Abstract
Background
Centrifugation (Cf) is a common method of fat processing but may be time consuming, especially when processing large volumes.
Objectives
To determine the effects on fat grafting time, volume efficiency, reoperations, and complication rates of Cf vs an autologous fat processing system (Rv) that incorporates fat harvesting and processing in a single unit.
Methods
We performed a retrospective cohort study of consecutive patients who underwent autologous fat grafting during reconstructive breast surgery with Rv or Cf. Endpoints measured were volume of fat harvested (lipoaspirate) and volume injected after processing, time to complete processing, reoperations, and complications. A budget impact model was used to estimate cost of Rv vs Cf.
Results
Ninety-eight patients underwent fat grafting with Rv, and 96 patients received Cf. Mean volumes of lipoaspirate (506.0 vs 126.1 mL) and fat injected (177.3 vs 79.2 mL) were significantly higher (P < .0001) in the Rv vs Cf group, respectively. Mean time to complete fat grafting was significantly shorter in the Rv vs Cf group (34.6 vs 90.1 minutes, respectively; P < .0001). Proportions of patients with nodule and cyst formation and/or who received reoperations were significantly less in the Rv vs Cf group. Based on these outcomes and an assumed per minute operating room cost, an average per patient cost savings of $2,870.08 was estimated with Rv vs Cf.
Conclusions
Compared to Cf, the Rv fat processing system allowed for a larger volume of fat to be processed for injection and decreased operative time in these patients, potentially translating to cost savings.
Level of Evidence: 3

In 2015, an estimated 231,840 new cases of invasive breast cancer were expected to be diagnosed in women in the United States, along with 60,290 new cases of non-invasive (in situ) breast cancer.1 Results from the Nationwide Inpatient Sample database showed immediate breast reconstruction rates increased on average 5% per year from 20.8% in 1998 to 37.8% in 2008.2 Approximately 102,215 post-mastectomy breast reconstruction procedures were performed in 2014, a 7% increase compared to the prior year.3 Moreover, nearly 62% of breast reconstructive procedures utilize autologous adipose cellular transplantation.4
Fat grafting, or autologous fat transfer, is increasingly being employed as an adjunctive technique in breast reconstruction for a variety of reasons.4 The technique provides the ability to shape and contour tissue through a minimally invasive approach and is associated with high patient satisfaction in numerous studies and systematic reviews.5-7 Tissue is removed from other parts of one's body—usually abdomen, thighs, and buttocks—by liposuction, then processed and injected into the breast area. This tissue is biocompatible, abundantly available, and can be injected in controlled amounts.
Results from a questionnaire issued to members of the American Society of Plastic Surgeons showed that respondents who use fat grafting for breast reconstruction most commonly use the procedure as an adjunct to implants to disguise the border or device and/or provide better shape (98%), as an adjunct to tissue flaps for improving shape or correcting contour of flaps (96%), and to address lumpectomy defects (87%).4 Grafting of fat can also be used to treat irradiated breast tissues and potentially prepare the bed for implant-based reconstruction.8,9
Fat grafting involves three steps: procurement, processing, and placement of the fat. Evidence suggests that method of processing is a critical variable in adipose cellular transplantation viability and retention.10 All fat processing methods seek to eliminate tumescent fluid, blood, cell fragments, and free oil11 in order to retain viable adipocytes in a concentrated form, which is believed to enhance graft take.12,13 There remains considerable debate over optimal processing methods for large-volume grafting, as traditional techniques were originally developed for small volume grafting.14 Centrifugation (Cf) is a commonly used method for autologous fat transfer.4,15 However, a frequent limitation of fat graft processing using a centrifugation technique is the time consuming and complex nature of the procedure in the operating room (OR), particularly when large volumes of fat are needed.14,16 Moreover, postoperative reoperations rates have ranged from 3% to 68% with Cf techniques, which may contribute to an increase in healthcare cost and utilization.17
A new commercially available autologous fat processing system (Rv; Revolve System, LifeCell Corporation, an ACELITY Company, Bridgewater, NJ) that incorporates fat harvesting, processing, and extraction within one system may simplify and increase efficiency of fat grafting. The lipoaspirate is simultaneously washed and filtered in a closed, integrated system. It actively washes and separates collagen strands and enhances the washing process for high-quality fat.
The purpose of this study was to compare the outcomes of adjunctive fat grafting with Rv vs Cf in 194 consecutive patients who underwent breast reconstruction. The amount of lipoaspirate, volume of fat injected after processing, OR time required to perform fat grafting, complications, and proportion of patients undergoing reoperations were primary endpoints used for comparison between the two groups. These inputs, along with inputs from published literature, were used to create a budget impact model to compare OR efficiency between the two groups.
METHODS
Evaluation of Clinical Outcomes
The Institutional Review Board at Peace Health Medical Group (Vancouver, WA) granted approval for this study. This was a retrospective cohort study that examined the records of consecutive breast surgery reconstruction patients who underwent autologous fat grafting with Cf between January 1, 2012 and December 31, 2012 compared to Rv between January 1, 2013 and December 31, 2013. All patients were followed for 6 months after the fat grafting procedure.
Records of all patients at least 18 years of age who received Coleman Cf18 technique in 2012 or Rv technique in 2013 were extracted from the data set and analyzed. Results from a preliminary analysis of this patient population were published previously in a review;19 a final analysis of the data was performed subsequently to evaluate additional outcome measures including proportion of patients undergoing reoperations, complication rates for each group during 6 months following the fat grafting procedure, and the budget impact of using Rv. All patients in both groups were treated with tumescent method and received preoperative and postoperative antibiotics for a total of 5 days. The ratio of tumescent solution to lipoaspirate was approximately 1:1 for all cases. Demographic information, volume of lipoaspirate obtained after fat harvesting, volume of fat injected after processing, amount of OR time spent to complete fat grafting technique (from start of lipoaspiration to end of injection), number of reoperations, and complications (nodule formation, cyst formation, or fat necrosis) were recorded for each case. If other breast procedures were performed on the same patient, fat grafting was performed after those procedures to ensure there was no lag time between lipoaspiration, fat processing, and fat injection.
Descriptive statistics for patient characteristics are reported as mean and standard deviation for continuous measures and frequency and percent for categorical measures. t tests for continuous measures and chi-square tests for categorical measures were used to evaluate differences in patient characteristics. In the evaluation of the clinical endpoints, general linear models were used for continuous dependent variables, and binary logistic regression was used for categorical dependent variables (reoperation and complication rates) to compare the Rv and Cf groups. We controlled for the effects of age, BMI, smoking, diabetes, unilateral/bilateral status, and previous radiation and chemotherapy exposure to reduce confounding effects. Least square means are reported for continuous outcomes after adjusting for covariates. Proportions and relative risks are reported for categorical outcomes. Data were analyzed using SAS 9.4 (SAS Institute Inc., Cary, NC) statistical software.
Budget Impact Model
A budget impact model was developed using results from this study along with other published studies to estimate OR costs of each technique. In the base-case scenario, an OR cost of $29.37/minute was utilized by taking an average of costs reported in published literature20,21 and inflating to 2015 dollars using the Medical Care Consumer Price Index. A sensitivity analysis was performed to test the model at minimum and maximum reported costs in literature ($17 and $38 respectively after adjusting for inflation). The list price for Rv of $495 was used as the Rv device cost. Centrifuge equipment is typically a capital cost that undergoes considerable depreciation over time; thus, a minimal $10 cost per centrifuge use was assumed in the base-case scenario. The model was also tested assuming a $0 cost per centrifuge use in the sensitivity analysis. The actual volume of fat injected differed between the two groups in this study, and because our budget impact model required using just one volume, a hypothetical volume of 150 mL was used as a standard volume for comparison of both groups. The choice to use the standardized 150 mL volume was based on suggestions from a previous survey of 30 surgeons.22 Grafting rate for the two techniques was calculated using the following formula:
In order to utilize a grafting rate that accounted for the variability amongst practices, the grafting rate was estimated by calculating the weighted average of grafting rate from this study and from one other comparable retrospective analysis performed by Brzezienski and Jarrell.19,23 The studies were combined and weighted by sample size to create weighted average grafting rates for Rv and Cf.
RESULTS
Evaluation of Clinical Outcomes
A total of 194 female fat grafting cases were analyzed. Of these, 98 females received Rv and 96 received Cf. All patients in the dataset who received Cf were treated between January 1 and December 31, 2012, and all patients who received Rv were treated between January 1 and December 31, 2013.
All fat grafting procedures in both groups were performed by a single plastic surgeon (A.G.); fat grafting was used in total autologous fat grafting, and as an adjunct to implants and other reconstructive procedures such as nipple reconstruction. None of the fat that was harvested was discarded prior to processing. Some of the breast reconstruction patients were breast cancer positive; the remaining patients in this series who were not breast cancer positive were either gene positive or had a strong family history of cancer.
The mean age of patients was 51.0 years (SD, 10.3; range, 22-76 years) and the mean BMI was 27.2 kg/m2 (SD, 6.0; range, 18-55 kg/m2). There were no significant differences between Cf and Rv patients with respect to mean age, BMI, smoking status, diabetes, unilateral/bilateral, and prior radiation. A significantly higher number of Cf patients vs Rv patients (41[42.7%] vs 25 [25.5%], P = .011, respectively) received chemotherapy (Table 1). After covariate adjustment, the mean volumes of lipoaspirate (506.0 vs 126.1 mL) and fat injected (177.3 vs 79.2 mL) were significantly higher (P < .0001) in the Rv group compared to the Cf group. Adjusted mean amount of time spent in the OR from lipoaspiration to injection was significantly shorter in the Rv group compared to the Cf group (34.6 vs 90.1 minutes, respectively; P < .0001) (Table 2).
Table 1.
Patient Characteristics
| Preoperative Variable | Rv (N = 98) | Cf (N = 96) | P Value |
|---|---|---|---|
| Age, mean (SD), range, years | 51.89 (10.568), 29-76 | 50.06 (10.019), 22-70 | .219 |
| BMI, mean (SD), range, kg/m2 | 27.38 (5.807), 19-55 | 27.06 (6.668), 18-52 | .726 |
| BMI > 30 kg/m2 | 26 (26.5%) | 23 (24%) | .680 |
| Smokers | 3 (3.1%) | 4 (4.2%) | .680 |
| Diabetes | 7 (7.1%) | 11 (11.5%) | .300 |
| Radiation | 27 (27.6%) | 30 (31.3%) | .572 |
| Chemotherapy bilateral procedure | 25 (25.5%) 92 (93.9%) |
41 (42.7%) 91 (94.8%) |
.011 .783 |
Table 2.
Outcomes in the First Visit
| Endpoint Measured | Rv (N = 98) |
Cf (N = 96) |
P Valuea | ||
|---|---|---|---|---|---|
| LS Mean (SE) | 95% CI | LS Mean (SE) | 95% CI | ||
| Lipoaspirate obtained (mL) | 506.0 (21.2) | 464.2, 547.8 | 126.1 (20.5) | 85.6, 166.6 | <.0001 |
| Fat injected (mL) | 177.3 (10.7) | 156.3, 198.3 | 79.2 (10.3) | 58.9, 99.6 | <.0001 |
| Time (minute) | 34.6 (2.7) | 29.2, 40.0 | 90.1 (2.7) | 84.8, 95.3 | <.0001 |
LS, Lipoaspirate.
aControlled for age, BMI, smoking, diabetes, unilateral/bilateral, and prior chemotherapy exposure.
Nodule and cyst formations were significantly fewer in the Rv vs Cf group (10/98 [10.2%] vs 27/96 [28.1%] and 7/98 [7.1%] vs 18/96 [18.8%], respectively (P < .05)). Fat necrosis formation was not significantly different between the two groups (3/98 [3.1%] vs 9/96 [9.4%], P = .131). The proportion of patients who underwent a reoperation within 6 months was significantly lower in the Rv group vs Cf group (37/98 [37.8%] vs 56/96 [58.3%], relative risk: 1.5, P < .05). All reoperations were conducted to add more soft tissue to the breast. Patient complication results are listed in Table 3.
Table 3.
Complications in the First Visit
| Complication | Rv (N = 98) N (%) | Cf (N = 96) N (%) | Relative Risk (95% CI) | P Valuea |
|---|---|---|---|---|
| Nodule formation | 10 (10.2%) | 27 (28.1%) | 2.8 (1.4, 5.4) | .004 |
| Cyst formation | 7 (7.1%) | 18 (18.8%) | 2.6 (1.1, 6.0) | .023 |
| Fat necrosis | 3 (3.1%) | 9 (9.4%) | 3.1 (0.9, 11.0) | .131 |
| Proportion of reoperations | 37 (37.8%) | 56 (58.3%) | 1.5 (1.1, 2.1) | .007 |
aControlled for age, BMI, prior chemotherapy exposure.
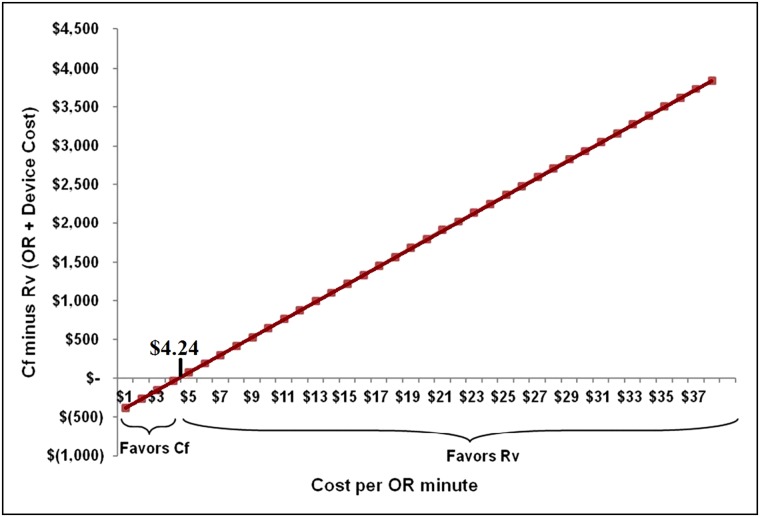
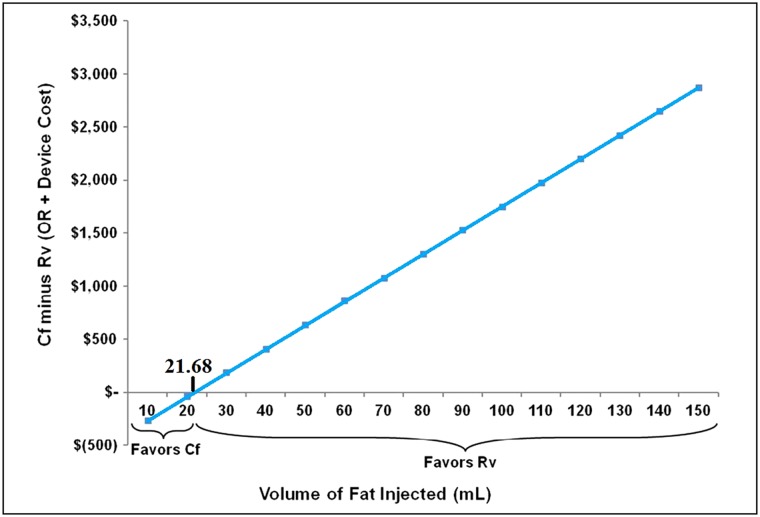
Budget Impact Model
The weighted average grafting rate was calculated to be 5.78 mL/min for Rv and 1.07 mL/min for Cf (Table 4). The standardized average time taken to inject 150 mL of fat was 25.95 minutes with Rv and 140.19 minutes with Cf. These estimates were utilized in the model and resulted in an estimated mean total cost of $1257.18 with Rv and $4127.26 with Cf including device cost, suggesting a cost savings of $2870.08 per patient with Rv. The sensitivity analysis showed similar results, with cost savings of $1457.00 to $3855.93 with Rv, assuming varied OR costs per minute of $17 to $38. Inputs, calculations and results for the budget impact model are shown in Table 5. Results from our model demonstrated that cost savings could be achieved with Rv even if the Cf equipment cost was $0. Cost savings were seen with Rv for any case where the OR cost per minute was higher than $4.24 and the volume of fat to be injected was at least 21.68 mL (Figures 1 and 2).
Table 4.
Grafting Rate Calculation
| Study | Cf |
Rv |
||||||
|---|---|---|---|---|---|---|---|---|
| N | Volume Injected (mL) | Time (min) | Rate (mL/min) | N | Volume Injected (mL) | Time (min) | Rate (mL/min) | |
| Brzezienski et al23 | 13 | 101.2 | 57.2 | 1.77 | 24 | 241.2 | 51.4 | 4.69 |
| Gabriel dataa | 96 | 83.6 | 85.6 | 0.98 | 98 | 182.7 | 30.2 | 6.05 |
| Weighted average | 1.07 | 5.78 | ||||||
aWithout covariates.
Table 5.
Budget Impact Model
| Rv | Cf | Difference (Cf – Rv) | |
|---|---|---|---|
| Model inputs | |||
| Number of patients | 100 | 100 | |
| Volume of fat injected (mL) | 150 mL | 150 mL | |
| Device cost | $495 | $10 | |
| Average time to inject 150 mL of fat (minutes) | 25.95 | 140.19 | |
| Proportion of reoperations | 37.8% | 58.3% | |
| OR cost – average $29.37/minute | |||
| OR cost | $762.18 | $4117.26 | $3355.08 |
| OR + device cost | $1257.18 | $4127.26 | $2870.08 |
| OR + device + reoperation Costa | $1732.40 | $6533.46 | $4801.06 |
| OR cost – minimum $17/minute | |||
| OR cost | $441.17 | $2383.16 | $1942.00 |
| OR + device cost | $936.17 | $2393.16 | $1457.00 |
| OR + device + reoperation Costa | $1290.04 | $3788.38 | $2498.34 |
| OR cost – maximum $38/minute | |||
| OR cost | $986.14 | $5327.07 | $4340.93 |
| OR + device cost | $1481.14 | $5337.07 | $3855.93 |
| OR + device + reoperation Costa | $2041.01 | $8448.58 | $6407.57 |
aThe fat processing system used during the reoperation was assumed to be the same as in the first visit.
Figure 1.
Breakeven point for operating room (OR) cost per minute.
Figure 2.
Breakeven point for volume of fat injected.
The model was further adjusted to include a second surgery cost based on the proportion of patients undergoing reoperations for Rv and Cf. In this adjusted model, the average total cost savings with Rv increased to $4801.06 per patient with a range of $2498.34 to $6407.57 based on a range of per-minute OR costs of $17 to $38. Finally, the model was tested at 100% reoperations for Rv and 0% for Cf to get conservative estimates and the results still showed an average cost savings of $1612.90 with Rv.
DISCUSSION
As the number of breast reconstruction procedures expands each year, addressing OR efficiency and outcomes is becoming increasingly important to cosmetic surgeons and patients. A major reason for the growing popularity of fat grafting may be that the technique allows surgeons to improve results of traditional implant-based breast surgery procedures, without changing the general treatment strategy.4 Fat grafting can provide a natural consistency and relatively long lasting result compared to synthetic fillers such as polylactic acid24 because it does not biodegrade over time; it can also improve cutaneous and subcutaneous trophicity,25 and limit granuloma and allergic reactions which could be provoked by nonautologous permanent fillers, such as expanded polytetrafluoroethylene.26,27
In this series of breast reconstruction patients, Cf was used for fat processing from January 1 to December 31, 2012 whereas Rv was used for processing between January 1 and December 31, 2013. We shifted from Cf to Rv use in 2013, as Rv had become available and our hospital administrators sought an outcomes comparison between the two different fat processing techniques. From our study, we found that a significantly greater volume of lipoaspirate was obtained, processed, and injected in a significantly shorter amount of time with use of Rv vs Cf fat grafting technique. The proportions of patients who experienced nodule and cyst formation, and/or underwent reoperation, were significantly lower with Rv fat grafting in our patient population. This difference in complication rates could impact patient satisfaction rates and the number of required patient follow-up visits, but these variables were not measured in the study.
Each patient with a nodule underwent an ultrasound and if a cyst was detected, it was aspirated; if fat necrosis was suspected, it was biopsied to confirm. No reoperations were necessary for the management of nodules in this study population. From the data it was not possible to determine the exact causality of nodule formation. The difference in nodule formation rates between the groups could be the result of exceeding the capacity of the recipient bed with autologous fat graft material. However, since the patient characteristics and technique practice did not differ between the two groups, this seems unlikely. Moreover, the Cf group had a higher rate of nodule formation even though smaller volumes were injected. Thus, these authors believe that this variance in nodule formation rates may be due to the differences between these two fat processing methods.
In this study, we observed that 35% of harvested fat was injected in the Rv group whereas 63% of harvested fat was injected in the Cf group. Based on our experience and a previous publication, we believe this content difference between the two groups was related to differences in processing and fat quality. Ansorge et al studied the quality and quantity of fat retention during autologous fat processing with the Rv system, compared to decantation and centrifugation in a prospective, pre-clinical study of 10 patients.10 Biochemical characteristics and free oil, adipose, and aqueous phases of the processed fats were determined. Fat grafts were implanted in nude mice; volume retention and quality of the fat grafts were evaluated after 28 days. The Rv system yielded significantly less blood cell debris, a higher percentage of adipose tissue, and a lower percentage of free oil compared with the other 2 methods. Fat tissue retention from Rv samples was significantly higher (73.2%) than that from decanted samples (37.5%) and similar to that from centrifuged samples (67.7%).10
There are few published studies to which we can directly compare our outcomes. Our literature search identified only one comparative retrospective data review of fat grafting patients who received Cf (n = 13) vs Rv (n = 24).23 The average rate of fat transfer with the Rv system was significantly faster compared to the Coleman technique in this study (4.69 vs 1.77 mL/minute, respectively; P < .0001).23 We chose to use a weighted average of the outcomes in this Brzezienski and Jarrell study and our current study in an attempt to determine a realistic average grafting rate (Table 4) for our budget impact model.
Of 456 members of the American Society of Plastic Surgeons who responded to a questionnaire in 2011/2012, 34% reported using centrifugation, 34% reported using filtration, and 28% reported using a sedimentation step.4 An earlier survey of 508 members of the ASPS in 2007 showed that of respondents who perform autologous fat grafting, 75% used a centrifugation technique.15 Based on these published survey results,15 and based on our review of the literature, centrifugation appears to be the most commonly reported technique for fat processing in autologous fat grafting of the breast, and was therefore chosen as the comparator in this study.
The Coleman technique is the most widely used centrifugation protocol28 and involves centrifuging the lipoaspirate at approximately 1200 × g (3000 rpm) for 3 minutes. However, Cf is relatively labor-intensive and time-consuming to perform in the OR, particularly with a high volume of fat transfer. It can also require specialized equipment, instruments, or supplies used to separate fat layers or harvest the fat. Rv largely eliminates the need for additional instrumentation and is easier to operate for the OR staff. It is a single use device that can be reused multiple times within the same procedure for the same patient.
Time savings in fat grafting is desirable because fat grafting Current Procedural Terminology codes are typically not well reimbursed, making a surgeon's time in the OR an important consideration with respect to cost of fat grafting. With this system, we have achieved major time savings in terms of processing because the hand processing component of the technique is removed. Lipoaspirate can be channeled directly into the system which eliminates lipoaspirate handling in syringes. Brzezienski and Jarrell calculated whether reduced fat handling time could translate to reduced overall costs with Rv vs conventional Cf.23 Their break-even cost analysis suggested use of Rv vs Cf in cases of planned fat transfer of 75 mL or more. In these cases, the price of the Rv device may be offset by savings in surgeon time and operating room costs.23
This technology could provide greater access to quick fat grafting for smaller community hospitals that may lack special instrumentation or additional trained personnel needed to perform complex fat grafting procedures. For best results, fat needs to be kept warm, at body temperature, from extraction to injection. A limitation of the Rv system is that if the fat is too fibrous, the system may not work properly.
Due to the high variability in graft volume retention rates, obtaining predictable, reliable, and consistent outcomes has historically been a major challenge in fat grafting. We have observed a high quality of fat with Rv and greater predictability in transfer with this washing/filtration system, compared to Cf. However, we have used visual observation and skin testing to judge the level of fat graft retention, and have not quantitatively measured volume retention, so it was not possible to accurately compare longer-term outcomes in the study groups.
Fat survival rate and longstanding results depend on indications and patient conditions as well as technique. Although there is a lack of large clinical studies with long-term follow-up (>4 years) evaluating the safety or effectiveness of any one technique of fat grafting, different processing techniques are known to affect differences in fat cell survival. Fat cell resorption rates vary widely in literature, with as much as 40% to 60% of volume of fat injected reported lost29-32 due to necrosis or resorption.11 Literature does not yet provide clear guidance as to the optimal technique at any of the stages of fat grafting, but a couple of recent studies suggest that the quality of fat and in vivo volume retention rates are fairly equally comparable between washing/filtration methods and centrifugation methods.10,33
Gabriel et al previously suggested based on a literature review and personal experience that use of lower suction pressure for liposuction, use of large bore-sized harvesting cannulas, use of low centrifugation forces (if using centrifugation for processing), use of low shear stress during injection, placement of small parcels of fat, and optimizing the volume of fat injected to the capacity of the recipient site were noted to be associated with improved fat retention.19,34,35 A longer time from harvest to injection also appears to negatively impact retention rates, largely because it is difficult to maintain the fat at body temperature over time.19 Controlled research is needed to determine whether the processing time savings achieved with Rv could have a positive effect on fat graft survival.
Results of this single-center, single-surgeon study are limited, and additional large, controlled studies are required to further determine differences between Rv and Cf. Study groups were not concurrent, and time may have played a role in differing outcomes between Rv and Cf. However, this seems unlikely as nothing in our technique changed over time, other than the method used for fat processing. Moreover, patient characteristics were similar between groups (with the exception of prior chemotherapy exposure). We examined time trends in our research but did not see any independent time trends. However, a concurrent control would be needed to definitively rule out the effect of time.
Another limitation of the study was that different volumes of fat were lipoaspirated and injected across the two groups. For budget impact calculations, we mitigated this limitation by standardizing the volume of fat to be injected as 150 mL. For purposes of comparison, we have used grafting rate (volume of fat injected divided by time) to compare the two groups. The difference in volumes could have influenced clinical outcomes but this was not studied. Finally, it was not possible to control additional patient co-morbidities such as smoking or diabetes in our analysis of complication and reoperation rates due to the small number of smokers and diabetics in each group.
CONCLUSION
Despite real and theoretical risks, there is widespread adoption of fat grafting in plastic and reconstructive surgery, and its use has grown dramatically in recent years.4 New technologies, such as Rv are needed to simplify and speed the processing of large volumes of fat. The Rv fat processing system decreased operative time in these patients, which translated into a potential cost savings and allowed for a larger volume of fat to be processed for injection compared to Cf. Percentages of patients who developed nodules or cysts, and/or who underwent a reoperation, were also significantly smaller in the Rv vs Cf group. Further research is needed to describe the relationship between complications and reoperations in fat grafting.
Disclosures
Dr Gabriel is a Consultant for LifeCell, an Acelity company. Ms Griffin, Ms Parekh, and Mr Macarios are employees of Acelity. Drs Champaneria and Maxwell declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Acknowledgement
The authors wish to thank Karen Beach (Acelity) for support in editing this manuscript.
REFERENCES
- 1.U.S. Breast Cancer Statistics. http://www.breastcancer.org/symptoms/understand_bc/statistics Accessed January 27, 2016.
- 2.Albornoz CR, Bach PB, Mehrara BJ et al. A paradigm shift in U.S.: Breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15-23. [DOI] [PubMed] [Google Scholar]
- 3.ASPS National Clearinghouse of Plastic Surgery Procedural Statistics: 2014 Plastic Surgery Statistics Report. http://www.plasticsurgery.org/Documents/news-resources/statistics/2014-statistics/plastic-surgery-statsitics-full-report.pdf Accessed March 23, 2016.
- 4.Kling RE, Mehrara BJ, Pusic AL et al. Trends in autologous fat grafting to the breast: a national survey of the american society of plastic surgeons. Plast Reconstr Surg. 2013;132:35-46. [DOI] [PubMed] [Google Scholar]
- 5.Leopardi D, Thavaneswaran P, Mutimer KL et al. Autologous fat transfer for breast augmentation: a systematic review. ANZ Journal of Surgery. 2014;84:225-230. [DOI] [PubMed] [Google Scholar]
- 6.Rosing JH, Wong G, Wong MS et al. Autologous fat grafting for primary breast augmentation: a systematic review. Aesthetic Plast Surg. 2011;35:882-890. [DOI] [PubMed] [Google Scholar]
- 7.Biazus JV, Falcao CC, Parizotto AC et al. Immediate reconstruction with autologous fat transfer following breast-Conserving surgery. Breast J. 2015;21:268-275. [DOI] [PubMed] [Google Scholar]
- 8.Salgarello M, Visconti G, Barone-Adesi L. Fat grafting and breast reconstruction with implant: another option for irradiated breast cancer patients. Plast Reconstr Surg. 2012;129:317-329. [DOI] [PubMed] [Google Scholar]
- 9.Sarfati I, Ihrai T, Kaufman G et al. Adipose-tissue grafting to the post-mastectomy irradiated chest wall: preparing the ground for implant reconstruction. J Plast Reconstr Aesthet Surg. 2011;64:1161-1166. [DOI] [PubMed] [Google Scholar]
- 10.Ansorge H, Garza JR, McCormack MC et al. Autologous fat processing via the Revolve system: quality and quantity of fat retention evaluated in an animal model. Aesthet Surg J. 2014;343:438-447. [DOI] [PubMed] [Google Scholar]
- 11.Gutowski KA. Current applications and safety of autologous fat grafts: a report of the ASPS fat graft task force. Plast Reconstr Surg. 2009;124:272-280. [DOI] [PubMed] [Google Scholar]
- 12.Allen RJ Jr, Canizares O Jr, Scharf C et al. Grading lipoaspirate: is there an optimal density for fat grafting? Plast Reconstr Surg. 2013;1311:38-45. [DOI] [PubMed] [Google Scholar]
- 13.Salinas HM, Broelsch F, Fernandes J et al. Abstract 136: centrifugation compared to a combined mesh/telfa technique for fat grafting: mechanism, outcomes and effect on ADSCs. Plast Reconstr Surg. 2014;133(3 Suppl):152. [DOI] [PubMed] [Google Scholar]
- 14.Coleman SR, Saboeiro AP. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg. 2007;119:775-785. [DOI] [PubMed] [Google Scholar]
- 15.Kaufman MR, Bradley JP, Dickinson B et al. Autologous fat transfer national consensus survey: trends in techniques for harvest, preparation, and application, and perception of short- and long-term results. Plast Reconstr Surg. 2007;119:323-331. [DOI] [PubMed] [Google Scholar]
- 16.Miller JJ, Popp JC. Fat hypertrophy after autologous fat transfer. Ophthal Plast Reconstr Surg. 2002;18:228-231. [DOI] [PubMed] [Google Scholar]
- 17.Spear SL, Coles CN, Leung BK et al. The safety, effectiveness, and efficiency of autologous fat grafting in breast surgery. Plast Reconstr Surg Glob Open. 2016;4(8):e827. ePub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coleman SR. Structural fat grafts: the ideal filler? Clin Plast Surg. 2001;28:111-119. [PubMed] [Google Scholar]
- 19.Gabriel A, Champaneria MC, Maxwell GP. Fat grafting and breast reconstruction: tips for ensuring predictability. Gland Surg. 2015;43:232-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Macario A. What does one minute of operating room time cost? J Clin Anesth. 2010;22:233-236. [DOI] [PubMed] [Google Scholar]
- 21.Jansen LA, Macadam SA. The use of alloderm in postmastectomy alloplastic breast reconstruction: Part II. A cost analysis. Plast Reconstr Surg. 2011;127:2245-2254. [DOI] [PubMed] [Google Scholar]
- 22.Lee LJ, Xu S, Mencer M et al. Effects of autologous fat grafting systems on inpatient operating room time and costs: a hospital budget impact analysis. Presented at the ISPOR 20th Annual International Meeting, May 16-20, 2015, Philadelphia, PA. [Google Scholar]
- 23.Brzezienski MA, Jarrell JA 4th. Autologous Fat Grafting to the Breast Using REVOLVE System to Reduce Clinical Costs. Ann Plast Surg. 2016;773:286–9. [DOI] [PubMed] [Google Scholar]
- 24.Vleggaar D. Soft-tissue augmentation and the role of poly-L-lactic acid. Plast Reconstr Surg. 2006;118:46S–54S. [DOI] [PubMed] [Google Scholar]
- 25.Nguyen PS, Desouches C, Gay AM, Hautier A, Magalon G. Development of micro-injection as an innovative autologous fat graft technique: The use of adipose tissue as dermal filler. J Plast Reconstr Aesthet Surg. 2012;6512:1692-1699. [DOI] [PubMed] [Google Scholar]
- 26.Maas CS, Denton AB. Synthetic soft tissue substitutes: 2001. Facial Plast Surg Clin North Am. 2001;92:219-227, viii. [PubMed] [Google Scholar]
- 27.De Boulle K. Management of complications after implantation of fillers. J Cosmet Dermatol. 2004;31:2-15. [DOI] [PubMed] [Google Scholar]
- 28.Kurita M, Matsumoto D, Shigeura T et al. Influences of centrifugation on cells and tissues in liposuction aspirates: optimized centrifugation for lipotransfer and cell isolation. Plast Reconstr Surg. 2008;121:1033-1041. [DOI] [PubMed] [Google Scholar]
- 29.Delay E, Streit L, Toussoun G et al. Lipomodelling: an important advance in breast surgery. Acta Chir Plast. 2013;55:34-43. [PubMed] [Google Scholar]
- 30.Illouz YG, Sterodimas A. Autologous fat transplantation to the breast: a personal technique with 25 years of experience. Aesthetic Plast Surg. 2009;33:706-715. [DOI] [PubMed] [Google Scholar]
- 31.Niechajev I, Sevcuk O. Long-term results of fat transplantation: clinical and histologic studies. Plast Reconstr Surg. 1994;94:496-506. [DOI] [PubMed] [Google Scholar]
- 32.Zocchi M. Microvascular transplantation of adipose tissue and serum level of adipocyte products. Aesthetic Plast Surg. 2008;32:464. [DOI] [PubMed] [Google Scholar]
- 33.Fisher C, Grahovac TL, Schafer ME et al. Comparison of harvest and processing techniques for fat grafting and adipose stem cell isolation. Plast Reconstr Surg. 2013;132:351-361. [DOI] [PubMed] [Google Scholar]
- 34.Choi M, Small K, Levovitz C et al. The volumetric analysis of fat graft survival in breast reconstruction. Plast Reconstr Surg. 2013;131:185-191. [DOI] [PubMed] [Google Scholar]
- 35.Del Vecchio DA, Del Vecchio SJ. The graft-to-capacity ratio: volumetric planning in large-volume fat transplantation. Plast Reconstr Surg. 2014;133:561-569. [DOI] [PubMed] [Google Scholar]