Abstract
Insomnia is a sleep disorder in which the subject encounters problems in sleeping. The aim of this study is to identify insomnia events from normal or effected person using time frequency analysis of PSD approach applied on EEG signals using channel ROC-LOC. In this research article, attributes and waveform of EEG signals of Human being are examined. The aim of this study is to draw the result in the form of signal spectral analysis of the changes in the domain of different stages of sleep. The analysis and calculation is performed in all stages of sleep of PSD of each EEG segment. Results indicate the possibility of recognizing insomnia events based on delta, theta, alpha and beta segments of EEG signals.
Abbreviations: EEG, Electro Encephalogram; ROC-LOC, Right of Central & Left of Central; PSD, Power spectrum Density
Keywords: Classification of Insomnia, Analysis of EEG Signal, Estimation of PSD
1. Introduction
The complexity of the human brain is one of the most well documented fields of academic study. Nowadays multiple technologies exist to record brain wave patterns, Electroencephalography being one of them. Through Electroencephalogram based signals, a better understanding of the complex inner mechanisms and their association with psychological and psychiatric disorders can be established [1].
Insomnia or sleeplessness is a sleep disorder in which there is an inability to fall asleep or to stay asleep as long as desired. Insomnia is characterized by:
-
1.
Frequently waking up during the night.
-
2.
Waking up early.
-
3.
General feeling of exhaustion.
-
4.
Deficit concentration prowess.
-
5.
Feeling slow and not-refreshed during the day.
Insomnia cases have seen a rapid climb over the past few years and coupled with pain and fatigue is one of the most common disorders in urban societies. Even though cases of insomnia are at alarming levels, awareness about it is at abysmal levels, both in victims and doctors. Compounding the issue is the fact that there are no widely accepted forms standard treatments [2].
DSM-5 criteria for insomnia contain the following:[13].
-
•
Predominant grievance of dissatisfaction with sleep quantity or quality, associated with one (or more) of the following symptoms:
-
•
Difficulty initiating sleep. (In children, this may manifest as difficulty initiating sleep without caregiver intervention.)
-
•
Difficulty maintaining sleep, characterized by frequent awakenings or problems returning to sleep after awakenings. (In children, this may manifest as difficulty returning to sleep without caregiver intervention.)
-
•
Early-morning awakening with inability to return to sleep.
General sleepless nights happen to everyone, leading to the misappropriation that insomnia is a natural reaction of an organism to tension or noise. However, insomnia is not symptom of other disorders but secondary to other medical conditions. The effects generated due to insomnia are:
-
1.
Daytime sleepiness.
-
2.
Irritable mood.
-
3.
Increased possibility of workplace accidents.
-
4.
Inability to effectively operate machinery.
-
5.
Lapse in concentration while driving.
2. Classification of insomnia
2.1. According to etiology
2.1.1. Insomnia disorder
When insomnia has no recognized physical (pain), affecting (depression/anxiety), Environmental (noise at night) or substance (drugs) cause, the condition is called Insomnia Disorder.
2.1.2. Comorbid Insomnia
This is when the victim has sleep problems because of something else, such as a fitness condition like asthma, depression, arthritis, cancer or stomachache; pain; drug being taken; or a material being used, like alcohol [3].
2.2. According to sleep pattern
2.2.1. Sleep-onset insomnia
When the victim takes a long time to get to sleep, but can sleep through the dark once sleep starts.
2.2.2. Sleep-maintenance insomnia
When sufferer wakes regularly during the night and sleep is fragmented [4].
2.3. According to duration
2.3.1. Transient insomnia
Durable less than a week. This is the most common and extensive form among the population.
2.3.2. Acute insomnia
Lasting between one and four weeks. It is connected to stress factors, but more longer-lasting than for transitory insomnia.
2.3.3. Chronic insomnia
Lasts for four or more weeks and may be due to essentially causes in the organism, eg a long-term physical or psychiatric sickness or it may have no obvious underlying cause [2].
3. Subject details and recorded data
Total twenty five volunteer subjects’ were selected for this study [5]. Nine subjects were suffering from the sleep disorder of insomnia and sixteen subjects were referred to as the normal group. The subject's details like gender, age, sleep duration of each stage etc. were taken. The subject demographics of both groups are shown in Table 1, Table 2 Respectively.
Table 1.
Normal person recorded data.
| S. NO. | SUBJECT | SLEEP TIME DURATION OF S0 SLEEP STAGE | SLEEP TIME DURATION OF S1 SLEEP STAGE | SLEEP TIME DURATION OF S2 SLEEP STAGE | SLEEP TIME DURATION OF S3 SLEEP STAGE | SLEEP TIME DURATION OF S4 SLEEP STAGE | SLEEP TIME DURATION OF REM SLEEP STAGE | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| G | P ID | A | START TIME | END TIME | START TIME | END TIME | START TIME | END TIME | START TIME | END TIME | START TIME | END TIME | START TIME | END TIME | |
| 1 | F | N1 | 37 | 22:09:33 | 22:10:33 | 06:19:33 | 06:20:33 | 23:29:33 | 23:30:33 | 00:35:03 | 00:36:03 | 22:40:33 | 22:41:33 | 23:36:33 | 23:37:33 |
| 2 | M | N2 | 34 | 22:19:06 | 22:20:06 | 00:44:06 | 00:45:06 | 23:20:06 | 23:21:06 | 22:47:06 | 22:48:06 | 22:52:06 | 22:53:06 | 00:20:36 | 00:21:36 |
| 3 | F | N3 | 35 | 23:10:42 | 23:11:42 | 04:57:42 | 04:58:42 | 23:55:12 | 23:56:12 | 23:20:42 | 23:21:42 | 23:25:12 | 23:26:12 | 01:00:42 | 01:01:42 |
| 4 | F | N4 | 25 | 22:36:37 | 22:37:37 | 06:41:37 | 06:42:37 | 23:54:07 | 23:55:07 | 03:33:07 | 03:34:07 | 00:29:07 | 00:30:07 | 01:07:37 | 01:0/8:37 |
| 5 | F | N5 | 35 | 22:49:48 | 22:50:48 | 22:53:18 | 22:54:18 | 00:01:18 | 00:02:18 | 00:52:48 | 00:53:48 | 01:05:48 | 01:06:48 | 01:18:48 | 01:19:48 |
| 6 | M | N6 | 31 | 22:38:39 | 22:39:39 | NA | NA | 23:03:39 | 23:04:39 | 01:03:39 | 01:04:39 | 00:34:39 | 00:35:39 | 23:58:09 | 23:59:09 |
| 7 | M | N7 | 31 | 22:21:11 | 22:22:11 | 06:27:41 | 06:28:41 | 00:00:41 | 00:01:41 | 03:21:41 | 03:22:41 | 23:04:11 | 23:05:11 | 00:31:11 | 00:32:11 |
| 8 | F | N8 | 42 | 22:17:41 | 22:18:41 | 05:58:41 | 05:59:41 | 00:00:41 | 00:01:41 | 22:56:41 | 22:57:41 | 23:06:41 | 23:07:41 | 00:23:41 | 00:24:41 |
| 9 | M | N9 | 31 | 22:56:13 | 22:57:13 | 23:15:43 | 23:16:43 | 23:43:13 | 23:44:13 | 23:49:13 | 23:50:13 | 23:52:43 | 23:53:43 | 00:38:43 | 00:39:43 |
| 10 | M | N10 | 23 | 23:24:52 | 23:25:52 | NA | NA | 23:58:22 | 23:59:22 | 01:34:22 | 01:35:22 | 00:04:52 | 00:05:52 | 01:12:52 | 01:13:52 |
| 11 | F | N11 | 28 | 22:37:16 | 22:38:16 | NA | NA | 23:08:46 | 23:09:46 | 00:38:16 | 00:39:16 | 23:36:16 | 23:37:16 | 00:17:16 | 00:18:16 |
| 12 | M | N12 | 29 | 15:14:22 | 15:15:22 | NA | NA | 15:30:52 | 15:31:52 | 15:38:52 | 15:39:52 | 15:55:22 | 15:56:22 | 16:34:22 | 16:35:22 |
| 13 | F | N13 | 24 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 14 | F | N14 | 35 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 15 | M | N15 | 34 | 22:00:22 | 22:01:22 | 22:14:52 | 22:15:52 | 22:28:52 | 22:29:52 | 22:34:52 | 22:35:52 | NA | NA | 23:46:22 | 23:47:22 |
| 16 | F | N16 | 41 | 22:35:17 | 22:36:17 | NA | NA | 23:58:17 | 23:59:17 | NA | NA | NA | NA | 23:50:17 | 23:51:17 |
Table 2.
Insomnia patient recorded data.
| SL NO. | PATIENT DETAILS | SLEEP TIME DURATION OF S0 SLEEP STAGE | SLEEP TIME DURATION OF S1 SLEEP STAGE | SLEEP TIME DURATION OF S2 SLEEP STAGE | SLEEP TIME DURATION OF S3 SLEEP STAGE | SLEEP TIME DURATION OF S4 SLEEP STAGE | SLEEP TIME DURATION OF REM SLEEP STAGE | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ID | GEN | AGE (Yrs) | START TIME | END TIME | START TIME | END TIME | START TIME | END TIME | START TIME | END TIME | START TIME | END TIME | START TIME | END TIME | |
| 1 | INS1 | M | 54 | 22:32:28 | 22:33:28 | 23:00:28 | 23:01:28 | 23:12:28 | 23:33:28 | 23:45:28 | 23:46:28 | N/A | N/A | 00:23:28 | 00:24:28 |
| 2 | INS2 | F | 58 | 18:27:38 | 18:28:38 | N/A | N/A | 23:24:38 | 23:25:38 | 00:17:38 | 00:18:38 | N/A | N/A | 00:54:38 | 00:55:38 |
| 3 | INS3 | M | 82 | 22:50:12 | 22:51:12 | 23:57:12 | 23:58:12 | 01:20:12 | 01:21:12 | 02:50:12 | 02:51:12 | 03:10:12 | 03:11:12 | 03:56:12 | 03:57:12 |
| 4 | INS4 | F | 58 | 21:36:34 | 21:37:34 | N/A | N/A | 01:46:34 | 01:47:34 | 22:36:34 | 22:37:34 | 23:40:34 | 23:41:34 | 22:50:34 | 22:51:34 |
| 5 | INS5 | F | 59 | 18:01:48 | 18:02:48 | 23:30:48 | 23:31:48 | 23:33:48 | 23:34:48 | 05:56:48 | 01:03:48 | 05:57:48 | 00:11:48 | 01:03:48 | 01:04:48 |
| 6 | INS6 | F | 54 | 23:40:47 | 23:41:47 | 01:00:47 | 01:01:47 | 00:00:47 | 00:01:47 | 01:36:47 | 01:37:47 | 00:10:47 | 00:11:47 | 00:57:47 | 00:58:47 |
| 7 | INS7 | F | 47 | 20:00:14 | 20:01:14 | 05:51:14 | 05:52:14 | 23:28:14 | 23:29:14 | 23:55:14 | 23:56:14 | 22:18:14 | 22:19:14 | 23:17:14 | 23:18:14 |
| 8 | INS8 | M | 64 | 22:44:34 | 22:45:34 | 23:38:34 | 23:39:34 | 02:21:34 | 02:22:34 | 05:09:34 | 05:10:34 | N/A | N/A | 02:09:34 | 02:10:34 |
| 9 | INS9 | M | 72 | 22:37:44 | 22:38:44 | 23:15:44 | 23:16:44 | 23:21:44 | 23:22:44 | 23:39:44 | 23:40:44 | 02:38:44 | 02:39:44 | 02:40:44 | 02:41:44 |
4. Analysis of EEG signal
4.1. Load EEG data
Load EEG Signals from physionet.org [5] in MATLAB workspace and the name of various signals Load (matName) command gives a signal in workspace named as ‘val’.
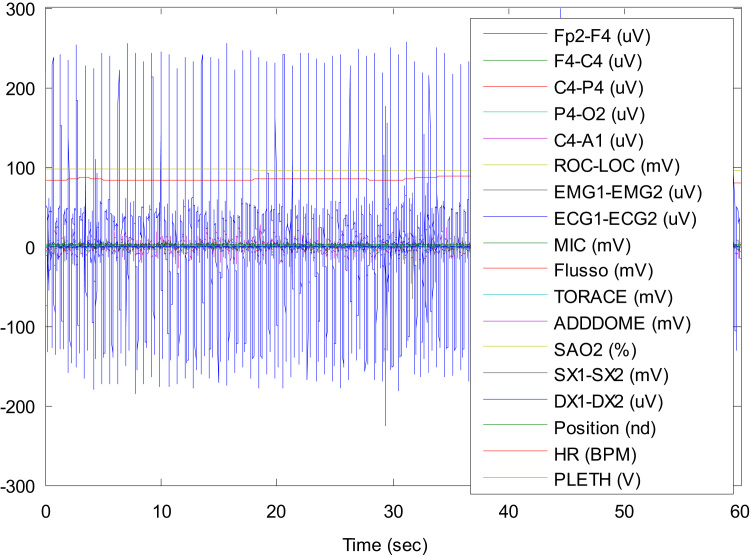
Fig. 1 shows the full signals and is on time basis. The signal is of one minute [6].
Fig. 1.
Complete EEG signal of S0 stage.
4.2. Extracting EEG signals
As discussed in the previous topic, we took the EEG signal where all the channels are interwoven in a single signal. Now from that Fig. 1 we extracted different common channels of all insomnia victims:
ROC-LOC, C4-P4, C4-A1, F4-C4, ECG1-ECG2, EMG1-EMG2, P4-O2 [6], [7].
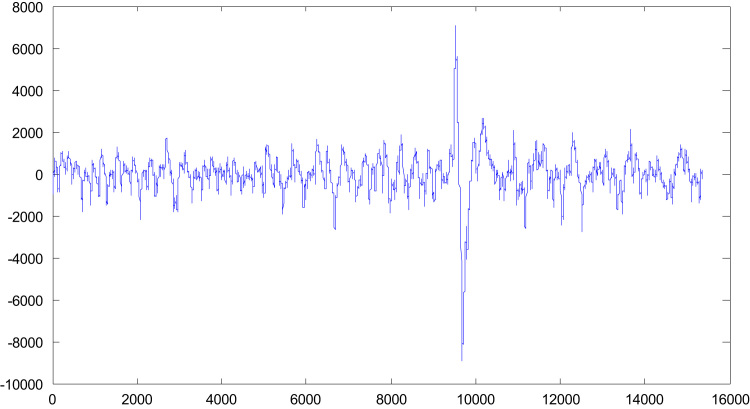
The channels shown here are C4-A1 and ROC-LOC. Fig. 2 is based on frequency basis. Here the sampling frequency is 256 Hz.
Fig. 2.
Different extracted signals on frequency basis.
4.3. Extracting stage of sleep from EEG signal
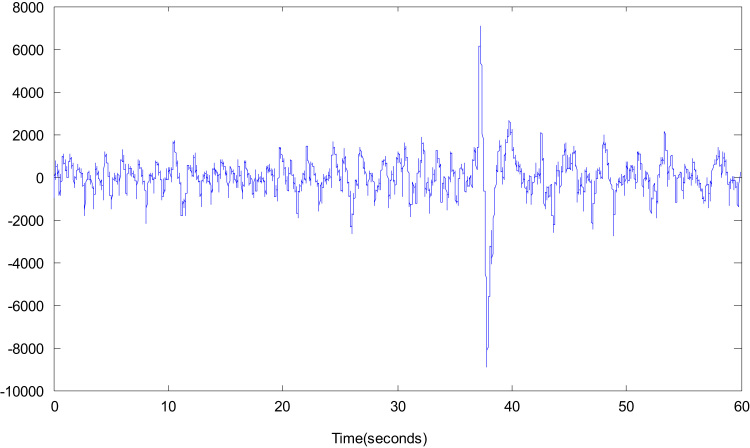
Now the Fig. 3 is based on time respect. The duration of clipped signal is 1 min (60 s) consisting of EEG signal of respective channel for S0 sleep stage.
Fig. 3.
Extracted different signals on time basis for S0 sleep stage.
4.4. Filtering of EEG signals
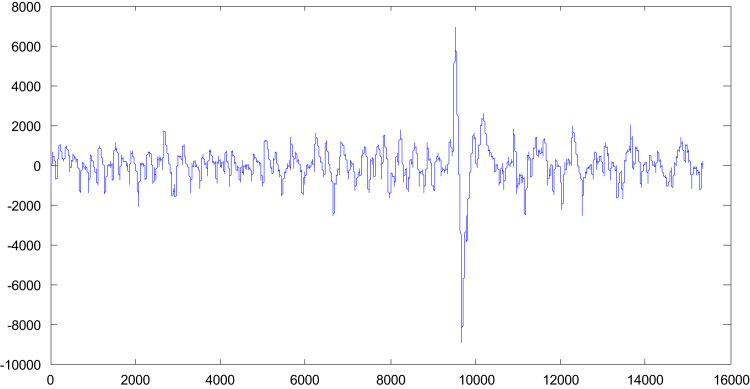
Now each clipped signal is preprocessed and then passed through the Hanning window low pass filter for removing the high frequency components that eventually indicate noise because major proportion of EEG signals are limited within the range of 25 Hz. Hence, the filter based in FIR filter design of order 200 with cut off frequency of 25 Hz with shape of hanning window is designed for low pass filtering of each sleep sage [6], [8].
The Fig. 4 is showing filtered signals for different channel.
Fig. 4.
Extracted different filtered signals for S0 sleep stage.
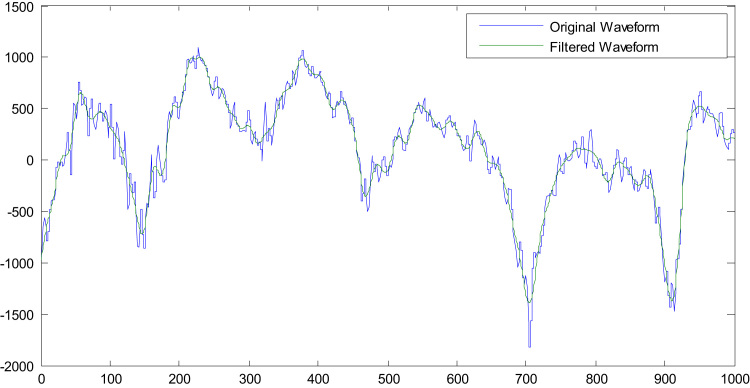
4.5. Comparison between original signal and filtered signal
The differences between original and filtered waveform is shown in Fig. 5. The MATLAB function ‘filtfilt’, which is a zero-phase filtering, is used as the filtering method [6]. Now both the original and filtered waveform is cut in 1:1000 ratios which give the detail on the minute differences of both signals.
Fig. 5.
Minute differences between original and filtered waveform.
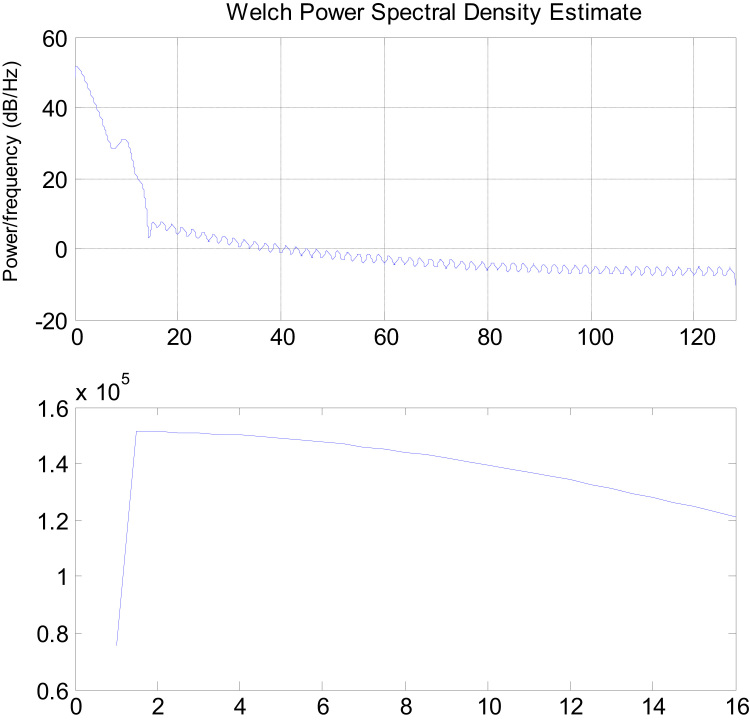
4.6. Estimation of power spectral density
An improved estimator of the PSD is the one proposed by Welch. The method consists of dividing the time series data into (possibly overlapping) segments, computing a modified periodogram of each segment, and then averaging the PSD estimates. The result is Welch's PSD estimate. Welch's method is implemented in the toolbox by the Welch method. Since PSD gives signal power with respect to the frequency spectrum, we require specifying the number of frequency slots to distribute the spectral power. It is called as number of FFT points (NFFT). The Fig. 6 is showing power spectral density (PSD) of different channels [6], [9], [12].
Fig. 6.
Figure showing PSD of different channels.
5. Result and discussion
Normalized power (P norm) of normal cases having no symptoms of sleep is analyzed and compared with pathological cases during S0 stage [10], [11]. Normalized power indicates the percentage of a particular EEG activity out of complete power. So it is found that it gives a better indication of measurements of detection of features instead of taking average power of particular EEG activity. We took 16 normal cases and 9 insomnia cases and then compared the results [6].
According to Table 3, delta activity normalized power for normal cases is found in range of 0.58–0.76 and for insomnia cases it is found in range of 0.81–0.89, hence we can see that normalized power of normal case is low as compared to insomnia victims.
Table 3.
Normalized power of Delta Activity.
| Stage S0 | Normal 1 | Normal 2 | Normal 3 | Insomnia 1 | Insomnia 5 | Insomnia 6 |
|---|---|---|---|---|---|---|
| P_delta (Normalized) | 0.58457 | 0.766656 | 0.75848 | 0.8999 | 0.81859 | 0.8732 |
 |
 |
|||||
Similarly for normalized power of theta activity, Pnorm for normal cases is high i.e. 0.17–0.28 and for insomnia case the range is from 0.078 to 0.16 which low (see Table 4).
Table 4.
Normalized power of Theta Activity.
| Stage S0 | Normal 1 | Normal 2 | Normal 3 | Insomnia 1 | Insomnia 6 |
|---|---|---|---|---|---|
| P_theta (Normalized) | 0.28546 | 0.17031 | 0.19047 | 0.078008 | 0.11943 |
 |
 |
||||
For the alpha activity, the normalized power for normal cases is in the range of 0.04–0.12 which is high while for the insomnia cases the range is low i.e. 0.006–0.02 (see Table 5).
Table 5.
Normalized power of Alpha Activity.
| Stage S0 | Normal 1 | Normal 2 | Normal 3 | Insomnia 1 | Insomnia 5 | Insomnia 6 |
|---|---|---|---|---|---|---|
| P_alpha (Normalized) | 0.12228 | 0.058187 | 0.04643 | 0.02153 | 0.01366 | 0.0066697 |
 |
 |
|||||
According to Table 6, normalized power of beta activity for normal cases are found in range 0.004–0.007 which is high, on the other hand in insomnia cases the range is 0.0005–0.0007 which is quite low as compared to normal cases.
Table 6.
Normalized power of Beta Activity.
| Stage S0 | Normal 1 | Normal 2 | Normal 3 | Insomnia 1 | Insomnia 5 | Insomnia 6 |
|---|---|---|---|---|---|---|
| P_beta (Normalized) | 0.0076992 | 0.004942 | 0.0046171 | 0.00056601 | 0.00067993 | 0.00070318 |
 |
 |
|||||
Table 4, Table 5, Table 6 indicate that insomnia patient have low normalized power for respectively theta, alpha and beta waves of EEG Signal. Table 3 indicate that insomnia patient have high normalized power for Delta wave of EEG signal.
6. Conclusion
We presented EEG Signals comparison between normal individuals and insomnia victims on basis of PSD of using ROC-LOC channel and defined the range for normalcy and for detecting insomnia victims, we utilizing the approach of short time frequency analysis of PSD applied on EEG signals. This method will replace the graphical method of detection that is in contemporary use. In the past we have diagnosed rapid eye movement behavior disorder and the future work will focus on the employment of this technique for other diseases like epileptic seizures and other sleep disorders. Based on the short time frequency analysis of Power Spectrum Density, the results indicate the possibility of recognizing insomnia events based on delta, theta, alpha and beta segments of EEG signals.
Competing interests
MMS is researcher. The other authors declare that they have no competing interests.
Authors' contributions
MMS designed the algorithm for experiments and performed the experiments and analyzed the data. GS and SHS help me and guide me during my work. All authors read and approved the final manuscript.
Footnotes
Peer review under responsibility of Brazilian Association of Sleep.
Contributor Information
Mohd Maroof Siddiqui, Email: maroofsiddiqui@yahoo.com.
Geetika Srivastava, Email: gsrivastava2@lko.amity.edu.
Syed Hasan Saeed, Email: s.saeed@rediffmail.com.
References
- 1.Chouvarda, I, et al. Insomnia types and sleep microstructure dynamics. Engineering in Medicine and Biology Society (EMBC), In: Proceedings of 2013 35th Annual International Conference of the IEEE. IEEE; 2013. [DOI] [PubMed]
- 2.Chouvarda, Ioanna, et al. Insomnia treatment assessment based on physiological data analysis. Engineering in Medicine and Biology Society, 2007 (EMBS 2007), In: Proceedings of 29th Annual International Conference of the IEEE. IEEE; 2007. [DOI] [PubMed]
- 3.Siddiqui Mohd Maroof. EEG signals play major role to diagnose sleep disorder. Int. J. Electron. Comput. Sci. Eng. 2013;2(2):503–505. [Google Scholar]
- 4.Chouvarda, I, et al. CAP sleep in insomnia: new methodological aspects for sleep microstructure analysis. Engineering in Medicine and Biology Society (EMBC), In: Proceedings of 2011 Annual International Conference of the IEEE. IEEE; 2011. [DOI] [PubMed]
- 5.〈http://physionet.org/cgi-bin/atm/ATM〉.
- 6.Siddiqui Mohd Maroof. Detection of rapid eye movement behavior disorder using short time frequency analysis of PSD approach applied on EEG signal (ROC-LOC) Biomed. Res. 2015;26(3):587–593. [Google Scholar]
- 7.Krajca V, Petranek S, Paul K, Matousek M, Mohylova J, Lhotska L. Automatic detection of sleep stages in neonatal EEG using the structural time profiles, In: Proceedings of the 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference Shanghai, China, September 1–4, 2005. [DOI] [PubMed]
- 8.Acharya R.U., Faust O., Kannathal N., Chua T., Laxminarayan S. Non-linear analysis of EEG signals at various sleep stages. Comput. Methods Prog. Biomed. 2005;80:37–45. doi: 10.1016/j.cmpb.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 9.Liu D., Pang Z., Lloyd S.R. Neural network method for detection of obstructive sleep apnea and narcolepsy based on pupil size and EEG. IEEE Trans. Neural Netw. 2008;19:308–318. doi: 10.1109/TNN.2007.908634. [DOI] [PubMed] [Google Scholar]
- 10.Iasemidis L.D. Epileptic seizure prediction and control. IEEE Trans. Biomed. Eng. 2003;50:549–558. doi: 10.1109/tbme.2003.810705. [DOI] [PubMed] [Google Scholar]
- 11.Tzallas A.T., Tsipouras M.G., Fotiadis D.I. Epileptic seizure detection in EEGs using time–frequency analysis. IEEE Trans. Inf. Technol. Biomed. 2009;13(5) doi: 10.1109/TITB.2009.2017939. [DOI] [PubMed] [Google Scholar]
- 12.Siddiqui Mohd Maroof. Detection of periodic limb movement with the help of short time frequency analysis of PSD applied on EEG signals. Extraction. 2015;4(11) [Google Scholar]
- 13.Sleep Wake Disorders . Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. American Psychiatric Association; Washington, D.C.: 2013. [Google Scholar]