Respiratory complications of preterm birth are an important cause of infant mortality and morbidity. This article looks at how advances in perinatal care have improved outcomes for preterm infants with respiratory distress syndrome and chronic lung disease.
Respiratory distress syndrome
Respiratory distress syndrome of prematurity is a major cause of morbidity and mortality in preterm infants. Primarily, respiratory distress syndrome is caused by deficiency of pulmonary surfactant. Surfactant is a complex mixture of phospholipids and proteins that reduces alveolar surface tension and maintains alveolar stability. As most alveolar surfactant is produced after about 30-32 weeks' gestation, preterm infants born before then will probably develop respiratory distress syndrome. In addition to short gestation, several other clinical risk factors have been identified.
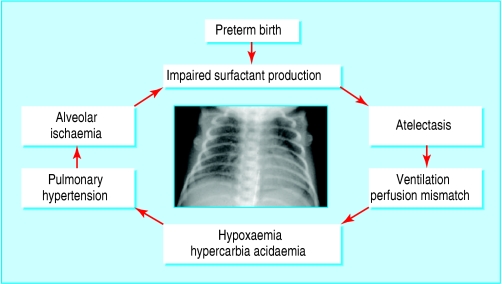
Figure 1.
Pathogenesis of respiratory distress syndrome is a “vicious cycle”
Preterm infants with respiratory distress syndrome present immediately or soon after birth with worsening respiratory distress. The presenting features include tachypnoea (respiratory rate > 60 breaths per minute); intercostal, subcostal, and sternal recession; expiratory grunting; cyanosis; and diminished breath sounds.
Table 1.
Risk factors for respiratory distress syndrome
| • Male sex |
| • White ethnic group |
| • Maternal diabetes |
| • Perinatal asphyxia |
| • Hypothermia |
| • Multifetal pregnancy |
| • Delivery by caesarean section |
If untreated, infants may become fatigued, apnoeic, and hypoxic. They may progress to respiratory failure and will need assisted ventilation. High airway pressures may be required to ventilate the stiff, non-compliant lungs, thereby increasing the risk of acute respiratory complications, such as pneumothorax, pneumomediastinum, and pulmonary interstitial emphysema.
Figure 2.
Endotracheal intubation and ventilation: intercostal drain for pneumothorax
Over the past 20-30 years, two major advances in perinatal management—the use of antenatal corticosteroids and exogenous surfactant replacement—have greatly improved clinical outcomes for preterm infants with respiratory distress syndrome.
Antenatal corticosteroids
Corticosteroids that cross the placenta (dexamethasone or betamethasone) given to women at risk of preterm delivery accelerate fetal surfactant production and lung maturation. The beneficial effects for preterm infants, including a 40% reduced risk of mortality, respiratory distress syndrome, and intraventricular haemorrhage were defined in randomised controlled trials throughout the 1970s and 1980s. The meta-analysis of these trials is a landmark in evidence based perinatal care. Despite the accumulation of such convincing evidence, it is only in the past decade that antenatal corticosteroids have become widely used in clinical practice.
Figure 3.
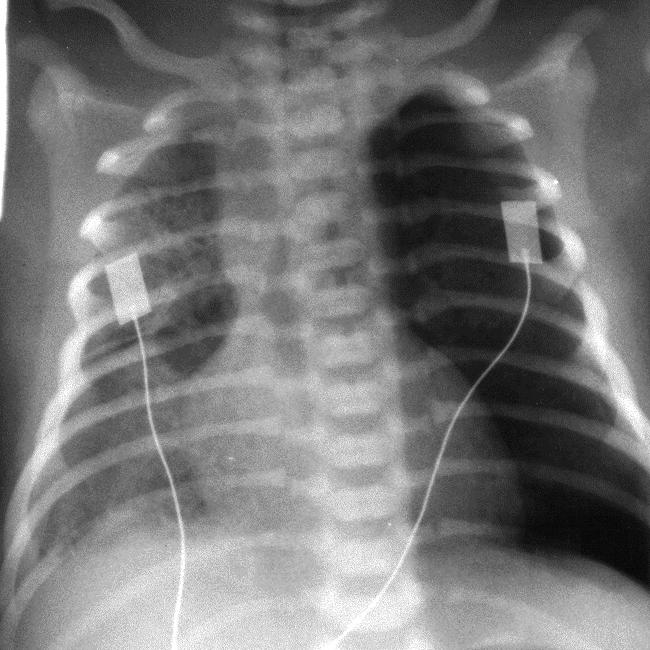
Chest x ray of left pneumothorax (undrained)
The effect of antenatal corticosteroids lasts about a week. A Cochrane systematic review concludes that there is insufficient evidence on the benefits and risks (possible adverse effects on the developing fetal brain) to recommend repeated doses of antenatal corticosteroids for women who have not delivered in one week of the initial course. This clinical uncertainty may be resolved when the results of further trials are available.
Surfactant replacement
Exogenous surfactant, given via an endotracheal tube, for the treatment or prophylaxis of respiratory distress syndrome is associated with a 40% reduction in neonatal mortality and a 30% to 65% reduction in the risk of pneumothorax. In infants at risk of developing respiratory distress syndrome, surfactant replacement is most effective when given at the time of delivery (prophylactic), rather than when symptoms develop (rescue). Treatment with repeated doses of surfactant improves survival compared with single dose treatment in infants with ongoing respiratory distress. Comparative trials have also shown that the use of natural surfactant extracts, usually porcine or bovine, is associated with a lower rate of mortality than if synthetic surfactant products are used.
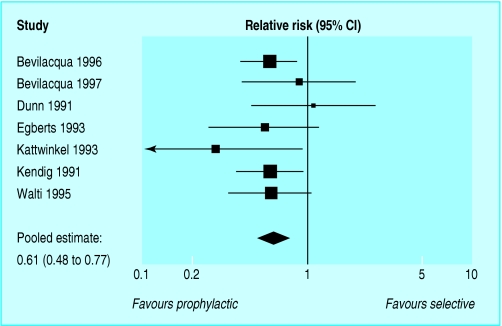
Figure 4.
Meta-analysis of prophylactic versus selective use of surfactant to prevent mortality in preterm infants. Adapted from Soll et al. Cochrane Database Syst Rev 2003;(4): CD000510
Mechanical ventilation
Preterm infants with respiratory distress syndrome often require a period of assisted ventilatory support. The aim is to treat the hypoxaemia and hypercarbia associated with respiratory distress syndrome while minimising ventilator associated lung trauma and oxygen toxicity.
Table 2.
Indications for mechanical ventilation in preterm infants with respiratory distress syndrome
| • Hypoxaemia (paO2 < 50 mmHg) |
| • Hypercarbia (paCO2 > 50 mmHg) |
| • Acidosis (pH < 7.25) |
| • Cardiorespiratory collapse |
| • Persistent apnoea or bradycardia |
In conventional mechanical ventilation, the positive pressure ventilator delivers a given numbers of breaths (for a set inspiratory time at a set pressure) regardless of the baby's inspiratory effort. Ventilating preterm babies at fast rates (> 40 breaths per minute) and with short inspiratory times (< 0.4 seconds) improves outcomes (including reducing the risk of pneumothorax) more than ventilation at lower rates with longer inspiratory times.
Modern ventilators can be set to trigger or to integrate with the baby's inspiratory effort (patient triggered ventilation). High frequency oscillator and jet ventilators deliver extremely rapid rates (about 600-800 breaths per minute) of very small tidal volumes. Although the results of physiological studies have indicated that these newer ventilators may have advantages over conventional mechanical ventilation, randomised controlled trials have not provided any convincing evidence of clinically important beneficial effects.
Continuous positive airway pressure
The simplest and least invasive type of ventilator provides nasal continuous positive airway pressure (nCPAP). These ventilators provide a constant end distending pressure to maintain alveolar recruitment, prevent atelectasis, and improve gas exchange.
Figure 5.
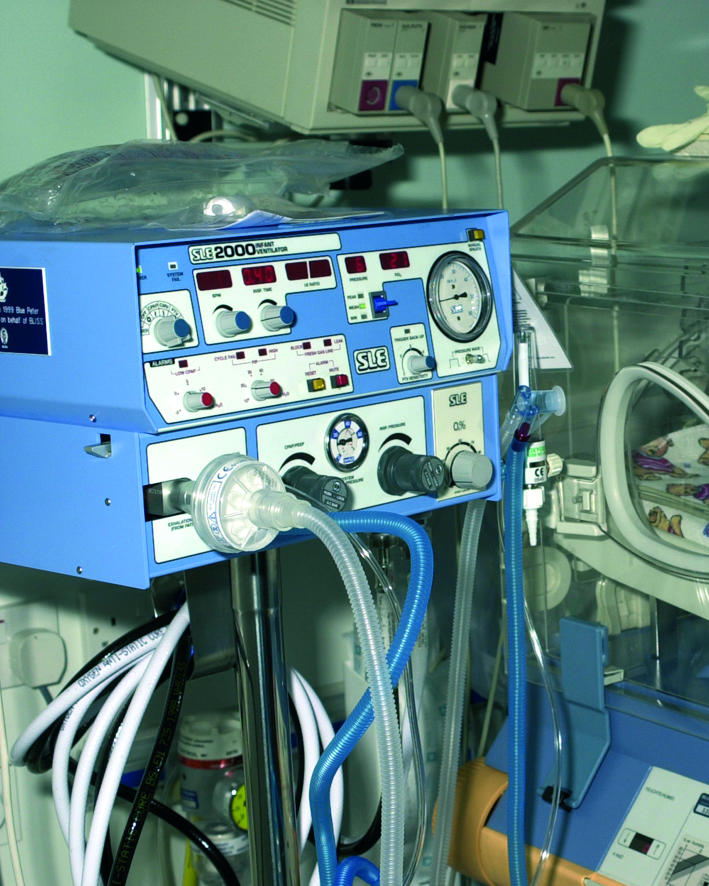
Conventional mechanical ventilators are usually set to deliver a given number of breaths for a set inspiratory time at a set pressure
After a period of endotracheal positive pressure ventilation, nCPAP is effective in preventing failure of extubation in preterm infants. Cohort studies have also showed that early use of nCPAP in preterm infants with respiratory distress syndrome may reduce the need for endotracheal intubation for positive pressure ventilation. Randomised trials are needed to determine the relative benefits and risks of prophylactic nCPAP in preterm infants, and to establish the optimal mode and timing of nCPAP use. These trials should also explore the effect of administering exogenous surfactant in association with nCPAP. Data from animal studies, and preliminary data from a randomised controlled trial, have provided some evidence that nCPAP combined with prophylactic surfactant might further reduce the need for endotracheal intubation and positive pressure ventilation.
Figure 6.
Nasal continuous positive airway pressure can be delivered via sealed nasal prongs or a nasal mask without the need for endotracheal intubation
Chronic lung disease
The most important long term complication of respiratory distress syndrome is chronic lung disease of prematurity, which is usually defined as a need for ventilatory support or supplemental oxygen at 36 weeks after conception. The risk of chronic lung disease is related to the degree of prematurity and severity of the initial lung disease and to the duration of mechanical ventilation and oxygen administration. Despite the use of antenatal corticosteroids and surfactant replacement, the incidence of chronic lung disease has continued to rise over the past decade, possibly because of the increased survival of extremely preterm infants.
Figure 7.
Infant with chronic lung disease (nasal prongs for oxygen)—chronic lung disease develops in about one quarter of preterm infants who receive positive pressure ventilation for respiratory distress syndrome
Table 3.
Risk factors for chronic lung disease
| • Short gestation |
| • Small for gestational age |
| • Severity of respiratory distress syndrome |
| • Duration of mechanical ventilation |
| • Duration of oxygen administration |
| • Patent ductus arteriosus |
| • Maternal chorioamnionitis |
| • Postnatal sepsis |
Postnatal steroids for chronic lung disease
Because inflammation (secondary to infection and ventilator induced lung damage) may be an important part of the disease process, corticosteroids have been used for prophylaxis and treatment of evolving or established chronic lung disease. Although systemic corticosteroids (dexamethasone or betamethasone) may have short term benefits such as earlier endotracheal extubation, there are also short term complications. These complications include hypertension, hyperglycaemia, gastrointestinal bleeding, hypertrophic cardiomyopathy, infection, and adrenal suppression. Additionally, recent studies in animal models and meta-analyses of clinical trials have highlighted concerns about long term complications, including poor brain growth and adverse developmental and neuromotor outcomes, including cerebral palsy.
The risk of adverse longer term outcomes seems to be greatest when corticosteroids are prescribed in the first few days after birth (prophylaxis). Data with regard to long term neurodevelopment when infants receive therapeutic corticosteroids after the first week of life are more reassuring. Until further evidence has been obtained, corticosteroids should be prescribed in exceptional circumstances only and after discussion of the possible risks with the infant's parents.
Figure 8.
Planning for home oxygen treatment needs to be carefully coordinated and should include a programme of education and training for all members of family who will be caring for the baby
Inhaled corticosteroids
Little evidence exists to support the use of nebulised corticosteroids for preterm infants with evolving or established respiratory distress syndrome, although their use in ventilated infants with chronic lung disease may allow earlier extubation.
Diuretics for chronic lung disease
Diuretics are often used to treat infants with chronic lung disease because they reduce pulmonary oedema, decrease oxygen requirements, and improve lung compliance. Diuretics, however, also cause electrolyte disturbances, bone loss, and nephrocalcinosis. Furthermore, there is little evidence that the use of diuretics has any long term clinically important benefits in preterm infants with chronic lung disease.
Table 4.
Preparation for home oxygen treatment
| • Parental training—how to monitor respiratory status, when to provide extra oxygen, when and where to get help, cardiorespiratory resuscitation |
| • Family support—usually from community nurse |
| • Risk assessment of the home environment |
| • Insurance of car and house |
| • Notify fire and ambulance services |
| • Financial help—disability parking permits, disability living allowances |
Home oxygen treatment
Infants with chronic lung disease, who remain dependent on supplemental oxygen to maintain appropriate oxygen saturation, but who are otherwise ready for discharge home, may be suitable for home oxygen treatment. Home oxygen treatment programmes are delivered by a multidisciplinary team that includes the family plus key staff from hospital, primary care, and pharmacy services.
Outside the context of a randomised, controlled trial the use of corticosteroids should be limited to exceptional clinical circumstances—for example, an infant on maximal ventilatory and oxygen support. In those circumstances, parents should be fully informed about the known short and long term risks and agree to treatment—American Academy of Pediatrics Committee on Fetus and Newborn. Pediatrics 2002;109: 330-8
After discharge home, infants with chronic lung disease have a higher risk of rehospitalisation with respiratory illness than infants of the same gestational age who do not have chronic lung disease. For example, one in eight infants with chronic lung disease requires readmission to hospital for respiratory syncitial virus bronchiolitis. Immunoprophylaxis with anti-respiratory syncitial virus antibodies may reduce hospital readmission rates. It is expensive, however, and has not been shown to be effective in reducing mortality or major morbidity, such as the need for mechanical ventilation. Parents can be reassured that infants with chronic lung disease have few clinically important respiratory problems in later childhood.
Figure 9.
Home oxygen treatment allows earlier hospital discharge but parents are committed to the programme for at least several months while the supplemental oxygen is gradually reduced
Conclusion
Advances in perinatal care, particularly the use of mechanical ventilation, antenatal steroids, and exogenous surfactant replacement have improved outcomes for preterm infants. The incidence of chronic lung disease has not decreased, however, and further research is needed to define safe and effective ways to prevent and treat this condition. These efforts should continue in parallel with the development and evaluation of family centred treatments for chronic lung disease, such as home oxygen treatment programmes.
Jenn Fraser is specialist registrar and Moira Walls is neonatal nurse in the neonatal intensive care unit, Ninewells Hospital and Medical School, Dundee.
The ABC of preterm birth is edited by William McGuire, senior lecturer in neonatal medicine, Tayside Institute of Child Health, Ninewells Hospital and Medical School, University of Dundee; and Peter W Fowlie, consultant paediatrician, Perth Royal Infirmary and Ninewells Hospital and Medical School, Dundee. The series will be published as a book in spring 2005.
Competing interests: For WMcG's competing interests see first article in the series.
References
- • Crowley P. Prophylactic corticosteroids for preterm birth. Cochrane Database Syst Rev 2003;(4): CD000065. [DOI] [PubMed]
- • Soll RF, Morley CJ. Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev 2003;(4): CD000510. [DOI] [PubMed]
- • Greenough A, Milner AD, Dimitriou G. Synchronized mechanical ventilation for respiratory support in newborn infants. Cochrane Database Syst Rev 2003;(4): CD000456. [DOI] [PubMed]
- • Henderson-Smart DJ, Bhuta T, Cools F, Offringa M. Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Cochrane Database Syst Rev 2003;(4): CD000104. [DOI] [PubMed]
- • Halliday HL, Ehrenkranz RA. Moderately early postnatal (7-14 days) corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst Rev 2003;(1): CD001144. [DOI] [PubMed]
- • Brion LP, Primhak RA, Ambrosio-Perez I. Diuretics acting on the distal renal tubule for preterm infants with (or developing) chronic lung disease. Cochrane Database Syst Rev 2003;(4): CD001817. [DOI] [PubMed]
- • Wang EEL, Tang NK. Immunoglobulin for preventing respiratory syncytial virus infection. Cochrane Database Syst Rev 2003;(4): CD001725. [DOI] [PubMed]