Abstract
AIM
To evaluate the results of the Ilizarov method in management of cases with bone loss, soft tissue loss and infection.
METHODS
Twenty eight patients with severe leg trauma complicated by bone loss, soft tissue loss and infection were managed by distraction osteogenesis in our institution. After radical debridement of all the infected and dead tissues the Ilizarov frame was applied, corticotomy was done and bone transport started. The wounds were left open to drain. Partial limb shortening was done in seven cases to reduce the size of both the skeletal and soft tissue defects. The average follow up period was 39 mo (range 27-56 mo).
RESULTS
The infection was eradicated in all cases. All the soft tissue defects healed during bone transport and plastic surgery was only required in 2 cases. Skeletal defects were treated in all cases. All patients required another surgery at the docking site to fashion the soft tissue and to cover the bone ends. The external fixation time ranged from 9 to 17 mo with an average of 13 mo. The complications included pin tract infection in 16 cases, wire breakage in 2 cases, unstable scar in 4 cases and chronic edema in 3 cases. According to the association for study and application of methods of Ilizarov score the bone results were excellent in 10, good in 16 and fair in 2 cases while the functional results were excellent in 8, good in 17 and fair in 3 cases.
CONCLUSION
Distraction osteogenesis is a good method that can treat the three problems of this triad simultaneously.
Keywords: Ilizarov methods, Bone defect, Soft tissue reconstruction, Open bone transport
Core tip: Bone and soft tissue loss represent a true challenge for both the orthopedic and plastic surgeons. The presence of bone and soft tissue infection further complicates limb reconstruction. In this study a series of 28 patients with severe lower limb trauma were managed by the Ilizarov method without the need for major plastic surgery. The results were encouraging.
INTRODUCTION
Bone loss represents a true challenge for orthopedic surgeons. Soft tissue loss may complicate the condition and makes reconstruction more difficult. Bone infection may further complicate the condition and makes reconstruction extremely difficult[1-4]. So, the triad of bone loss, soft tissue loss and infection is considered to be an unhappy triad in the field of limb reconstruction. In the presence of this triad the scope for reconstruction becomes very narrow and amputation may be the end result.
It is important to restore a healthy soft tissue envelope for proper treatment of this complex problem. This could be done by major plastic surgery in the form of local myocutaneous flaps, or free flaps. But, in the presence of infection the chance for success of these plastic surgeries becomes very limited[5,6]. During distraction osteogenesis all the tissues are lengthened including the bone, vessels, nerves, muscles and skin. This gradual lengthening may lead to spontaneous closure of the soft tissue defects without the need for plastic surgery[7-9].
The aim of this study is to evaluate the results of distraction osteogenesis in management of cases with severe leg trauma complicated by bone loss, soft tissue loss and infection.
MATERIALS AND METHODS
Between April 2007 and Jun 2014, twenty eight patients with bone loss, soft tissue loss and infection were treated by distraction osteogenesis in our institution. The average age of the patients was 37 years (range: 16-58 years). There were 23 males and 5 females. The etiology of this complex problem was trauma sequelae in all of the cases. Plastic surgery was performed in 12 cases but it failed because of infection. After radical debridement, the average size of the skeletal defects was 8 cm (range: 6 to 14 cm) and the soft tissue defects ranged from 3 cm × 4 cm to 6 cm × 11 cm, with an average of 5 cm × 7 cm. The defects were located in the proximal third of the leg in 6 patients, middle third in 13 patients and distal third in 9 patients. All cases were infected with an active discharge. The ethical committee in our institution approved this study. Informed consent was taken from the patients before being included in the study. Under general or spinal anesthesia, the infected and dense fibrous tissues were excised. The infected and necrotic bone ends were debrided down to a healthy bleeding surface. Further debridement of the exposed bone ends was done until they became well covered by the skin and soft tissue. The Ilizarov frame was applied and corticotomy was performed in a healthy bone segment. The wounds were left open to drain (Figure 1). Physiotherapy was started early in the postoperative period to avoid joint contracture. It involved isometric contraction of the quadriceps muscles, active and passive range of movement and stretching exercises for the hamstring and gastrocsoleous complex. Bone transport was started after a latent period of about one week. Patients were discharged after an average of 8 d and followed up regularly in the outpatient clinic. During bone transport the bone segment carries its surrounding soft tissues with it and the soft tissue defects gradually close. As transport is done without sufficient soft tissue coverage it is called open bone transport. At the time of docking the skin becomes incarcerated between the bone ends (Figure 1D). At this stage the patient is taken to theater again where the soft tissue is removed from the docking site and the skin is fashioned to cover the bone ends. Transverse skin incision is preferred in this step to facilitate skin closure. It was made along the bone ends of the proximal and distal fragments. The incision was deepened down to the bone and the soft tissues were removed from the docking site. The bone ends were freshened and compressed against each other by the frame. This compression approximates the skin edges together and facilitates their closure over the bone ends (Figure 2). Bone graft was done at this time to stimulate bone healing in 15 cases. Partial limb shortening was done in 7 cases to reduce the size of both the soft tissue and bone gaps. After docking, bone lengthening was continued to equalize the limb lengths in those cases.
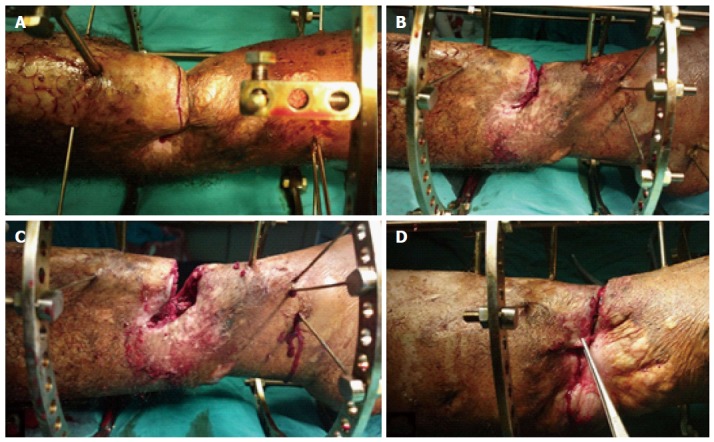
Figure 1.

Surgical technique. The infected and necrotic bones are excised (A) and further debridement of the bone ends is done until they recessed under the skin and soft tissues (B); C: The Ilizarov frame is applied and bone transport started; D: At the time of docking the skin is invaginated between the bone ends.
Figure 2.
Management of the docking site. A: Transverse skin incision is made along the bone ends at the docking site; B: The incision is deepened down to the bone and the soft tissues are removed from the docking site; C: The bone ends are freshened and compressed against each other by the frame; D: This compression approximates the skin edges together and facilitates their closure over the bone ends.
The frame was removed after healing of the docking site and full maturation of the regenerated bone. The average follow up period was 39 mo (range: 27 to 56 mo). The results were evaluated according to the association for study and application of methods of Ilizarov (ASAMI) scoring system[10]. In this system the results are divided into bone results and functional results. The bone results are evaluated according to union, infection, deformity and limb length discrepancy while the functional results are evaluated according to daily activities, joint stiffness, limp, pain and presence of reflex sympathetic dystrophy.
RESULTS
The infection was eradicated in all of the cases. All the soft tissue defects healed during the process of bone transport and plastic surgery was only required in two cases. Bone defects were bridged in all cases (Figure 3). All patients required another surgery at the time of docking to fashion the soft tissue and to cover the bone ends. The docking sites united without the need for bone graft in 13 cases and with bone graft in 15 cases. The average time of external fixation was 13 mo (range: 9 to 17 mo). The complications in this study were pin tract infection in 16 cases (treated by local care and oral antibiotics), wire breakage in 2 cases (treated by reinsertion of new wires), unstable scar in 4 cases and chronic edema in 3 cases. The limb length discrepancy did not exceed 2.5 cm except in one case. No cases were complicated by amputation or reflex sympathetic dystrophy. Using the ASAMI scoring system, the bone results were excellent in 10, good in 16 and fair in 2 cases while the functional results were excellent in 8, good in 17 and fair in 3 cases.
Figure 3.

Middle third bone and soft tissue defects. A: Forty-seven year old male patient with combined bone loss, soft tissue loss and infection of his left leg as a complication of an open fracture of the tibia and fibula; B: Debridement of the bone ends was done, Ilizarov frame applied and bone transport started; C: During bone transport the soft tissue defect gradually closes; D: At the time of docking the skin was fashioned over the bone ends; E: After removal of the frame with good bone healing; F: The patient with good alignment and complete healing of the soft tissue.
DISCUSSION
The tibia is the most common site for open fracture of the long bones due to its anatomic location and scanty soft tissue coverage. Also it is more liable for complications due to its poor blood supply. These complications include soft tissue necrosis, bone loss and infection[11-13]. Successful treatment of the soft tissue loss is vital for bone healing. This could be done by free or local myocutaneous flaps. But, in certain situations these major plastic surgeries may be not feasible or they may endanger the limb survival. These conditions include severe infection and local vascular problems. In the presence of infection the chance for success of plastic surgery is limited and additional surgery may be required to control infection prior to the major plastic surgery[5,14,15]. After severe trauma some limbs may be left with only one blood vessel and if it is used as a feeding artery for the graft this may threaten the limb life. In case of failure of these surgeries the choice between amputation and another modality of reconstruction should be made.
In this study, 28 patients with the complex problem of bone loss, soft tissue loss and infection were treated by the Ilizarov method with satisfactory results in most of them. All the wounds healed during bone transport and plastic surgery was only required in two cases. We found that it was not necessary to restore the soft tissue coverage before skeletal reconstruction. After thorough debridement the combined bone and soft tissue gaps could be treated simultaneously by the process of distraction osteogenesis. In the two cases that required plastic surgery, the soft tissue defects were big - 4 cm × 7 cm and 5 cm × 9 cm, respectively. During bone transport the defects decreased but did not close completely. The infection was eradicated in both of them and they were easily treated by local muscle flaps.
To avoid protrusion of the bone fragment from the wound during distraction the bone ends must be debrided until they become well covered by the skin. So, when distraction is started the bone fragment carries its surrounding soft tissue with it and the soft tissue creeps gradually until the defect heals spontaneously[9].
The soft tissue defects in the lower third of the leg are difficult to treat. Free-flaps is the best method for coverage of soft tissue defects in this area but the procedure is technically difficult, requires skilled surgeons and the recipient site should have suitable vessels which is a big problem in major tibial fractures[16-18]. Perforator-based flaps or a distally-based soleus flap may be suitable for the lower third of the leg but the results are controversial[19-21]. Karbalaeikhani et al[21] used a soleus flap to treat soft tissue defects in the middle and lower third of the leg and reported a high failure rate in the distal third. They recommend preoperative assessment by angiography before surgery.
In this study, the defects were present in the distal third of the leg in 9 patients. All of them were treated by the Ilizarov method and none of them required plastic surgery (Figure 4). Partial shortening of the limb helps to reduce the size of the bone and soft tissue defects and decreases the time required for soft tissue healing. After docking the frame must be adjusted to allow for further lengthening to restore the limb length.
Figure 4.
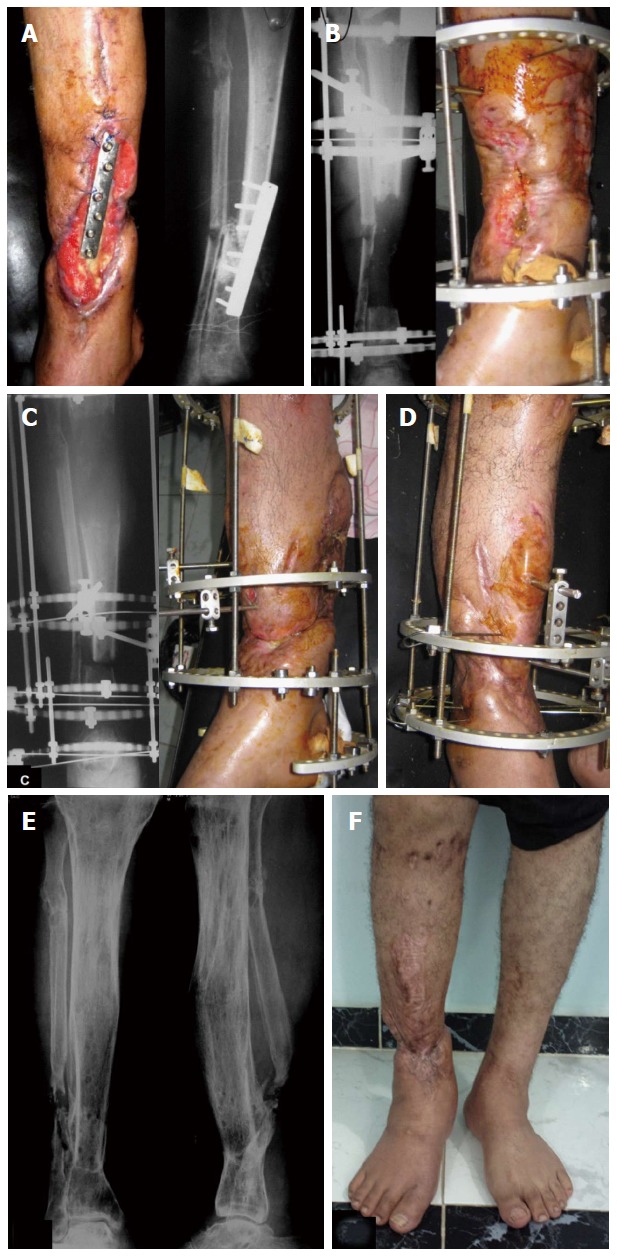
Lower third bone and soft tissue defects. A: Thirty-nine year old male patient with skin loss, infection and exposed plate in the lower third of his right leg; B: After radical debridement and application of the Ilizarov external fixator; At the time of docking the skin was fashioned to cover the bone ends (C) and it healed completely (D); After removal of the frame with good bone healing (E) and the patient with good alignment and complete healing of the soft tissue (F).
Bone graft was required in 15 cases to stimulate bone healing at the docking site. In such cases small amounts of cancellous bone graft were sufficient for this purpose. The unstable scar is an important problem with this technique. It happened in four of our patients early in the course of this study. It usually occurs at the docking site because the skin is thin and adherent in this area. This skin is liable to injury and chronic ulceration due to minor trauma. Prolonged protection of the skin is required to prevent it from injury. We could avoid this complication by resection of more bone at the time of docking until thick healthy skin meets each other over the bone at the docking site.
The method of Ilizarov is good for reconstruction of patients with bone loss, soft tissue loss and infection. The three problems could be treated simultaneously without the need for major plastic surgery. Infection is treated by radical debridement while the bone and soft tissue defects are managed by bone and soft tissue transport. Good experience with the Ilizarov frame, better understanding of the distraction process and proper handling of the soft tissues are required to get the best results.
COMMENTS
Background
Bone and soft tissue loss are common after major limb trauma. The presence of infection will further complicate limb reconstruction. The healthy soft tissue envelope is essential for bone healing. This could be achieved by either local or free myocutaneous flaps. Unfortunately these surgeries are technically demanding, time consuming and may be associated with major complications.
Research frontiers
During distraction osteogenesis both the bone and soft tissue are lengthened which may help in spontaneous closure of the soft tissue defect.
Innovations and breakthroughs
In this study the complex problem of combined bone loss, soft tissue loss and infection was treated by distraction osteogenesis without the need for major plastic surgery except in 2 cases.
Applications
This method could be used for treatment of cases with post traumatic bone and soft tissue loss with or without infection. It is not necessary to restore the soft tissue envelope before osseous reconstruction. During bone transport both the bone and soft tissue defects will heal spontaneously. It is highly indicated after failure of plastic surgeries and for cases with a poor vascular bed that does not allow major plastic surgery to be done.
Terminology
Distraction osteogenesis is the mechanical induction of new bone formation between two bony surfaces when they are gradually pulled apart. It was developed by Ilizarov in the fifties of the last century. A low grade cortical osteotomy is made in a healthy bone segment and the circular external fixator is usually used to apply the distraction force. It is also known as Ilizarov method; Bone transport: A condition in which a healthy bone segment is transported locally and gradually through the soft tissue to bridge a bone defect; The docking site is the site where the bone ends come to meet each other after bone transport.
Peer-review
The paper reports a good method for the treatment of lower limb tissue loss. It is interesting and well written. References are adequate.
Footnotes
Institutional review board statement: The study was approved by the ethical committee in our institution.
Informed consent statement: All patients gave their informed consent before being included in the study.
Conflict-of-interest statement: The author has no conflict of interest.
Data sharing statement: No available data sharing.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Egypt
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: April 26, 2016
First decision: July 5, 2016
Article in press: August 29, 2016
P- Reviewer: Lui PPY, Minana MD, Negosanti L S- Editor: Ji FF L- Editor: O’Neill E- Editor: Wu HL
References
- 1.Ilizarov GA, Ledyaev VI. The replacement of long tubular bone defects by lengthening distraction osteotomy of one of the fragments. 1969. Clin Orthop Relat Res. 1992;(280):7–10. [PubMed] [Google Scholar]
- 2.Green SA. Skeletal defects. A comparison of bone grafting and bone transport for segmental skeletal defects. Clin Orthop Relat Res. 1994;(301):111–117. [PubMed] [Google Scholar]
- 3.Yazar S, Lin CH, Wei FC. One-stage reconstruction of composite bone and soft-tissue defects in traumatic lower extremities. Plast Reconstr Surg. 2004;114:1457–1466. doi: 10.1097/01.prs.0000138811.88807.65. [DOI] [PubMed] [Google Scholar]
- 4.Gordon L, Chiu EJ. Treatment of infected non-unions and segmental defects of the tibia with staged microvascular muscle transplantation and bone-grafting. J Bone Joint Surg Am. 1988;70:377–386. [PubMed] [Google Scholar]
- 5.Jordan DJ, Malahias M, Hindocha S, Juma A. Flap decisions and options in soft tissue coverage of the lower limb. Open Orthop J. 2014;8:423–432. doi: 10.2174/1874325001408010423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jain AK, Sinha S. Infected nonunion of the long bones. Clin Orthop Relat Res. 2005;(431):57–65. doi: 10.1097/01.blo.0000152868.29134.92. [DOI] [PubMed] [Google Scholar]
- 7.Paley D, Maar DC. Ilizarov bone transport treatment for tibial defects. J Orthop Trauma. 2000;14:76–85. doi: 10.1097/00005131-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Robert Rozbruch S, Weitzman AM, Tracey Watson J, Freudigman P, Katz HV, Ilizarov S. Simultaneous treatment of tibial bone and soft-tissue defects with the Ilizarov method. J Orthop Trauma. 2006;20:197–205. doi: 10.1097/00005131-200603000-00006. [DOI] [PubMed] [Google Scholar]
- 9.El-Alfy B, El-Mowafi H, El-Moghazy N. Distraction osteogenesis in management of composite bone and soft tissue defects. Int Orthop. 2010;34:115–118. doi: 10.1007/s00264-008-0574-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paley D, Catagni MA, Argnani F, Villa A, Benedetti GB, Cattaneo R. Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res. 1989;(241):146–165. [PubMed] [Google Scholar]
- 11.Court-Brown CM, Bugler KE, Clement ND, Duckworth AD, McQueen MM. The epidemiology of open fractures in adults. A 15-year review. Injury. 2012;43:891–897. doi: 10.1016/j.injury.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Canale ST, Beaty JH. Campbell’s Operative Orthopaedics. 12th ed. Missouri: Mosby; 2012. pp. 1405–1406. [Google Scholar]
- 13.Bucholz RW, Heckman JD, Court-Brown CM. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2009. pp. 376–377. [Google Scholar]
- 14.Olesen UK, Juul R, Bonde CT, Moser C, McNally M, Jensen LT, Elberg JJ, Eckardt H. A review of forty five open tibial fractures covered with free flaps. Analysis of complications, microbiology and prognostic factors. Int Orthop. 2015;39:1159–1166. doi: 10.1007/s00264-015-2712-z. [DOI] [PubMed] [Google Scholar]
- 15.Schöttle PB, Werner CM, Dumont CE. Two-stage reconstruction with free vascularized soft tissue transfer and conventional bone graft for infected nonunions of the tibia: 6 patients followed for 1.5 to 5 years. Acta Orthop. 2005;76:878–883. doi: 10.1080/17453670510045534. [DOI] [PubMed] [Google Scholar]
- 16.Heller L, Levin LS. Lower extremity microsurgical reconstruction. Plast Reconstr Surg. 2001;108:1029–141; quiz 1042. doi: 10.1097/00006534-200109150-00036. [DOI] [PubMed] [Google Scholar]
- 17.Pu LL, Medalie DA, Rosenblum WJ, Lawrence SJ, Vasconez HC. Free tissue transfer to a difficult wound of the lower extremity. Ann Plast Surg. 2004;53:222–228. doi: 10.1097/01.sap.0000120526.11702.29. [DOI] [PubMed] [Google Scholar]
- 18.Abdelrahman I, Moghazy A, Abbas A, Elmasry M, Adly O, Elbadawy M, Steinvall I, Sjoberg F. A prospective randomized cost billing comparison of local fasciocutaneous perforator versus free Gracilis flap reconstruction for lower limb in a developing economy. J Plast Reconstr Aesthet Surg. 2016;69:1121–1127. doi: 10.1016/j.bjps.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 19.Tajsic N, Winkel R, Husum H. Distally based perforator flaps for reconstruction of post-traumatic defects of the lower leg and foot. A review of the anatomy and clinical outcomes. Injury. 2014;45:469–477. doi: 10.1016/j.injury.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Pu LL. Successful soft-tissue coverage of a tibial wound in the distal third of the leg with a medial hemisoleus muscle flap. Plast Reconstr Surg. 2005;115:245–251. [PubMed] [Google Scholar]
- 21.Karbalaeikhani A, Saied A, Heshmati A. Effectiveness of the Gastrocsoleous Flap for Coverage of Soft Tissue Defects in Leg with Emphasis on the Distal Third. Arch Bone Jt Surg. 2015;3:193–197. [PMC free article] [PubMed] [Google Scholar]


