Abstract
IN BRIEF This study quantitatively measures diabetes stigma and its associated psychosocial impact in a large population of U.S. patients with type 1 or type 2 diabetes using an online survey sent to 12,000 people with diabetes. A majority of respondents with type 1 (76%) or type 2 (52%) diabetes reported that diabetes comes with stigma. Perceptions of stigma were significantly higher among respondents with type 1 diabetes than among those with type 2 diabetes, with the highest rate in parents of children with type 1 diabetes (83%) and the lowest rate in people with type 2 diabetes who did not use insulin (49%). Our results suggest that a disturbingly high percentage of people with diabetes experience stigma, particularly those with type 1 or type 2 diabetes who are on intensive insulin therapy. The experience of stigma disproportionately affects those with a higher BMI, higher A1C, and poorer self-reported blood glucose control, suggesting that those who need the most help are also the most affected by stigma.
Diabetes is a chronic disease that affects 29 million Americans and requires ongoing patient self-management to manage blood glucose and prevent complications. Although extensive research has characterized the underlying physiology of diabetes (1–3), less work has addressed the disease’s psychosocial demands and their consequent effects on management and quality of life.
Health-related stigma is a psychological factor known to influence the lives of people with chronic medical conditions such as HIV/AIDS (4–7), epilepsy (8–10), and obesity (11–14). Stigma is defined as a characteristic of a person that differs negatively from culturally defined norms, and stigmatization occurs when there is perception of a stigma that results in a punitive response. Perceived stigmatization, or felt stigma, is when an individual believes that others perceive a personal characteristic as deviant and respond unfairly (15,16). In this article, the term diabetes stigma refers to the experiences of negative feelings such as exclusion, rejection, or blame due to the perceived stigmatization of having diabetes.
Socially identifiable characteristics related to diabetes can include insulin injections, blood glucose monitoring, dietary restrictions, obesity, and hypoglycemic episodes, all of which can contribute to the experience of diabetes stigma. Studies investigating the psychosocial consequences of being stigmatized have reported patients with diabetes experiencing feelings of fear, embarrassment, blame, guilt, anxiety, and low self-esteem (17,18). These negative emotions can result in depression (19,20) and are correlated with an increased rate of complications such as retinopathy, macrovascular problems, and sexual dysfunction (21). Patients have reported “looks of contempt” when injecting insulin in public, workplace discrimination, and limitations in traveling, maintaining friendships, and adopting children resulting from diabetes stigma (18,22). Feeling stigmatized can also affect diabetes management directly because patients may be less likely to use or adopt recommended therapies that may be apparent in public, such as taking insulin injections, using an insulin pump, or self-monitoring blood glucose (23–25). In many cases, people with diabetes avoid full disclosure about their disease to both peers and health care professionals because they fear judgment or blame (18).
Type 1 and type 2 diabetes are distinct in how the diseases arise and how they are managed. Most of the existing studies on diabetes stigma have focused on type 2 diabetes (18,22,24,26–29), with a minority addressing stigma in type 1 diabetes (18,30). Additionally, many of these studies were qualitative and derived from small population samples. Although a small sample size allows for an intimate understanding of diabetes stigma, it is unclear whether these findings are representative of a large and diverse diabetes population. Here, we provide a robust quantitative and qualitative assessment of diabetes stigma in patients with type 1 or type 2 diabetes. Working with a panel of diverse patients who answer quarterly diabetes surveys, we investigated the existence, impact, and common forms of diabetes stigma.
Design and Methods
Questions about diabetes stigma were included in the dQ&A Market Research quarterly survey that is administered to a large panel of people with diabetes.
Patient Recruitment and Criteria
Inclusion criteria for the stigma analysis required respondents to be diagnosed with either type 1 or type 2 diabetes. For individuals with diabetes who were <18 years of age, parents answered on behalf of their children. People with prediabetes or gestational diabetes were excluded from this analysis. Respondents received $5 for completing the survey and were entered into a drawing to win a $200 Amazon gift card.
Data Collection
Participants in the dQ&A patient panel are asked routine survey questions that include self-reporting of several health and demographic parameters, diabetes treatment behaviors, attitudes concerning diabetes management, and questions about product choices and product satisfaction. The panel is invited to participate in four quarterly surveys per year and may be asked to participate in smaller surveys based on their patient profile. For this study, six questions were mixed with the normal survey, addressing the presence, forms, and impact of diabetes stigma. Fewer than 5% of survey questions require a response to move forward, and none of the stigma questions forced an answer. The survey was programmed and fielded using Qualtrics software (Qualtrics, Provo, Utah).
Of the 12,000 patients who re-ceived this survey in the fourth quarter of 2013, 5,422 (45%) responded to the questions about diabetes stigma, including 1,572 respondents with type 1 diabetes and 3,850 respondents with type 2 diabetes. Respondents differed by demographics, diabetes type, and diabetes management (Table 1).
TABLE 1.
Baseline Characteristics of dQ&A Patient Panel Respondents to the Stigma Survey (n = 5,422)
| Respondents With Type 1 Diabetes (%) | Respondents With Type 2 Diabetes (%) | |
|---|---|---|
| A1C ≤7% >7% |
49 51 |
61 39 |
| Therapy No insulin Insulin Pump/MDI |
0 100 92 |
55 45 14 |
| Age-group Child Adult Senior |
13 77 10 |
0 71 29 |
| Sex Male Female |
38 64 |
38 62 |
| Employment Employed Not employed Other |
59 3 38 |
43 4 53 |
| Ethnicity White Hispanic Black Asian Native American Other |
92 3 1 2 1 1 |
85 3 7 2 2 1 |
| Income | ||
| <$50,000 | 28 | 54 |
| ≥$50,000 to <$100,000 | 40 | 33 |
| ≥$100,000 | 32 | 14 |
| U.S. Region West Midwest South Northeast |
26 23 29 22 |
20 26 35 19 |
| Education | ||
| ≤High school diploma/equivalent | 13 | 16 |
| Some college or bachelor’s degree | 59 | 65 |
| Graduate or professional degree | 28 | 18 |
Respondents first indicated whether they felt that diabetes was associated with stigma (Table 2). Those who answered “Yes” were asked to identify the specific experiences of stigma they have perceived with a pick list (having a character flaw or fault, failure of personal responsibility, and being a burden on the health care system) and a write-in option for others. For the forms of stigma calculations, the proportion of responses from people with type 1 diabetes was adjusted down to a 7.5% population benchmark to better reflect type 1 prevalence within the general diabetes population.
TABLE 2.
Prevalence of Diabetes-Related Stigma (Percentage of Respondents Who Believe Diabetes Comes With Social Stigma), by Diabetes Type, Management Regimen, and Healthographic and Demographic Factors
| Diabetes Type and Therapy Regimen | Type 1 Diabetes | % (n) | Type 2 Diabetes | % (n) | P |
|---|---|---|---|---|---|
| All | 76A (1,168) | All | 52D (1,995) | A vs. D <0.0001 B vs. C 0.006 D vs. E 0.0261 D vs. F 0.038 D vs. G <0.0001 |
|
| Adults | 74B (1,001) | No insulin | 49E (1,038) | ||
| Parents | 83C (166) | Insulin | 55F (957) | ||
| Pump/MDI | 76 (1,093) | Pump/MDI | 61G (336) |
| Healthographic/Demographic Factors | Type 1 (% [n]) | Type 1 P | Type 2 (% [n]) | Type 2 P | |
|---|---|---|---|---|---|
| A1C ≤7% >7% |
74 (528) 78 (577) |
NS | 49 (1,041) 56 (751) |
<0.0005 | |
| BMI ≤25 kg/m2 >25 kg/m2 |
75 (422) 74 (542) |
NS | 47 (190) 52 (1,792) |
0.033 | |
| Self-reported blood glucose control Not well controlled Neutral Well controlled |
71 (42) 77A (430) 72B (497) |
A vs. B 0.028 | 64A (210) 53B (856) 48C (926) |
A vs. B <0.0005 A vs. C <0.0005 B vs. C 0.004 |
|
| Diabetes duration Diagnosis ≤10 years ago Diagnosis >10 years ago |
84 (397) 72 (771) |
<0.0001 | 53 (1,099) 50 (876) |
NS | |
| Sex Male Female |
68 (379) 80 (787) |
<0.0005 | 43 (638) 57 (1,352) |
<0.0005 | |
| Depression Yes No |
78 (160) 74 (811) |
NS | 58 (480) 50 (1,515) |
<0.0005 | |
| Income <$50,000 ≥$50,000 to <$100,000 ≥$100,000 |
75 (249) 76 (252) 79 (296) |
NS | 51 (846) 54 (537) 53 (220) |
NS | |
| U.S. Region West Midwest South Northeast |
76 (296) 73 (252) 76 (335) 76 (252) |
NS | 53 (397) 51 (511) 52 (688) 51 (379) |
NS | |
| Education ≤High school diploma/equivalent Some college or bachelor’s degree Graduate or professional degree |
73A (143) 74B (675) 80C (342) |
B vs. C 0.017 | 47A (291) 52B (1,301) 55C (391) |
A vs. B 0.026 A vs. C 0.004 |
|
To evaluate the impact of diabetes stigma, respondents used a 10-point scale to indicate how strongly they agreed with statements about the impact of diabetes stigma on emotional and social aspects and on diabetes management, with 1 indicating complete disagreement and 10 indicating very strong agreement. Those who selected 9 or 10 were defined as strongly agreeing with the statement. A conditional variable was created that counted respondents who selected 9 or 10 for one of the statements in each of the emotional, social, and diabetes management categories to be included in the analysis. Respondents were only counted once in each category regardless of whether they selected 9 or 10 for multiple statements. Respondents also answered an open-ended question about recommendations to reduce diabetes stigma. Open-ended responses were reviewed to identify key words and phrases that allowed for categorization into psychosocial themes. The majority of statements were placed into one category of best fit, with some statements that included multiple themes placed into more than one category. All data were analyzed using MarketSight software (MarketSight, Newton, Mass.) and Excel (Microsoft, Redmond, Wash.). Statistical significance was tested using a z test at the 95% confidence level.
Results
Prevalence of Diabetes Stigma
A significantly greater percentage of respondents with type 1 diabetes reported diabetes stigma than those with type 2 diabetes (76 vs. 52%, respectively; P <0.0001; Table 2). Factors associated with significant increases in the perception of diabetes stigma among all respondents (regardless of diabetes type) included being female and having a graduate or professional degree. There were no significant differences in reported stigma across U.S. geographical regions or annual household incomes in either diabetes population.
Among respondents with type 1 diabetes, parents of children with diabetes were significantly more likely to perceive diabetes stigma than adults with diabetes (83 vs. 74%, P = 0.006). Respondents with type 1 diabetes were not segmented by therapy intensity because 100% were on insulin, and 92% were receiving intensive therapy (using an insulin pump or multiple daily injections [MDIs]).
The perception of diabetes stigma among respondents with type 2 diabetes significantly increased with greater therapy intensity: 49% of non–insulin-using respondents reported the presence of diabetes stigma compared to 55% of those receiving insulin (P <0.0005) and 61% of those receiving intensive insulin therapy (P <0.0005). Several other factors were associated with increased perception of diabetes stigma in type 2 diabetes respondents, including A1C >7%, BMI ≥25 kg/m2, self-reported uncontrolled blood glucose, and self-reported presence of depression (Table 2).
Forms of Stigma
The most widely reported experience of diabetes stigma (regardless of diabetes type) was the perception of having a character flaw/failure of personal responsibility (81%), followed by the perception of being a burden on the health care system (65%). The greatest difference between respondents with type 1 diabetes and those with type 2 diabetes related to misunderstandings about diabetes, including views that diabetes is contagious or that all types of diabetes are the same. Of respondents who specified another form of stigma (open-ended response), 38% with type 1 diabetes vs. 16% with type 2 diabetes said they experienced stigma from misunderstandings about diabetes.
Consequences of Diabetes Stigma
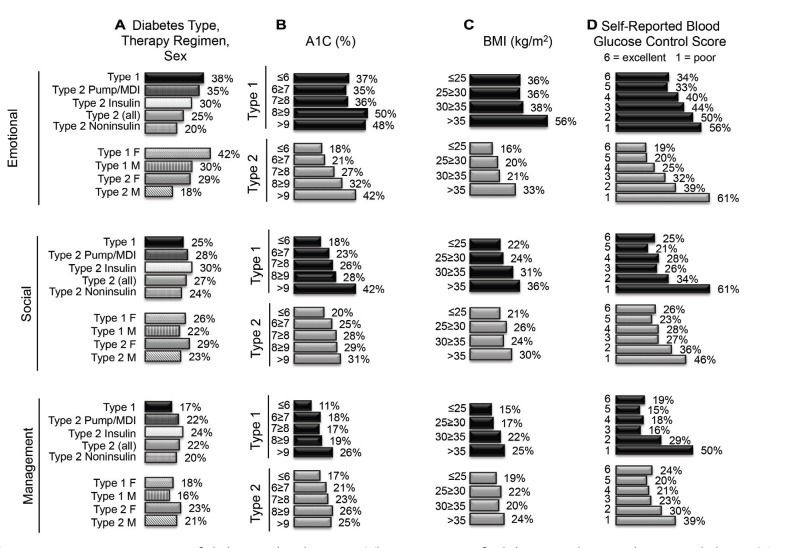
Figure 1 presents the percentage of respondents who strongly agreed (scoring 9 or 10 on a 10-point scale) that other people’s perceptions of diabetes have affected their:
Emotional life: experiencing feelings of guilt, shame, blame, embarrassment, and isolation
Social life: being open about diabetes, finding a supportive community, having a full social life, and succeeding at work
Diabetes management: successful management, adherence, good choices
FIGURE 1.
Consequences of diabetes-related stigma. The percentage of adult respondents with type 1 diabetes (Type 1, n = 1,334), type 2 diabetes (Type 2 [all], n = 3,833), type 2 diabetes on pump or MDI therapy (Type 2 Pump/MDI, n = 544), type 2 diabetes on insulin therapy (Type 2 Insulin, n = 1,721), type 2 diabetes not on insulin (Type 2 Noninsulin, n = 2,112), females with type 1 diabetes (Type 1 F, n = 860), males with type 1 diabetes (Type 1 M, n = 472), females with type 2 diabetes (Type 2 F, n = 2,349), and males with type 2 diabetes (Type 2 M, n = 1,468) who strongly agree (scoring 9 or 10 on a 10-point scale) that other people’s perceptions of diabetes have caused them to experience difficulty with an emotional aspect (experiencing feelings of guilt, shame, blame, embarrassment, and isolation), social aspect (being open about diabetes, finding a supportive community, having a full social life, and succeeding at work), or diabetes management aspect (successful management, adherence, and good choices) of living with diabetes. Statements are segmented by the factors associated with a significant increase in reporting of diabetes stigma (Table 1), including diabetes type, therapy regimen, and sex (A), A1C (B), BMI (C), and self-reported blood glucose control (D).
The impact of diabetes stigma on all aspects of life was significantly associated with a higher A1C (>7 vs. ≤7%), higher BMI (≥25 vs. <25 kg/m2), and poorer self-reported blood glucose control (uncontrolled vs. controlled). Respondents with type 1 or type 2 diabetes with uncontrolled blood glucose reported the highest rates of stigma in all aspects of their lives (Figure 1D).
Emotional Life
Respondents with type 1 diabetes (38%), particularly females (42%), strongly agreed that other people’s perceptions of diabetes have led them to experience guilt, shame, blame, embarrassment, and isolation. This is in contrast to the lower levels of reported emotional impact from stigma in males with type 1 diabetes (30%) and in respondents with type 2 diabetes (25%). Males with type 2 diabetes reported the lowest emotional impact of diabetes stigma (18%). Among respondents with type 2 diabetes, however, the impact of diabetes stigma on the emotional aspects of life was associated with increased therapy intensity (20% in noninsulin users vs. 30% in insulin users vs. 35% in pump/MDI users) (Figure 1A).
Social Life
More than one in four respondents with type 1 diabetes (22–26%) or type 2 diabetes (23–30%) strongly agreed that diabetes stigma negatively affected their social life (Figure 1A).
Diabetes Management
There was a significant difference between respondents with type 1 diabetes (17%) and those with type 2 diabetes (22%) who felt the negative impact of diabetes stigma on diabetes management (P <0.0005), with a particular disparity in females with type 1 diabetes compared to females with type 2 diabetes (18 vs. 23%; P = 0.003) (Figure 1A).
Ways to Reduce Diabetes Stigma
Respondents shared recommendations for ways to reduce diabetes stigma. Increasing public knowledge about the general causes of diabetes was the most common response, mentioned by 46% of adults with type 1 diabetes and 40% of respondents with type 2 diabetes. To a lesser extent, both respondents with type 1 diabetes (18%) and those with type 2 diabetes (19%) recommended increased education about the management of diabetes, such as how distinct types of diabetes require different treatments. There was a stark difference in the percentage of respondents who suggested that the naming for diabetes should be changed (19% of respondents with type 1 diabetes favored this change vs. 0% with type 2 diabetes).
Both respondents with type 1 diabetes (13%) and those with type 2 diabetes (14%) recommended changes that have public impact (e.g., revising policies, creating school programs, changing nutritional options in restaurants, and using social media, celebrity campaigns, and fundraising/awareness actions). Respondents with type 2 diabetes (15%) and those with type 1 diabetes (10%) hoped to reduce the perception that people with diabetes are considered to be incapable or to have limited abilities by increasing awareness of the social or work-related aspects of diabetes. Other respondents advocated for greater general education about diabetes, with this recommendation mentioned more by those with type 2 diabetes (17%) than by those with type 1 diabetes (9%).
Conclusions
Prevalence of Diabetes Stigma
There is a limited understanding of the prevalence of diabetes stigma in the larger population, and few studies have examined stigma in both type 1 and type 2 diabetes. By surveying a large and diverse patient panel engaged by dQ&A Market Research, we found that a majority of people with type 1 or type 2 diabetes reported that they felt stigma associated with their disease. This perception was significantly higher in individuals with type 1 diabetes compared to those with type 2 diabetes and was particularly elevated in females and the parents of children with type 1 diabetes. We found that increased perception of diabetes stigma was associated with being female and with having higher education levels. For those with type 2 diabetes, perception of diabetes stigma appeared to be associated with uncontrolled diabetes and higher visibility of the disease, as suggested by the greater perception of diabetes stigma among those with higher A1C levels, higher BMI, poorly controlled blood glucose, depression, and greater therapy intensity.
The finding that respondents with type 1 diabetes perceived more diabetes stigma than those with type 2 diabetes may be surprising, given previous research and public discussion focused on the stigma associated with type 2 diabetes (18,22,24,26–29). In type 2 diabetes, diabetes stigma increased with intensity of therapy. With that in mind, it is perhaps not surprising that individuals with type 1 diabetes felt more stigma than others, given the need for MDI or pump therapy, frequent blood glucose testing, and/or use of a continuous glucose monitoring device, all of which are highly visible to others.
Experiences of Diabetes Stigma
The most commonly reported experience of stigma was the perception that diabetes is a character flaw or the result of a failure in personal responsibility. Patients have described feeling judged and blamed by others for causing their own diabetes through overeating, poor diet, inactivity, laziness, or being overweight or obese. This is consistent with qualitative studies in type 2 diabetes that have found shame and blame to be a common theme associated with stigma (17,18). However, we found this form of stigma common to both respondents with type 1 diabetes (83%) and those with type 2 diabetes (81%), demonstrating that this misconception contributes to stigma for both types of diabetes. This disparity may be the result of less public awareness of type 1 diabetes, leading to confusion about whether it is different from type 2 diabetes, whether it is contagious, which therapies are needed (e.g., diet and exercise vs. taking pills vs. insulin therapy), and other misunderstandings about the etiology and management of the disease.
The second most common form of diabetes stigma felt by respondents in both groups was the belief that people with diabetes are a burden on the health care system. This could be the result of greater public focus on controlling health care costs, high-profile reports on the rising rates of type 2 diabetes, and the common perception that diabetes is a failure of personal responsibility rather than a combination of genetic, environmental, and lifestyle factors.
Recommendations to Reduce Diabetes Stigma
The most common recommendation to reduce diabetes stigma was to focus on increasing diabetes education for the general public, particularly with regard to the causes of the various forms of the disease. Many individuals with type 1 diabetes, but none with type 2 diabetes, suggested changing the naming of diabetes, potentially indicating that people with type 1 diabetes feel additional stigma related to misperceptions of the different types of diabetes. Indeed, 19% of adults and parents of children with type 1 diabetes suggested changing the naming and lexicon associated with diabetes, specifically disassociating type 1 from type 2 diabetes or avoiding terms such as “obese” or “diabetic.” These data support the need to look critically at current awareness efforts to ensure that they use appropriate language to educate the public about what causes type 1 and type 2 diabetes and how the diseases are managed.
Consequences of Diabetes Stigma
Respondents with the poorest self-reported degree of blood glucose control reported the highest rates of diabetes stigma that adversely affected the social, emotional, and diabetes management aspects of their lives. This was true for respondents with either type 1 or type 2 diabetes, suggesting that groups who need the most help and support for their diabetes are also those most negatively affected by diabetes stigma.
Limitations
Our study has several limitations. First, all answers, including demographic data, were self-reported and collected online. The questions most influenced by this issue are those that use a scale scoring system of agreement because each person has a different definition of agreement, and comfort levels vary in sharing experiences of diabetes stigma. Also, parents or guardians of children with type 1 diabetes were allowed to take the survey on behalf of their child. These answers reflect the parents’ perceptions of diabetes stigma for their child and not necessarily the children’s experiences. Second, although we surveyed a robust and diverse population, our panel is not nationally representative; respondents recruited from online diabetes communities skew toward those who may be more engaged in their diabetes management and have the resources to seek support online. The panel’s representation of ethnic minorities is lower than in the general diabetes population.
Implications and Future Directions
Our results suggest that a majority of people with type 1 or type 2 diabetes believe the disease comes with stigma, which negatively affects many aspects of daily life. People with type 1 diabetes appear to experience more diabetes stigma than those with type 2 diabetes, although feelings of stigma increase as therapy intensity increases (i.e., from noninsulin to insulin to intensive insulin therapy).
We hope this work prompts further exploration of the differences in diabetes stigma experienced by people with type 1 or type 2 diabetes, potentially leading to identification of the reasons why certain subpopulations are at risk for increased perception of stigma. Further research should be performed on how diabetes stigma affects daily life, which specific aspects of therapy are associated with the greatest diabetes stigma, and which therapies and technologies mitigate the negative feelings that stigmatized people face.
There is an overwhelming need for increased public education and better-informed conversation about what causes diabetes and the daily experience of living with the disease. The widely held misconception that people with diabetes are responsible for developing their disease or that they have a character flaw is the predominant form of stigma directed against people with diabetes. There may be cases in which health care provider communication that is perceived as judging and blaming can contribute to diabetes stigma in patients, particularly among those who are struggling to attain effective disease management. Health care professionals can play a key role in addressing diabetes stigma through gaining a better understanding of how stigma affects daily life and helping to promote education about the disease.
Future education can target misbelief by emphasizing the complex genetic, environmental, biological, and lifestyle causes of both type 1 and type 2 diabetes, increasing understanding of the challenges of diabetes management, and examining the negative impact of stigmatizing “shame and blame” beliefs. Given the high prevalence of stigma, the diabetes community should develop campaigns and interventions to help address the issue.
Acknowledgments
The authors thank Bennet Dunlap, Manny Hernandez, Scott Johnson, and Kerri Sparling for inspiration on developing the early questions for patients and for bringing various important patient perspectives to this project. Additional thanks go to Jasmine Carvalho and Vincent Wu of dQ&A for assistance in preparing data for the poster; to Rebecca S. Xu, Jenny S. Tan, and Sabrina Lee of Close Concerns for assistance with the bucketing of open-ended responses for our analysis; and to Sarah A. Odeh of Close Concerns for critically reading the manuscript.
Author Contributions
N.F.L. participated in the analysis, interpretation, and presentation of the data and critical revision of the manuscript. A.S.B. participated in the study conception and design; analysis and interpretation of data; and critical revision of the manuscript. A.E.F. participated in the quantification, analysis, and presentation of data and the drafting of the manuscript. M.F.W. and R.W. participated in the study conception and design; quantification of data; and critical revision of the manuscript. S.J.G. and K.L.C. participated in the interpretation of data and critical revision of the manuscript. A.S.B., K.L.C. and R.W. supervised the project. R.W. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Publication
This work was presented as a poster at the American Diabetes Association’s 74th Scientific Sessions in San Francisco, Calif., in June 2014.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Funding
This work was supported by dQ&A Market Research, The diaTribe Foundation, and Close Concerns.
References
- 1.Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature 2001;414:782–787 [DOI] [PubMed] [Google Scholar]
- 2.Muoio DM, Newgard CB. Mechanisms of disease: molecular and metabolic mechanisms of insulin resistance and beta-cell failure in type 2 diabetes. Nat Rev Mol Cell Biol 2008;9:193–205 [DOI] [PubMed] [Google Scholar]
- 3.Bluestone JA, Herold K, Eisenbarth G. Genetics, pathogenesis and clinical interventions in type 1 diabetes. Nature 2010;464:1293–1300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? AIDS Educ Prev 2003 Feb;15(3):49–69 [DOI] [PubMed] [Google Scholar]
- 5.Mahajan AP, Sayles JN, Patel VA, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS 2008;22(Suppl. 2):S67–S79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abadía-Barrero CE, Castro A. Experiences of stigma and access to HAART in children and adolescents living with HIV/AIDS in Brazil. Soc Sci Med 2006;62:1219–1228 [DOI] [PubMed] [Google Scholar]
- 7.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med 2003;57:13–24 [DOI] [PubMed] [Google Scholar]
- 8.Jacoby A, Snape D, Baker GA. Epilepsy and social identity: the stigma of a chronic neurological disorder. Lancet Neurol 2005;4:171–178 [DOI] [PubMed] [Google Scholar]
- 9.MacLeod JS, Austin JK. Stigma in the lives of adolescents with epilepsy: a review of the literature. Epilepsy Behav 2003;4:112–117 [DOI] [PubMed] [Google Scholar]
- 10.Whatley AD, DiIorio CK, Yeager K. Examining the relationships of depressive symptoms, stigma, social support and regimen-specific support on quality of life in adult patients with epilepsy. Health Educ Res 2010;25:575–584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Puhl RM, Moss-Racusin CA, Schwartz MB, Brownell KD. Weight stigmatization and bias reduction: perspectives of overweight and obese adults. Health Educ Res 2008;23:347–358 [DOI] [PubMed] [Google Scholar]
- 12.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17:941–964 [DOI] [PubMed] [Google Scholar]
- 13.Zettel-Watson L, Britton M. The impact of obesity on the social participation of older adults. J Gen Psychol 2008;135:409–423 [DOI] [PubMed] [Google Scholar]
- 14.Sikorski C, Luppa M, Brähler E, König H-H, Riedel-Heller SG. Obese children, adults and senior citizens in the eyes of the general public: results of a representative study on stigma and causation of obesity. PLoS One 2012;7:e46924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goffman E. Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs, N.J, Prentice-Hall, 1963 [Google Scholar]
- 16.Link BG, Phelan JC. Stigma and its public health implications. Lancet 2006;367:528–529 [DOI] [PubMed] [Google Scholar]
- 17.Schabert J, Browne JL, Mosely K, Speight J. Social stigma in diabetes: a framework to understand a growing problem for an increasing epidemic. Patient 2013;6:1–10 [DOI] [PubMed] [Google Scholar]
- 18.Browne JL, Ventura A, Mosely K, Speight J. ‘I call it the blame and shame disease’: a qualitative study about perceptions of social stigma surrounding type 2 diabetes. BMJ Open 2013;3:e003384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldney RD, Phillips PJ, Fisher LJ, Wilson DH. Diabetes, depression, and quality of life: a population study. Diabetes Care 2004;27:1066–1070 [DOI] [PubMed] [Google Scholar]
- 20.Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care 2008;31:2383–2390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med 2001;63:619–630 [DOI] [PubMed] [Google Scholar]
- 22.Tak-Ying Shiu A, Kwan JJY-M, Wong RY-M. Social stigma as a barrier to diabetes self-management: implications for multi-level interventions. J Clin Nurs 2003;12:149–150 [DOI] [PubMed] [Google Scholar]
- 23.Polonsky WH, Fisher L, Guzman S, Villa-Caballero L, Edelman SV. Psychological insulin resistance in patients with type 2 diabetes: the scope of the problem. Diabetes Care 2005;28:2543–2545 [DOI] [PubMed] [Google Scholar]
- 24.Ong WM, Chua SS, Ng CJ. Barriers and facilitators to self-monitoring of blood glucose in people with type 2 diabetes using insulin: a qualitative study. Patient Prefer Adherence 2014;8:237–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ritholz MD, Smaldone A, Lee J, Castillo A, Wolpert H, Weinger K. Perceptions of psychosocial factors and the insulin pump. Diabetes Care 2007;30:549–554 [DOI] [PubMed] [Google Scholar]
- 26.Teixeira ME, Budd GM. Obesity stigma: a newly recognized barrier to comprehensive and effective type 2 diabetes management. J Am Acad Nurse Pract 2010;22:527–533 [DOI] [PubMed] [Google Scholar]
- 27.Reid TS. Insulin for type 2 diabetes mellitus: separating the myths from the facts. Insulin 2007;2:182–189 [Google Scholar]
- 28.Wellard SJ, Rennie S, King R. Perceptions of people with type 2 diabetes about self-management and the efficacy of community based services. Contemp Nurse 2008;29:218–226 [DOI] [PubMed] [Google Scholar]
- 29.Broom D, Whittaker A. Controlling diabetes, controlling diabetics: moral language in the management of diabetes type 2. Soc Sci Med 2004;58:2371–2382 [DOI] [PubMed] [Google Scholar]
- 30.Winkley K, Ismail K, Landau S, Eisler I. Psychological interventions to improve glycaemic control in patients with type 1 diabetes: systematic review and meta-analysis of randomised controlled trials. BMJ 2006;333:65–70 [DOI] [PMC free article] [PubMed] [Google Scholar]