Diabetes, the most common metabolic disorder in primary care, is the leading cause of cardiovascular disease, renal failure, retinopathy, and lower-extremity amputations (1). Diabetic foot abnormalities, including ulcers and lower-extremity amputations, are associated with substantial morbidity, loss of quality of life, and disability and are very costly for the individuals affected, their families, and society as a whole (2). Approximately 84% of nontraumatic major amputations in individuals with diabetes are preceded by foot abnormalities such as an ulceration (3). According to the Centers for Disease Control and Prevention, the total cost of diagnosed diabetes in the United States was $245 billion in 2012, with the majority of costs attributed to a high occurrence of hospital admissions, including $9 billion associated with foot ulcers alone (2).
Clinical Issue and Local Problem
Diabetes is a treatable condition, yet it is the seventh leading cause of death in South Carolina. South Carolina ranks tenth highest in the nation in the percentage of population with diabetes (4). In 2013, South Carolina had the fourth highest prevalence of diabetes in the United States, with ∼25,000 diabetes-related hospitalizations and emergency visits, costing $367 million. The cost of diabetes care in South Carolina is expected to exceed $3 billion in 2016 and to hit $4 billion by 2020 (5). Many of the costs associated with diabetes could be reduced with preventive intervention in the primary care setting, where diabetes is the most common metabolic disorder encountered. However, gaps occur in the care and management of diabetes, especially in the area of foot care. In 2012, an Institute for Preventive Foot Health/National Purchase Diary survey revealed that only 46% of patients with diabetes reported ever having foot screenings with their primary care provider (6).
Foot complications, specifically ulcers and amputations, are the number one reason for hospitalization in patients with diabetes (7). Thus, early recognition and proper management of patients at risk for developing foot ulcers and lower-extremity amputations are crucial. Performing regular foot exams on patients with diabetes in the primary care setting should be a high priority (7). In response to the need for more consistent foot exams, an American Diabetes Association (ADA) task force created the Comprehensive Foot Examination and Risk Assessment. In addition, the ADA’s Standards of Medical Care in Diabetes—2016 recommend an annual comprehensive foot examination to identify risk factors predictive of foot abnormalities, ulcerations, and amputations to decrease morbidity and mortality (7). Foot ulcers and other lower-extremity complications are considered common, multifaceted, and costly and are linked to increased morbidity, loss of quality of life, and mortality, providing further evidence that more frequent comprehensive foot exams are beneficial (8).
Routine Diabetic Foot Exams
A proper foot exam for patients with diabetes should include a thorough history and assessment for risk factors, inspection for any abnormalities, a neurological assessment (i.e., using a 10-g monofilament test to assess pinprick sensation and a tuning fork to determine sensitivity to vibration), and a vascular evaluation of foot pulses (Table 1). In 2014, the Centers for Medicaid and Medicare Services (CMS) included an annual foot exam in primary care as a clinical quality measure (CQM). A quality measure is a tool that tracks and measures the value of a health care service and uses data to quantify a provider’s delivery of quality patient care. CMS uses the electronic medical record (EMR) incentive program to track CQMs, and health care practices receive reimbursement when the appropriate measures are documented. This program helps establish incentive payments to qualified professionals and hospitals, critical shortage hospitals, and Medicare Advantage Organizations to endorse meaningful use of EMRs. An example would be completion and correct documentation of a foot exam using an EMR in the primary care setting. The foot exam, a CQM, must include a visual inspection, sensory exam with a monofilament, and assessment of peripheral pulses (9). These components must be documented for primary care providers to receive the incentive increase from CMS.
TABLE 1.
Comprehensive Foot Examination
| History and Assessment for Risk Factors |
|---|
| History: • History of diabetes • Previous ulcerations, amputations, or nonhealing wounds • Charcot joint or other foot deformities • Vascular surgery (stents or bypass) or angioplasty • Cigarette smoking Neuropathic symptoms: • Burning or shooting pain, electrical or sharp sensations • Numbness or altered sensation (i.e., feeling dead or missing) Vascular symptoms: • Claudication, pain associated with movement, or pain at rest Other complications from diabetes: • History of nephropathy or retinopathy • Ongoing podiatry involvement |
| Inspection |
| Dermatological: • Skin status: color, thickness, dryness, and cracking • Sweating • Infection: check nails and between the toes for fungal infections • Ulceration • Calluses or blistering, with or without bleeding Musculoskeletal: • Deformity (e.g., hammer toe, Charcot joint) • Muscle wasting (wrinkling between metatarsals) |
| Neurological Assessment |
| • 10-g monofilament test • Vibration using 128-Hz tuning fork • Pinprick sensation • Ankle reflexes • Vibration perception threshold |
| Vascular Assessment |
| • Foot pulses • Ankle-brachial index test, if indicated |
Referral to a podiatrist should be considered whenever skin breakdowns or ulcerations fail to respond to primary treatment or when a patient’s status and risk factors indicate high risk for advanced complications (7).
Barriers to Appropriate Foot Care
Barriers to comprehensive foot exams include time restraints, lack of awareness and training about the importance of preventive foot exams, and lack of suitable tools such as a monofilament, tuning fork, or reflex hammer. The average primary care provider visit lasts <15 minutes, and a routine foot exam typically takes 3 minutes (8). When patients do not report foot pain or a specific foot problem or do not specifically request a foot exam, providers may not see the necessity of completing a routine foot exam. Additionally, for providers who are unfamiliar with the merits or components of a foot exam (i.e., visual, sensory, and pulse checks) and do not have available training, these exams may be overlooked. Occasionally, patients may refuse their provider’s request to perform a foot exam if they are uncomfortable having their feet exposed or examined (8,10). Overcoming the real-world barriers to routine comprehensive foot exams at every appointment is essential to reduce morbidity and mortality associated with foot complications.
Project Purpose
A quality improvement project was implemented at a primary care office in the southeastern United States that serves patients from all socioeconomic backgrounds, races, and religious affiliations from infancy to 100 years of age. The site cares for ∼16,000 patients annually, and 30% have diagnosed diabetes. After reviewing the clinic’s CMS quality measure reports, the office manager and providers implemented a quality improvement project to increase the rate of foot checks among patients with diabetes to detect foot abnormalities and prevent or reduce the severity of further complications. The project sample included adult patients aged 18–75 years with diabetes (type 1 or type 2) who presented for initial and follow-up appointments. The clinical question they sought to answer was, “Will the implementation of an EMR foot exam template, placement of foot exam posters in exam rooms, and staff education increase the frequency of routine foot exams and increase the detection of foot abnormalities among patients with diabetes in this primary care setting?
Interventions and Methods
Bonnel and Smith (11) defined the framework of a quality improvement project as abstractions of reality that represent situations. The framework should provide a foundation and determine the basis of its scope of practice. The guiding framework used for this quality improvement project was the four-step model for organizing and carrying out change known as the Plan-Do-Check-Act cycle. Step 1 is to recognize an opportunity for change. Step 2 is to test the change by implementing a small-scale intervention. The third step is to review results and analyze what was learned. The final step is to act by making the decision to either continue the intervention or evaluate a different plan (12).
Project Design
A retrospective chart review was conducted to determine the percentage of patients with diabetes who received a foot exam and to identify the number and type of abnormalities detected during a 3-month pre-intervention period from September 2014 through November 2014. Subsequently, the entire practice was introduced to the quality improvement project. Staff were educated about the ADA standards of care and specifically the ADA recommendations for foot care, and informational posters were placed in all exam rooms to educate patients about proper foot care (7).
The clinic’s medical assistants and nurses were instructed to ask patients with diabetes to remove their shoes and socks after vital signs were obtained. During visits, the providers conducted thorough foot exams for all patients with diabetes. The goal was to provide foot exams during every follow-up visit. The providers were encouraged to use the template in the EMR to document foot exams for patients with diabetes. Three months after implementation of the intervention, the percentage of patients with diabetes who received a routine foot exam was calculated, and the numbers and types of foot abnormalities detected were tallied.
Instruments for Outcomes Measurement
To evaluate the intervention, the percentage of patients with diabetes who received a foot exam before implementation of the intervention was compared to the percentage of patients with diabetes who received a foot exam within 3 months after the intervention was initiated, as well as the numbers and types of foot abnormalities detected during the respective time periods. Data were de-identified and aggregated for this quality improvement project.
Data Collection
The practice manager and information technology specialists gathered data from the EMR system identifying International Classification of Diseases (ICD)-9 and ICD-10 codes to obtain the pre-intervention and post-implementation outcome measures. Pre-intervention data were gathered for the 3-month period of September to November 2014. The intervention was initiated in August 2015, and post-intervention data were collected for the 3-month period from September to November 2015. Diabetes initial and follow-up appointments are scheduled throughout the year without an increase in volume during any particular months. An ICD-9 code search for diabetes mellitus (type 1 and type 2), including codes 250.00–250.03, was used to collect pre-intervention data and post-intervention data through September 2015, and an ICD-10 code search, including codes I11.9 and I10.9, was used for October and November 2015. All data were sorted based on the use of the EMR foot exam template for pre-intervention records and the reinforced use of the template for post-implementation records. Finally, a manual chart audit was conducted to identify documented foot abnormalities, which included calluses, bunions, ulcerations, decreased sensation, onychomycosis, less than 2+ pulses, increased dryness, and amputations.
Data Analysis and Results
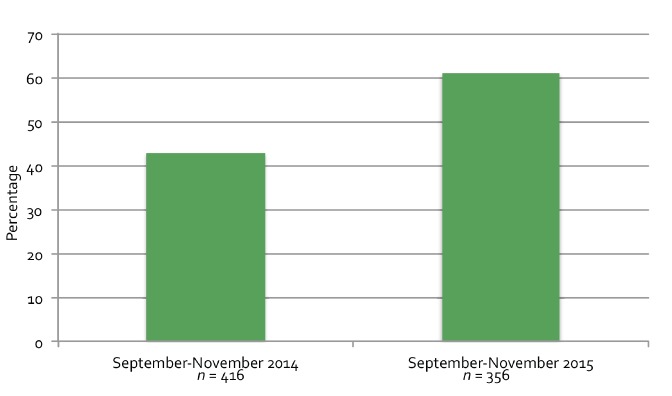
Rates of the performance of a proper foot exam and number of foot abnormalities were analyzed for the pre-intervention (n = 416) and post-implementation (n = 356) periods. Performance of foot exams increased by ∼20% (range 43–60%) (Figure 1), and the number of foot abnormalities detected increased by 67%, from 43 to 72 (Table 2). The types of foot abnormalities were also tallied (Table 2).
FIGURE 1.
Percentage of patients with diabetes who received foot exams. In 2014, 416 patients with diabetes were seen from September through November, and 180 received foot exams. In 2015, 356 patients with diabetes were seen from September through November, and 216 received foot exams.
TABLE 2.
Abnormalities Detected During Foot Exams
| Pre-Intervention | Post-Intervention | |
|---|---|---|
| Total abnormalities detected (n) | 43 | 72 |
| Ulcerations (n) | 17 | 29 |
| Decreased sensation (n) | 13 | 7 |
| Decreased pulses (n) | 7 | 12 |
| Calluses (n) | 3 | 14 |
| Plantar warts (n) | 2 | 0 |
| Amputations (n) | 1 | 1 |
| Thickened toenails (n) | 0 | 4 |
| Dry, cracked, or flaky skin (n) | 0 | 3 |
| Bunions (n) | 0 | 2 |
Discussion
Strengths and Limitations
This quality improvement project demonstrated that implementation of an EMR foot exam template, use of exam room posters, and staff education increased the percentage of foot exams completed and improved the detection of foot abnormalities among patients with diabetes in this primary care setting. The strengths of this project included crucial assistance from and buy-in of the office manager and invaluable support from staff members throughout the project. The limitations included discrepancies in documentation among staff and providers and human error resulting from manual chart audits when assessing foot abnormalities, leading to possible skewing of results. A recommendation for future projects would be to include daily flow sheets of diabetes quality measures, including foot exams, eye exams, laboratory checks, and others, for providers to use to track patients’ status.
Implications for Practice
This quality improvement project reinforces the importance of implementing interventions such as displaying foot exam posters, using EMR templates, and providing staff education to improve the rates of annual foot exams performed for patients with diabetes. It is recommended that this initiative be implemented at other practices to improve the rate of foot exams and facilitate early detection of abnormalities to prevent lower-extremity complications of diabetes. This strategy is also applicable to the early prevention and treatment for other diabetes-related complications.
Confidentiality
No identifying data (patient names, medical record numbers, or dates of birth) or demographic data were reviewed or collected during any part of this project. All participating team members were trained on the Health Insurance Portability and Accountability Act.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.Buttaro TM, Trybulski J, Bailey PP, Sandberg-Cook J. Primary Care: A Collaborative Practice. St. Louis, Mo, Mosby Elsevier, 2013 [Google Scholar]
- 2.Centers for Disease Control and Prevention National diabetes statistics report: estimates of diabetes and its burden in the United States, 2014. Atlanta, Ga, U.S. Department of Health and Human Services; Available from http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed 25 September 2014 [Google Scholar]
- 3.American Diabetes Association Statistics about diabetes. Available from http://www.diabetes.org/diabetes-basics/statistics. Accessed 25 September 2014
- 4.Heidari K, Myers PM. Brief update on the burden of diabetes in South Carolina. Am J Med Sci 2013;345:302–306 [DOI] [PubMed] [Google Scholar]
- 5.Medical University of South Carolina Diabetes Initiative of South Carolina. Available from http://clinicaldepartments.musc.edu/medicine/divisions/endocrinology/dsc. Accessed 21 January 2016
- 6.Institute for Preventative Health National Foot Health Assessment. Available from http://www.ipfh.org/images/research_materials/2012_National_Foot_Health_Assessment_June_2012.pdf. Accessed 15 February 2016
- 7.American Diabetes Association Summary of revisions. In Standards of Medical Care in Diabetes—2016. Diabetes Care 2016;39(Suppl. 1):S4–S5 [DOI] [PubMed] [Google Scholar]
- 8.Miller JD, Carter E, Shih J, et al. How to do a 3-minute diabetic foot exam. J Fam Pract 2014;63:646–656 [PubMed] [Google Scholar]
- 9.Centers for Medicaid and Medicare Services (2014) Proposed clinical quality measures for 2014. Available from http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityMeasures/Downloads/Eligible-Providers-2014-Proposed-EHR-Incentive-Program-CQM.pdf. Accessed 25 September 2015
- 10.Boulton AJ, Armstrong DG, Albert SF, et al. Comprehensive foot examination and risk assessment: a report of the Task Force of the Foot Care Interest Group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes Care 2008;31:1679–1685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonnel W, Smith KV. Proposal Writing for Nursing Capstones and Clinical Projects. New York, N.Y, Springer, 2014 [Google Scholar]
- 12.American Society for Quality Plan-Do-Check-Act (PDCA) cycle. Available from http://asq.org/learn-about-quality/project-planning-tools/overview/pdca-cycle.html. Accessed 25 September 2015