Abstract
Purpose of the Study:
Lesbian, gay, bisexual, and transgender (LGBT) older adults comprise a diverse and growing health disparate population. In the present study, using the Health Equity Promotion Model, we investigated pathways by which LGBT older adults experience resilience, risk, and marginalization and their relationship to attaining positive health outcomes.
Design and Methods:
Aging with Pride: National Health, Aging, and Sexuality/Gender Study (NHAS) is the first longitudinal research project designed to examine the health, aging, and well-being of LGBT adults aged 50 and older. Using data from 2014 (N = 2,415), we tested a structural equation model linking lifetime marginalization, identity affirmation and management, social and psychological resources, and health behaviors to positive health outcomes.
Results:
Identity affirmation positively predicted social resources and mental health, and social resources positively predicted mental health. Marginalization was associated with fewer social resources for LGBT older adults with an open identity management style, lower identity affirmation for LGBT older adults who strategically concealed their sexual identity, and poorer mental health. Mental health was associated with better health behaviors, which in turn predicted positive physical health outcomes.
Implications:
Although a health disparate population, good health among LGBT older adults appears to be attained via multiple resilience and risk pathways. Providers must remain aware of the historical contexts in which LGBT older adults lived and the strengths they developed in order to understand their health and to develop tailored and targeted prevention and intervention services.
Keywords: Sexual minority, Health, Equity, Resilience, Strengths, Disparities
Along with the increasing diversity of the aging population, the number of lesbian, gay, bisexual, and transgender (LGBT) older adults is growing rapidly: Currently 2.7 million U.S. adults aged 50 and older self-identify as LGBT (Fredriksen-Goldsen & Kim, 2015), a figure that will likely exceed 5 million by 2060 (Fredriksen-Goldsen & Kim, 2017). A growing body of research has documented mental and physical health disparities among LGBT older adults compared with older adults in the general population (Fredriksen-Goldsen, Cook-Daniels, et al., 2014; Fredriksen-Goldsen, Kim, Barkan, Muraco, & Hoy-Ellis, 2013; Fredriksen-Goldsen, Shiu, et al., in press; Wallace, Cochran, Durazo, & Ford, 2011). Yet, despite disparities, most LGBT older adults enjoy good health and supportive social relationships, are connected to their communities, engage in health-promoting behaviors, and are satisfied with their lives (Fredriksen-Goldsen, Kim, Shiu, Goldsen, & Emlet, 2015), showing resilience in the face of adversity and historical marginalization.
Although several key risk factors for physical and mental health problems have been identified among LGBT older adults, to date, we know little about the mechanisms linking experiences, behavior, and psychological and social resources with positive health outcomes in these communities. Understanding these mechanisms is critical to identify strengths that may be harnessed to promote optimal aging among LGBT older adults. In the present study, we utilized a health equity life-course approach to investigate key protective and risk-related mechanisms contributing to positive health outcomes among LGBT older adults.
Conceptual Framework: The Health Equity Promotion Model
Although most sexual and gender minority research has been guided by stress and coping models (Hatzenbuehler, Nolen-Hoeksema, & Dovidio, 2009; Meyer, 2003), the Health Equity Promotion Model (HEPM; Fredriksen-Goldsen, Simoni, et al., 2014) situates health more broadly within the life course, asserting that optimal aging is linked to the availability over time of opportunities that promote health. This model highlights how (a) social positions and (b) structural and environmental contexts intersect across the life course with (c) health-promoting and risk processes (psychological, social, behavioral, and biological) to culminate in the health and well-being of LGBT adults as they age. Based on the HEPM, in the present study, we examined whether, and to what extent, psychological, social, and behavioral processes predict health outcomes among LGBT older adults. We also investigated how marginalization influences these processes by serving as a barrier to opportunities for securing health-relevant resources. Here, we review what is known about these components of the HEPM as they relate to the health of LGBT older adults.
Historical and Environmental Context
The HEPM incorporates systemic, structural, and interpersonal forms of marginalization and social exclusion, which can systematically and institutionally disadvantage LGBT people across the life course (Hatzenbuehler et al., 2009). LGBT older adults came of age in an era when same-sex behavior and gender nonconformity were severely stigmatized and/or criminalized, and they report high rates of lifetime victimization and discrimination (Fredriksen-Goldsen, Cook-Daniels, et al., 2014; Fredriksen-Goldsen, Emlet, et al., 2013; Herek, 2009). Day-to-day marginalization, including microaggressions (Sue et al., 2007), has been found to be strongly associated with psychological distress (Szymanski, 2006; Woodford, Chonody, Kulick, Brennan, & Renn, 2015; Wright & Wegner, 2012) and poor mental and physical health outcomes (see review, Pascoe & Smart Richman, 2009). For some LGBT older adults, these adverse experiences may serve as a barrier against opportunities to attain optimal health. At the same time, many faced with marginalization and adversity exercise resilience, which is associated with good health and access to psychological and social resources (Fredriksen-Goldsen, Kim, et al., 2015).
Psychological Resources
We conceptualize identity appraisal as the evaluation of the perceived value of one’s LGBT identity, which may be influenced by experiences of marginalization as well as by the historical and environmental contexts in which one has lived. A positive identity appraisal (i.e., identity affirmation) has been associated with greater well-being, life satisfaction, and social connectedness, and less negative affect (Kertzner, Meyer, Frost, & Stirratt, 2009; Mayfield, 2001; Mohr & Kendra, 2011; Riggle, Mohr, Rostosky, Fingerhut, & Balsam, 2014). Research, however, has not adequately investigated the associations between identity affirmation and physical health among LGBT older adults. A negative identity appraisal (i.e., identity stigma), on the other hand, is thought to result when individuals internalize societal prejudice against sexual and gender minorities (Herek, Gillis, & Cogan, 2015), which has been associated with social constraints (Frost & Meyer, 2009), mental health problems (Newcomb & Mustanski, 2010), and physical health symptoms (Lewis, Derlega, Clarke, & Kuang, 2006).
Regardless of the valence of their identity appraisal, LGBT older adults may employ a variety of styles for managing the disclosure or nondisclosure of their LGBT identity to others (Lance, Anderson, & Croteau, 2010). The influence of marginalization on identity appraisal and social resources may differ depending on identity management style. For example, open disclosure of LGBT identity may expose a person to discrimination, but may also help them connect to identity-affirming support networks (Erosheva, Kim, Emlet, & Fredriksen-Goldsen, 2016). Some LGBT individuals, on the other hand, may strategically conceal their identity to protect themselves from discrimination (Newheiser & Barreto, 2014). There is evidence that managing one’s identity openly (i.e., having a high level of outness) is associated with better psychological well-being (Legate, Ryan, & Weinstein, 2012), but we know little about how different identity management styles are associated with physical health. This is the first study to fully examine how identity appraisal and identity management contribute to health outcomes among LGBT older adults.
Social Resources
Social connectedness, which provides emotional, instrumental, and financial support, is strongly associated with mental and physical health in the general older adult population (Cornwell & Waite, 2009). For instance, participation in social activities, such as volunteering and religious activities, is associated with mental and physical health (Anaby, Miller, Jarus, Eng, & Noreau, 2011; Tang, 2008), as is being partnered or married (see review, Manzoli, Villari, Pirone, & Boccia, 2007). Similar health benefits of social connectedness exist among LGBT older adults, including partnership status (Williams & Fredriksen-Goldsen, 2014) and size of social network and level of social support (Masini & Barrett, 2008), but social contexts and availability of social resources may differ; for example, sexual minority older adults are less likely to be married and less likely to have children than heterosexuals of similar age (Fredriksen-Goldsen, Kim, et al., 2013) and are much more likely to rely heavily on extended kin, such as partners, close friends, and ex-partners (Fredriksen, 1999; Fredriksen-Goldsen, Kim, Muraco, & Mincer, 2009; Muraco & Fredriksen-Goldsen, 2011). The processes linking these differences with health outcomes, however, are not yet well understood.
Mental Health
Mental health research with LGBT older adults has focused primarily on the associations between risk factors and mental health problems. To fully understand mental health, however, both the absence of mental illness and the presence of psychological well-being need to be considered (Westerhof & Keyes, 2010). Moreover, in order to understand and promote health equity of LGBT older adults, it is necessary to understand the influence mental health has on physical health. In the general older adult population, several studies have documented psychological distress and high levels of stress as predictors of poor physical health (Graham, Christian, & Kiecolt-Glaser, 2006; Paul, Ayis, & Ebrahim, 2006). There is also accumulating literature documenting how poor mental health may relate to health-risk behaviors among sexual minority individuals (Kamen et al., 2014), although this has not been investigated among LGBT older adults. Yet, to date, little remains known about how good mental health may promote physical health in LGBT older adults.
Health Behaviors
Health behaviors are related to mental health and can maintain or change physical health. In this study, we examined both health-promoting and health-risk behaviors. Previous studies have primarily focused on health-risk behaviors among LGBT older adults, including limited physical activity and smoking, which are associated with poor general health and disability (Fredriksen-Goldsen, Emlet, et al., 2013) and lower physical and mental health quality of life (Fredriksen-Goldsen, Kim, et al., 2015). In the general population, poor mental health, such as increased distress, is associated with increased likelihood of health-risk behaviors, including smoking (Lawrence & Williams, 2016). However, these processes have not yet been investigated in LGBT older adults nor has the interplay of mental and physical health with health-promoting (rather than health-risk) behaviors.
Physical Health
Physical health, a multidimensional construct, incorporates physical functioning and general perceived health status as well as the presence or absence of disability and chronic conditions and diseases (Johnson & Wolinsky, 1993). Although previous studies of physical health in LGBT older adults have focused on negative health outcomes (Fredriksen-Goldsen, Kim, et al., 2013; Wallace et al., 2011), here we examined how mechanisms of resilience and risk lead to positive physical health. Existing literature suggests a complex network of pathways that operate across the life span to culminate in healthy old age. The goal of the present study was to investigate and synthesize the mechanisms associated with good health in a national sample of LGBT older adults.
Hypotheses
(a) Identity affirmation and social resources, as protective factors, will be positively associated with mental health; (b) marginalization, as a risk factor, will be associated with lower levels of identity affirmation and social resources, accounting in part for the negative relationship between marginalization and mental health; (c) health-promoting and health-risk behaviors will mediate the relationship between mental and physical health, with health-promoting behaviors being associated with better physical health; and (d) identity management style will moderate the relationship of marginalization with identity affirmation and social resources; specifically, for LGBT older adults who conceal their identities, marginalization will be negatively associated with identity affirmation and social resources.
Design and Methods
Sample Characteristics
Of 2,450 participants who participated in Aging with Pride: National Health, Aging, and Sexuality/Gender Study (NHAS), 2,415 participants were included in the present analysis (age range: 50–98 years); 35 participants were excluded because of missing data. This longitudinal study investigates the life-course experiences, health, aging, and well-being of LGBT older adults; here, we report a cross-sectional analysis of the 2014 data. The inclusion criteria were being born in 1964 or earlier and self-identifying as LGBT or as someone who was engaged in same-sex sexual behavior, or attracted to or who had a romantic relationship with someone of the same sex or gender. Participants were recruited utilizing a dual sampling frame (aging agency lists across all U.S. Census divisions and social network clustering chain referral), stratifying by cohort, gender, race/ethnicity, and geographic location. The social network clustering chain referral was utilized to recruit LGBT older adults who were not affiliated with aging agencies and to meet the stratification goal. Paper and online surveys were completed according to each participant’s preference. Participants were compensated $20 for their time.
Measures
Marginalization
Marginalization was modeled as a latent variable with four indicators: lifetime victimization, lifetime discrimination, day-to-day discrimination, and microaggressions (Fredriksen-Goldsen & Kim, 2017). This study assessed lifetime victimization with a scale asking about the frequency of lifetime LGBT victimization experiences (nine items, e.g., “I was threatened with physical violence”; 0 = Never, 3 = 3 or more times), and lifetime discrimination related to LGBT identities was measured with five items (e.g., “I was not hired for a job”; 0 = Never, 3 = 3 or more times). Summed scores were computed for the two scales, ranging from 0 to 27 for victimization and from 0 to 15 for discrimination, with a higher score indicating more lifetime experiences (α = .85 and α = .77, respectively). Day-to-day discrimination (being treated with less respect due to one or more minority statuses) was assessed with six items (adapted from Williams, Yu, Jackson, & Anderson, 1997) measuring frequency of experiences. Items included, “People do things that devalue and humiliate you” (0 = Never, 5 = Almost every day) with α = .91. Microaggressions related to LGBT identities assessed three domains, including microinvalidation/insult, microassault, and hostile environment, with eight items asking about the frequency of experiences such as “People use derogatory terms to refer to LGBT individuals in your presence” (0 = Never, 5 = Almost every day) with α = .85. The sums of the lifetime victimization and discrimination scales and the means of the day-to-day discrimination and microaggressions scales served as indicators for the latent variable with standardized factor loadings of .69, .74, .76, and .55, respectively.
Psychological Resources
Psychological resources were assessed using latent variables for identity appraisal and management. Identity appraisal was modeled as a latent variable with two indicators: identity affirmation and identity stigma (Fredriksen-Goldsen & Kim, 2017). Identity affirmation was assessed with the mean of four items (1 = Strongly disagree, 6 = Strongly agree), for example, “I am proud to be LGBT” (α = .81). Identity stigma was also assessed with the mean of four items regarding negative attitudes, for example, “I feel ashamed of myself for being LGBT” (α = .83), which were reverse coded so that higher scores on the latent variable indicate greater identity affirmation. Standardized factor loadings were .85 and .78, respectively.
Aging with Pride: NHAS assessed identity management styles for expressing one’s sexual and/or gender identity to others. The scale consists of nine items including explicitly expressing one’s sexual or gender identity (e.g., “When people assume that I’m not LGBT, I correct them”), passively expressing one’s LGBT identity (e.g., “I display objects (magazines, symbols) that suggest my sexual orientation or gender identity”), and concealing one’s identity (e.g., “I make comments to give the impression that I am not LGBT”), each rated on a 6-point Likert scale (1 = Strongly disagree, 6 = Strongly agree). Clusters of participants endorsing similar patterns of identity management styles were identified separately using latent class analysis, which revealed two underlying clusters: Participants who used consistent open identification as their primary identity management style (coded 0), who were characterized by high ratings of explicit items, moderate ratings of passive items, and low ratings of concealing items; those who used strategic concealment (coded 1), who were characterized by low-to-moderate ratings on items across all three dimensions.
Social Resources
Level of social resources was modeled as a latent variable encompassing four related constructs: perceived social support (abbreviated MOS-Social Support Scale; Gjesfjeld, Greeno, & Kim, 2008; Sherbourne & Stewart, 1991), measured as the mean of four items regarding availability of support (e.g., “Someone to help with daily chores if you were sick”; 0 = Never, 4 = Very often; α = .86); social participation (Fredriksen-Goldsen & Kim, 2017), measured as the mean frequency of engaging in seven different social activities over the past month (e.g., talking on the phone, socializing with friends or family; 1 = Never, 5 = Every day; α = .70); community engagement (Fredriksen-Goldsen & Kim, 2017), measured as the mean of four items regarding relationship with the LGBT community (e.g., “I feel part of the community”; 1 = Strongly disagree, 6 = Strongly agree; α = .86); and relationship status, measured by the single item “What is your current relationship status?” (0 = Single, 1 = Partnered or married). Each construct was used as an indicator for the latent variable with standardized factor loadings of .84, .45, .35, and .73, respectively.
Mental Health
Mental health was modeled as a latent variable with three indicators, including positive affect, negative affect, and perceived stress. The means of two subscales, which assess frequency of positive affect (two items, e.g., “I felt hopeful about the future”; α = .74) and negative affect (eight items, e.g., “I felt that everything I did was an effort”; α = .84) over the past week (0 = Less than 1 day, 3 = 5–7 days), were used from the short form of Center for Epidemiological Studies-Depression scale (Andresen, Malmgren, Carter, & Patrick, 1994). Perceived stress was measured as the mean of the four-item Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983), which assesses frequency and ability to cope with perceived psychological stressful experiences over the past 30 days, such as “How often have you felt that things were going your way?” and “How often have you felt that you were unable to control the important things in your life?” (1 = Never, 5 = Fairly often; α = .81). Items assessing positive affect were not reverse coded; negative affect and perceived stress were reverse coded with higher scores indicating more positive mental health. Each mean was used as an indicator for the latent variable with standardized factor loadings of .86, .79, and .69, respectively.
Health Behavior
Health-promoting behavior was measured as a latent variable with three indicators: number of days per typical week engaging in moderate physical activity; number of days per typical week engaging in vigorous physical activity; and number of days per typical week engaging in leisure or other wellness activities (Fredriksen-Goldsen & Kim, 2017). Standardized factor loadings were .69, .57, and .31, respectively. Health-risk behavior was measured as a latent variable with two indicators: current smoking (0 = No, 1 = Yes) and frequency of experiencing insufficient food intake (1 = Never, 5 = Always). Standardized factor loadings were .40 and .65, respectively.
Physical Health
Physical health, as a multidimensional construct (Johnson & Wolinsky, 1993), was modeled as a latent variable with five indicators (Fredriksen-Goldsen & Kim, 2017), coded so that higher scores on the latent variable indicate better physical health: physical functioning, the mean of eight items measuring lower and upper extremity performance (1 = Extreme difficulty or cannot do, 5 = No difficulty; α = .90); ability to perform activities of daily living (ADLs and instrumental ADLs) measured by the means of six and five items, respectively (1 = Extreme difficulty or cannot do, 5 = No difficulty; α = .89 and .77); general health, measured by a single item rating overall health (1 = Poor, 5 = Excellent); and number of chronic health conditions including heart attack, heart disease, high blood pressure, arthritis, osteoporosis, diabetes, lung disease, stroke, dementia or Alzheimer’s disease, and cancer (Brault, 2008; Freedman, Schoeni, Martin, & Cornman, 2007) as well as HIV/AIDS. Standardized factor loadings were .39, .82, .80, .79, and .67, respectively.
Demographic and Background Characteristics
Control covariates included age in years; gender (1 = Male); sexual orientation (1 = Gay or lesbian); race/ethnicity (1 = Non-Hispanic White); education (1 = More than high school); and income (1 = Above 200% of federal poverty level [FPL]).
Data Analytic Strategy
In order to reduce sampling bias and increase the generalizability of the findings, we applied survey weights to statistical analyses. Survey weights were computed utilizing three external probability samples’ data as benchmarks following two-step postsurvey adjustment, as has been applied to other types of nonprobability samples (Lee, 2006; Lee & Valliant, 2009). In the first step, the Aging with Pride: NHAS sample was combined with the National Health Interview Survey (NHIS) sample ascertaining sexual orientation by sexual identity, and we computed the probability of being selected from the NHIS versus the Aging with Pride: NHAS sample by using a logistic regression model with age, sex, sexual orientation, Hispanic ethnicity, race, education, region, and home ownership as covariates. In the second step, we further calibrated the weights for those in same-sex partnerships, another indicator of sexual orientation. The population totals by age, race/ethnicity, gender, education, marital status, and region were estimated from the NHIS, the American Community Survey (ACS), and the Health and Retirement Study (HRS). See Fredriksen-Goldsen and Kim (2017) for detailed information regarding the postsurvey adjustment procedures. All study procedures and materials were approved by the Human Subjects Division of University of Washington.
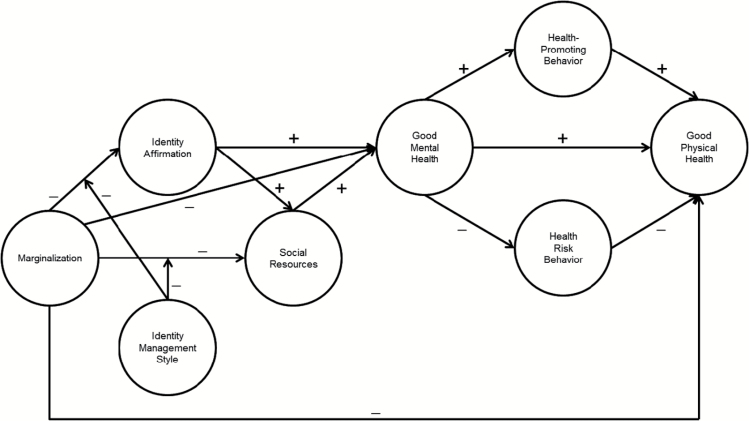
Distributions of study variables were examined and bivariate correlations were computed between study variables. We tested the hypotheses using structural equation modeling, conducted in Mplus version 7.4 (Muthén & Muthén, 1998–2015). Latent variables were first constructed separately using confirmatory factor analysis to ensure good fit between measurement models and the data. The hypothesized structural model (Figure 1) was then fitted to the data using maximum likelihood estimation with robust standard errors (MLR estimator in Mplus). Model fit was assessed with two steps. First, because absolute fit statistics (e.g., chi square) are unavailable for models containing latent variable interactions, a nested model with no interaction term was computed using a weighted least squares estimator to obtain indices of absolute model fit (Mooijaart & Satorra, 2012). Second, relative fit statistics (Akaike information criterion, Bayesian information criterion, and log likelihood) were compared between the nested model (recomputed with MLR estimator) and the hypothesized (latent interaction) model to determine whether including the interactions significantly improved model fit. Although this does not provide a perfect test of absolute model fit because different estimators are used, it provides the strongest available evidence to assess the hypothesized model.
Figure 1.
Hypothesized structural equation model. For ease of interpretation, observed indicators of latent variables are not displayed.
Significant moderation effects were probed, and indirect effects were computed using bias-corrected bootstrapping to generate confidence intervals (CIs). Indirect effects with moderated pathways were computed conditionally (i.e., separately for participants with different identity management styles). All models were computed controlling for the effects of age, gender, sexual orientation, race/ethnicity, education, and income.
Results
Weighted estimates of demographic characteristics are shown in Table 1. LGBT older adults were demographically diverse. Twenty-two percent were people of color, and half were male. Seventeen percent were transgender. Although most identified their sexual orientation as gay or lesbian, 17% were bisexual older adults. Approximately three quarters had more than a high school education; nearly 30% were living at or below 200% FPL. Approximately half were currently employed. Bivariate correlations among continuous latent variables are shown in Table 2. All were significant and in the expected directions.
Table 1.
Demographic Characteristics (N = 2415)
| Variable | Mean (SD) or % |
|---|---|
| Gender | |
| Female | 43.17% |
| Male | 50.76% |
| Other | 6.06% |
| Transgender | 16.6% |
| Sexual orientation | |
| Gay or lesbian | 72.49% |
| Bisexual | 17.19% |
| Other | 10.32% |
| Age in years | 61.45 (12.07) |
| Race/ethnicity, non-Hispanic White | 78.05% |
| Education, >high school | 74.68% |
| Income, >200% FPL | 71.43% |
| Currently employed | 48.15% |
Note: FPL = federal poverty level. Weighted estimates are presented.
Table 2.
Estimated Correlations Among Continuous Latent Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|
| 1. Marginalization | — | ||||||
| 2. Identity affirmation | −.099* | — | |||||
| 3. Social resources | −.186** | .303** | — | ||||
| 4. Mental health | −.384** | .295** | .575** | — | |||
| 5. Health-promoting behavior | −.137** | .074** | .175** | .344** | — | ||
| 6. Health-risk behavior | .250** | −.213** | −.442** | −.710** | −.219** | — | |
| 7. Physical health | −.303** | .174** | .373** | .573** | .378** | −.645** | — |
Note: Weighted estimates are presented.
*p < .05; **p < .01.
Model Selection
Absolute model fit for a nested model with no interaction term was acceptable (χ2(298) = 338.52, p = .053; root mean square error of approximation = 0.008 [90% CI = 0.00–0.01]; comparative fit index = 0.994; Tucker–Lewis index = 0.990). Comparisons of log likelihoods, which can be used to estimate chi-square difference tests of relative fit between nested models, indicated the moderating effect of identity management styles significantly improved model fit over the nested model (χ2 difference(4) = 134.74, p < .01), suggesting acceptable absolute fit for the hypothesized model as well.
Structural Equation Modeling
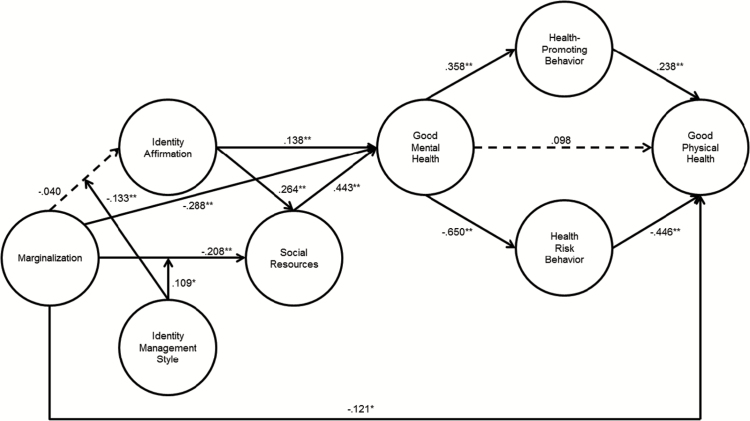
The final fitted model is shown in Figure 2. Identity affirmation positively predicted social resources and mental health, and social resources positively predicted mental health. Marginalization negatively predicted social resources, mental health, and physical health. Contrary to predictions, the negative main effect of marginalization on identity affirmation was nonsignificant (however, see Moderating Effects of Identity Management Style section). Mental health did not directly predict better physical health as expected; however, it did predict more health-promoting behavior and less health-risk behavior, which in turn were associated positively and negatively, respectively, with physical health.
Figure 2.
Final fitted structural equation model. Dashed lines indicate nonsignificant paths. All estimates are standardized and weighted. For ease of interpretation, observed indicators of latent variables are not displayed. *p < .05; **p < .01.
Proportions of explained variance for the dependent latent variables in the model were as follows: 31.4% for identity affirmation, 23.5% for social resources, 47.1% for mental health, 14.5% for health-promoting behavior, 59.1% for health-risk behavior, and 56.1% for physical health.
Moderating Effects of Identity Management Style
Identity management style significantly moderated the path from marginalization to identity affirmation. Although there was no significant main effect of marginalization on identity affirmation, the interaction revealed that the effect was, in fact, significant and negative for participants with the strategic concealing identity management style, such that those with greater marginalization had a lower level of identity affirmation.
There was also a moderating effect of identity management style on the path from marginalization to social resources. The negative main effect of marginalization on social resources was significant, but the interaction revealed that it was significant only for those with the open identity management style: For those participants, but not for participants with the strategic concealing identity management style, marginalization was negatively associated with social resources.
Indirect Effects
When indirect effects linking marginalization to physical health were examined (Table 3), unconditional and conditional pathways were significant. The unconditional pathway linked mental health to physical health via health-promoting and health-risk behaviors while marginalization was negatively associated with mental health. The conditional pathways showed that the mechanisms between marginalization and mental health differ by identity management strategy. For participants with the open identity management style, the pathways via social resources, mental health, and health-promoting and health-risk behaviors were significant. For participants with the conceal identity management style, the pathways via identity affirmation, mental health, and health-promoting and health-risk behaviors as well as via identity affirmation, social resources, mental health, and health-promoting and health-risk behaviors were significant.
Table 3.
Indirect Effects Linking Marginalization and Physical Health
| Unconditional indirect effects | Estimate | 95% CI | ||
|---|---|---|---|---|
| Marginalization → mental health → physical health | −0.042 | −0.148, 0.066 | ||
| Marginalization → mental health → health-promoting behavior → physical health | −0.037 | −0.066, −0.014 | ||
| Marginalization → mental health → health-risk behavior → poor physical health | −0.125 | −0.272, −0.028 | ||
| Conditional indirect effects | Opena: Estimate | Opena: 95% CI | Concealb: Estimate | Concealb: 95% CI |
| Marginalization → identity affirmation → mental health → physical health | −0.001 | −0.006, 0.002 | −0.008 | −0.036, 0.012 |
| Marginalization → identity affirmation → mental health → health-promoting behavior → physical health | −0.001 | −0.003, 0.001 | −0.007 | −0.017, −0.001 |
| Marginalization → identity affirmation → mental health → health-risk behavior → physical health | −0.002 | −0.009, 0.002 | −0.024 | −0.062, −0.003 |
| Marginalization → social resources →mental health → physical health | −0.014 | −0.054, 0.019 | 0.006 | −0.020, 0.037 |
| Marginalization → social resources → mental health → health-promoting behavior → physical health | −0.012 | −0.024, −0.003 | 0.005 | −0.009, 0.021 |
| Marginalization → social resources → mental health → health-risk behavior → physical health | −0.040 | −0.087, −0.008 | 0.017 | −0.033, 0.075 |
| Marginalization → identity affirmation → social resources → mental health → physical health | −0.001 | −0.005, 0.002 | −0.007 | −0.027, 0.012 |
| Marginalization → identity affirmation → social resources → mental health → health-promoting behavior → physical health | −0.001 | −0.002, 0.001 | −0.006 | −0.015, −0.001 |
| Marginalization → identity affirmation → social resources → mental health → health-risk behavior → physical health | −0.002 | −0.008, 0.004 | −0.020 | −0.057, −0.003 |
Note: CI = confidence interval. Significant indirect effects (i.e., those whose confidence interval excludes zero) appear in bold. Weighted estimates are presented.
aOpen = open identity management style. bConceal = strategic concealing identity management style.
Discussion
The purpose of this study was to investigate, based on the HEPM, how the interplay of psychological, social, and behavioral processes contributes to physical health among LGBT older adults. We identified a direct association between marginalization and physical health and delineated multiple indirect pathways to explain the association. As hypothesized, identity affirmation and social resources contributed positively to mental health, which in turn predicted physical health via health behaviors. We also characterized the moderating role of identity management style on the associations of marginalization with psychological and social resources. This analysis provides support for the HEPM as a framework for investigating diverse pathways culminating in the health of LGBT older adults, highlighting multiple mechanisms of resilience and risk. Previous studies have rarely identified mechanisms that lead to good health enjoyed by older adults in marginalized populations.
Identity affirmation has not been adequately addressed in previous research of LGBT older adults. Social identity theorists argue that positive identity appraisal is related to affirmative feelings of one’s group membership and identity pride (Phinney & Ong, 2007). In studies of race and ethnicity, identity affirmation has been associated with psychological resources. For example, self-affirmation is associated with self-regulatory strengths (Schmeichel & Vohs, 2009) and identity affirmation negatively associated with mental health problems (Hughes, Kiecolt, Keith, & Demo, 2015). Similarly, we found that identity affirmation was associated with positive mental health. This study suggests that affirmation of one’s sexual or gender identity warrants further attention as a component of protective pathways leading to good health and promoting health equity. For instance, our findings suggest that identity affirmation may be instrumental for LGBT older adults to access social resources, which in turn, as hypothesized, promoted good mental and physical health.
As we hypothesized, good mental health was associated with good physical health through its effects on health-promoting and health-risk behaviors. Good mental health was positively associated with health-promoting behaviors, including physical and leisure activities, and negatively associated with health-risk behaviors, including smoking and insufficient food intake. Such behaviors, and the mental health considerations that influence them, are promising targets both for identifying LGBT older adults at risk for deteriorating health and for the development of community-based interventions designed to improve health in high-risk subgroups.
As hypothesized, marginalization, as a life-course risk factor, was negatively linked to social resources and to mental health, consistent with strong evidence from prior research that victimization and discrimination contribute to poor mental health among sexual (Meyer, 2003) and gender (Rood, Puckett, Pantalone, & Bradford, 2015) minorities and more specifically among LGBT older adults (Emlet, Fredriksen-Goldsen, & Kim, 2013; Fredriksen-Goldsen, Emlet, et al., 2013). We also found that higher levels of marginalization were directly negatively associated with good physical health, consistent with other studies in this population supporting a strong and deleterious association between marginalization and physical health (Andersen, Hughes, Zou, & Wilsnack, 2014; Fredriksen-Goldsen, Emlet, et al., 2013; Fredriksen-Goldsen, Kim, et al., 2015). In this study, we utilized a multidimensional measurement of marginalization by incorporating measures of both lifetime adverse experiences and ongoing adversity, including day-to-day discrimination across marginalized identities, as well as LGBT-specific microaggressions. Particularly, as policies and cultural attitudes surrounding LGBT identities continue to shift, in future longitudinal studies it will be beneficial to continue to investigate various forms of marginalization and their differential impact on the mental and physical health of LGBT older adults.
As hypothesized, we found that individuals with different identity management styles carried different mechanisms of risk and resilience linking marginalization with health outcomes. In the relationship between marginalization and social resources, higher marginalization predicted significantly lower social resources, but only for those with an open identity management style. In discriminatory contexts, those who are highly visible as LGBT may be ostracized or have limited access to supportive communities. For those who strategically concealed their identity, on the other hand, marginalization was not significantly associated with social resources, suggesting that concealing (at least some of the time) may have been protective for LGBT older adults, especially within the historical and environmental context of their lives. This finding runs counter to other research findings showing, for example, that concealing one’s sexual identity is linked to a higher likelihood of living alone among older sexual minorities (Kim & Fredriksen-Goldsen, 2016), whereas being out to friends and neighbors predicts larger social networks among older LGBT older adults (Erosheva et al., 2016). Clearly, additional research is needed to understand the complexities of different identity management styles and their interplay with diverse social contexts.
The effect of marginalization on identity affirmation was also conditional on identity management style: The negative path from marginalization to identity affirmation was only significant for those who concealed their sexual identities. This moderation effect is notable given the large body of research indicating that discrimination experiences predict higher levels of internalized stigma and shame based on one’s sexual or gender minority identity. For example, Emlet (2006) found that among those living with HIV, both institutional and social discrimination emerged as factors contributing to older adults’ HIV-related perceived stigma. Although most literature argues that openly identifying as a sexual or gender minority is associated with good health, in the case of heightened vulnerabilities (e.g., frailty or poor health), it may be associated with worse health outcomes. Taken together, our findings regarding the moderating effects of identity management style suggest that strategically concealing one’s LGBT identity in environments one knows or suspects to be hostile toward sexual or gender minorities may be socially protective for LGBT older adults, but also may take a toll personally, whereas being consistently open may be psychologically protective but take a social toll.
Although this study identified key mechanisms associated with the health of LGBT older adults, the findings were based on cross-sectional data from a single survey wave, and conclusions about causal associations are not warranted. In future research incorporating longitudinal data, we will be able to address change in health over time and the temporal nature of factors associated with change. In this study, we reduced sampling bias by using survey weights based on population-based estimates. However, some bias still remains that should be considered in the interpretation of these findings; some segments of the population are especially hard to reach (e.g., those who are not connected to aging agencies and have few or no LGBT peers), and although we used multiple means to reach such hidden-within-hidden populations, they still may not have been adequately captured in our sampling strategy. In addition, there are likely additional predictors of health outcomes that were outside the scope of this study. For example, genetic and other biological risk factors associated with health problems were not taken into account in these analyses. Notably, the direct path from marginalization to health outcomes remained significant after accounting for several indirect pathways, suggesting additional mechanisms are at play and should be investigated in future research. For example, biological responses to chronically stressful conditions (e.g., elevated cortisol) may explain part of the association between marginalization and physical health. In future work using multiple waves of longitudinal data, including biological measures, we will be able to address these and other important questions.
Conclusion
This study revealed that psychological and social resources were associated with better mental health, which in turn fostered health-promoting behavior and good physical health among LGBT older adults. These indirect paths illuminate the strengths that help many LGBT older adults remain resilient and in good health even in marginalizing contexts. Furthermore, this study sets the stage for future longitudinal investigation of how LGBT older adults’ protective and risk factors are associated with their health trajectories over time as they age. The findings presented in this study suggest that tailored interventions promoting identity affirmation and strategic identity management as well as psychological, social, and behavioral resources need to be developed to promote optimal health of LGBT older adults. Future waves of longitudinal data will help us to comprehensively examine mechanisms underlying sexual and gender minority health inequities in older age, an important step toward successful health promotion in older adult populations.
Funding
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG026526 (K. I. Fredriksen-Goldsen, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Anaby D. Miller W. C. Jarus T. Eng J. J., & Noreau L (2011). Participation and well-being among older adults living with chronic conditions. Social Indicators Research, 100, 171–183. doi:10.1007/s11205-010-9611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen J. P. Hughes T. L. Zou C., & Wilsnack S. C (2014). Lifetime victimization and physical health outcomes among lesbian and heterosexual women. PLoS One, 9, e101939. doi:10.1371/journal.pone.0101939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andresen E. M. Malmgren J. A. Carter W. B., & Patrick D. L (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). American Journal of Preventive Medicine, 10, 77–84. [PubMed] [Google Scholar]
- Brault M. (2008). Americans with disabilities: 2005 (Current Population Reports, P70-117). Retrieved from http://www.census.gov/prod/2008pubs/p70-117.pdf
- Cohen S. Kamarck T., & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. [PubMed] [Google Scholar]
- Cornwell E., & Waite L (2009). Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior, 50, 31–48. doi:10.1177/002214650905000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emlet C. A. (2006). “You’re awfully old to have this disease”: Experiences of stigma and ageism in adults 50 years an older living with HIV/AIDS. The Gerontologist, 46, 781–790. doi:10.1093/geront/46.6.781 [DOI] [PubMed] [Google Scholar]
- Emlet C. A. Fredriksen-Goldsen K. I., & Kim H. J (2013). Risk and protective factors associated with health-related quality of life among older gay and bisexual men living with HIV disease. The Gerontologist, 53, 963–972. doi:10.1093/geront/gns191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erosheva E. A. Kim H. J. Emlet C., & Fredriksen-Goldsen K. I (2016). Social networks of lesbian, gay, bisexual, and transgender older adults. Research on Aging, 38, 98–123. doi:10.1177/0164027515581859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen K. I. (1999). Family caregiving responsibilities among lesbians and gay men. Social Work, 44, 142–155. doi:10.1093/sw/44.2.142 [DOI] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. Cook-Daniels L. Kim H. J. Erosheva E. A. Emlet C. A. Hoy-Ellis C. P.,…Muraco A (2014). Physical and mental health of transgender older adults: An at-risk and underserved population. The Gerontologist, 54, 488–500. doi:10.1093/geront/gnt021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. Emlet C. A. Kim H. J. Muraco A. Erosheva E. A. Goldsen J., & Hoy-Ellis C. P (2013). The physical and mental health of lesbian, gay male, and bisexual (LGB) older adults: The role of key health indicators and risk and protective factors. The Gerontologist, 53, 664–675. doi:10.1093/geront/gns123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I., & Kim H. J (2015). Count me in: Response to sexual orientation measures among older adults. Research on Aging, 37, 464–480. doi:10.1177/0164027514542109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I., & Kim H.-J (2017). The science of conducting research with LGBT older adults—An introduction to Aging with Pride: National Health, Aging, and Sexuality/Gender Study. The Gerontologist, 57, S1-S14. doi:10.1093/geront/gnw212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. Kim H. J. Barkan S. E. Muraco A., & Hoy-Ellis C. P (2013). Health disparities among lesbian, gay, and bisexual older adults: Results from a population-based study. American Journal of Public Health, 103, 1802–1809. doi:10.2105/AJPH.2012.301110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. Kim H. J. Muraco A., & Mincer S (2009). Chronically ill midlife and older lesbians, gay men, and bisexuals and their informal caregivers: The impact of the social context. Sexuality Research & Social Policy, 6, 52–64. doi:10.1525/srsp.2009.6.4.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. Kim H. J. Shiu C. Goldsen J., & Emlet C. A (2015). Successful aging among LGBT older adults: Physical and mental health-related quality of life by age group. The Gerontologist, 55, 154–168. doi:10.1093/geront/gnu081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. Shiu C. Bryan A. E. B. Goldsen J., & Kim H.-J (in press). Health equity and aging of bisexual older adults: Pathways of risk and resilience. Journal of Gerontology: Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. Simoni J. M. Kim H. J. Lehavot K. Walters K. L. Yang J.,…Muraco A (2014). The Health Equity Promotion Model: Reconceptualization of lesbian, gay, bisexual, and transgender (LGBT) health disparities. The American Journal of Orthopsychiatry, 84, 653–663. doi:10.1037/ort0000030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman V. A. Schoeni R. F. Martin L. G., & Cornman J. C (2007). Chronic conditions and the decline in late-life disability. Demography, 44, 459–477. [DOI] [PubMed] [Google Scholar]
- Frost D. M., & Meyer I. H (2009). Internalized homophobia and relationship quality among lesbians, gay men, and bisexuals. Journal of Counseling Psychology, 56, 97–109. doi:10.1037/a0012844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjesfjeld C. Greeno C., & Kim K (2008). A confirmatory factor analysis of an abbreviated social support instrument: The MOS-SSS. Research on Social Work Practice, 18, 231–237. doi:10.1177/1049731507309830 [Google Scholar]
- Graham J. E. Christian L. M., & Kiecolt-Glaser J. K (2006). Stress, age, and immune function: Toward a lifespan approach. Journal of Behavioral Medicine, 29, 389–400. doi:10.1007/s10865-006-9057-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler M. L. Nolen-Hoeksema S., & Dovidio J (2009). How does stigma “get under the skin”?: The mediating role of emotion regulation. Psychological Science, 20, 1282–1289. doi:10.1111/j.1467-9280.2009.02441.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek G. M. (2009). Hate crimes and stigma-related experiences among sexual minority adults in the United States: Prevalence estimates from a national probability sample. Journal of Interpersonal Violence, 24, 54–74. doi:10.1177/0886260508316477 [DOI] [PubMed] [Google Scholar]
- Herek G. M. Gillis J. R., & Cogan J. C (2015). Internalized stigma among sexual minority adults: Insights from a social psychological perspective. Stigma and Health, 1, 18–34. doi:10.1037/2376–6972.1.s.18 [Google Scholar]
- Hughes M. Kiecolt K. J. Keith V. M., & Demo D. H (2015). Racial identity and well-being among African Americans. Social Psychology Quarterly, 78, 25–48. doi:10.1177/0190272514554043 [Google Scholar]
- Johnson R. J., & Wolinsky F. D (1993). The structure of health status among older adults: Disease, disability, functional limitation, and perceived health. Journal of Health and Social Behavior, 34, 105–121. [PubMed] [Google Scholar]
- Kamen C. Palesh O. Gerry A. A. Andrykowski M. A. Heckler C. Mohile S.,…Mustian K (2014). Disparities in health risk behavior and psychological distress among gay versus heterosexual male cancer survivors. LGBT Health, 1, 86–92. doi:10.1089/lgbt.2013.0022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kertzner R. M. Meyer I. H. Frost D. M., & Stirratt M. J (2009). Social and psychological well-being in lesbians, gay men, and bisexuals: The effects of race, gender, age, and sexual identity. The American Journal of Orthopsychiatry, 79, 500–510. doi:10.1037/a0016848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H.-J., & Fredriksen-Goldsen K. I (2016). Living arrangement and loneliness among lesbian, gay, and bisexual older adults. The Gerontologist, 56, 548–558. doi:10.1093/geront/gnu083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lance T. S. Anderson M. Z., & Croteau J. M (2010). Improving measurement of workplace sexual identity management. Career Development Quarterly, 59, 19–26. doi:10.1002/j.2161-0045.2010.tb00127.x [Google Scholar]
- Lawrence D., & Williams J. M (2016). Trends in smoking rates by level of psychological distress: Time series analysis of US National Health Interview Survey data 1997–2014. Nicotine & Tobacco Research, 18, 1463–1470. doi:10.1093/ntr/ntv272 [DOI] [PubMed] [Google Scholar]
- Lee S. (2006). Propensity score adjustment as a weighting scheme for volunteer panel web surveys. Journal of Official Statistics, 22, 329–349. [Google Scholar]
- Lee S., & Valliant R (2009). Estimation for volunteer panel web surveys using propensity score adjustment and calibration adjustment. Sociological Methods & Research, 37, 319–343. doi:10.1177/0049124108329643 [Google Scholar]
- Legate N. Ryan R. M., & Weinstein N (2012). Is coming out always a “good thing”? Exploring the relations of autonomy support, outness, and wellness for lesbian, gay, and bisexual individuals. Social Psychological and Personality Science, 3, 145–152. doi:10.1177/1948550611411929 [Google Scholar]
- Lewis R. J. Derlega V. J. Clarke E. G., & Kuang J. C (2006). Stigma consciousness, social constraints, and lesbian well-being. Journal of Counseling Psychology, 53, 48–56. doi:10.1037/0022-0167.53.1.48 [Google Scholar]
- Manzoli L. Villari P. Pirone G. M., & Boccia A (2007). Marital status and mortality in the elderly: A systematic review and meta-analysis. Social Science & Medicine, 64, 77–94. doi:10.1016/j.socscimed.2006.08.031 [DOI] [PubMed] [Google Scholar]
- Masini B. E., & Barrett H. A (2008). Social support as a predictor of psychological and physical well-being and lifestyle in lesbian, gay, and bisexual adults aged 50 and over. Journal of Gay & Lesbian Social Services, 20, 91–110. doi:10.1080/10538720802179013 [Google Scholar]
- Mayfield W. (2001). The development of an Internalized Homonegativity Inventory for gay men. Journal of Homosexuality, 41, 53–76. doi:10.1300/J082v41n02_04 [DOI] [PubMed] [Google Scholar]
- Meyer I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. doi:10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr J. J., & Kendra M. S (2011). Revision and extension of a multidimensional measure of sexual minority identity: the Lesbian, Gay, and Bisexual Identity Scale. Journal of Counseling Psychology, 58, 234–245. doi:10.1037/a0022858 [DOI] [PubMed] [Google Scholar]
- Mooijaart A., & Satorra A (2012). Moment testing for interaction terms in structural equation modeling. Psychometrika, 77, 65–84. doi:10.1007/s11336-011-9232-6 [Google Scholar]
- Muraco A., & Fredriksen-Goldsen K. I (2011). That’s what friends do: Informal caregiving for chronically ill midlife and older LGB adults. Journal of Social and Personal Relationships, 28, 1073–1092. doi:10.1177/0265407511402419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., & Muthén B. O (1998. –2015). Mplus user’s guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Newcomb M. E., & Mustanski B (2010). Internalized homophobia and internalizing mental health problems: A meta-analytic review. Clinical Psychology Review, 30, 1019–1029. doi:10.1016/j.cpr.2010.07.003 [DOI] [PubMed] [Google Scholar]
- Newheiser A.-K., & Barreto M (2014). Hidden costs of hiding stigma: Ironic interpersonal consequences of concealing a stigmatized identity in social interactions. Journal of Experimental Social Psychology, 52, 58–70. doi:10.1016/j.jesp.2014.01.002 [Google Scholar]
- Pascoe E. A., & Smart Richman L (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135, 531–554. doi:10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul C. Ayis S., & Ebrahim S (2006). Psychological distress, loneliness, and disability in old age. Psychology, Health & Medicine, 11, 221–232. doi:10.1080/135485005 [DOI] [PubMed] [Google Scholar]
- Phinney J. S., & Ong A. D (2007). Conceptualization and measurement of ethnic identity: Current status and future directions. Journal of Counseling Psychology, 54, 271–281. doi:10.1037/0022-0167.54.3.271 [Google Scholar]
- Riggle E. D. B. Mohr J. J. Rostosky S. S. Fingerhut A. W., & Balsam K. F (2014). A multifactor Lesbian, Gay, and Bisexual Positive Identity Measure (LGB-PIM). Psychology of Sexual Orientation and Gender Diversity, 1, 398–411. doi:10.1037/sgd0000057 [Google Scholar]
- Rood B. A. Puckett J. A. Pantalone D. W., & Bradford J. B (2015). Predictors of suicidal ideation in a statewide sample of transgender individuals. LGBT Health, 2, 270–275. doi:10.1089/lgbt.2013.0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmeichel B. J., & Vohs K (2009). Self-affirmation and self-control: Affirming core values counteracts ego depletion. Journal of Personality and Social Psychology, 96, 770–782. doi:10.1037/a0014635 [DOI] [PubMed] [Google Scholar]
- Sherbourne C. D., & Stewart A. L (1991). The MOS social support survey. Social Science & Medicine, 32, 705–714. doi:10.1016/0277-9536(91)90150-b [DOI] [PubMed] [Google Scholar]
- Sue D. W. Capodilupo C. M. Torino G. C. Bucceri J. M. Holder A. M. Nadal K. L., & Esquilin M (2007). Racial microaggressions in everyday life: implications for clinical practice. The American Psychologist, 62, 271–286. doi:10.1037/0003-066X.62.4.271 [DOI] [PubMed] [Google Scholar]
- Szymanski D. M. (2006). Does internalized heterosexism moderate the link between heterosexist events and lesbians’ psychological distress? Sex Roles, 54, 227–234. doi:10.1007/s11199-006-9340-4 [Google Scholar]
- Tang F. (2008). Late-life volunteering and trajectories of physical health. Journal of Applied Gerontology, 28, 524–533. doi:10.1177/0733464808327454 [Google Scholar]
- Wallace S. P. Cochran S. D. Durazo E. M., & Ford C. L (2011). The health of aging lesbian, gay and bisexual adults in California. Los Angeles: Policy Brief UCLA Center for Health Policy Research. Retrieved from http://healthpolicy.ucla.edu/publications/Documents/PDF/aginglgbpb.pdf. [PMC free article] [PubMed] [Google Scholar]
- Westerhof G. J., & Keyes C. L (2010). Mental illness and mental health: The two continua model across the lifespan. Journal of Adult Development, 17, 110–119. doi:10.1007/s10804-009-9082-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams M. E., & Fredriksen-Goldsen K. I (2014). Same-sex partnerships and the health of older adults. Journal of Community Psychology, 42, 558–570. doi:10.1002/jcop.21637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R. Yu Y. Jackson J. S., & Anderson N. B (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2, 335–351. doi:10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
- Woodford M. R. Chonody J. M. Kulick A. Brennan D. J., & Renn K (2015). The LGBQ microaggressions on campus scale: A scale development and validation study. Journal of Homosexuality, 62, 1660–1687. doi:10.1080/00918369.2015.1078205 [DOI] [PubMed] [Google Scholar]
- Wright A. J., & Wegner R. T (2012). Homonegative microaggressions and their impact on LGB individuals: A measure validity study. Journal of LGBT Issues in Counseling, 6, 34–54. doi:10.1080/15538605.2012.648578 [Google Scholar]