Abstract
Obstructive sleep apnea (OSA) is characterized by episodes of pharyngeal collapse during sleep. Craniofacial alterations such as retrognathia are often found in OSA patients. Maxillomandibular advancement (MMA) surgeries increase the pharyngeal space and are a treatment option for OSA. The aim of this study was to present a successful case of MMA surgery in the treatment of OSA. A patient with moderate OSA (apnea-hypopnea index (AHI)=25.2) and mandibular retrognathism and Maxillomandibular asymmetry underwent MMA surgery. The apnea-hypopnea index (AHI) were considerably improved after six months (IAH =6.7) and one year of treatment (IAH=0.2).
Keywords: Maxillomandibular advancement, Obstructive Sleep Apnea Syndrome, Mandibular retrognathism
1. Introduction
Obstructive sleep apnea syndrome (OSAS) is characterized by obstructive events of the upper airway (UAW) during sleep, which can be associated with clinical signs and symptoms such as snoring, excessive daytime sleepiness, impaired memory, and fatigue [1].
Although CPAP is the first choice for treatment of OSAS in adults, 17–54% of patients do not take this therapy for long periods [2]. Because of low compliance of CPAP, other forms of treatment, such as maxillomandibular advancement (MMA) surgery, were suggested as an alternative for CPAP and tracheostomy in the treatment of OSAS [2], [3]. It is an alternative to severe OSA treatment in patients with maxillomandibular abnormalities, and patients with mild and moderate OSAS there are other treatment alternatives.
A meta-analysis of 22 studies (627 subjects with OSA) determined that MMA is highly effective with a mean decrease in AHI from 64/h to 11/h (P<0.001) with pooled surgical success and cure (AHI<5/h) rates of 86% and 43%, respectively [18].
OSAS patients have diminished UAW dimensions associated with maxillomandibular abnormalities[4]. Imaging tests such as cone beam computed tomography (CBCT) have shown that the UAW is significantly smaller in patients with OSAS [5]. For the other hand, MMA surgery increased the anteroposterior and lateral dimensions of the upper airway from the level of the hard palate to the hyoid bone [6]. When MMA and chin advancement are combined into a single surgical procedure, forward displacement of the soft palate, base of the tongue, hyoid bone, and anterior wall of the pharynx occurs, increasing the volume of the nasopharynx (NP), oropharynx (OP) and hypopharynx (HP) [7].
The purpose of this case report is to present the changes in the AHI and the volumetric changes in the UAW in a patient with severe OSAS treated with MMA surgery and advancement genioplasty.
2. Case report
Patient ERM (29 years old, Caucasian, with a body mass index (BMI) of 24.93 kg/m2) consulted the otorhinolaryngology service for treatment of sleep disturbances. His main complaints were snoring (visual analog scale of 10 cm =8 - held by his wife), breathing pauses during the night observed by his partner, excessive daytime sleepiness (Epworth score =12), and fatigue.
A complete polysomnographic evaluation was recommended, according to the American Academy of sleep Medicine (AASM) (2007) guidelines and considering the recommended rule for hypopnea. The patient showed an apnea-hypopnea index (AHI) of 30.8. The patient was referred for treatment with CPAP but was intolerant to its use after a few months.
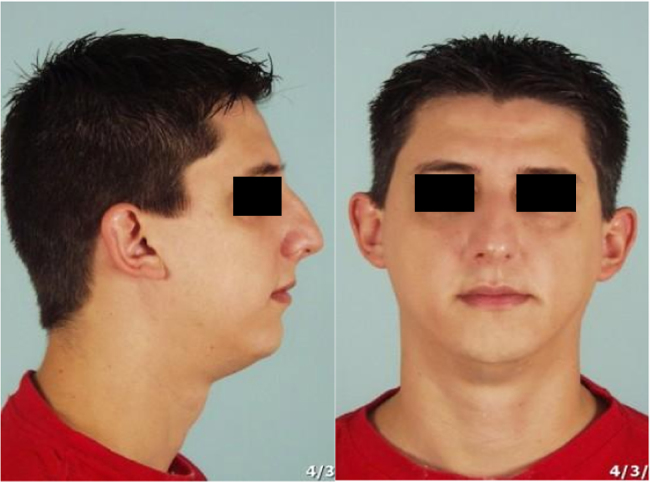
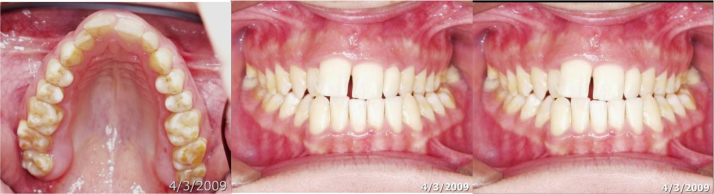
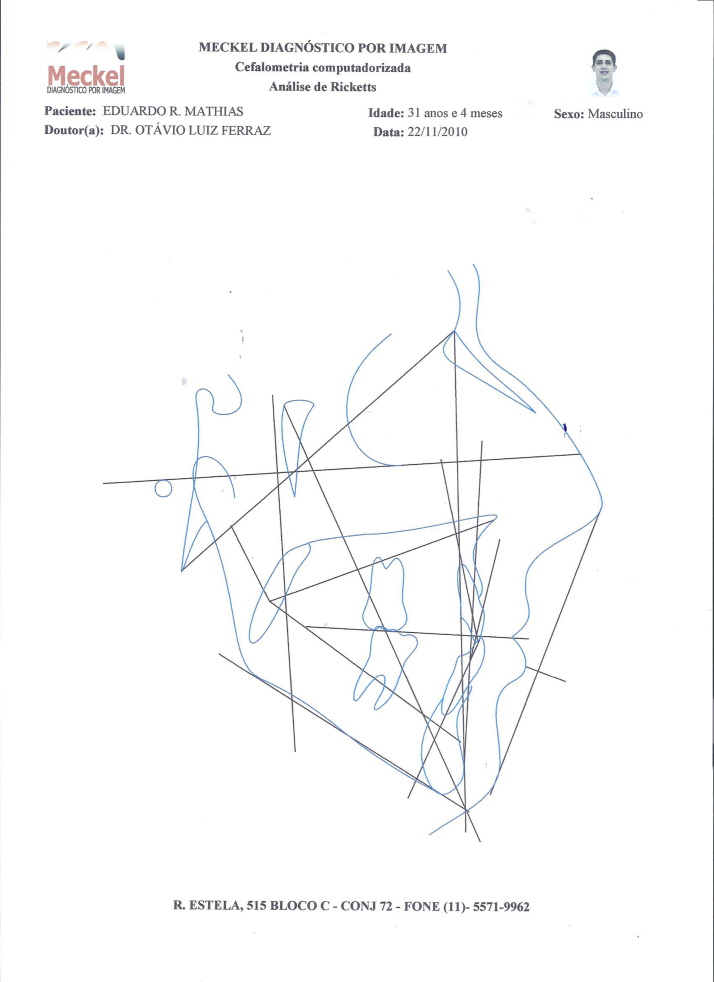
MMA surgery and advancement genioplasty were indicated due to a mandibular anteroposterior deficiency and maxilomandibular asymmetry (Fig. 1). On clinical examination, the patient showed Angle Class II malocclusion, transverse maxillary atresia, a bilateral crossbite, and a modified Mallampati classification of 4 (Fig. 2).
Fig. 1.
Facial features pre-treatment.
Fig. 2.
Intraoral features pre-treatment.
The patient was then referred for preoperative orthodontic treatment. The Epworth Sleepiness Scale (ESS), an overnight polysomnographic evaluation, and CBCT were performed before treatment, after orthodontic treatment, and one year after MMA surgery. A polysomnographic evaluation and the ESS were also administered six months after the surgery. The patient signed an informed consent form for the proposed treatment, and the guidelines of the Declaration of Helsinki were followed.
A complete polysomnographic evaluation was performed using a digital system (EMBLA® S7000, Embla Systems, Inc., Broomfield, CO, USA) according to the manual of the American Academy of Sleep Medicine (2007) [8]. The hypopnea stage was defined according to the recommended rule (AASM, 2007) [8].
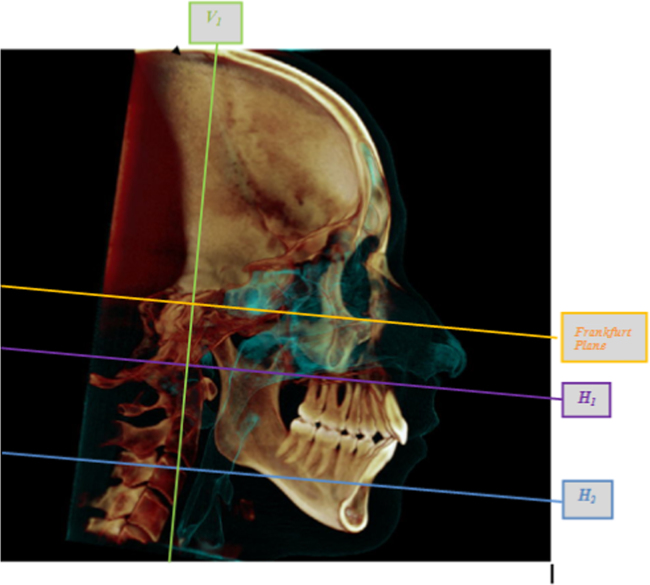
CBCT was performed at a specialized radiological center using i-CAT® imaging equipment (Imaging Sciences International, Hatfield, PA, USA). All images were calibrated using the following parameters: 36.90 mA, 120 kVp, an exposure time of 40 s, an extended height field of view (FOV), a voxel resolution (volume element) of 0.3 mm, a resolution of 1024×1024 pixels, and 12 bits per pixel. During image acquisition, the individual remained in a seated positioned with the Frankfurt plane parallel to the ground and the midsagittal plane perpendicular to the ground, with his lips at rest. The image acquisition extended from 2 cm above the glabella to the lower region of the head (chin and neck), including the inferior border of the fourth cervical vertebra (C4). Axial sections (0.3 mm thick) were obtained and exported in the Digital Imaging and Communication in Medicine (DICOM) format. The Dolphin Imaging® 3-D software, version 11.5 (Dolphin Imaging & Solutions, Chatsworth, CA, USA), was used to process and manipulate the volumetric data (DICOM files) of the NP, OP, and HP to assess the total volume (TV) selected from these pre-defined structures and the position and changes of the most constricted airspace segment (smallest area - SA). A postoperative CBCT evaluation was performed 12 months after the MMA surgery, while polysomnographic evaluations were performed at six and 12 months after the MMA surgery. The points and lines used to define the region evaluated are described in Fig. 3.
-
•
Upper limit of the OP: a line parallel to the Frankfurt plane passing through the Basion (Ba), which is termed Horizontal 1 (H1);
-
•
Lower limit of the OP: a line parallel to the Frankfurt plane passing through the most anterior-inferior border of the third cervical vertebra (C3), which is termed Horizontal 2 (H2);
Fig. 3.
Demarcation of the regions on a CBCT image.
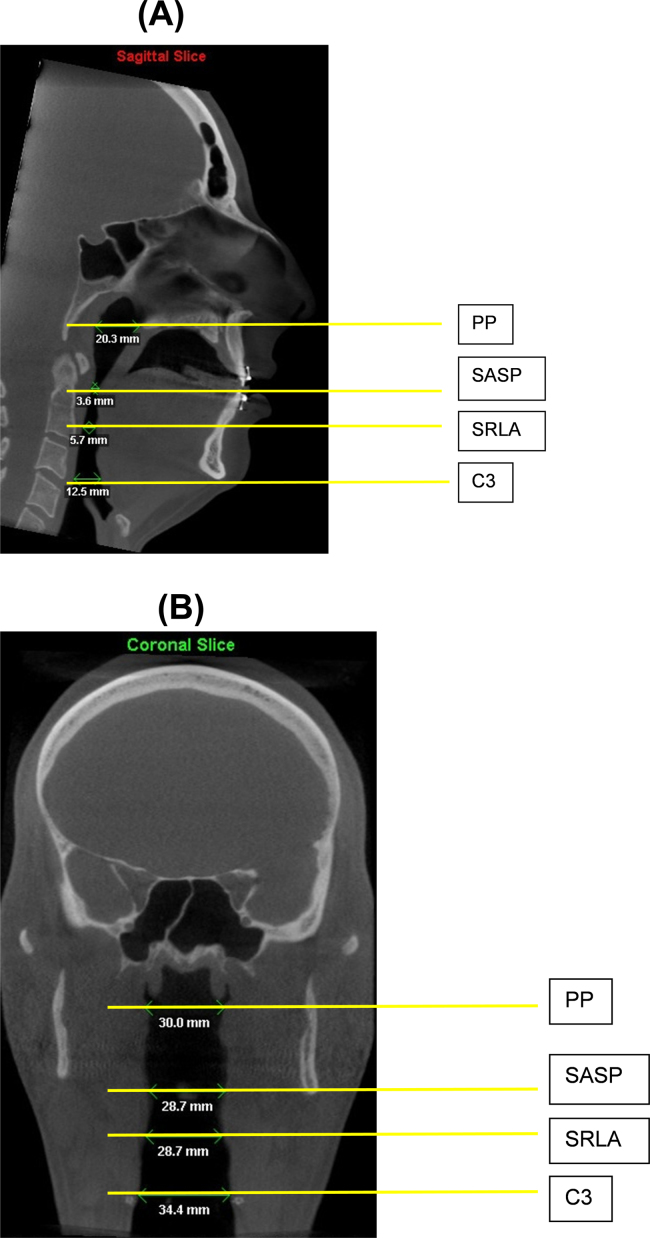
The linear measurements were also evaluated in two dimensions, both in the sagittal plane (anteroposterior measurement) and in the coronal plane (lateral measurement). For this purpose, the following points and lines were used according to [7] (Fig. 4A, B):
-
•
PP line: continuation of the palatal plane
-
•
SASP line: smallest area of the soft palate
-
•
SRLA line: smallest retrolingual area
-
•
C3 line: a line passing through the inferior border of the C3
Fig. 4.
(A) Two-dimensional demarcation of the regions in on a CBCT image: sagittal plane. (B) Two-dimensional demarcation of the regions on a CBCT.
3. Results
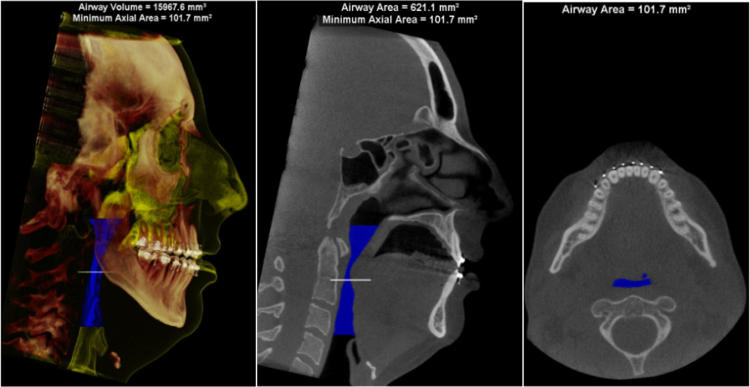
The duration of the preoperative orthodontic treatment was 18 months and the patient was treated with CPAP during this period. Fig. 5 shows the facial condition after orthodontic treatment and before MMA surgery. After the completion of orthodontic treatment, the patient exhibited the following characteristics: BMI=24.4 kg/m2, AHI=25.2/h, ESS=11, TV=15967.6 mm³, and SA=101.7 mm2 (Table 1, Table 2, Fig. 6).
Fig. 5.
Facial features after orthodontic treatment.
Table 1.
Anthropometric and polysomnography variables.
| Baseline | Post-orthodontics | 6 months post-surgery | 12 months post-surgery | ||
|---|---|---|---|---|---|
| Anthropometry | |||||
| BMI | 24.9 | 24.4 | 24.1 | 25.2 | |
| Polysomnography | |||||
| TST | 309.5 | 412.5 | 367 | 308.0 | |
| % SE | 77.1 | 90.9 | 93.6 | 71.0 | |
| % N1 | 4.8 | 15.2 | 3.1 | 9.3 | |
| % N2 | 73.5 | 37.8 | 51.4 | 61.9 | |
| % N3 | 11.6 | 18.4 | 27.7 | 7.1 | |
| % REM | 10.1 | 28.6 | 17.8 | 21.8 | |
| AI | 15.5 | 24.2 | 22 | 16.2 | |
| AHI | 30.8 | 25.2 | 6.7 | 0.2 | |
| Baseline saturation | 96.3 | 95.8 | 95.6 | 94.2 | |
| Mean saturation | 95.5 | 95.1 | 94.9 | 93.7 | |
| Minimum saturation | 90.0 | 86.0 | 89 | 88 | |
TST – Total sleep time, SE – Sleep efficiency, REM – Rapid eye movement, AI – Arousal index, AHI – Apnea-hypopnea index.
Table 2.
Tomographic variables.
| Variables | Baseline | Post-Orthodontics | 12 months post-surgery |
|---|---|---|---|
| Total volume (mm3) | 19741.9 | 15967.6 | 24075.2 |
| Smallest area (mm2) | 169.9 | 101.7 | 266.3 |
| PP Sagittal (mm) | 22.4 | 20.3 | 24.6 |
| SASP Sagittal (mm) | 5.4 | 3.6 | 8.8 |
| SRLA Sagittal (mm) | 9.3 | 5.7 | 11.5 |
| C3 Sagittal (mm) | 16.9 | 12.5 | 15.9 |
| PP Coronal (mm) | 41.9 | 21.4 | 30 |
| SASP Coronal (mm) | 23.7 | 24.2 | 28.7 |
| SRLA Coronal (mm) | 26.2 | 10 | 28.7 |
| C3 Coronal (mm) | 35.5 | 24.6 | 34.4 |
PP line: continuation of the palatal plane, SASP line: smallest area of the soft palate, SRLA line: smallest retrolingual area, C3 line: line passing through the inferior border of the C3.
Fig. 6.
Post-orthodontic treatment (pre-surgery) tomography.
In the MMA surgery and advancement genioplasty, the following bone movements were performed: maxillary anterior repositioning of 7.0 mm, maxillary superior repositioning of 3.0 mm, mandibular advancement with counterclockwise rotation of 6.0 mm, and anteroinferior chin repositioning of 3.0 mm, in addition to a turbinectomy and septoplasty.
Bilateral sagittal split osteotomy of the mandible (BSSO) It was held and there was neuropraxia the inferior alveolar nerve with lip-mental paresthesia around 6 months, returning after this period.
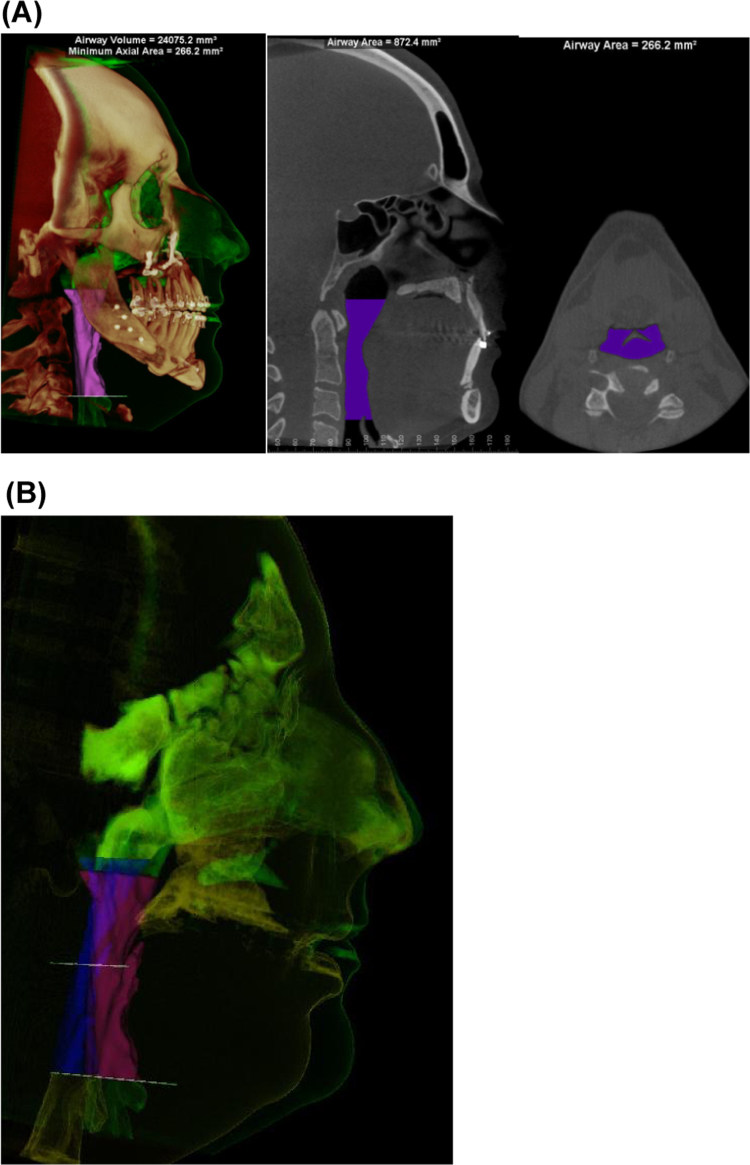
Six months after the surgery, the patient exhibited the following characteristics: BMI=24.0 kg/m2, AHI=6.7/h, and ESS=5 (Table 1). Twelve months after the MMA surgery, the patient exhibited the following characteristics: BMI=25.2 kg/m2, AHI=0.2/h, ESS=4, TV=24075.2 mm³, and SA=266.3 mm2 (Table 1, Table 2, Fig. 6). Fig. 7 shows the facial aspect of the patient one year after the surgery, and Fig. 8 shows the volume and area on the CBCT image one year after surgery. Visual analog scale of 10 cm=1 – held by his wife.
Fig. 7.

Facial features after surgery.
Fig. 8.
(A) Post-surgery tomography. (B) Pre- and post-surgery image overlay.
When the preoperative tomographic images and the images obtained 12 months post-surgery were compared, a 56% increase in the TV (15967.6 mm³ to 24075.2 mm³) and a 162% increase in the SA (101.7 mm2 to 266.3 mm2), which is now located in the HP rather than in the OP (preoperative CBCT), were observed (Table 2).
When the baseline tomographic images and the 12-month postoperative images were compared, a TV increase of 21.95% in relation to the baseline CBCT image (19741.9 mm³ to 24075.2 mm³) and an SA increase of 56.75% (169.9 mm2 - OP to 266.3 mm2 - HP) were observed (Table 2). The linear measurements are shown in Table 3.
Table 3.
Linear measurements.
| Variables | Baseline | Post-Orthodontics | 12 months post-surgery |
|---|---|---|---|
| PP Sagittal (mm) | 22.4 | 20.3 | 24.6 |
| SASP Sagittal (mm) | 5.4 | 3.6 | 8.8 |
| SRLA Sagittal (mm) | 9.3 | 5.7 | 11.5 |
| C3 Sagittal (mm) | 16.9 | 12.5 | 15.9 |
| PP Coronal (mm) | 41.9 | 21.4 | 30 |
| SASP Coronal (mm) | 23.7 | 24.2 | 28.7 |
| SRLA Coronal (mm) | 26.2 | 10 | 28.7 |
| C3 Coronal (mm) | 35.5 | 24.6 | 34.4 |
PP line: continuation of the palatal plane, SASP line: smallest area of the soft palate, SRLA line: smallest retrolingual area, C3 line: line passing through the inferior border of the C3.
4. Discussion
CPAP therapy has been considered the gold standard for treatment of OSAS in adults. However, despite the success potential of CPAP, non-adherence by patients remains a major problem [9]. Some publications have been critical regarding surgeries and their results [10]. Elshaug et al. (2007) [10] proposed that for surgical treatments with success rates based on the AHI, the results should be between 5 and 10.
The currently accepted surgical success criteria of a 50% reduction of the respiratory disturbance index (RDI) and less than 20 events per hour follows the same logic used in the criteria established for the use of CPAP [11]. Vicini et al. (2010) reported a significant reduction (p<0.0001) in the AHI, from 49.33±16.85 to 4.44±5.76, after MMA surgery (n=61) [12].
Young patient, skinny, AHI not as high, not too low minimal oxyhemoglobin saturation and significant craniofacial anomaly, has been reported in the literature as predictors of success for the AMM surgery [18]. The patient reported here underwent MMA surgery was 29 years old with a body mass index (BMI) of 24.93 kg/m2, AHI of 25.2/h and was carrying bi-retrusion maxilomandibular. These characteristics presented by the patient in question were in accordance with predictors of success/cure with literature.
MMA surgeries have been extensively studied and accepted as a successful therapy for the treatment of patients with OSAS [13], and bone repositioning has been found to be stable over the long term [14]. According to Riley et al. (2000), maxillomandibular bone advancements of approximately 10 mm increase the size of the OP both in the anteroposterior and laterolateral directions [15]. Moreover, Holty and Guilleminault (2010) showed that maxillary advancement of approximately 8.4 mm (±2.8 mm) led to a success rate of less than 80%, while maxillary advancement of approximately 9.9 mm (±1.3 mm) increased the success rate to more than 80% [16].
In this case report, although the planned and obtained maxillomandibular advancement was 7.0 mm, in addition to the chin advancement of 3.0 mm (these movements were limited by the patient's facial aesthetics), the results after 12 months showed an increase in the dimensions of the OP both in the laterolateral and anteroposterior directions. The TV of the airway and the SA were increased and remained stable for a period of one year. Postoperative CBCT images showed that the volume of the section of the pharynx evaluated increased by approximately 56%, which is directly related to the maxillomandibular advancement of 7.0 mm.
Raffaini and Pisani (2013) [17] obtained a mean increase of 56% in the TV of the analyzed segment and a 112% increase in the SA in patients undergoing MMA with mean mandibular advancement of 10 mm. Our study also observed a TV increase of 56%, and the SA was increased by 162%. Both studies considered the same segment extending from the palatal plane to the inferior border of the C3.
It should be noted that the size and shape of the airway are extremely variable, depending on the position of the head and the breathing phase (expiration or inspiration) [18], and there are no standards to which the present airway volume result can be compared. However, a comparison of the pre and postoperative volumes demonstrates the changes after the MMA and chin advancement surgery.
Another interesting finding is that the linear measurements in the sagittal plane (PP, SASP, and SRLA) and in the coronal plane (SASP and SRLA) of the airway increased when the baseline and preoperative measurements were compared with the postoperative measurements. It is also worth noting that all linear and volumetric measurements decreased between the baseline and preoperative/post-orthodontic treatment CBCT examinations, except for the SASP in the coronal plane. These differences occur because the placement of the teeth in the correct position by the orthodontic treatment, i.e., eliminating dental compensation (inclinations that the teeth seek in an attempt to mask the skeletal deformity), results in a reduction of the intraoral space, and thus a posterior repositioning of the tongue occurs, which further decreases the oropharyngeal airspace. This dental inclination correction treatment before surgery allows greater bone advancement during the surgery, which alters the facial aesthetics of these patients. If orthodontic treatments were not performed, the teeth would have inclinations that would push the lips forward, which would limit bone advancement because the patients could have biprotrusion, which would change the facial appearance.
Another interesting point is that the airway patency is not preserved when the lateral pharyngeal dimensions are decreased [19]. In this case report, an increase in the laterolateral pharyngeal dimensions was produced. When referring to the success rate of a surgical intervention, the follow-up time should be considered. Several studies have only considered short long-term follow-up times (three to six months) [20], [21]. In contrast, Li et al. (2000) demonstrated that MMA is stable after 50.7±31.9 months regardless of whether it is performed alone or with other surgeries [22]. In the present report, a 12-month follow-up is presented, and stability of the polysomnographic and dimensional parameters of the airway was maintained over this period.
The patient in the present report had severe OSAS and was treated with MMA and chin advancement surgery. Although the bone movements did not obtain the maxillomandibular advancement values described in the literature for the successful treatment of OSAS, we observed a significant increase in the airway volume, in the segment that was studied, the SA, and in the anteroposterior and lateral linear measurements. This procedure provided an effective treatment for severe OSAS with a decrease in the AHI from 30.8 to 0.2 and a consequent reduction in daytime sleepiness.
Acknowledgement
The authors thank the Associação Fundo de Apoio a Pesquisa (AFIP) for financial support.
Footnotes
Peer review under responsibility of Brazilian Association of Sleep.
Peer review under responsibility of Brazilian Association of Sleep.
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.slsci.2016.07.005.
Appendix A. Supplementary material
Fig. S1.
The core spectra of the chips’ surfaces after APTES and GO-COOH coating.
.
References
- 1.Gottlieb D.J., Whitney C.W., Bonekat W.H., Iber C., James G.D., Lebowitz M. Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study. Am. J. Respir. Crit. Care Med. 1999;159:502. doi: 10.1164/ajrccm.159.2.9804051. [DOI] [PubMed] [Google Scholar]
- 2.Weaver T.E., Grunstein R.R. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc. Am. Thorac. Soc. 2008;5:173–178. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuo P.C., West R.A., Bloomquist D.S., McNeil R.W. The effect of mandibular osteotomy in three patients with hypersomnia sleep apnea. Oral. Surg. Oral. MEd. Oral. Pathol. 1979;48:385–392. doi: 10.1016/0030-4220(79)90063-x. [DOI] [PubMed] [Google Scholar]
- 4.Boyd S.B., Walters A.S., Waite P., Harding S.M., Song Y. Long-term effectiveness and safety of maxillomandibular advancement for treatment of obstructive sleep apnea. J. Clin. Sleep Med. 2015;11:699–708. doi: 10.5664/jcsm.4838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johns F.R., Strollo P.J., Buckley M., Constantino J. The influence of craniofacial structure on obstructive sleep apnea in young adults. J. Oral. Maxillofac. Surg. 1998;56:596–602. doi: 10.1016/s0278-2391(98)90459-1. [DOI] [PubMed] [Google Scholar]
- 6.Schwab R.J., Gefter W.B., Hoffman E.A., Gupta K.B., Pack A.I. Dynamic upper airway imaging during awake respiration in normal subjects and patients with sleep disordered breathing. Am. Rev. Respir. Dis. 1993;148:1385–1400. doi: 10.1164/ajrccm/148.5.1385. [DOI] [PubMed] [Google Scholar]
- 7.Fairburn S.C., Waite P.D., Vilos G., Harding S.M., Bernreuter W., Cure J. Three-dimensional changes in upper airways of patients with obstructive sleep apnea following maxillomandibular advancement. J. Oral. Maxillofac. Surg. 2007;65:6–12. doi: 10.1016/j.joms.2005.11.119. [DOI] [PubMed] [Google Scholar]
- 8.El A.S., El H., Palomo J.M., Baur D.A. A 3-dimensional airway analysis of an obstructive sleep apnea surgical correction with cone beam computed tomography. J. Oral. Maxillofac. Surg. 2011;69:2424–2436. doi: 10.1016/j.joms.2010.11.046. [DOI] [PubMed] [Google Scholar]
- 9.Iber C.A.-I.S., Chesson A.L., Jr., Quan S.F. American Academy of Sleep Medicine,; Westchester: 2007. The AAM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. [Google Scholar]
- 10.Edmonds J.C., Yang H., King T.S., Sawyer D.A., Rizzo A., Sawyer A.M. Claustrophobic tendencies and continuous positive airway pressure therapy non-adherence in adults with obstructive sleep apnea. Heart Lung. 2015;44:100–106. doi: 10.1016/j.hrtlng.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elshaug A.G., Moss J.R., Southcott A.M., Hiller J.E. Redefining success in airway surgery for obstructive sleep apnea: a meta analysis and synthesis of the evidence. Sleep. 2007;30:461–467. doi: 10.1093/sleep/30.4.461. [DOI] [PubMed] [Google Scholar]
- 12.Kasey K.L. Maxillomandibular advancement for obstructive sleep apnea. J. Oral. Maxillofac. Surg. 2011;69:687–694. doi: 10.1016/j.joms.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 13.Vicini C., Dallan I., Campanini A., De Vito A., Barbanti F., Giorgiomarrano G. Surgery vs ventilation in adult severe obstructive sleep apnea syndrome. Am. J. Otolaryngol. 2010;31:14–20. doi: 10.1016/j.amjoto.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Goodday R. Diagnosis, treatment planning, and surgical correction of obstructive sleep apnea. J. Oral. Maxillofac. Surg. 2009;67:2183–2196. doi: 10.1016/j.joms.2009.03.035. [DOI] [PubMed] [Google Scholar]
- 15.Nimkarn Y., Miles P.G., Waite P.D. Maxillomandibular advancement surgery in obstructive sleep apnea syndrome patients: long-term surgical stability. J. Oral. Maxillofac. Surg. 1995;53:1414–1418. doi: 10.1016/0278-2391(95)90667-3. [DOI] [PubMed] [Google Scholar]
- 16.Riley R.W., Powell N.B., Li K.K., Troell R.J., Guilleminault C. Surgery and obstructive sleep apnea: long-term clinical outcomes. Otolaryngol. Head. Neck Surg. 2000;122:415–421. doi: 10.1016/S0194-5998(00)70058-1. [DOI] [PubMed] [Google Scholar]
- 17.Holty J.E., Guilleminault C. Surgical options for the treatment of obstructive sleep apnea. Med. Clin. North Am. 2010;94:479–515. doi: 10.1016/j.mcna.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Raffaini M., Pisani C. Clinical and cone-beam computed tomography evaluation of the three-dimensional increase in pharyngeal airway space following maxillo-mandibular rotation-advancement for Class II-correction in patients without sleep apnoea (OSA) J. Craniomaxillofac. Surg. 2013;41:552–557. doi: 10.1016/j.jcms.2012.11.022. [DOI] [PubMed] [Google Scholar]
- 19.Yildirim N., Fitzpatrick M.F., Whyte K.F., Jalleh R., Wightman A.J., Douglas N.J. The effect of posture on upper airway dimensions in normal subjects and in patients with the sleep apnea/hypopnea syndrome. Am. Rev. Respir. Dis. 1991;144:845–847. doi: 10.1164/ajrccm/144.4.845. [DOI] [PubMed] [Google Scholar]
- 20.Fogel R.B., Malhotra A., Dalagiorgou G., Robinson M.K., Jakab M., Kikinis R. Anatomic and physiologic predictors of apnea severity in morbidly obese subjects. Sleep. 2003;26:150–155. doi: 10.1093/sleep/26.2.150. [DOI] [PubMed] [Google Scholar]
- 21.Conradt R., Hochban W., Heitmann J., Brandenburg U., Cassel W., Penzel T. Sleep fragmentation and daytime vigilance in patients with OSA treated by surgical maxillomandibular advancement compared to CPAP therapy. J. Sleep Res. 1998;7:217–223. doi: 10.1046/j.1365-2869.1998.00116.x. [DOI] [PubMed] [Google Scholar]
- 22.Gregg J.M., Zedalis D., Howard C.W., Boyle R.P., Prussin A.J. Surgical alternatives for treatment of obstructive sleep apnoea: review and case series. Ann. R. Austral. Coll. Dent. Surg. 2000;15:181–184. [PubMed] [Google Scholar]