Abstract
Introduction
Obstructive sleep apnea syndrome (OSA) is diagnosed through polysomnography (PSG) or respiratory polygraphy (RP). Self-administered home-based RP using devices with data transmission could facilitate diagnosis in distant populations. The purpose of this work was to describe a telemedicine initiative using RP in four satellite outpatient care clinics (OCC) of Buenos Aires Hospital Británico Central (HBC).
Materials and methods
OCC technicians were trained both in the use of RP. Raw signals were sent to HBC via intranet software for scoring and final report.
Results
During a 24-month 499 RP were performed in 499 patients: 303 men (60.7%) with the following characteristics (mean and standard deviation): valid time for manual analysis: 392.8 min (±100.1), AHI: 17.05 (±16.49 and percentile 25–75 [Pt]: 5–23) ev/hour, ODI (criterion 3%): 18.05 (±16.48 and Pt 25–75: 6–25) ev/hour, and time below 90% (T<90): 17.9% (±23.4 and Pt 25–75: 1–23). The distribution of diagnoses (absolute value and percentage) was: normal (66/13%), snoring (70/14%), mild (167/33.5%), moderate (110/22%), and severe (86/17.2%). Continuous positive airway pressure (CPAP) was indicated for 191 patients (38.6%). Twenty recordings (4%) were considered invalid and the RP had to be repeated.
PSG at HBC was indicated in 60 (12.1%) cases (mild OSA or normal AHI with high ESS or cardiovascular disease).
Conclusions
Physicians were able to diagnosis OSA by doing portable respiratory polygraphy at distance. The remote diagnosis strategy presented short delays, safe data transmission, and low rate of missing data.
Keywords: Respiratory polygraphy, OSA, Telemedicine
1. Introduction
The development and use of communications technology in healthcare is aimed at enhancing the capabilities of healthcare settings (access to centralized databases and coordinated work between medical teams from remote clinics and reference center).
Telemedicine techniques may allow physicians to diagnose highly prevalent diseases that have a considerable impact on society's health and wellbeing and for which there are effective treatments available (e.g. sleep apnea syndrome).[1].
Supervised full-night PSG is the gold standard to confirm the diagnosis of obstructive sleep apnea syndrome (OSA). [2], [3] This procedure requires suitably equipped facilities staffed with qualified personnel. These laboratories are not always available or easy to reach for patients, which results in long waiting lists and considerable secondary costs.
Limited-channel portable devices (respiratory polygraphs) have sensors to record respiratory physiological variables and are currently accepted as a reliable, validated method. [2], [3], [4] We have recently described experiences with self-administered respiratory polygraphy (RP), a strategy with obvious advantages for large urban areas. [5], [6].
Given the high prevalence of OSA [2], [3] and the need for pragmatic diagnostic solutions [2], we analyzed the feasibility of establishing a network of satellite units for the diagnosis of sleep disorders in neighborhoods of Greater Buenos Aires connected to a reference hospital with a Central Sleep Unit (HBC).
We devised a virtual sleep center, where “equipment traditionally used by experts is used by NON-experts” and had qualified personnel perform systematic scoring and reports. We assessed the feasibility of obtaining remote RP recordings through raw respiratory signals sent by outpatient care clinics (OCC) technicians to the reference sleep laboratory at HBC. Secondary objectives were to assess delays, loss of recordings or need to repeat the test, and need for polysomnography (PSG).
2. Materials and methods
2.1. HBC and satellite OCCs
HBC promotes decentralization through the creation of smaller units (OCCs) that work under its coordination.
HBC conducts self-administered RPs have been available since 2008. [5] Satellite OCCs (4 at present) have enhanced their equipment and services (radiology, laboratory, general medicine, and specialties) to satisfy the needs of distant populations in an effort to achieve timely diagnosis of prevalent diseases according to established regulations and protocols.
The OCCs in Vicente Lopez (North of Greater Buenos Aires), Lomas de Zamora (South of Buenos Aires' suburbs), and M.T. de Alvear (North of the City of Buenos Aires) are located 19, 11, and 5 km away from HBC respectively. The Cardiology Unit is neighbor to HBC. These centers have qualified technicians who perform cardiac procedures according to international standards and pulmonologists who offer scheduled outpatient consultations. They are connected with HBC via intranet for mostly administrative purposes. The 6 senior technicians selected to operate the respiratory polygraphs are familiar with the use of recording equipment (Holter ECG and outpatient monitoring devices to measure blood pressure at OCC). They received basic training: 3 theoretical-practical sessions about OSA, the implementation of sleep scores and questionnaires as per protocol, practical training in basic diagnostic procedures, use of self-administered RP, and basic techniques to interpret respiratory signals. Training sessions were delivered by pulmonologists, who also distributed reading material and literature on specific topics. A landline and mobile phone numbers, and a mail box were made available for questions 24 h×7 days.
The protocol was approved by the medical board and the institutional review board in October 2012.
2.2. Inclusion and exclusion criteria
Adult patients with clinical suspicion of OSA through cardinal symptoms like snoring, witnessed apneas, or excessive daytime sleepiness were referred by their reference physicians for home-based self-administered RP according to the protocol in effect at HBC . [5] They were enrolled at OCCs during a 24-month period (between March 2013 and March 2015).
Patients with heart failure, neuromuscular disease, diagnosis of chronic obstructive pulmonary disease (COPD) and on continuous positive airway pressure (CPAP) or other type of ventilatory support or oxygen therapy were excluded from the study.
2.3. Measurements
All patients completed an updated version of Epworth (ESS) scale translated into Spanish, [7] the Berlin questionnaire, [8] and STOP-BANG questionnaire components [9] when they picked up the respiratory polygraphy devices.
The level III device used was Apnea Link Plus™ (ResMed. Australia) which includes nasal pressure cannula, respiratory effort sensor, and oximetry. It was operated on disposable batteries. The internal memory of the device can store up to 15 MB, which represents almost 12 h of data recordings. All patients were coached in the correct use of the device, including a practical demonstration, and received simple illustrations showing how to set up and use the device. Recordings were taken at home during one night. The following day, raw data (not edited) were attached to an e-mail (exported in a specific format: . OSA) together with clinical information and questionnaires’ scores and sent via intranet to HBC's lung function laboratory using Microsoft Outlook™. At the lab, recorded data were downloaded and imported to specialized software (Apnea Link 9.0), and later edited manually and systematically by experts. Data were encrypted according to institutional security standards for the protection of personal information.
2.4. Manual scoring
Recordings were analyzed with specialized software in windows of varying duration, usually in 3–5 min epochs. Respiratory events were corrected manually whenever necessary. Recording sections with low quality signals or transient disconnections were removed. Apnea was defined as a >80% drop from baseline airflow for ≥10 s; and hypopnea as a 50% drop for ≥10 s associated to ≥3% oxygen desaturation. [10] The apnea/hypopnea index (AHI) was calculated as the number of apneas/hypopneas per hour of valid total recording time (TRT). Patients were classified as normal (AHI <5/h), mild (AHI ≥5 and <15), moderate (AHI ≥15 and <30), severe (AHI ≥30).
Each final report with the corresponding suggested treatment was sent by e-mail (PDF format) to the corresponding OCC. RP appointment dates, recordings obtained, data transmitted, and final reports were kept in our files. For each specific case, OCC pulmonologists were in charge of clinical decisions and indication and monitoring of CPAP according to current standards, [3] without the involvement of other protocol investigators.
2.5. Statistical analysis
The Kolmogorov-Smirnov test was used to assess data distribution. Variables with normal distribution are expressed as mean values and standard deviations, and variables without normal distribution are expressed as mean and percentile values (25–75%). Direct cost data were sourced from the centralized SAP™ system for services. Statistical analysis was performed with Graph Pad Prism-5™ software.
3. Results
During a 24-month period 499 RP were performed in 499 patients: 303 men (60.7%) with the following characteristics (mean values and standard deviation): age; 55.3 years±14, body mass index [BMI]; 31.33±6.6 kg/m2 and ESS; 8.5±0.2. All patients had some level of education (10/10.1% elementary education only), 88.3% were at a high risk for OSA according to the Berlin questionnaire, and 33.7% obtained >10 points in ESS (Table 1).
Table 1.
Characteristics of study population.
| Variable | Value |
|---|---|
| n | 499 |
| Male | 303 (59.8%) |
| Female | 196 (39.2%) |
| Age (years) | 55.3±14a (18–92) |
| BMI | 31.3±6.6a (17–57) |
| Epworth sleepiness scale | 8.5±0.2a (0–24) |
| Berlin questionnaire (high risk sleep apnea) | 88.3% |
| Obese (%) | 54.1% |
| Education level | 99 (100%) |
| Elementary education level | 10 (10.1%) |
BMI=Body mass index
Mean and standard deviation.
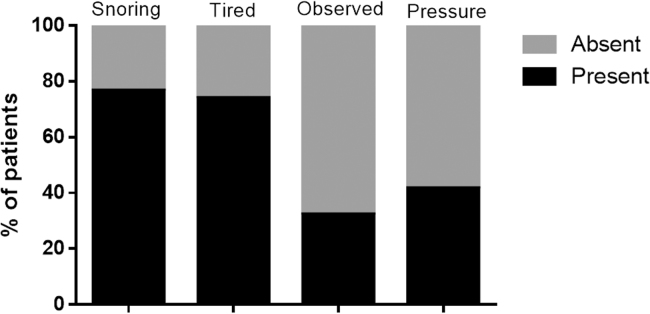
The most frequent reasons for indication of RP were: snoring (76%), observed apneas (32%), sleepiness or poor sleep quality (74%), and snoring associated to arterial hypertension (AHT) 41% (Fig. 1). The Fig. 2 shows distribution according to anthropometric parameters.
Fig. 1.
Symptoms according to STOP questionnaire (n: 499).
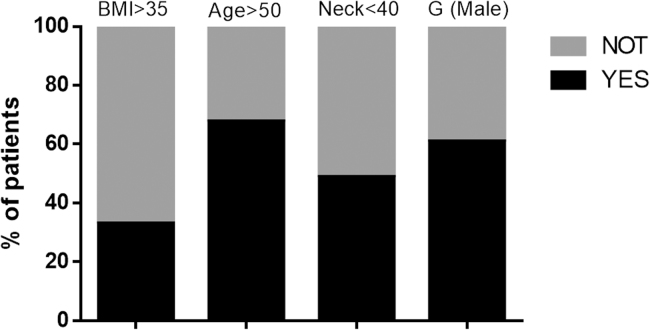
Fig. 2.
Anthropometric parameters (n: 499).
The referring units were pulmonology (80%), cardiology (12%), clinical medicine (4%), and otolaryngologist (4%).
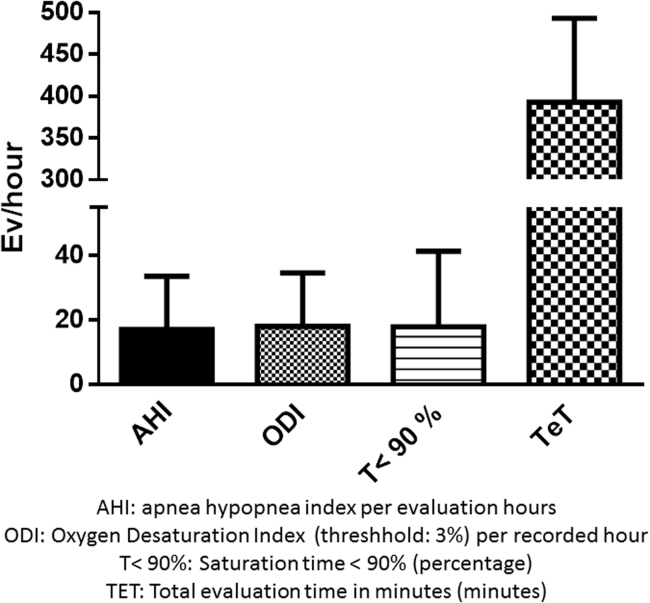
The polygraphic indicators (Table 2) across the population were; valid time for manual analysis: 392 min (±100.1), AHI: 17.05 (±16.49 and percentile 25–75 [Pt]: 5–23), ODI (criterion 3%): 18.05 (±16.48 and Pt 25–75: 6–25) ev/hour, and time below 90% (T<90): 17.9% (±23.4 and Pt 25–75: 1–23) Fig. 3.
Table 2.
Polygraphic indicators.
| Variable | Value |
|---|---|
| Total time of valid recordings (minutes) | 392.8±100 |
| AHI | 17±16.4a |
| ODI | 18±16.4a |
| T<90 (% TTR) | 17.9±23.4 |
| Central apneas (ev/hour) | 1 (0.1–5.1)b |
| Obstructive apneas (ev/hour) | 1 (0.2–2)b |
| Hypopneas (ev/hour) | 10.6 (3.5–15.9)b |
| Mixed apneas (ev/hour) | 5.5 (0.2–6.1)b |
AHI: Apnea Hypopnea Index per recording time. ODI: O2 desaturation index ≥3%.
T<90: Time under SaO2<90%. TRT: total recording time.
Values expressed as mean and standard deviation.
Values expressed as median and P25–75.
Fig. 3.
Indicators for home-based self-administered PR.
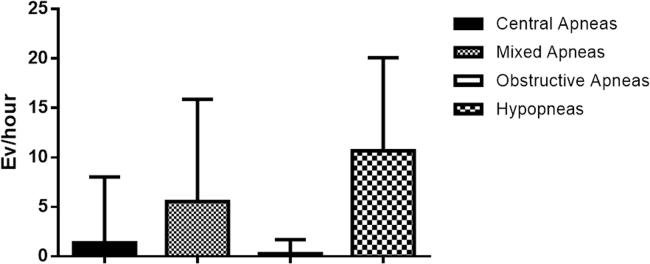
Fig. 4 shows the prevalence of hypopneas in documented respiratory disorders (events/hour).
Fig. 4.
Types of respiratory events in home-based RP.
The mean size of the raw file (.OSA) reached 4.69 Megabytes±1.11 and mean delays (business days) were: 5.3 business days±3.7 for RP recordings (from the time the appointment was made until final recordings were obtained), 1.64 days±2.3 for transmission of raw signals for analysis, and 1.1 days±0.9 for delivery of final report. No data were lost to transmission in any case.
The distribution of diagnoses was as follows (absolute value and percentage): normal (66/13%), snoring (70/14%), mild (167/33.5%), moderate (110/22%), and severe (86/17.2%) patients. CPAP was indicated for 191 patients (38.6%).
Twenty recordings (4%) were considered invalid because of cannula or oximeter disconnection resulting in TRT<240 min of valid recordings for manual analysis. The test had to be repeated on a different night. Full PSG at HBC was suggested as a complementary test in 60 (12.1%) cases (mild OSA or normal AHI with high ESS or cardiovascular disease). Five symptomatic patients that had been classified as mild OSA after RP were diagnosed as moderate OSA after PSG. If we take into account the direct cost of baseline RP, loss of profit from repeat testing, and PSGs performed upon conflicting results, test-related costs (direct costs) were 30% lower than those of conventional PSG, had it been the scenario (Table 3).
Table 3.
Direct cost related to the diagnostic test; PR vs. conventional PSG (theoretical scenario).
| Diagnostic strategy based on RP | n | Price per testa | Final direct cost |
|---|---|---|---|
| 1. RPs | 499 | 173 | 86.327 |
| 2. PSG at HBC (discordant RP) | 60 | 308 | 18.480 |
| Direct cost OCC | 499 + 20 + 60 | 108.267 | |
| Diagnostic strategy based on RP | 499 | 308 | 153.692 |
| Net savings | 45.425 | ||
Average price for RP and PSG (2015) with oxymetry (fees and expenses) according to HBC´s operative system for HMO and other health plans
American Dollars refers to current exchange rate.
4. Discussion
This pilot experience to assess the clinical feasibility and applicability of telemedicine resources can be useful to design models for the diagnosis of OSA in populations at risk for this disease. This strategy may clear crowded reference centers, shorten waiting lists, and avoid patients´ unnecessary visits to hospital.
This prospective study was aimed at exploring the feasibility of using RP with remote data transmission including data loss, performance of technicians with basic training, and data transmission within a network. Thus, considering this was neither a comparative nor a randomized study, it may have the consequent selection bias and weaknesses of observational designs.
We used respiratory polygraphs with simple settings, 3 channels, and 5 basic signals (level III of the AASM), [4] with the aim of conducting a pilot test for identification of potential anomalies during raw data downloading, export, and/or transmission from remote centers to HBC's sleep laboratory.
Our country has a vast territory and there are large areas without resources to study prevalent diseases with well-documented consequences such as OSA. By creating low-complexity centers able to obtain recordings from high-risk patients and centralizing the reading processes in experienced personnel, it may be possible to avoid unnecessary and costly transfer of patients and/or healthcare personnel.
Between 1999 and 2000, Kristo and col. assessed a telematic data transmission system via Internet at Walter Reed Army Medical Center (El Paso, Texas, USA). [11] They had recordings interpreted by qualified personnel at a sleep unit demonstrating that a remote study with an adequate cost-effectiveness ratio was technically feasible. In a contemporary study, Pelletier and Fleury [12] evaluated comparative cost and diagnostic effectiveness of an Internet telemonitored home-based PSG (level II). They demonstrated the reliability of this procedure, which was also preferred by patients. The cost of distant monitoring (telematic approach), however, was 159% higher than that of the home-based study. [12], [13].
In 2005, a Spanish article stated “in addition to reducing testing costs, polygraphy has decentralized diagnosis from reference units by facilitating diagnosis at smaller centers that work with the reference units in a coordinated manner.” [14] The same article commented on the growing optimism regarding technological progress and the development of “equipment traditionally used by experts, which is now used by non-experts.” It has also been described in the literature that strategies developed within basic healthcare levels (general practitioners, nursing, low-complexity medical centers) are useful to enhance the diagnostic capacity of healthcare centers. [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15] It is worth mentioning that this type of coordination is not formally established in Argentina, though a pilot experience has been reported by two centers [16].
The diagnostic technology used may not be as important as the qualifications and experience of people interpreting the results. [2], [6], [14].
Good quality RP recordings accompanied by sensible clinical evaluations allow diagnosis of OSA in two thirds of patients without the need for an appointment at a sleep unit. Appointments, therefore, can be reserved for PSG in more severe or difficult to diagnose cases. [2], [5], [6], [14].
Some countries with socialized medicine concerned with optimizing resources and implementing practical methods to diagnose prevalent diseases have conducted telemedicine experiences for the diagnosis of OSA. Recently, Coma del Corral et al. have published the results of the pilot study they carried out in Burgos (Spain). They used telematic techniques in real-time RP (monitored on line) and teleconsultation for indication of CPAP (video consultation) in patients with a suspicion of OSA living >80 km from the Sleep Unit [17]. 75% of the 40 patients enrolled complied with their CPAP treatment during a six-month follow-up period without seeing the specialist in person. The cost of diagnosis and treatment was lower in the telematic approach. A European group has reported similar results after conducting a multicenter study that demonstrated the cost-effectiveness of telemonitoring CPAP treatment in patients with OSA. [18].
The reliability of the network is evidenced by the low failure rate observed in RP testing at OCC. The repetition rate stood at 4%, matching a previous study performed with similar self-administered devices at HBC in 2013 [5].
The decision to use an intranet (wired network) instead of Wi-Fi was due to confidentiality and data protection concerns. However, the use of WLAN networks or a new generation of polygraphy devices with “cloud storage” capabilities is feasible at a minimum cost.
Delays remained within an acceptable range (less than a week) and the strategy permitted bedside testing.
Lastly, direct costs related with diagnostic test price were lower for RP, even when considering repeat testing and PSGs performed to clear doubts. Indirect costs were not analyzed, such as the cost for patients in terms of trips to and from HBC and driving hours in urban areas, cost of maintenance of PSG laboratory facilities, technicians’ fees, risk of equipment damage, and extended waiting lists, among others. Another advantage of satellite units is that the profitability of sleep units can be improved through the addition of virtual beds without a significant increase in operating costs, since the same qualified personnel will be reading and analyzing the recordings. In our particular case, we already had an intranet and set up terminals so there were not extra costs and it was possible to transmit data without additional costs.
Telemedicine holds the key to future integration of all the levels of care involved in the management of OSA patients. The World Health Organization defines telemedicine as
“The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities”.
Even though telemedicine approaches for OSA have not been extensively studied, data are promising and call for more studies to learn the true cost-effectiveness ratio of these strategies.
4.1. Final comments
This pilot program shows the feasibility of conducting RP testing away from high-complexity centers. This initiative can be applicable to large countries with limited resources. A communication network model, similar to the one described herein, could be used hundreds or thousands of kilometers away from the larger high-complexity unit.
Cost of patients’ transfers due to lack of available PSG beds may be reduced through the creation of low-complexity units for initial testing of patients with a suspicion for OSA. Data transmission and telematic RP could be a good option for the development of diagnosis networks, thus saving valuable resources for selected cases.
This decentralized diagnostic strategy of using home-based self-administered RP with data transmission and analysis by experts presented acceptable delays, reduced direct costs and allowed the indication of CPAP treatment to one third of the study population.
Footnotes
Peer review under responsibility of Brazilian Association of Sleep.
References
- 1.Cooper C.B. Respiratory applications of telemedicine. Thorax. 2009;64:189–191. doi: 10.1136/thx.2008.104810. [DOI] [PubMed] [Google Scholar]
- 2.de Sueño Grupo Español. Documento consenso español sobre el síndrome de apneas-hipopneas del sueño. Arch Bronconeumol. 2005;41(Suppl. 4):7. doi: 10.1016/s1579-2129(06)60248-6. [DOI] [PubMed] [Google Scholar]
- 3.Nogueira F., Nigro C., Cambursano H., Borsini E., Silio J., Avila J. Practical guidelines for the diagnosis and treatment of obstructive sleep apnea syndrome. Medicina. 2013;73(4):349–362. [PubMed] [Google Scholar]
- 4.Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable monitoring task force of the American academy of sleep medicine. J Clin Sleep Med. Vol. 3(7); 2007. [PMC free article] [PubMed]
- 5.Borsini E., Maldonado L., Décima T., Bosio M., Quadrelli S., Chertcoff J., Salvado A. Estrategia de utilización domiciliaria de la poligrafía respiratoria con instalación por el propio paciente. RAMR. 2013;13(1):4–11. [Google Scholar]
- 6.Borsini E., Bosio M., Quadrelli S., Campos J., Décima T., Chertcoff J. Poligrafía respiratoria en el diagnóstico de los trastornos respiratorios durante el sueño. Una herramienta necesaria para el neumonólogo. RAMR. 2012;12(4):152–160. [Google Scholar]
- 7.Chiner E., Arriero J.M., Signes-Costa J., Marco J., Fuentes I. Validation of the Spanish version of the Epworth Sleepiness Scale in patients with a sleep apnea síndrome. Arch Bronconeumol 1999. 1999;35:422–427. doi: 10.1016/s0300-2896(15)30037-5. [DOI] [PubMed] [Google Scholar]
- 8.Ahmadi N., Chung S.A., Gibbs A., Shapiro C.M. The Berlin questionnaire for sleep apnea in a sleep clinic population: relationship to polysomnographic measurement of respiratory disturbance. Sleep Breath. 2008;12:39–45. doi: 10.1007/s11325-007-0125-y. [DOI] [PubMed] [Google Scholar]
- 9.Chung F., Yegneswaran B., Liao P., Chung S.A., Vairavanathan S., Islam S., Khajehdehi A., Shapiro C.M. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812–821. doi: 10.1097/ALN.0b013e31816d83e4. [DOI] [PubMed] [Google Scholar]
- 10.Berry R.B. Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American academy of sleep medicine. J Clin Sleep Med. 2012;8(5):597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kristo D.A., Andrada T., Eliasson A.H., Poropatich R.K., Netzer C.M., Bradley J.P., Loube D.I., Netzer N.C. Telemedicine in the sleep laboratory: Feasibility and economic advantages of polysomnograms transferred online. Telemed J E Health. 2001;7:219–224. doi: 10.1089/153056201316970911. [Erratum in Telemed J E Health. 2001;7:347] [DOI] [PubMed] [Google Scholar]
- 12.Pelletier-Fleury N., Lanoe´ J.L., Phillipe C., Gagnadoux F., Rakotonanahary D., Fleury B. Economic studies and ‘technical’ evaluation of telemedicine: the case of telemonitored polysomnography. Health Policy. 1999;49:179–194. doi: 10.1016/s0168-8510(99)00054-8. [DOI] [PubMed] [Google Scholar]
- 13.Pelletier-Fleury N., Gagnadoux F., Philippe C., Rakotonanahary D., Lanoe´ J.L., Fleury B. A cost-minimization study of telemedicine. The case of telemonitored polysomnography to diagnose obstructive sleep apnea syndrome. Int J Technol Assess Health Care. 2001;17:604–611. [PubMed] [Google Scholar]
- 14.Durán-Cantolla J. New directions in the diagnosis of sleep apnea-hypopnea syndrome. Arch Bronconeumol. 2005;41(12) doi: 10.1016/s1579-2129(06)60330-3. 645-8. [DOI] [PubMed] [Google Scholar]
- 15.Mulgrew A.T., Fox N., Ayas N.T., Ryan F. Diagnosis and initial management of obstructive sleep apnea without polysomnography. Ann Intern Med. 2007;146:157–166. doi: 10.7326/0003-4819-146-3-200702060-00004. [DOI] [PubMed] [Google Scholar]
- 16.Borsini E., González C., Koreikis M., Campos J., Bosio M., Ernst G., Salvado A. Red de complejidad creciente en el diagnóstico de SAHOS. RAMR. 2015;2 00-00. [Google Scholar]
- 17.Coma-Del-Corral M.J., Alonso-Álvarez M.L., Allende M., Cordero J., Ordax E., Masa F. Reliability of telemedicine in the diagnosis and treatment of sleep apnea syndrome. Telemed J E Health. 2013;19(1):7–12. doi: 10.1089/tmj.2012.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Isetta V., Negrín M.A., Monasterio C. A Bayesian cost-effectiveness analysis of a telemedicine-based strategy for the management of sleep apnoea: a multicentre randomised controlled trial. Thorax. 2015;70:1054–1061. doi: 10.1136/thoraxjnl-2015-207032. [DOI] [PubMed] [Google Scholar]