Abstract
Sleep complaints and sleep disturbances are highly prevalent in patients with psychiatric disorders. During hospitalization the patients’ condition may be even worse but little is known about the subjective sleep quality in psychiatric hospitals. Thus, we have investigated subjective sleep quality and mean sleep duration in patients with different psychiatric disorders at the end of hospitalization. For a period of one year, inpatients of a psychiatric hospital with diagnosis of substance use disorder (SUD), schizophrenia (SCZ), or anxiety/depressive disorders (AND) were routinely asked to fill in an easily comprehensible sleep quality questionnaire at the end of their hospitalization. Age, gender, subjective sleep quality, and sleep duration were analyzed; sleep duration was classified according to age-specific recommendations. Data of n=309 patients (age 52.1±17.9y, 56.1% women) were analyzed (n=63 SUD, n=50 SCZ, n=196 AND). Mean sleep duration was 7.0±2.0 h; 20.7% of patients had sleep durations below and 4.5% above age-specific recommendations. Non-restorative sleep during hospitalization was reported “almost always” in 38.2% (n=118), and “occasionally” in 30.1% (n=93). Subjective sleep quality was significantly associated with sleep duration (rs=−0.31, P<0.0005), but not with age, gender or diagnostic subgroup. The study showed that a great proportion of patients reported poor subjective sleep quality during hospitalization, regardless of age, gender and psychiatric diagnosis. As sleep quality was significantly associated with short sleep duration, a first step could be to take care to achieve recommended age-specific sleep durations in psychiatric hospitals.
Keywords: Sleep quality, Sleep duration, Psychiatric disorders, Hospitalization
1. Introduction
Sleep complaints and sleep disturbances are highly prevalent in neuropsychiatric disorders across the lifespan [1], [2]. Up to 80% of patients with schizophrenia spectrum disorder (SCZ) report sleep disturbances [3], including increased sleep onset latency, shorter sleep duration (total sleep time) and decreased sleep efficiency [1], [2]. Self-reported sleep disturbances are already prevalent in early psychosis and seem to be associated with symptom severity [4].
Sleep disturbances and non-restorative sleep are frequently occurring in patients with anxiety and depressive disorders (AND) [1], [2], [5], [6], [7]. Compared to healthy subjects, both insomnia (40–90%) and hypersomnia (5–10%) are more common in depression and related affective disorders. Persistent sleep disturbances are a major risk of developing depressive disorders, are part of the diagnostic criteria for major depressive disorders, and quite frequently continue during remission of depressive and anxiety disorders [5], [7], [8].
Alcohol and drugs of abuse have disruptive effects on sleep; accordingly, 50–90% of patients with substance use disorders (SUD), i.e. alcohol or drug dependence, have sleep disturbances, particularly longer sleep onset latency and shorter sleep duration as well as distorted sleep architecture [9], [10]. As consequences, reduced alertness, impaired next-day function, and increased daytime sleepiness are highly prevalent in patients with SUD [2], [10], [11]. Insomnia and poor subjective sleep quality are present during active substance use, intensified during discontinuation and withdrawal, and often persist even in abstinent patients [1]. Moreover, longitudinal studies suggest that enduring short sleep durations and insomnia are general risk factors for the development and non-remission of neuropsychiatric disorders, particularly of anxiety/depressive disorders (AND) and SUD [1], [6], [7], [12].
Additionally, the unique and independent importance of sleep disorders in patients with medical or psychiatric disorders has been corroborated with the transition from the forth to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV to DSM-5). Consistent with this view a bidirectional relationship between sleep disturbances and psychiatric disorders has to be assumed [13].
Based on a systematic review of available literature relating sleep duration to health, the National Sleep Foundation (NSF) has recommended sleep times at different life stages [14] which are largely in agreement with other recommending statements [15], [16]. Recommendations comprise optimum daily sleep durations for different age stages, acceptable and potentially even appropriate lower and higher sleep durations, and sleep durations outside this range (not recommendable, i.e. too low or too high). Meta-analyses have suggested that particularly short sleep durations (i.e. <5 h) are clearly associated with a heightened risk of metabolic and cardiovascular diseases [17], [18].
Taken together, all presently available findings suggest that insomnia and non-restorative sleep are highly frequent in patients with psychiatric disorders. It is assumed that due to the severity of illness and additional stress factors the poor sleep quality of patients with neuropsychiatric disorders is even worse during hospitalization [19], [20]. However, little is known about the sleep duration and subjective sleep quality of patients in psychiatric hospitals [21]. Thus, we have analyzed sleep duration and subjective sleep quality in patients with SUD, SCZ or AND at the end of their hospitalization.
2. Methods
2.1. Patients and design
Questionnaire data from adult inpatients (18–65 years) were consecutively sampled for 12 months at a university-affiliated regional psychiatric clinic and retrospectively analyzed. The study is part of a larger, self-financed health services research project on chronobiology, sleep, and mood in psychiatric disorders (CSMP). All included patients were able to consent and the study was approved by the local ethics committee. All patients of 6 wards specialized for the treatment of patients with either substance use disorder (SUD) (2 wards, about 80% alcohol dependence and 20% other SUDs), schizophrenia and related disorders (SCZ) (one ward), or anxiety and depressive disorders (AND) (3 wards) were asked to fill in a short self-rating sleep questionnaire [21], [22] on sleep duration and subjective sleep quality voluntarily and fully anonymously before discharge.
2.2. Assessment
The questionnaire comprises items regarding sex, age, and psychiatric disorder or complaints and problems as well as sleep-related questions. Sleep duration at night (i.e. weighted mean of workdays and weekends, mean hours) and sleep quality (“non-restorative sleep”; 3-point scale: 0=never, 1=occasionally/sometimes, 2=almost always) were assessed as an average of the period of hospitalization. As potentially influencing factors, caffeine consumption (0=no, 1=≤three cups of coffee/tea; 2=four or more cups of coffee/tea per day) and smoking status (0=never, 1=≤three cig/d; 2=three or more cig/d) were included in the present analyses; other aspects of the project will be reported in detail elsewhere.
Patients were treated according to current treatment guidelines and with sleep-promoting non-pharmacological and pharmacological measures as needed, no patient received sleep deprivation treatment.
2.3. Statistics
Subjective sleep quality and sleep duration were categorically and dimensionally analyzed, and descriptive statistics were calculated (frequencies, mean, standard deviation, 95% confidence intervals). Variables were compared between different patient groups (SUD, SCZ and AND) by means of analyses of variance (ANOVA) (dimensional data) or Chi2 tests (categorical data). To control for age effects, sleep duration was converted into age-specific categories according to the NSF recommendations [14] (Table 1).
Table 1.
Recommended sleep duration in adults [14].
| Recommendation | Age group |
|
|---|---|---|
| Young adults (18–25 years) | Adults (26–65 years) | |
| (A) Low, not recommended | <6 h | <6 h |
| (B) Low, may be appropriate | 6–7 h | 6–7 h |
| (C) Recommended | 7−9 h | 7−9 h |
| (D) High, may be appropriate | 10−11 h | 9−10 h |
| (E) High, not recommended | >11 h | >10 h |
Associations between variables were calculated using non-parametric rank correlations (Spearman's rs). The level of statistical significance was set at two-tailed α=0.05.
3. Results
Data of 309 patients could be analyzed with a substantially larger number of patients with anxiety or depressive disorder (AND). In Table 2, patients’ characteristics and sleep-related variables are reported for three diagnostic groups.
Table 2.
Patients’ characteristics.
| SUD |
SCZ |
AND |
Total |
Group differences | |
|---|---|---|---|---|---|
| N=63 | N=50 | N=196 | N=309 | ||
| Age [years] | 41.6±10.8 | 34.7±11.3 | 58.1±16.2 | 52.1±17.9 | aP<0.001 |
| % female | 26.3 | 52.0 | 64.6 | 56.1 | bP<0.001 |
| Subjective Sleep Quality | |||||
| Non-restorative sleep [0–2] | 1.2±0.8 | 0.9±0.8 | 1.1±0.8 | 1.1±0.8 | aP=0.10 |
| % Non-restorative sleep (occasionally or always) | 74.6 | 60.0 | 68.4 | 68.3 | bP=0.25 |
| % never | 25.4 | 40.0 | 31.6 | 31.7 | bP=0.29 |
| % sometimes | 27.0 | 32.0 | 30.6 | 30.1 | |
| % always | 47.6 | 28.0 | 37.8 | 38.2 | |
| Sleep duration and age-specific recommendations | |||||
| Mean sleep duration [h] | 6.0±1.6 | 7.7±1.6 | 7.1±2.0 | 6.9±2.0 | aP<0.001 |
| % not recommended sleep duration | 42.9 | 10.0 | 23.5 | 25.2 | bP<0.001 |
| % not recommended low | 42.9 | 8.0 | 16.8 | 20.7 | – |
| % may be appropriate low | 28.6 | 20.0 | 22.4 | 23.3 | |
| % recommended | 23.8 | 56.0 | 45.9 | 43.0 | |
| % may be appropriate high | 4.8 | 14.0 | 8.2 | 8.4 | |
| % not recommended high | 0.0 | 2.0 | 6.6 | 4.5 | |
| % smoking>3 cig/d | 84.1 | 64.6 | 62.1 | 67.2 | bP=0.005 |
| % coffee/tea>3 cups/d | 73.0 | 50.0 | 49.2 | 54.5 | bP=0.004 |
SUD, substance use disorder; SCZ, schizophrenia and related disorders; AND, anxiety and depressive disorders.
analysis of variance (ANOVA).
Chi2 tests.
Age differed significantly between diagnostic groups (AND>SUD>SCZ). Significantly less females were in the group of patients with SUD compared to SCZ or AND.
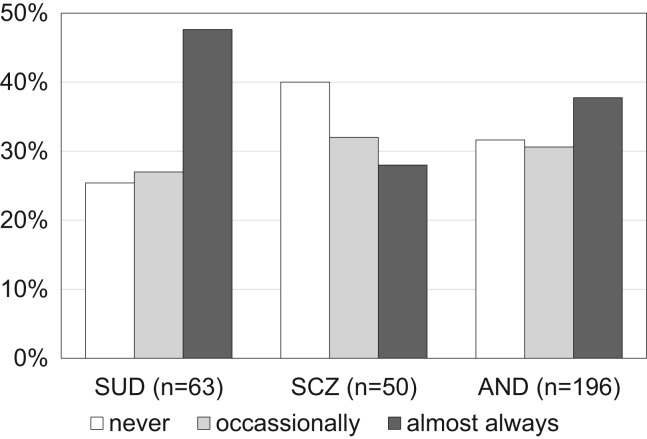
More than 2/3 of all patients reported poor subjective sleep quality (occasionally or always) during hospitalization without significant differences between the diagnostic groups (see also Fig. 1). Numerically, the highest proportion of patients with persistently poor subjective sleep quality during hospitalization was found in the SUD group. Additionally, significantly higher proportions of patients with SUD were smokers or reported higher caffeine consumption (more than 3 cups of coffee or tea a day).
Fig. 1.
Subjective sleep quality in patients with psychiatric disorders during hospitalization. SUD, substance use disorder; SCZ, schizophrenia and related disorders; AND, anxiety and depressive disorders.
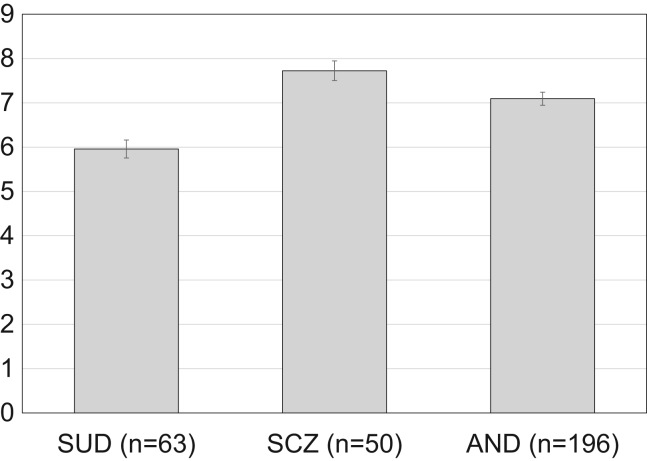
Mean sleep duration was significantly different between groups: SUD patients reported significantly lower sleep durations (95%CI [5.6–6.4 h]) than patients with SCZ (95% [7.3–8.2 h]) or AND (95% [6.7–7.2 h]) (Fig. 2).
Fig. 2.
Self-reported mean sleep duration during hospitalization in different diagnostic groups. Means±standard error of means (SEM); SUD, substance use disorder; SCZ, schizophrenia and related disorders; AND, anxiety and depressive disorders.
The analysis of age-specific recommended sleep durations revealed similar results: the significantly highest proportion of patients with non-recommended low sleep duration (43%) was found among patients with SUD (AND 24%; SCZ 10%; c.f. Table 2).
No significant gender differences were found with respect to clinical or sleep-related variables with the exception of a lower proportion of smoking women (59.6%) than men (76.3%, Chi2 test, P=0.006). Table 3 shows correlations of age and other sleep-related variables. Age showed a low, but significant negative correlation with sleep duration (r=−0.13, P=0.027) and a significant negative association with smoking (r=−0.40; P<0.0005) (Table 3).
Table 3.
Rank correlations (rs) of age and sleep-related variables.
| SQI | MSD | MSDc | Smoking | Caffeine | |
|---|---|---|---|---|---|
| Age [years] | −0.04 | −0.13* | −0.01 | −0.40*** | −0.07 |
| Sleep quality index SQI [0–2] | – | −0.27*** | −0.34*** | −0.03 | −0.04 |
| Mean sleep duration MSD [h] | – | +0.92*** | −0.03 | +0.06 | |
| MSD categories [1–5] | – | −0.11 | +0.02 | ||
| Smoking status [0–2] | – | +0.35*** |
SQI, sleep quality index (non-restorative sleep); MSD, mean sleep duration; MSDc, categories of sleep duration recommendations;
P<0.05.
P<0.001.
Subjective sleep quality (0−2) was significantly correlated with the mean sleep duration controlling for age (partial correlation; r=−0.28; P<0.0005). A similar correlation emerged between sleep quality ratings and categories of age-specific recommendations (rs=−0.34; P<0.0005).
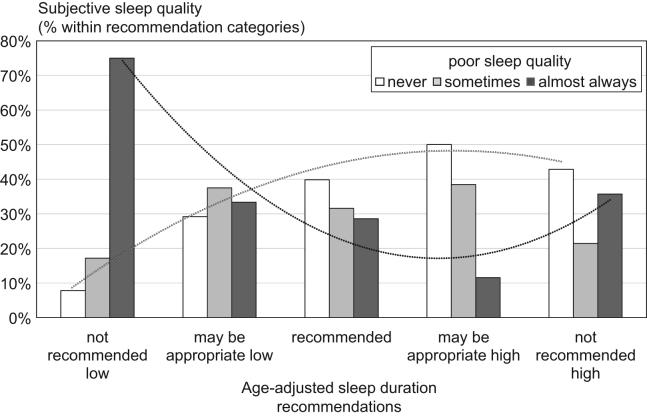
The relationship between recommended sleep duration and sleep quality is illustrated in Fig. 3. More than 75% of patients within the category of not recommended low sleep duration (i.e. <6 h) reported poor sleep quality. The highest proportion of patients with good subjective sleep quality (50%) was found within the category of patients with recommended normal to high sleep duration. The quadratic polynomial components superimposed in Fig. 3 illustrate a u-shaped relationship between recommended sleep duration and good sleep quality and an inverted u-shaped relationship between sleep duration and poor sleep quality.
Fig. 3.
Sleep duration and subjective sleep quality. Dotted lines represent quadratic (polynomial) trend lines; ┈ “almost always” poor sleep quality; ┈ “never” poor sleep quality.
4. Discussion
The study investigated subjective sleep quality and self-reported sleep duration in patients aged 18–65 years with a major neuropsychiatric disorder (schizophrenia spectrum disorders, substance use disorders, anxiety/depressive disorders) before discharge from hospitalization. A high prevalence of sleep disturbances in patients with different neuropsychiatric disorders during all illness stages has been repeatedly shown [1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [23]. However, subjective sleep quality and sleep duration has rarely been investigated during hospitalization in these patients.
Our results indicate that about 2/3 of inpatients with SCZ, SUD or AND experience poor subjective sleep quality during hospitalization. This number corresponds to prevalence rates of insomnia and sleep disorders found in clinical studies in patients with neuropsychiatric disorders [1], [2], [9], [10]. The large proportion of patients reporting non-restorative sleep during hospitalization in the present study (68.3%) did not significantly differ between diagnostic groups and was even higher than that found in general hospitals (medical/surgical hospitals: 45.6%) [19], [20]. However, the studies are hardly comparable due to different assessment methods, settings, and samples.
In the present study, gender and age were not significantly associated with subjective sleep quality. In the general population, a female predisposition of insomnia has been confirmed [24]. Moreover, age-related changes of objective sleep parameters, particularly higher sleep latencies and proportions of sleep stages 1/2 as well as lower nighttime sleep amounts have been found with increasing age [25], [26]. However, there are other findings at least in patients with depression relating increasing age to normalized sleep duration, reduced sleep onset latencies [27], as well as less-severe sleep-wake symptoms [28]. Smaller age-related changes are found, if at all, with self-reported sleep variables and subjective sleep quality compared to polysomnography measures [26], [28].
This discrepancy could at least partly reflect decreased symptom awareness in elderly patients [28]. Furthermore, the present analysis was limited to patients within an age range between 18 and 65 years to avoid confounding with sleep disturbances related to higher age. The present study revealed only limited evidence that caffeine consumption or smoking had an impact on sleep in patients with neuropsychiatric disorders during hospitalization. These findings are in line with reviews and meta-analyses showing potential sleep-disturbing properties of caffeine and nicotine [29] but also, that low to moderate caffeine consumption, mostly during morning hours, and regular smoking has little effect on subjective or polysomnographic sleep measures [10], [30]. Moreover the daily intake of 2–3 cups of coffee or tea appears to be associated with neutral or even beneficial effects for most health outcomes (cardiovascular and renal diseases, diabetes mellitus) [31], [32].
In the present study sleep duration emerged as the main factor contributing to subjective sleep quality. Across different diagnoses (SUD, SCZ, AND) the poorest subjective sleep quality was reported by patients with non-recommended low (and high) mean sleep durations. The analyses of age-specific recommendations were corroborated by a significant age-adjusted correlation between sleep duration and sleep quality.
It has, however, to be taken into account that in the present study the measure of sleep duration was exclusively subjective. It is known that sleep time misperceptions are common among subjects with sleep difficulties, particularly insomnia, with a however broad continuum between substantial under- and overestimates compared to polysomnographically estimated sleep durations [33], [34], [35]. Thus, perceived duration and quality of sleep seem to constitute important indicators of sleep disturbances beside and in addition to objective sleep measures [35]. A further potential limitation of the present study is its cross-sectional design with only one assessment of sleep quality at the end of hospitalization excluding e.g. pre-post comparisons.
Converging evidence suggests that short - but also excessively long – nighttime sleep durations bear the risk of mental and physical health problems in adults at least until reaching the age of 65 [15], [16], [36]. Accordingly, associations between sleep duration and daytime functioning are assumed to be associated in a curvilinear fashion with very low and excessively high sleep durations bearing the highest risk of impairment [13].
5. Conclusions
Although in the present study sleep duration and subjective sleep quality showed a shared variance of only about 10%, sleep duration was by large the most substantial factor influencing sleep quality. Clinicians should be aware that both insomnia and hypersomnia are associated with poor sleep quality [37] and that persistently short sleep duration and insomnia are great risks for higher morbidity and mortality [36], [38], [39]. Moreover, our results suggest that more efforts should be undertaken to ensure individually recommended, age-specific sleep durations during hospitalization in patients with psychiatric disorders.
Conflict of interests
None.
Acknowledgment
The authors would like to thank Dorothee Jochim for her support.
Footnotes
Peer review under responsibility of Brazilian Association of Sleep.
References
- 1.Spiegelhalder K., Regen W., Nanovska S., Baglioni C., Riemann D. Comorbid sleep disorders in neuropsychiatric disorders across the life cycle. Curr Psychiatry Rep. 2013;15:364. doi: 10.1007/s11920-013-0364-5. [DOI] [PubMed] [Google Scholar]
- 2.Benca R.M., Obermeyer W.H., Thisted R.A., Gillin J.C. Sleep and psychiatric disorders. A meta-analysis. Arch Gen Psychiatry. 1992;49:651–668. doi: 10.1001/archpsyc.1992.01820080059010. [DOI] [PubMed] [Google Scholar]
- 3.Klingaman E.A., Palmer-Bacon J., Bennett M.E., Rowland L.M. Sleep disorders among people with schizophrenia: emerging research. Curr Psychiatry Rep. 2015;17:79. doi: 10.1007/s11920-015-0616-7. [DOI] [PubMed] [Google Scholar]
- 4.Davies G, Haddock G, Yung AR, Mulligan LD, Kyle SD. A systematic review of the nature and correlates of sleep disturbance in early psychosis. Sleep Med Rev; 2016 Jan 14 [Epub ahead of print] [DOI] [PubMed]
- 5.Murphy M.J., Peterson M.J. Sleep disturbances in depression. Sleep Med Clin. 2015;10:17–23. doi: 10.1016/j.jsmc.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Mill J.G., Hoogendijk W.J., Vogelzangs N., van Dyck R., Penninx B.W. Insomnia and sleep duration in a large cohort of patients with major depressive disorder and anxiety disorders. J Clin Psychiatry. 2010;71:239–246. doi: 10.4088/JCP.09m05218gry. [DOI] [PubMed] [Google Scholar]
- 7.Soehner A.M., Kaplan K.A., Harvey A.G. Prevalence and clinical correlates of co-occurring insomnia and hypersomnia symptoms in depression. J Affect Disord. 2014;167:93–97. doi: 10.1016/j.jad.2014.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Medina A.B., Lechuga D.A., Escandón O.S., Moctezuma J.V. Update of sleep alterations in depression. Sleep Sci. 2014;7:165–169. doi: 10.1016/j.slsci.2014.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lucchesi L.M., Pradella-Hallinan M., Lucchesi M., Moraes W.A. Sleep in psychiatric disorders. Rev Bras Psiquiatr. 2005;27(Suppl 1):27–32. doi: 10.1590/s1516-44462005000500006. [DOI] [PubMed] [Google Scholar]
- 10.Conroy D.A., Arnedt J.T. Sleep and substance use disorders: an update. Curr Psychiatry Rep. 2014;16:487. doi: 10.1007/s11920-014-0487-3. [DOI] [PubMed] [Google Scholar]
- 11.Roehrs T.A., Roth T. Sleep disturbance in substance use disorders. Psychiatr Clin North Am. 2015;38:793–803. doi: 10.1016/j.psc.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Breslau N., Roth T., Rosenthal L., Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39:411–418. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 13.Winokur A. The relationship between sleep disturbances and psychiatric disorders: introduction and overview. Psychiatr Clin North Am. 2015;38:603–614. doi: 10.1016/j.psc.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 14.National Sleep Foundation. Sleep duration recommendations. National Sleep Foundation (NSF); 2015. 〈www.sleepfoundation.org〉.
- 15.Watson N.F., Badr M.S., Belenky G., Bliwise D.L., Buxton O.M., Buysse D. Joint consensus statement of the american academy of sleep medicine and sleep research society on the recommended amount of sleep for a healthy adult: methodology and discussion. Sleep. 2015;38:1161–1183. doi: 10.5665/sleep.4886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watson N.F., Badr M.S., Belenky G., Bliwise D.L., Buxton O.M., Buysse D. Recommended amount of sleep for a healthy adult: a joint consensus statement of the american academy of sleep medicine and sleep research society. Sleep. 2015;38:843–844. doi: 10.5665/sleep.4716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xi B., He D., Zhang M., Xue J., Zhou D. Short sleep duration predicts risk of metabolic syndrome: a systematic review and meta-analysis. Sleep Med Rev. 2014;18:293–297. doi: 10.1016/j.smrv.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 18.Iftikhar I.H., Donley M.A., Mindel J., Pleister A., Soriano S., Magalang U.J. Sleep duration and metabolic syndrome. An updated dose-risk meta-analysis. Ann Am Thorac Soc. 2015;12:1364–1372. doi: 10.1513/AnnalsATS.201504-190OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lei Z., Qiongjing Y., Qiuli W., Sabrina K., Xiaojing L., Changli W. Sleep quality and sleep disturbing factors of inpatients in a Chinese general hospital. J Clin Nurs. 2009;18:2521–2529. doi: 10.1111/j.1365-2702.2009.02846.x. [DOI] [PubMed] [Google Scholar]
- 20.Park M.J., Kim K.H. What affects the subjective sleep quality of hospitalized elderly patients? Geriatr Gerontol Int. 2016 doi: 10.1111/ggi.12743. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Cabanel N., Kundermann B., Olschinski C., Müller M.J. Subjective sleep quality in a psychiatric hospital. Somnologie. 2015;19:186–192. [Google Scholar]
- 22.Fietze I., Wiesenäcker D., Blau A., Penzel T. Schlafqualität im Krankenhaus und der Einfluss von Lärm. Somnologie. 2008;12:167–175. [Google Scholar]
- 23.Jones S.G., Benca R.M. Circadian disruption in psychiatric disorders. Sleep Med Clin. 2015;10:481–493. doi: 10.1016/j.jsmc.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 24.Zhang B., Wing Y.K. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29:85–93. doi: 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]
- 25.Ohayon M.M., Carskadon M.A., Guilleminault C., Vitiello M.V. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–1273. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 26.Floyd J.A., Medler S.M., Ager J.W., Janisse J.J. Age-related changes in initiation and maintenance of sleep: a meta-analysis. Res Nurs Health. 2000;23:106–117. doi: 10.1002/(sici)1098-240x(200004)23:2<106::aid-nur3>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 27.Xian H., Gonzalez C., Deych E., Farris S., Ding J., Shannon W. Age-related effects on circadian phase in the sleep of patients with depression and insomnia. Behav Sleep Med. 2015;13:208–216. doi: 10.1080/15402002.2013.855213. [DOI] [PubMed] [Google Scholar]
- 28.Vaz Fragoso C.A., Van Ness P.H., Araujo K.L., Iannone L.P., Klar Yaggi H. Age-related differences in sleep-wake symptoms of adults undergoing polysomnography. J Am Geriatr Soc. 2015;63:1845–1851. doi: 10.1111/jgs.13632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garcia A.N., Salloum I.M. Polysomnographic sleep disturbances in nicotine, caffeine, alcohol, cocaine, opioid, and cannabis use: a focused review. Am J Addict. 2015;24:590–598. doi: 10.1111/ajad.12291. [DOI] [PubMed] [Google Scholar]
- 30.Youngberg M.R., Karpov I.O., Begley A., Pollock B.G., Buysse D.J. Clinical and physiological correlates of caffeine and caffeine metabolites in primary insomnia. J Clin Sleep Med. 2011;7:196–203. [PMC free article] [PubMed] [Google Scholar]
- 31.Floegel A., Pischon T., Bergmann M.M., Teucher B., Kaaks R., Boeing H. Coffee consumption and risk of chronic disease in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Germany study. Am J Clin Nutr. 2012;95:901–908. doi: 10.3945/ajcn.111.023648. [DOI] [PubMed] [Google Scholar]
- 32.O’Keefe J.H., Bhatti S.K., Patil H.R., DiNicolantonio J.J., Lucan S.C., Lavie C.J. Effects of habitual coffee consumption on cardiometabolic disease, cardiovascular health, and all-cause mortality. J Am Coll Cardiol. 2013;62:1043–1051. doi: 10.1016/j.jacc.2013.06.035. [DOI] [PubMed] [Google Scholar]
- 33.Edinger J.D., Fins A.I. The distribution and clinical significance of sleep time misperceptions among insomniacs. Sleep. 1995;18:232–239. doi: 10.1093/sleep/18.4.232. [DOI] [PubMed] [Google Scholar]
- 34.Means M.K., Edinger J.D., Glenn D.M., Fins A.I. Accuracy of sleep perceptions among insomnia sufferers and normal sleepers. Sleep Med. 2003;4:285–296. doi: 10.1016/s1389-9457(03)00057-1. [DOI] [PubMed] [Google Scholar]
- 35.Pinto L.R., Jr, Pinto M.C., Goulart L.I., Truksinas E., Rossi M.V., Morin C.M. Sleep perception in insomniacs, sleep-disordered breathing patients, and healthy volunteers--an important biologic parameter of sleep. Sleep Med. 2009;10:865–868. doi: 10.1016/j.sleep.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 36.Shen X., Wu Y., Zhang D. Nighttime sleep duration, 24-hour sleep duration and risk of all-cause mortality among adults: a meta-analysis of prospective cohort studies. Sci Rep. 2016;6:21480. doi: 10.1038/srep21480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ohayon M.M., Reynolds C.F., 3rd, Dauvilliers Y. Excessive sleep duration and quality of life. Ann Neurol. 2013;73:785–794. doi: 10.1002/ana.23818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Mill J.G., Vogelzangs N., van Someren E.J., Hoogendijk W.J., Penninx B.W. Sleep duration, but not insomnia, predicts the 2-year course of depressive and anxiety disorders. J Clin Psychiatry. 2014;75:119–126. doi: 10.4088/JCP.12m08047. [DOI] [PubMed] [Google Scholar]
- 39.Vgontzas A.N., Fernandez-Mendoza J., Bixler E.O., Singareddy R., Shaffer M.L., Calhoun S.L. Persistent insomnia: the role of objective short sleep duration and mental health. Sleep. 2012;35:61–68. doi: 10.5665/sleep.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]