo showed at least an 8- to 10-fold higher level of CD8β expression than the less bright tetramer-staining cells (Fig. 4a). However, no difference was seen in TCRβ levels (Fig. 4a Middle), indicating that the differences in avidity were not due to TCR levels, and that the brighter CD8β staining was not due to a difference in cell size that would affect all surface molecules. Thus, high-avidity bulk CTLs studied ex vivo from spleens of immunized mice express higher levels of CD8.
To address the molecular connection between high IL-15Rα levels and high avidity, we hypothesized that signaling through the IL-15R complex might induce greater CD8β expression in high-avidity CD8+ CTLs, accounting for the higher functional avidity. This hypothesis was tested in vitro by measuring the effect of IL-15 on the expression levels of CD8α and CD8β. The levels of CD8β in high-avidity CTLs were remarkably increased by the increasing doses of IL-15, and the maximum level of CD8β was almost 2.7-fold higher than that of the same high-avidity CTL line without IL-15 (Fig. 4b). Thus, even a high-avidity CTL line, which already has higher levels of CD8β expression, can be induced to express even higher levels of CD8β when stimulated with IL-15. The levels of CD8α were also increased by IL-15, but the magnitude of the increase (2.2-fold) was slightly lower than that of CD8β. This finding suggests that treatment of high-avidity CTLs with IL-15 could increase not only the total level of CD8 coreceptor but also the ratio of CD8β to CD8α, and therefore the proportion of CD8 molecules existing as CD8αβ heterodimers, which were previously reported to contribute to enhanced functional activity of high-avidity CD8+ CTLs (29-31). These dramatic changes in CD8α and CD8β levels were not observed in low-avidity CTLs. Because only small differences were seen in CD3 staining (Fig. 4b), and no difference in cell size was detected in forward/side scattergram (data not shown), the results were not simply due to blastogenesis induced by IL-15. We have found that P18-I10-specific CD8+ CTLs induced with vPE16/IL-15 expressed higher levels of CD8αβ than CTLs induced with vPE16 alone (Fig. 10, which is published as supporting information on the PNAS web site). Thus, IL-15 during immunization induces higher-avidity CTLs (Fig. 1) expressing higher levels of CD8 coreceptor (Fig. 4a). Taken together, these results support our working hypothesis that CD8+ CTLs expressing higher levels of IL-15Rα display higher functional avidity in part by an unexpected mechanism involving IL-15-mediated up-regulation of CD8αβ, which is one determinant of functional avidity.
To investigate whether up-regulation of CD8αβ coreceptor by IL-15 affected the functional avidity of CD8+ CTLs, we examined the effect of IL-15 on IFN-γ production by high-avidity CD8+ CTLs as a function of antigen concentration. Indeed, IL-15 during antigen stimulation significantly enhanced the functional activity of high-avidity CD8+ CTLs (Fig. 4c), but not low-avidity CTLs (data not shown), by increasing the sensitivity to antigen 10-fold. Maximal response was not changed substantially, only sensitivity to peptide. Thus, even a high-avidity CTL line can be further induced to display even higher functional avidity by treatment with IL-15.
Moreover, purified high- but not low-avidity CD8+ CTLs reproducibly produced low levels of IFN-γ when stimulated only with IL-15 without presenting cells (Fig. 4d), which was consistent with greater IL-15Rα expression. CTL lines were rested in media without cytokine for 3 days, purified by positive selection with anti-CD8, and stimulated by IL-15 in the absence of antigen-presenting cells. The results are consistent with the ability of IL-15Rα on the T cells themselves to present in cis and augment the T cell's responsiveness to IL-15, in addition to the known ability of IL-15Rα on antigen-presenting cells to present IL-15 to T cells in trans (32).
Discussion
We propose that the affinity maturation of antigen-specific CD8+ T cells occurs in two different ways: competition for antigen and for IL-15. Antigen-competition affinity maturation involves selective induction and expansion of high-avidity CD8+ T cells by primary and secondary antigenic stimulation. In the primary response, CD8+ T cells undergo functional avidity maturation during acute lymphocytic choriomeningitis virus infection (6), and increased costimulatory signals selectively induced high-avidity CD8+ CTLs (8). For the secondary immune response, the use of α- and β-chain TCRs was narrowed by boosting (33, 34), and narrowing of the TCR repertoire was due to the loss of T cells expressing low affinity for tetramer (9). More recently, CD8+ T cell affinity maturation by antigenic stimulation has been demonstrated by showing that high-avidity CD8+ CTLs competed more efficiently for antigen than low-avidity CTLs during the secondary response (7, 35, 36).
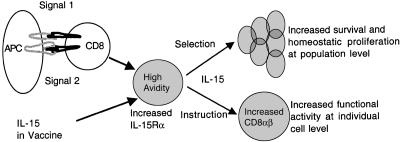
Besides such expected competition for antigen, we have now defined two mechanisms of CTL avidity maturation, both dependent on IL-15, one instructive at the individual cell level, and another selective at the population level (Fig. 5). The former builds on the findings that CD8+ T cell functional avidity did not depend solely on TCR affinity, but also relied on optimization of the CD8+ T cell signal transduction (6, 31, 37, 38). The role of CD8β in increasing the efficiency of coreceptor function of CD8 molecules has been well described (29, 30, 39-42). CD8β substantially increased the avidity of TCR ligand binding (29), and high-avidity CTL lines expressed higher levels of CD8β (38). Indeed, functional avidity of CD8+ T cells with the same TCR is influenced by the levels of CD8β and its colocalization with the TCR in lipid rafts (31). Also, the cytoplasmic domain of CD8β could activate CD8α-mediated Lck activity (43, 44), which was correlated with functional avidity (6). Therefore, it has been concluded that the levels of CD8αβ on T cells can influence the avidity of CD8+ T cells. Thus, as a possible molecular mechanism, for the association between CTL avidity and IL-15Rα and CD8β expression, we asked whether IL-15 might up-regulate CD8β expression, accounting for the increased functional avidity. Indeed, we found that high-avidity CD8+ CTLs expressed remarkably high levels of CD8β ex vivo, and unexpectedly, that the level of CD8β was greatly enhanced by IL-15. This IL-15-mediated CD8β expression was not observed in low-avidity CD8+ CTLs expressing low levels of IL-15Rα. The functional effect is independently confirmed by the observation that high-avidity CTLs can be induced to display even higher functional avidity by culturing in IL-15 (Fig. 4c). Therefore, we now propose that IL-15 selects CD8+ CTLs expressing relatively high levels of IL-15Rα during the priming. It is possible that a stronger signal in high-avidity T cells also up-regulates IL-15Rα. Furthermore, we propose that such CTLs expressing higher levels of IL-15Rα are more sensitive to IL-15 and therefore maintain higher levels of CD8αβ, accounting for the higher functional avidity and perpetuation of the cycle of avidity maturation (Fig. 5).
Fig. 5.
Proposed mechanism by which IL-15 mediates antigen-independent avidity maturation of CD8+ T cells by both instruction at the individual cell level and selection at the population level. High-avidity CTLs are induced to express high levels of IL-15Rα, either by a strong signal through the TCR and costimulatory receptors (signals 1 and 2, respectively) or by selection or induction by IL-15 during priming (IL-15 in a vaccine or produced by dendritic cells). These high-avidity CTLs are thus more sensitive to low endogenous levels of IL-15, which then promotes preferential survival and homeostatic proliferation of the high-avidity CTLs, resulting in selection of a higher average avidity at the population level, or induces up-regulation of CD8αβ coreceptor, resulting in increased functional avidity at the individual cell level.
We also find that IL-15 can mediate CTL avidity maturation by a selective mechanism at the population level (Fig. 5), by selective maintenance of homeostatic proliferation. We now see that avidity maturation is primarily dependent on the levels of IL-15Rα on CD8+ T cells, suggesting competition for low endogenous levels of IL-15. The ability of high-avidity CD8+ CTLs to continuously divide in response to the limited amount of IL-15 in the immunologically quiescent host (Fig. 2d) and the increased expression of antiapoptotic protein, Bcl-2, may further contribute to the persistence of high-avidity CD8+ CTLs. Our data showing a decreased proportion of high-avidity CTLs in IL-15Rα (-/-) mice provide independent support for the critical role of IL-15 and IL-15Rα for the selective maintenance of high-avidity CD8+ CTLs. Although Dubois et al. (32) showed that IL-15Rα on an antigen-presenting cell could present IL-15 in trans to a T cell expressing only IL-15/IL-2Rβ and -γ, it is nevertheless plausible that IL-15Rα on T cells could act in cis to increase sensitivity to low levels of IL-15, giving those T cells expressing high IL-15Rα a survival advantage for greater homeostatic proliferation in response to limited IL-15 in the immune quiescent host. Indeed, data in Fig. 4d showing greater response to IL-15 of purified CD8+ high-avidity T cells expressing more IL-15Rα in the relative absence of antigen-presenting cells are consistent with this hypothesis. On the other hand, low-avidity CTL expressing low levels of IL-15Rα may be poor competitors for endogenous IL-15 and die off over time. Thus, the average avidity of the population would increase over time, accounting for avidity maturation. The idea that competition for cytokines could select for CTLs with higher functional avidity for antigen is unexpected.
Moreover, subsequent long-term antigen-independent avidity maturation was determined in the induction phase of the immune response, because priming in the presence of IL-15 selected for or induced higher-avidity CD8+ CTLs expressing higher levels of IL-15Rα. These CTLs induced by a vaccine expressing IL-15 showed greater functional avidity by three independent criteria, proliferation, lytic activity, and IFN-γ production (Fig. 1), as well as greater tetramer staining (Fig. 2c) and greater CD8 expression (Fig. 4 a and b). Because high-avidity CTLs are more effective at clearing virus infections and killing tumor cells (1-5), use of IL-15 in vaccines could result in a quantitatively and qualitatively improved CTL response.
In conclusion, the levels of IL-15Rα on CD8+ CTL and availability of IL-15 in vivo are critical factors for avidity maturation. High-avidity CD8+ CTLs express higher levels of IL-15Rα, and this expression results in the long-term maintenance of high- but not low-avidity CD8+ CTLs, accounting for maturation of average avidity of the population over time. Moreover, IL-15 increased the expression of CD8αβ, resulting in enhanced functional activity at the individual cell level, and this instructive mechanism was seen only in cells expressing higher IL-15Rα. Our data provide an explanation for the long-standing phenomenon of T cell avidity maturation and should contribute to the development of new vaccine strategies against viral infections and cancers.
Supplementary Material
Acknowledgments
We thank Dr. Alfred Singer for critical reading of the manuscript and very helpful suggestions; Drs. Peter C. Doherty, Ronald N. Germain, and Dennis Klinman for helpful discussion; and Karren Wolcott for assistance with preparative sorting of T cells.
Abbreviations: CTL, cytotoxic T lymphocyte; TCR, T cell receptor; CFSE, carboxy fluorescein (diacetate) succinimidyl ester.
References
- 1.Alexander-Miller, M. A., Leggatt, G. R. & Berzofsky, J. A. (1996) Proc. Natl. Acad. Sci. USA 93, 4102-4107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gallimore, A., Dumrese, T., Hengartner, H., Zinkernagel, R. M. & Rammensee, H. G. (1998) J. Exp. Med. 187, 1647-1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Derby, M. A., Alexander-Miller, M. A., Tse, R. & Berzofsky, J. A. (2001) J. Immunol. 166, 1690-1697. [DOI] [PubMed] [Google Scholar]
- 4.Yee, C., Savage, P. A., Lee, P. P., Davis, M. M. & Greenberg, P. D. (1999) J. Immunol. 162, 2227-2234. [PubMed] [Google Scholar]
- 5.Zeh, H. J., III, Perry-Lalley, D., Dudley, M. E., Rosenberg, S. A. & Yang, J. C. (1999) J. Immunol. 162, 989-994. [PubMed] [Google Scholar]
- 6.Slifka, M. K. & Whitton, J. L. (2001) Nat. Immunol. 2, 711-717. [DOI] [PubMed] [Google Scholar]
- 7.Busch, D. H. & Pamer, E. G. (1999) J. Exp. Med. 189, 701-710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oh, S., Hodge, J. W., Ahlers, J. D., Burke, D. S., Schlom, J. & Berzofsky, J. A. (2003) J. Immunol. 170, 2523-2530. [DOI] [PubMed] [Google Scholar]
- 9.Savage, P. A., Boniface, J. J. & Davis, M. M. (1999) Immunity 10, 485-492. [DOI] [PubMed] [Google Scholar]
- 10.Zhang, X., Sun, S., Hwang, I., Tough, D. F. & Sprent, J. (1998) Immunity 8, 591-599. [DOI] [PubMed] [Google Scholar]
- 11.Ku, C. C., Murakami, M., Sakamoto, A., Kappler, J. & Marrack, P. (2000) Science 288, 675-678. [DOI] [PubMed] [Google Scholar]
- 12.Becker, T. C., Wherry, E. J., Boone, D., Murali-Krishna, K., Antia, R., Ma, A. & Ahmed, R. (2002) J. Exp. Med. 195, 1541-1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim, J. J., Trivedi, N. N., Nottingham, L. K., Morrison, L., Tsai, A., Hu, Y., Mahalingam, S., Dang, K., Ahn, L., Doyle, N. K., et al. (1998) Eur. J. Immunol. 28, 1089-1103. [DOI] [PubMed] [Google Scholar]
- 14.Oh, S., Berzofsky, J. A., Burke, D. S., Waldmann, T. A. & Perera, L. P. (2003) Proc. Natl. Acad. Sci. USA 100, 3392-3397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van Stipdonk, M. J., Hardenberg, G., Bijker, M. S., Lemmens, E. E., Droin, N. M., Green, D. R. & Schoenberger, S. P. (2003) Nat. Immunol. 4, 361-365. [DOI] [PubMed] [Google Scholar]
- 16.Gett, A. V., Sallusto, F., Lanzavecchia, A. & Geginat, J. (2003) Nat. Immunol. 4, 355-360. [DOI] [PubMed] [Google Scholar]
- 17.Badovinac, V. P., Porter, B. B. & Harty, J. T. (2002) Nat. Immunol. 3, 619-626. [DOI] [PubMed] [Google Scholar]
- 18.Earl, P. L., Hugin, A. W. & Moss, B. (1990) J. Virol. 64, 2448-2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alexander-Miller, M. A., Leggatt, G. R., Sarin, A. & Berzofsky, J. A. (1996) J. Exp. Med. 184, 485-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whelan, J. A., Dunbar, P. R., Price, D. A., Purbhoo, M. A., Lechner, F., Ogg, G. S., Griffiths, G., Phillips, R. E., Cerundolo, V. & Sewell, A. K. (1999) J. Immunol. 163, 4342-4348. [PubMed] [Google Scholar]
- 21.Dutoit, V., Rubio-Godoy, V., Dietrich, P. Y., Quiqueres, A. L., Schnuriger, V., Rimoldi, D., Lienard, D., Speiser, D., Guillaume, P., Batard, P., et al. (2001) Cancer Res. 61, 5850-5856. [PubMed] [Google Scholar]
- 22.Burrows, S. R., Kienzle, N., Winterhalter, A., Bharadwaj, M., Altman, J. D. & Brooks, A. (2000) J. Immunol. 165, 6229-6234. [DOI] [PubMed] [Google Scholar]
- 23.Choi, E. M., Chen, J. L., Wooldridge, L., Salio, M., Lissina, A., Lissin, N., Hermans, I. F., Silk, J. D., Mirza, F., Palmowski, M. J., et al. (2003) J. Immunol. 171, 5116-5123. [DOI] [PubMed] [Google Scholar]
- 24.Denkberg, G., Cohen, C. J. & Reiter, Y. (2001) J. Immunol. 167, 270-276. [DOI] [PubMed] [Google Scholar]
- 25.Daniels, M. A. & Jameson, S. C. (2000) J. Exp. Med. 191, 335-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pittet, M. J., Rubio-Godoy, V., Bioley, G., Guillaume, P., Batard, P., Speiser, D., Luescher, I., Cerottini, J. C., Romero, P. & Zippelius, A. (2003) J. Immunol. 171, 1844-1849. [DOI] [PubMed] [Google Scholar]
- 27.Burkett, P. R., Koka, R., Chien, M., Chai, S., Chan, F., Ma, A. & Boone, D. L. (2003) Proc. Natl. Acad. Sci. USA 100, 4724-4729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaech, S. M. & Ahmed, R. (2001) Nat. Immunol. 2, 415-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arcaro, A., Gregoire, C., Bakker, T. R., Baldi, L., Jordan, M., Goffin, L., Boucheron, N., Wurm, F., van der Merwe, P. A., Malissen, B. & Luescher, I. F. (2001) J. Exp. Med. 194, 1485-1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arcaro, A., Gregoire, C., Boucheron, N., Stotz, S., Palmer, E., Malissen, B. & Luescher, I. F. (2000) J. Immunol. 165, 2068-2076. [DOI] [PubMed] [Google Scholar]
- 31.Cawthon, A. G. & Alexander-Miller, M. A. (2002) J. Immunol. 169, 3492-3498. [DOI] [PubMed] [Google Scholar]
- 32.Dubois, S., Mariner, J., Waldmann, T. A. & Tagaya, Y. (2002) Immunity 17, 537-547. [DOI] [PubMed] [Google Scholar]
- 33.McHeyzer-Williams, M. G. & Davis, M. M. (1995) Science 268, 106-111. [DOI] [PubMed] [Google Scholar]
- 34.Lin, M. Y. & Welsh, R. M. (1998) J. Exp. Med. 188, 1993-2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kedl, R. M., Schaefer, B. C., Kappler, J. W. & Marrack, P. (2002) Nat. Immunol. 3, 27-32. [DOI] [PubMed] [Google Scholar]
- 36.Rodriguez, F., Harkins, S., Slifka, M. K. & Whitton, J. L. (2002) J. Virol. 76, 4251-4259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Derby, M. A., Wang, J., Margulies, D. H. & Berzofsky, J. A. (2001) Int. Immunol. 13, 817-824. [DOI] [PubMed] [Google Scholar]
- 38.Cawthon, A. G., Lu, H. & Alexander-Miller, M. A. (2001) J. Immunol. 167, 2577-2584. [DOI] [PubMed] [Google Scholar]
- 39.Bosselut, R., Kubo, S., Guinter, T., Kopacz, J. L., Altman, J. D., Feigenbaum, L. & Singer, A. (2000) Immunity 12, 409-418. [DOI] [PubMed] [Google Scholar]
- 40.Wheeler, C. J., Chen, J. Y., Potter, T. A. & Parnes, J. R. (1998) J. Immunol. 160, 4199-4207. [PubMed] [Google Scholar]
- 41.Renard, V., Romero, P., Vivier, E., Malissen, B. & Luescher, I. F. (1996) J. Exp. Med. 184, 2439-2444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Irie, H. Y., Mong, M. S., Itano, A., Crooks, M. E., Littman, D. R., Burakoff, S. J. & Robey, E. (1998) J. Immunol. 161, 183-191. [PubMed] [Google Scholar]
- 43.Kwan Lim, G. E., McNeill, L., Whitley, K., Becker, D. L. & Zamoyska, R. (1998) Eur. J. Immunol. 28, 745-754. [DOI] [PubMed] [Google Scholar]
- 44.Bosselut, R., Zhang, W., Ashe, J. M., Kopacz, J. L., Samelson, L. E. & Singer, A. (1999) J. Exp. Med. 190, 1517-1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.