Abstract
Purpose of the Study:
Optimal engagement in health care plays a critical role in the success of disease prevention and treatment, particularly for older adults who are often in greater need of health care services. However, to date, there is still limited knowledge about the relationship between depression and health care engagement among lesbian, gay, bisexual, and transgender (LGBT) older adults.
Design and Methods:
This study utilized data from Aging with Pride: National Health, Aging, Sexuality/Gender Study, from the 2014 survey with 2,450 LGBT adults 50 years old and older. Multiple-variable regression was utilized to evaluate relationships between three indicators of health care engagement and four depression groups after controlling for background characteristics and discrimination in health care. Health care engagement indicators were “not using preventive care,” “not seeking care when needed,” and “difficulty in adhering to treatments.” Depression groups were defined by depression diagnosis and symptomatology, including Diagnosed-Symptomatic group (Diag-Sympt), Diagnosed-Nonsymptomatic group (Diag-NoSympt), Nondiagnosed-Symptomatic group (NoDiag-Sympt), and Nondiagnosed-Nonsymptomatic group (NoDiag-NoSympt).
Results:
Depression groups displayed different patterns and levels of health care engagement. The Diag-Sympt group displayed the highest “difficulty in adhering to treatments.” Diag-NoSympt group displayed the lowest “not using preventive care.” The NoDiag-Sympt group reported the highest “not using preventive care” and “not seeking care when needed.” The NoDiag-NoSympt group had the lowest “not seeking care when needed” and “difficulty in adhering to treatments.”
Implications:
Depression diagnosis and symptomatology are jointly associated with health care engagement among LGBT older adults. Interventions aiming to promote health care engagement among this population should simultaneously consider both depression diagnosis and symptomatology.
Keywords: Depression, Access to and utilization of services, Sexuality, Gay, Lesbian, Bisexual & Transgender
Engagement in health care has emerged as an important consideration in health care research and practice over the last decade for its central role in the success of disease prevention and treatment. Consistently found to be associated with better health among patients (Coulter, 2002; Hubbard, Kidd, Donaghy, McDonald, & Kearney, 2007), engagement in health care is strongly associated with lower medical expenditures (Dentzer, 2013; Oshima Lee & Emanuel, 2013) by almost $2,000 per capita in a year (Greene, Hibbard, Sacks, Overton, & Parrotta, 2015).
Optimal engagement in health care is critical for lesbian, gay, bisexual, and transgender (LGBT) populations, who on average may be at greater risk of developing chronic conditions compared with heterosexual and nontransgender peers (Institute of Medicine, 2011) due to negative physiological and psychological stress responses triggered by adverse experiences (Lick, Durso, & Johnson, 2013), and therefore may have elevated needs for health services. Indeed, in a population-based study using National Health Interview Survey data, Fredriksen-Goldsen and colleagues found that sexual minority men and women 50 years old and older experience disparities in several physical and mental health indicators; compared with heterosexual peers, lesbian, gay and bisexual older adults are more likely to report receiving diagnoses out of 12 common chronic conditions and are more likely to report subclinical depressive symptomatology (Fredriksen-Goldsen et al., under review).
To better understand health care engagement among LGBT older adults, this study is guided by the Health Equity Promotion Model (HEPM; Fredriksen-Goldsen, Simoni, Kim et al., 2014), an integrative model for conceptualizing the health and well-being of LGBT older adults that takes into full consideration life course development. In the HEPM, LGBT older adults’ structural constraints can influence their health-promoting behaviors, which in turn can further impact their mental health. The inherently time-dynamic nature of the HEPM, however, also implies potential bidirectional relationships between mental health and health-promoting behaviors overtime (Fredriksen-Goldsen & Kim, 2017). Therefore, health care engagement, conceptualized as a key health-promoting behavior, is not only influenced by structural constraints, but also linked to mental health conditions among LGBT older adults. To date, most previous research on health care engagement among LGBT adults has focused solely on structural constraints, in particular past discriminatory experiences in health care, and concluded that discriminatory experiences in health care are a major barrier for care-seeking among LGBT population (Institute of Medicine, 2011, p. 61–67). However, there has been insufficient attention to the interplay between mental health and behavioral factors as mechanisms influencing health care engagement. In this paper, we focus on the role of mental health, including depression diagnoses and depressive symptomatology, in health care engagement among LGBT older adults.
Gruman and colleagues define engagement in health care as “the actions individuals must take to obtain the greatest benefit from the health care services” and emphasize observable behaviors that signify individuals’ involvement in their care in which they integrate necessary information, professional opinions, and their unique needs to prevent or manage illness (Gruman, Rovner, French, et al., 2010). Consistent with Gruman and colleagues’ approach, in this study, we operationalize health care engagement as three key actions along the spectrum of interactions between individuals and the health care system that align with differing stages of health care use: utilizing preventive care, seeking care when needed, and adhering to treatment recommendations.
As contextualized in the HEPM, health care engagement is a key health-promoting behavior that may be associated with mental health, including depressive symptomatology and depression diagnoses. In the general population, those with depression appear to be less engaged in health care (Lord, Malone, & Mitchell, 2010; Carney & Jones, 2006; Bradford, Kim, Braxton, Marx, Butterfield, & Elbogen, 2008) in part due to decreased self-efficacy and decreased motivation in self-care behaviors (Detweiler-Bedell, Friedman, Leventhal, Miller, & Leventhal, 2008; Egede, & Osborn, 2010; Lin, Katon, Von Korff et al., 2004; Salovey, & Birnbaum, 1989). It has been found, for example, across large-scale and population-based studies that adults living with depression are less likely to utilize a wide variety of preventive care services, such as Pap smear, vaccination, cholesterol screening, blood pressure screening (Lord, Malone, & Mitchell, 2010), and mammography (Carney & Jones, 2006), and are more likely to report delayed health care and unmet medical needs (Bradford, Kim, Braxton, Marx, Butterfield, & Elbogen, 2008). Disparities in health care access faced by adults with depression also persist into older adulthood. In both epidemiological and administrative data, older adults living with depression are less likely to utilize preventive services (Koroukian, Bakaki, Golchin, Tyler, & Loue, 2012) and make fewer visits to their health care providers (Cradock-O’Leary, Young, Yano, Wang, & Lee, 2002).
It is also well documented that depression is often under- or over-diagnosed among adults, in particular older adults (Licht-Strunk, van der Kooij, van Schaik, et al., 2005; Morichi, Dell’Aquila, Trotta, Belluigi, Lattanzio, & Cherubini, 2015). Depression has been consistently estimated to impact nearly 20% or more of LGBT older adults across studies, as compared to 1 to 5 percentages among general older population in the U.S. (Institute of Medicine, 2011, p 256–257). If obtaining a diagnosis signifies a critical step in treatment and recovery (Callahan, Bertakis, Azari, Helms, Robbins, & Miller, 1997), depressed LGBT older adults with and without diagnoses will likely embark on different trajectories in their depressive symptomatology, which in turn may have cascading effects on subsequent health care engagement.
Prototypically, there are four groups based on presence or absence of depression diagnosis and current depressive symptomatology that may be associated with the extent of health care engagement among LGBT older adults. They are summarized as followed: Diagnosed-Symptomatic group (Diag-Sympt), Diagnosed-Nonsymptomatic group (Diag-NoSympt), Nondiagnosed-Symptomatic group (NoDiag-Sympt), and Nondiagnosed-Nonsymptomatic group (NoDiag-NoSympt). Both the Diag-Sympt and Diag-NoSympt groups have had prior experiences in interacting with health care systems and have received a diagnosis of depression. They differ in that the Diag-Sympt group also has current depressive symptomatology at clinical levels while the Diag-NoSympt group does not. Similarly, both Diag-Sympt and NoDiag-Sympt have current depressive symptomatology. However, the NoDiag-Sympt group has not had a diagnosis of depression, whereas Diag-Sympt has received a depression diagnosis.
Given the paucity of literature in health care engagement considering both depression diagnosis and symptomatology, it remains unknown whether and how depression diagnosis and symptomatology are associated with health care engagement among LGBT older adults. Evidence from HIV/AIDS care may provide some relevant insights; for example, HIV-positive patients who received treatment for depression significantly increased their adherence to treatments, as compared with those who did not receive such treatment (Yun, Maravi, Kobayashi, Barton, & Davidson, 2005). Such findings suggest that the differing depression groups among LGBT older adults will display different levels of health care engagement, depending on presence or absence of a depression diagnosis as well as current depressive symptomatology.
To our knowledge, no empirical study has investigated the relationship between health care engagement and depression among LGBT older adults, even though this population is at elevated risk of disparities across these indicators. This paper will address this important gap, investigating the role of depression diagnosis and symptomatology in health care engagement among LGBT older adults. We hypothesize that the groups, as defined by depression diagnosis and symptomatology, will have differing levels of health care engagement, after controlling for background characteristics and discriminatory experiences in health care. We expect that the NoDiag-NoSympt group will have the most optimal health care engagement, while NoDiag-Sympt and Diag-Sympt groups will have the lowest levels of engagement. Moreover, we hypothesize that the Diag-NoSympt will have better health care engagement compared with both the NoDiag-Sympt and Diag-Sympt groups. This information is necessary to support the development of interventions to effectively promote health care engagement among LGBT older adults, which is an important step toward developing strategies to reduce health disparities in this at-risk population.
Research Methods
Data
The current study utilized and analyzed the data from Aging with Pride: National Health, Aging, Sexuality/Gender Study (NHAS), a longitudinal study following 2,450 LGBT adults 50 years old and older through mail and web-based surveys via collaborations with 17 community partner agencies serving LGBT older adults across the United States. The data were from the 2014 study survey and included the full sample of participants. Inclusion criteria were: adults aged 50 and older, who self-identified as lesbian, gay, bisexual, or transgender or engaged in a sexual or romantic relationship with someone of the same sex or gender. More information about the study designs is documented in Fredriksen-Goldsen and Kim (2017) in this issue.
In order to reduce sampling bias and increase the generalizability of the findings, we applied survey weights to statistical analyses. Survey weights were computed utilizing three external probability samples’ data as benchmarks following two-step postsurvey adjustment, as has been applied to other types of nonprobability samples (Lee, 2006; Lee & Valliant, 2009). In the first step, the Aging with Pride: NHAS sample was combined with the National Health Interview Survey (NHIS) sample ascertaining sexual orientation by sexual identity, and we computed the probability of being selected from the NHIS versus the Aging with Pride: NHAS sample by using a logistic regression model with age, sex, sexual orientation, Hispanic ethnicity, race, education, region, and house ownership as covariates. In the second step, we further calibrated the weights for those in same-sex partnerships, another indicator of sexual orientation. The population totals by age, race/ethnicity, gender, education, marital status, and region were estimated from the NHIS, the American Community Survey (ACS), and the Health and Retirement Study (HRS). See Fredriksen-Goldsen and Kim (2017) for detailed information regarding the postsurvey adjustment procedures.
Measurement
The variables selected for this study included depression, health care engagement, and selected control variables, including background characteristics and discrimination in health care.
Depression
The construct of depression encompassed two components, lifetime diagnosis and current depressive symptomatology. Lifetime diagnosis was measured by an item that asked participants whether they had ever been told by a doctor or medical professional that they had depression. Current depressive symptomatology was measured by the Center for Epidemiologic Studies Short Depression Scale (CES-D; Andresen, Malmgren, Carter, & Patrick, 1994). CES-D has 10 items regarding how frequently participants experienced the feelings and thoughts described in the items over the past week; for example, “I felt depressed.” As recommended, a 4-point Likert scale was used, ranging from less than 1 day (= 0) to 5–7 days (= 3) and a summed score was computed, with higher scores representing greater levels of depressive symptomatology. Participants whose CES-D scores exceeded 10 were considered to have clinically significant depressive symptomatology (Andresen, Malmgren, Carter, & Patrick, 1994). This binary variable was used along with lifetime diagnosis to create four groups: diagnosed-symptomatic group (Diag-Sympt), diagnosed-nonsymptomatic group (Diag-NoSympt), nondiagnosed-symptomatic group (NoDiag-Sympt), and nondiagnosed-nonsymptomatic group (NoDiag-NoSympt).
Health care engagement
The construct of health care engagement was operationally defined as three major key actions (not using preventive care, not seeking care when needed, difficulty in adhering to treatment) and an overall index (index of health care engagement). Using preventive care was measured by an item asking when was the last time participants visited a doctor for a routine checkup, excluding exams for specific injuries or illnesses. LGBT older adults whose last visits were more than 1 year ago were considered not meeting the recommendations by the Centers for Disease Control and Prevention (CDC, 2005) for preventive care use for older adults. Not seeking care when needed was measured by an item asking whether LGBT older adults experienced any sexual problems or concerns for three months or more during the past year, such as having no interest in sex, or pain during or after sex and whether LGBT older adults ever discussed sex with their doctors after they turned 50. If LGBT older adults experienced sexual problems or concerns for 3 months during the past year but had not discussed it with providers, they were considered not seeking care when needed. Difficulty in adhering to treatment was measured by a single item, asking LGBT older adults how much difficulty they had with taking medications in the correct dosages and/or at the correct time in the past month. A 5-point Likert scale was used, ranging from none to extremely or cannot do. LGBT older adults indicating mild difficulty or above were considered as having difficulty in adhering to treatment. Finally, an index of health care engagement was computed by summing the three health care engagement items, or three domains, ranging from 0 (none of the domains) to 3 (all of the domains). Due to the empirical distribution of the index scores and the small cell size for category 3 (all domains), this index was recoded as 0 (none of the domains), 1 (1 domain), and 2 (2 or more domains). Note that the higher scores on the health care engagement index represented greater levels of lack of health care engagement.
Control variables
Several background characteristics and discrimination in health care were selected to adjust for the estimated relationships between depression and health care engagement among LGBT older adults. These background characteristics included age, gender (female, male, other), sexual orientation (lesbian, gay, bisexual, heterosexual, and other), race/ethnicity (Hispanic, non-Hispanic White, Black, and Others), transgender (yes vs. no), 200% federal poverty level (FPL; at or below 200% FPL vs. above 200% FPL), educational attainment (at or below high school vs. more than high school), and health insurance (uninsured vs. some health care coverage). We also adjusted for discrimination in health care, which was measured by one item, asking LGBT older adults how many times over their lifetime they were denied or provided inferior health care because they are, or were thought to be, LGBT, rated on a 4-point Likert scale, ranging from never (= 0) to 3 or more times (= 3).
Analyses
Descriptive analyses were applied to obtain an overall picture of LGBT older adults as well as the four depression subgroups of LGBT older adults, including distributions of selected background characteristics, prevalence of depression diagnosis and current depressive symptomatology, and health care engagement behaviors. Bivariate analyses were further applied to compare the four depression groups over the selected background characteristics as well as health care engagement behaviors. To better evaluate the relationships between the four depression groups and the three specific health care engagement behaviors, we applied multiple-variable logistic regression with the three health care engagement behaviors as outcomes. To evaluate the relationships between depression and the index of health care engagement, we also applied multiple-variable ordinal regression. Because ordinal regression requires an assumption of proportional odds between equations, Brant tests were used to test the proportional odds assumption (Liu, 2009). To adjust for potential sampling errors, we applied survey weights to all analyses. Finally, Wald tests were used to conduct post hoc group comparisons between the four depression groups. All the analyses were conducted in a commercial statistical package, Stata 14 (StataCorp, 2015).
Results
Descriptive and Bivariate Analyses
The weighted results of descriptive and bivariate analyses are summarized in Table 1. The average age of LGBT older adults was 61.38 years old; 43.79% were female and 50.71% male; 72.47% self-identified as lesbian or gay, 17.22% bisexual, and 10.32% heterosexual or other; 14.22% were transgender; 77.76% were non-Hispanic White; 71.52% lived above 200% FPL; 25.41% had a high school degree or less, 38.26% completed at least some college, and 36.33% had a college degree or higher. Among this population, 94.86% had some health care coverage. Finally, 17.21% of the population had encountered discrimination in health care (i.e., received inferior care or denied care).
Table 1.
Descriptive and Bivariate Analyses on Background Characteristics
| Total | Diag-Sympt Group | Diag-NoSympt Group | NoDiag-Sympt Group | NoDiag-NoSympt Group | p | |
|---|---|---|---|---|---|---|
| Sample size | 2,404 | 462 | 372 | 276 | 1,294 | |
| % | 100% | 23.07 | 15.05 | 13.33 | 48.56 | — |
| Depression (%) | ||||||
| Diagnosis | 38.21 | 100 | 100 | 0 | 0 | — |
| Current symptoms | 36.40 | 100 | 0 | 100 | 0 | — |
| Health care engagement | ||||||
| Not utilizing preventive care (%) | 16.77 | 16.97 | 9.73 | 23.80 | 16.98 | .036 |
| Not seeking care when needed (%) | 17.87 | 25.52 | 14.11 | 25.86 | 13.24 | <.001 |
| Had sexual problems | 44.14 | 58.53 | 45.84 | 54.22 | 34.09 | <.001 |
| Did not discuss with providers | 40.40 | 43.63 | 30.50 | 47.73 | 38.77 | 0.221 |
| Difficulty in adhering treatments (%) | 21.77 | 46.13 | 20.58 | 27.66 | 8.86 | <.001 |
| Index of health care engagement (%) | <.001 | |||||
| Lack of engagement in 0 domain | 54.44 | 34.59 | 64.24 | 35.62 | 65.99 | |
| Lack of engagement in 1 domain | 36.20 | 46.29 | 27.68 | 53.29 | 29.36 | |
| Lack of engagement in 2+ domains | 9.36 | 19.12 | 8.08 | 11.09 | 4.65 | |
| Background characteristics | ||||||
| Age (mean, SD) | 61.38 (8.13) | 59.40 (6.43) | 60.79 (7.67) | 60.40 (7.35) | 62.79 (9.02) | <.001 |
| Gender (%) | .239 | |||||
| Female | 43.79 | 38.01 | 43.39 | 44.92 | 46.36 | |
| Male | 50.71 | 52.96 | 51.05 | 49.79 | 49.78 | |
| Others | 5.50 | 9.02 | 5.57 | 5.30 | 3.86 | |
| Sexual orientation (%) | .625 | |||||
| Lesbian/gay | 72.47 | 67.40 | 74.35 | 70.63 | 74.83 | |
| Bisexual | 17.22 | 18.69 | 16.98 | 20.26 | 15.74 | |
| Heterosexual/something else | 10.32 | 13.91 | 8.66 | 9.11 | 9.44 | |
| Transgender: yes (%) | 14.22 | 18.02 | 13.93 | 12.04 | 13.09 | .434 |
| Race/ethnicity (%) | .003 | |||||
| Non-Hispanic White | 77.76 | 72.99 | 82.65 | 62.35 | 82.75 | |
| Hispanic | 9.01 | 10.56 | 6.36 | 14.81 | 7.50 | |
| Black | 8.94 | 10.52 | 7.45 | 16.16 | 6.66 | |
| Others | 4.29 | 5.93 | 3.54 | 6.68 | 3.08 | |
| 200% federal poverty level: above (%) | 71.52 | 54.74 | 75.55 | 56.79 | 82.09 | <.001 |
| Education attainment (%) | <.001 | |||||
| High school or below | 25.41 | 33.52 | 18.95 | 41.46 | 19.14 | |
| Some college | 38.26 | 36.09 | 34.81 | 31.10 | 42.32 | |
| College graduate or above | 36.33 | 30.39 | 46.24 | 27.44 | 38.54 | |
| Health insurance: any (%) | 94.86 | 92.36 | 98.15 | 91.80 | 95.86 | .063 |
| Discrimination in health care: ever (%) | 17.21 | 30.62 | 13.82 | 16.22 | 12.18 | <.001 |
Note: Weighted estimates are shown in the table. NoDiag-NoSympt = non-diagnosed-non-symptomatic; Diag-NoSympt = diagnosed-non-symptomatic; NoDiag-Sympt = non-diagnosed-symptomatic; Diag-Sympt = diagnosed-symptomatic.
In terms of health care engagement, 16.77% of the LGBT older adults did not utilize preventive care the preceding year, 17.87% did not seek health care when they experienced difficulties or concerns (44.14% had encountered sexual problems, and among which 40.40% did not discuss with their providers about their sexual health concerns), and 21.77% reported difficulty in adhering to treatments. Overall, 54.44% of the LGBT older adults reported full health care engagement, 36.20% reported a lack of one type of health care engagement, and 9.36% reported a lack of at least 2 types of engagement in care.
Among LGBT older adults, about 38.21% had received a lifetime depression diagnosis, whereas 36.40% had current depressive symptomatology. After breaking down the overall population by diagnosis and current symptomatology, the Diag-Sympt group consisted of 23.07%, Diag-NoSympt group 15.05%, NoDiag-Sympt group 13.33%, and NoDiag-NoSympt group 48.56%. Across the four depression groups, several important differences regarding health care engagement emerged. As indicated by the index of health care engagement, Diag-Sympt and NoDiag-Sympt groups had significantly lower health care engagement compared with Diag-NoSympt and NoDiag-NoSympt groups. Although the Diag-Sympt group had the lowest engagement in adhering to treatments (46.13%), the NoDiag-Sympt group had the lowest engagement in utilizing preventive care (23.80%) and seeking care (25.86%). Both the Diag-Sympt and NoDiag-Sympt groups were less likely to report full engagement, 34.59% and 35.62%, respectively, as compared with the other two groups.
The depression groups also differed significantly in several background characteristics. The NoDiag-NoSympt group was significantly older than the other three groups. The Diag-Sympt and NoDiag-Sympt groups were less likely to be non-Hispanic White (72.99% and 62.35%, respectively), less likely to live above 200% FPL (54.74 and 56.79%, respectively), and less likely to have postsecondary education (66.48% and 58.54%, respectively) as compared with the other two groups. Finally, the Diag-Sympt group was more likely to have experienced discrimination in health care (30.62%).
Multiple-Variable Logistic and Ordinal Regression
The results for the multiple-variable regressions are presented in Table 2. As shown in the table, after controlling for background characteristics and discrimination, depression groups differed significantly in their levels of health care engagement. Compared with the NoDiag-NoSympt group, the Diag-NoSympt group had significantly lower odds (Adjusted odds ratio [AOR] = 0.51, p < .05) of not using preventive care but higher odds (AOR = 2.45, p < .01) of reporting difficulty in adhering to treatments. NoDiag-Sympt group, in contrast, had higher odds of not seeking care (AOR = 2.41, p < .01) and reporting difficulty in adhering to treatments (AOR = 2.63, p < .01) as compared with NoDiag-NoSympt group.
Table 2.
Results for Weighted Regressions for Health Care Engagement Outcomes
| Not use preventive care last year | Not seek care when needed last year | Difficulty in adhering to treatments last month | Index for health care engagement | |
|---|---|---|---|---|
| AOR (SE) | AOR (SE) | AOR (SE) | AOR (SE) | |
| Nondiagnosed-nonsymptomatic (NoDiag-NoSympt) | (Ref) | (Ref) | (Ref) | (Ref) |
| Diagnosed-nonsymptomatic (Diag-NoSympt) | 0.51 (0.15)* | 1.19 (0.34) | 2.45 (0.72)** | 1.14 (0.24) |
| Nondiagnosed-symptomatic (NoDiag-Sympt) | 1.47 (0.43) | 2.41 (0.68)** | 2.63 (0.84)** | 2.59 (0.53)** |
| Diagnosed-symptomatic group (Diag-Sympt) | 0.77 (0.20) | 2.28 (0.54)** | 7.08 (1.80)** | 3.38 (0.65)** |
Note: Weighted estimates are shown in the table. AOR = adjusted odds ratio. Estimations were adjusted for: age, gender, sexual orientation, transgender, race/ethnicity, education, 200% federal poverty level, health insurance coverage, and discrimination in health care settings.
*p < .05; **p < .01.
The results of Wald tests found that the NoDiag-Sympt group had higher odds of not using preventive care (p < .01) and not seeking care (p < .05) as compared with the Diag-NoSympt group. Finally, the Diag-Sympt group as compared with the NoDiag-NoSympt group had higher odds of not seeking care (AOR = 2.28, p < .01) and reporting difficulty in adhering to treatments (AOR = 7.08, p < .01). The Diag-Sympt group had marginally lower odds (p = .054) of not using preventive care compared with NoDiag-Sympt group, but higher odds (p = .04) of not seeking care compared with Diag-NoSympt group. The Diag-Sympt group also had higher odds of reporting difficulty in adhering to treatments compared with Diag-NoSympt (p < .01) and NoDiag-Sympt (p < .01) groups.
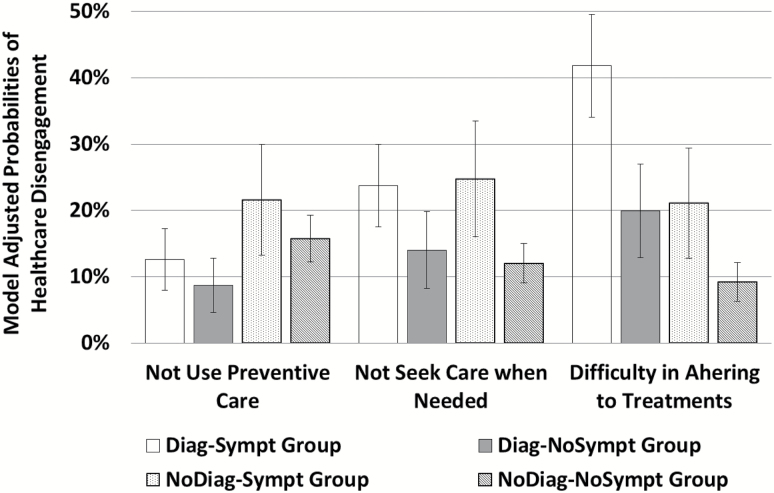
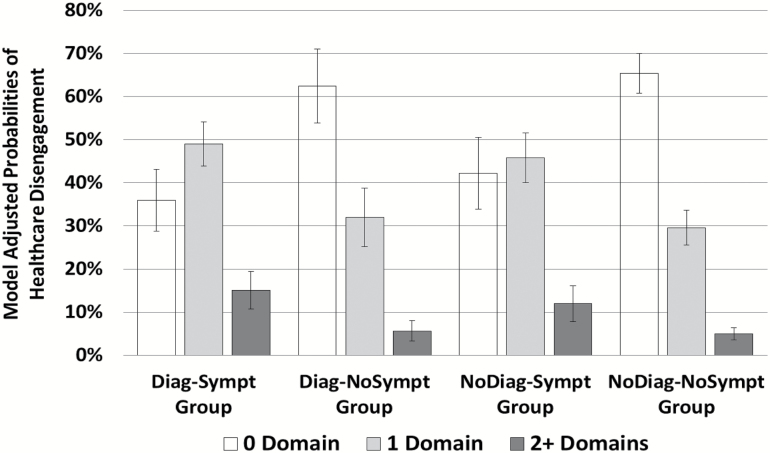
The results of ordinal regression were summarized in the far right column of Table 2. Because the Brant tests did not reach 0.05 significance levels (p = .383), the proportional odds assumption in ordinal regression was not violated. The NoDiag-Sympt and Diag-Sympt groups had higher odds (AOR = 2.59, p < .01 and AOR = 3.38, p < .01, respectively) of having one level higher (from 0 to 1 and from 1 to more than 2) on the index for health care engagement compared with the NoDiag-NoSympt group. The results of these tests also found that both the NoDiag-Sympt and Diag-Sympt groups had higher odds (p < .01) compared with Diag-NoSympt group of having one level higher on the engagement index. There was no evidence to support that the NoDiag-Sympt and Diag-Sympt were different on the engagement index. Figure 1 illustrated the model adjusted probabilities of health care engagement across the four depression groups. As shown, while only 8.71% of the Diag-NoSympt group did not use preventive care last year, 21.56% of the NoDiag-Sympt group did not; while among the NoDiag-NoSympt and Diag-NoSympt groups only about 13% did not seek care when needed, NoDiag-Sympt and Diag-Sympt groups had about 24.77%; finally, while 9.22% of the NoDiag-NoSympt group reported any difficulty in adhering to treatments, 19.93% of the Diag-NoSympt group did, 21.10% of NoDiag-Sympt group did, and 41.81% of the Diag-Sympt group did. Figure 2 demonstrates the model adjusted probabilities of reporting different levels of health care engagement across the four depression groups. As shown, the NoDiag-NoSympt and Diag-NoSympt groups had similar levels of health care engagement while the NoDiag-Sympt and Diag-Sympt groups were similar. About half of the NoDiag-Sympt and Diag-Sympt groups reported a lack of engagement in 1 domain, and more than 10% reported problems in 2 or more domains.
Figure 1.
Probabilities of lack of engagement by tasks and depression groups. Diag-Sympt = diagnosed-symptomatic; Diag-NoSympt = diagnosed-nonsymptomatic; NoDiag-Sympt = nondiagnosed-symptomatic; NoDiag-NoSympt = nondiagnosed-nonsymptomatic
Figure 2.
Probabilities of lack of engagement by numbers of domains and depression groups. Diag-Sympt = diagnosed-symptomatic; Diag-NoSympt = diagnosed-nonsymptomatic; NoDiag-Sympt = nondiagnosed-symptomatic; NoDiag-NoSympt = nondiagnosed-nonsymptomatic.
Discussion
This is the first empirical study, to the best of our knowledge, to evaluate the relationship between health care engagement and depression among LGBT older adults. This study is not only guided by the HEPM in selection of variables, but also contributes to theory building by testing reversed direction of association between depression and health care engagement, yielding potential bidirectional relationships between mental health and health-promoting behaviors. In this study, we incorporated the complexities of depression, simultaneously considering both depression diagnosis and current depressive symptomatology, into the study design in order to evaluate their relationship with health care engagement in this population. The results show that depression among LGBT older adults is significantly associated with suboptimal engagement in health care even after controlling for background characteristics and discrimination in health care settings, as reflected in the different patterns of health care engagement displayed by the four depression groups. Although the NoDiag-NoSympt group generally displayed the most optimal health care engagement, the Diag-Sympt and NoDiag-Sympt groups experienced significantly lower health care engagement. Diag-NoSympt group, on the other hand, shared similar health care engagement with the NoDiag-NoSympt group, except that the Diag-NoSympt group was less likely to report not using preventive care and more likely to report difficulty in adhering to treatments.
These results support our hypotheses that different subgroups of LGBT older adults as defined by depression diagnosis and symptomatology would have different levels of health care engagement. These results further provide evidence to highlight heterogeneity in depression among LGBT older and illustrate the importance of considering such complexities in study designs when evaluating the relationships between depression and health care engagement. We found the four different depression groups were associated with health care engagement to varying extents and the patterns of these relationships also differed across the three health care engagement behaviors we assessed. Such divergent findings may be partly attributed to the fact that although all the selected measures are considered important components in health care engagement, they may represent different dimensions of a health care engagement continuum and require differing cognitive, motivational, and affective resources for successful implementation. This may partially explain why they do not share uniform relationships with depression diagnosis and symptomatology.
As expected, LGBT older adults with neither a lifetime depression diagnosis nor current depressive symptomatology (NoDiag-NoSympt group) had the highest levels of health care engagement in general. This is consistent with the literature that patients without depression diagnosis and with lower depressive symptomatology are more likely to proactively address their health concerns (Ironson, Balbin, Stuetzle et al., 2005; Marshall, Beach, Saha et al., 2013) and optimally adhere to treatments (DiMatteo, Lepper, & Croghan, 2000; Gonzalez, Batchelder, Psaros, & Safren, 2011). In contrast, LGBT older adults who had received a depression diagnosis but report no symptoms (Diag-NoSympt group) may be recovering from depression and had higher levels of health care engagement in utilizing preventive care, even compared with the NoDiag-NoSympt group. This may be due to the fact that prior experiences with health care system are associated with subsequent utilization of preventive care among older adults and sexual minorities (Chi & Neuzil, 2004; Fish & Anthony, 2005; Ross & Duff, 1982). LGBT older adults who had received a depression diagnosis might also have had more prior experiences in interacting with the health care system, which led to greater use of preventive care. Thus, LGBT older adults in the Diag-NoSympt group may benefit from previous engagement in their depression treatment and be more likely to engage in preventive care. However, the Diag-NoSympt group was more likely to report difficulties in adhering to treatments as compared with NoDiag-NoSympt group. This may be due to the fact that adherence depends on cognitive functioning, which may become chronically compromised in individuals who have experienced depression, even after depressive symptoms are successfully treated (Jeon & Kim, 2015).
As expected, LGBT older adults who suffered from active depressive symptomatology experienced lower levels of health care engagement regardless of their diagnosis history, such that both NoDiag-Sympt and Diag-Sympt groups of LGBT older adults had significantly lower health care engagement in general. In particular, LGBT older adults in both the NoDiag-Sympt and Diag-Sympt groups had higher probabilities of not seeking care even when they had problems or concerns. This is consistent with previous findings that individuals with serious psychological distress are more likely to avoid health care or lack the motivation to seek care (Stobbe, Wierdsma, Kok et al., 2013; Ye, Shim, & Rust, 2012). Moreover, LGBT older adults who had a diagnosis and were currently depressed (Diag-Sympt group) reported the highest levels of difficulty in treatment adherence yet slightly better engagement in preventive care as compared with depressed LGBT older adults without a diagnosis (NoDiag-Sympt group). This may be because the Diag-Sympt group captures those chronically depressed LGBT older adults whose cognitive functioning has been further compromised (Riso, du Toit, Blandino et al., 2003), but who still have acquired advantages from their prior experiences in receiving depression care, enabling them to greater utilize preventive services. Finally, in contrast, LGBT older adults who suffered from current depressive symptomatology without having a diagnosis (NoDiag-Sympt group) reported the lower engagement across tasks. This group of LGBT older adults not only was negatively influenced by active depressive symptomatology, but also perhaps did not have access to the benefits from the health care system as their depressive symptomatology was unnoticed.
As there is an established literature body documenting excessive utilization of health care services among older adults living with depression (Fischer, Wei, Rolnick et al., 2002; Koenig, Shelp, Goli, Cohen, & Blazer, 1989; Luber, Meyers, Williams-Russo et al., 2001), our findings that LGBT older adults with depressive symptomatology reported lower engagement even when they perceived a health concern (not seeking care) compared to their peers without depressive symptomatology warrant further attention. On the one hand, these findings suggest elevated risk for LGBT older adults with depressive symptomatology. On the other, such a difference may also be attributed to the measurement we employed in this study, which may have capture a different construct other than health care utilization. To date, most existing studies measure health care utilization by counting whether study participants did or did not utilize certain health services, while in our study we aimed to capture whether our participants discussed their health concerns within the context of sexual health. Because sexual health remains a topic that is difficult for many to discuss, it has been relatively neglected in many clinical settings, particularly in geriatric primary care (Gott, 2006; Gott & Hinchliff, 2003). In such settings, it may further tax LGBT older adults’ cognitive and motivational resources to initiate conversations with primary care providers about their sexual health concerns and sexual health. In fact, the construct we measured may be conceptually more similar to the constructs studied in emerging research that targets dismantling complex relationships among depression, delay in care (Sullivan, Ciechanowski, Russo, et al., 2009), and avoidance of health care (Taber, Leyva, & Persoskie, 2015; Ye, Shim, & Rust, 2012), which when compounded, may lead to worse health outcomes and greater utilization of health care, especially more acute and expensive types of services, such as emergency care (Bayliss, Ellis, Shoup et al., 2012) and hospitalization.
These research results need to be interpreted in the light of potential limitations of the study. First, the current study utilized data from the 2014 survey of Aging with Pride: NHAS, which is cross-sectional. Thus, it is impossible to fully establish causal direction. Moreover, the results are constrained by the limited numbers and types of health care engagement tasks selected in this study, which may have rendered study results less generalizable to different types of health care engagement with other health care needs. Although we adopted Gruman and colleagues approach that defined health care engagement as critical tasks needed to be carried out by health care consumers, the original list included more than 10 different tasks (Gruman, Rovner, French, et al., 2010). As shown in this study, different health care engagement tasks may have varying relationships with mental health because of different cognitive, motivational, and affective resources required. Our measurement of depression diagnosis involved a wide time-frame which may increase potential recall biases of participants. It may be promising for future studies to employ longitudinal designs with more extensive measurement of a wider array of health care engagement tasks in relation to a greater variety of health concerns, as well as depression diagnosis measure with a short recall time-frame. With true longitudinal designs, it will be more feasible to identify causal directions and to evaluate bidirectional impacts between depression and health care engagement overtime among LGBT older adults. The longitudinal information can further provide more reliable roadmaps to design intervention studies. Finally, in order to isolate the relationship between depression and health care engagement we have “controlled” for the selected background factors that often characterize social positions and stratification. However, since social positions can have profound effects on health care engagement (Mugavero, 2008), we encourage future studies to adapt an “intersectionality approach” which simultaneously considers the interwoven effects of sexuality, gender identity, mental health, and social positions on health care engagement.
Regardless of these limitations, this study is likely the first to document the complicated relationships between depression diagnosis, current depressive symptomatology, and health care engagement among LGBT older adults. The study results highlight the importance for health care and aging service providers to attend to LGBT older adults’ mental health, a critical component that has been long missing in the literature of health care engagement. These findings strongly suggest that both lifetime and current mental health states signifying illness progression and recovery must be considered. As Prince and colleagues almost a decade ago argued “mental disorders can delay help-seeking, reduce the likelihood of detection and diagnosis, or do both”; they further concluded that there is “no health without mental health” (Prince, Patel, Saxena et al., 2007, p. 864). As a result, it may be helpful to provide screening for potential depressive symptomatology within both primary care and community aging-related service settings, as well as to develop and offer necessary interventions that aim to promote both health care engagement and mental health well-being among this vulnerable and growing population.
Funding
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG026526 (K. I. Fredriksen-Goldsen, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Andresen E. M. Malmgren J. A. Carter W. B., & Patrick D. L (1994). Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). American Journal of Preventive Medicine, 10(2), 77–84. [PubMed] [Google Scholar]
- Bradford D. W. Kim M. M. Braxton L. E. Marx C. E. Butterfield M., & Elbogen E. B (2008). Access to medical care among persons with psychotic and major affective disorders. Psychiatric Services (Washington, D.C.), 59(8), 847–852. doi:10.1176/ps.2008.59.8.847 [DOI] [PubMed] [Google Scholar]
- Bayliss E. A. Ellis J. L. Shoup J. A. Zeng C. McQuillan D. B., & Steiner J. F (2012). Association of patient-centered outcomes with patient-reported and ICD-9-based morbidity measures. Annals of Family Medicine, 10(2), 126–133. doi:10.1370/afm.1364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callahan E. J. Bertakis K. D. Azari R. Helms L. J. Robbins J., & Miller J (1997). Depression in primary care: patient factors that influence recognition. Family Medicine, 29(3), 172–176. [PubMed] [Google Scholar]
- Carney C. P., & Jones L. E (2006). The influence of type and severity of mental illness on receipt of screening mammography. Journal of General Internal Medicine, 21(10), 1097–1104. doi:10.1111/j.1525-1497.2006.00565.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (2005) Centers for disease control and prevention. The Guide to Community Preventive Services, 1996, 223–303. [Google Scholar]
- Chi R. C., & Neuzil K. M (2004). The association of sociodemographic factors and patient attitudes on influenza vaccination rates in older persons. The American Journal of the Medical Sciences, 327(3), 113–117. doi:10.1097/00000441-200403000-00001 [DOI] [PubMed] [Google Scholar]
- Coulter A. (2002). The autonomous patient. London: Nuffield Trust. [Google Scholar]
- Cradock-O’Leary J. Young A. S. Yano E. M. Wang M., & Lee M. L (2002). Use of general medical services by VA patients with psychiatric disorders. Psychiatric Services (Washington, D.C.), 53(7), 874–878. doi:10.1176/appi.ps.53.7.874 [DOI] [PubMed] [Google Scholar]
- Detweiler-Bedell J. B. Friedman M. A. Leventhal H. Miller I. W., & Leventhal E. A (2008). Integrating co-morbid depression and chronic physical disease management: identifying and resolving failures in self-regulation. Clinical Psychology Review, 28(8), 1426–1446. doi:10.1016/j.cpr.2008.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dentzer S. (2013). Rx for the ‘blockbuster drug’ of patient engagement. Health Affairs (Project Hope), 32(2), 202. doi:10.1377/hlthaff.2013.0037 [DOI] [PubMed] [Google Scholar]
- DiMatteo M. R. Lepper H. S., & Croghan T. W (2000). Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Archives of Internal Medicine, 160(14), 2101–2107. doi:10.1001/archinte.160.14.2101 [DOI] [PubMed] [Google Scholar]
- Egede L. E., & Osborn C. Y (2010). Role of motivation in the relationship between depression, self-care, and glycemic control in adults with type 2 diabetes. The Diabetes Educator, 36(2), 276–283. doi:10.1177/0145721710361389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish J., & Anthony D (2005). UK national Lesbians and Health Care Survey. Women & Health, 41(3), 27–45. doi:10.1300/J013v41n03_02 [DOI] [PubMed] [Google Scholar]
- Fischer L. R. Wei F. Rolnick S. J. Jackson J. M. Rush W. A. Garrard J. M.,…Luepke L. J (2002). Geriatric depression, antidepressant treatment, and healthcare utilization in a health maintenance organization. Journal of the American Geriatrics Society, 50(2), 307–312. doi: 10.1046/j.1532-5415. 2002.50063.x [DOI] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I., & Kim H.-J (2017). The science of conducting research with LGBT older adults - An introduction to Aging with Pride: National Health, Aging, Sexuality/Gender Study. The Gerontologist, 57, S1-S14. doi:10.1093/geront/gnw212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K. I. Simoni J. M. Kim H. J. Lehavot K. Walters K. L. Yang J.,…Muraco A (2014). The Health Equity Promotion Model: Reconceptualization of lesbian, gay, bisexual, and transgender (LGBT) health disparities. The American journal of orthopsychiatry, 84(6), 653–663. doi:10.1037/ort0000030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez J. S. Batchelder A. W. Psaros C., & Safren S. A (2011). Depression and HIV/AIDS treatment nonadherence: a review and meta-analysis. Journal of Acquired Immune Deficiency Syndromes (1999), 58(2), 181–187. doi:10.1097/QAI.0b013e31822d490a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gott M. (2006). Sexual health and the new ageing. Age and Ageing, 35(2), 106–107. doi:10.1093/ageing/afj050 [DOI] [PubMed] [Google Scholar]
- Gott M., & Hinchliff S (2003). Barriers to seeking treatment for sexual problems in primary care: a qualitative study with older people. Family Practice, 20(6), 690–695. doi:10.1093/fampra/cmg612 [DOI] [PubMed] [Google Scholar]
- Greene J. Hibbard J. H. Sacks R. Overton V., & Parrotta C. D (2015). When patient activation levels change, health outcomes and costs change, too. Health Affairs (Project Hope), 34(3), 431–437. doi:10.1377/hlthaff.2014.0452 [DOI] [PubMed] [Google Scholar]
- Gruman J. Rovner M. H. French M. E. Jeffress D. Sofaer S. Shaller D., & Prager D. J (2010). From patient education to patient engagement: Implications for the field of patient education. Patient Education and Counseling, 78(3), 350–356. doi:10.1016/j.pec.2010.02.002 [DOI] [PubMed] [Google Scholar]
- Hubbard G. Kidd L. Donaghy E. McDonald C., & Kearney N (2007). A review of literature about involving people affected by cancer in research, policy and planning and practice. Patient Education and Counseling, 65(1), 21–33. doi:10.1016/j.pec.2006.02.009 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (2011). Health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Ironson G. Balbin E. Stuetzle R. Fletcher M. A. O’Cleirigh C. Laurenceau J. P.,…Solomon G (2005). Dispositional optimism and the mechanisms by which it predicts slower disease progression in HIV: Proactive behavior, avoidant coping, and depression. International Journal of Behavioral Medicine, 12(2), 86–97. doi:10.1207/s15327558ijbm1202_6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeon S.W., & Kim Y. K (2015). Cognitive impairment in depression. Current Psychiatry Reviews, 11(4), 280–289. doi:10.2174/1573400511666150831201635 [Google Scholar]
- Koenig H. G. Shelp F. Goli V. Cohen H. J., & Blazer D. G (1989). Survival and health care utilization in elderly medical inpatients with major depression. Journal of the American Geriatrics Society, 37(7), 599–606. doi:10.1111/j.1532-5415.1989.tb01249.x [DOI] [PubMed] [Google Scholar]
- Koroukian S. M. Bakaki P. M. Golchin N. Tyler C., & Loue S (2012). Mental illness and use of screening mammography among Medicaid beneficiaries. American Journal of Preventive Medicine, 42(6), 606–609. doi:10.1016/j.amepre.2012.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. (2006). Propensity score adjustment as a weighting scheme for volunteer panel web surveys. Journal of Official Statistics, 22(2), 329–349. [Google Scholar]
- Lee S., & Valliant R (2009). Estimation for volunteer panel web surveys using propensity score adjustment and calibration adjustment. Sociological Methods & Research, 37(3), 319–343. doi:10.1177/0049124108329643 [Google Scholar]
- Licht-Strunk E. van der Kooij K. G. van Schaik D. J. van Marwijk H. W. van Hout H. P. de Haan M., & Beekman A. T (2005). Prevalence of depression in older patients consulting their general practitioner in The Netherlands. International Journal of Geriatric Psychiatry, 20(11), 1013–1019. doi: 10.1002/gps.1391 [DOI] [PubMed] [Google Scholar]
- Lin E. H. Katon W. Von Korff M. Rutter C. Simon G. E. Oliver M.,…Young B (2004). Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care, 27(9), 2154–2160. doi:10.2337/diacare.27.9.2154 [DOI] [PubMed] [Google Scholar]
- Lick D. J. Durso L. E., & Johnson K. L (2013). Minority stress and physical health among sexual minorities. Perspectives on Psychological Science: A Journal of the Association for Psychological Science, 8(5), 521–548. doi:10.1177/1745691613497965 [DOI] [PubMed] [Google Scholar]
- Liu X. (2009). Ordinal regression analysis: Fitting the proportional odds model using Stata, SAS and SPSS. Journal of Modern Applied Statistical Methods, 8(2), 30. [Google Scholar]
- Lord O., Malone D., & Mitchell A. J (2010). Receipt of preventive medical care and medical screening for patients with mental illness: A comparative analysis. General hospital psychiatry, 32(5), 519–543. doi:10.1016/j.genhosppsych.2010.04.004 [DOI] [PubMed] [Google Scholar]
- Luber M. P. Meyers B. S. Williams-Russo P. G. Hollenberg J. P. DiDomenico T. N. Charlson M. E., & Alexopoulos G. S (2001). Depression and service utilization in elderly primary care patients. The American Journal of Geriatric Psychiatry, 9(2), 169–176. doi:10.1097/00019442-200105000-00009 [PubMed] [Google Scholar]
- Marshall R. Beach M. C. Saha S. Mori T. Loveless M. O. Hibbard J. H.,…Korthuis P. T (2013). Patient activation and improved outcomes in HIV-infected patients. Journal of General Internal Medicine, 28(5), 668–674. doi:10.1007/s11606-012-2307-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morichi V. Dell’Aquila G. Trotta F. Belluigi A. Lattanzio F., & Cherubini A (2015). Diagnosing and treating depression in older and oldest old. Current Pharmaceutical Design, 21(13), 1690–1698. [DOI] [PubMed] [Google Scholar]
- Mugavero M. J. (2008). Improving engagement in HIV care: what can we do? Topics in HIV Medicine: A Publication of the International AIDS Society, USA, 16(5), 156–161. [PubMed] [Google Scholar]
- Oshima Lee E., & Emanuel E. J (2013). Shared decision making to improve care and reduce costs. The New England Journal of Medicine, 368(1), 6–8. doi:10.1056/NEJMp1209500 [DOI] [PubMed] [Google Scholar]
- Prince M. Patel V. Saxena S. Maj M. Maselko J. Phillips M. R., & Rahman A (2007). No health without mental health. Lancet (London, England), 370(9590), 859–877. doi:10.1016/S0140-6736(07)61238-0 [DOI] [PubMed] [Google Scholar]
- Riso L. P. du Toit P. L. Blandino J. A. Penna S. Dacey S. Duin J. S.,…Ulmer C. S (2003). Cognitive aspects of chronic depression. Journal of Abnormal Psychology, 112(1), 72–80. [PubMed] [Google Scholar]
- Ross C. E., & Duff R. S (1982). Returning to the doctor: the effect of client characteristics, type of practice, and experiences with care. Journal of Health and Social Behavior, 23(2), 119–131. [PubMed] [Google Scholar]
- Salovey P., & Birnbaum D (1989). Influence of mood on health-relevant cognitions. Journal of Personality and Social Psychology, 57(3), 539–551. doi:10.1037/0022-3514.57.3.539 [DOI] [PubMed] [Google Scholar]
- Stobbe J. Wierdsma A. I. Kok R. M. Kroon H. Depla M. Roosenschoon B. J., & Mulder C. L (2013). Lack of motivation for treatment associated with greater care needs and psychosocial problems. Aging & Mental Health, 17(8), 1052–1058. doi:10.1080/13607863.2013.807422 [DOI] [PubMed] [Google Scholar]
- Sullivan M. D. Ciechanowski P. S. Russo J. E. Soine L. A. Jordan-Keith K. Ting H. H., & Caldwell J. H (2009). Understanding why patients delay seeking care for acute coronary syndromes. Circulation: Cardiovascular Quality and Outcomes, 2(3), 148–154. doi:10.1161/CIRCOUTCOMES.108.825471 [DOI] [PubMed] [Google Scholar]
- Taber J. M. Leyva B., & Persoskie A (2015). Why do people avoid medical care? A qualitative study using national data. Journal of General Internal Medicine, 30(3), 290–297. doi:10.1007/s11606-014-3089-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye J. Shim R., & Rust G (2012). Health care avoidance among people with serious psychological distress: analyses of 2007 Health Information National Trends Survey. Journal of Health Care for the Poor and Underserved, 23(4), 1620–1629. doi:10.1353/hpu.2012.0189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yun L. W. Maravi M. Kobayashi J. S. Barton P. L., & Davidson A. J (2005). Antidepressant treatment improves adherence to antiretroviral therapy among depressed HIV-infected patients. Journal of Acquired Immune Deficiency Syndromes (1999), 38(4), 432–438. [DOI] [PubMed] [Google Scholar]