Abstract
Purpose of the Study:
Janus, the two-faced, Roman god of beginnings and transitions, is used as a metaphor to explore our personal narratives and our quantitative research on the experiences of older women with dementia in long-term care (LTC). Two research questions are addressed: (a) How do our quantitative data map onto our mothers’ experiences? (b) What lessons do our mothers’ experiences offer for the care of older women with dementia?
Design and Methods:
Informed by a life-course perspective, we triangulate administrative data on 3,717 women with dementia receiving LTC in British Columbia, Canada, with personal narratives—the stories of our mothers who made the transition from home care into residential (nursing home) care.
Results:
Our quantitative data reveal that the home care to residential care transition is the most common LTC trajectory for women with dementia who are most likely to be widowed and living alone in suburban areas. On entry into residential care, they exhibit greater frailty in terms of activities of daily living, cognition, aggression, and incontinence. Our personal narrative data on our mothers reveals that the relatively straightforward pathways through LTC for women with dementia, are often considerably more complex in a real-world context. Attention is drawn to the public and private services, hospitalization patterns, and substantial communication gaps experienced by our moms and families.
Implications:
A life-course perspective, and qualitative and quantitative data facilitate understanding the care journeys—health and service trajectories of older women with dementia.
Keywords: Relocation and transition, Qualitative research methods, Quantitative research methods, Continuum of care, Dementia
Writing over a decade ago about their mother’s experience of nursing home care after a serious stroke, Kane and West (2005) argued that society appears uninterested in making the necessary commitment to care for frail older adults in creative, compassionate, and appropriate ways aligned with goals of quality of care and quality of life. In this special issue called, Aging-It’s Personal, we explore this concern by triangulating data from our funded research program with our personal narratives describing our mothers’ experiences as clients of the long-term care (LTC) system.
As social gerontologists, we have spent much of our careers studying health service provision for vulnerable older adults. As adult children, we have recent personal and family-centered experience related to our mothers’ care journeys as women who began their service trajectory in home care and continued on to become clients of residential (nursing home) care until their deaths. In this article, we employ the metaphor of Janus, the two-faced Roman god of beginnings and transitions, to explore how our personal and professional worlds have intertwined, affecting us indelibly as family members, sparking our research questions, and giving us a greater appreciation for the ways that care is navigated. We consider what these overlaps reveal about the experiences of older women living with dementia and their families, drawing on a life-course perspective as a theoretical lens, to link our personal and professional perspectives. Two research questions are addressed: (a) How well do our quantitative data map onto our mothers’ experiences? (b) What lessons do our mothers’ experiences offer for the care of older women with dementia?
Background
The formal LTC sector includes a broad array of publicly and privately funded services, ranging from home care (HC; including home nursing, personal support, and therapies) through assisted living (AL) and finally, 24-h nursing home or residential care (RC; Menec et al., 2009). These services occupy an important place within the overall health care continuum but have been criticized as being fragmented and poorly integrated and coordinated (Dilworth-Anderson, Hilliard, Williams, & Palmer, 2011). Additionally, because these services (acute care, primary care, home care, and residential care) are organized and delivered in silos, no one sector has responsibility for ensuring continuity across systems. In other words, clients are viewed as leaving one system of care (e.g., home care) to enter another (e.g., nursing home care) resulting in care provision that is guided by a “discharge mentality,” rather than functioning under a philosophy of “continuous care management” (Dilworth-Anderson et al., 2011).
Additionally, research has focused more on singular care transitions (Wysocki et al., 2014) and their predictors (Callahan et al., 2012; Luppa et al., 2010) rather than examining the overall patterns of service use for LTC clients over time (Coleman, Min, Chomiak, & Kramer, 2004; Murtaugh & Litke, 2002). This gap in knowledge, coupled with the increasing prevalence of dementia among older persons, provides an important rationale for this work (Alzheimer Society of Canada, 2010; WHO, 2015). Improved understanding of the pathways, predictors, and experiences of persons with dementia and their families is crucial for health care planners and decision makers in the multifaceted care of these complex populations.
A life-course perspective acknowledges the diversity and complexity of experience across time and space and is therefore useful in understanding the care journeys of women with dementia (McDaniel & Bernard, 2011). Key principles of this perspective include a consideration of temporal (how what happens in early life affects outcomes in later life) and geographical events (e.g., wars, recessions) and their contexts (social, political, and economic); the timing of lives (e.g., adolescence, old age); the heterogeneity of individuals (characteristics that influence different trajectories such as age, gender, social class, and ethnicity); linked lives (lives are interdependent and connected particularly within family units); and human agency and personal control (individuals are active agents who shape and are shaped by social structures and events; Dannefer, 2011; Elder, 1985; Mayer, 2009; McDaniel & Bernard, 2011).
The health of an individual with dementia on the LTC trajectory from home into nursing home care tends to be characterized as one of progressive disability in terms of cognitive and physical functioning (Moorhouse & Mallery, 2012). At the same time, the pace of change can be much slower compared to those with other life-threatening illnesses such as cancer or heart failure (Moorhouse & Mallery, 2012), leading some researchers to suggest that persons with dementia represent a distinct subgroup with unique service requirements (Covinsky, Eng, Lui, Sands, & Yaffe, 2003; Kane & West, 2005). For some, the slower pace of change can make it harder to recognize their palliative status, thereby restricting access to specialized, end-of-life services when needed (Covinsky et al., 2003). Research also indicates that persons with dementia experience more care transitions than others (Coleman & Boult, 2003) and have a higher risk of adverse events such as medication errors, hospitalizations, stress and anxiety, and other problems than those without the disease (Manderson et al., 2012). Although most individuals with dementia are cared for at home, the progression of the disease often leads to higher levels of care (McCabe, You, & Tatangelo, 2016), with increased likelihood of institutionalization over time (Eska et al., 2013).
Informal caregivers form the bulwark of the support systems of persons with dementia, providing a wide range of services such as help with personal care and instrumental activities (Gitlin & Wolff, 2011; Rosenthal, Martin-Matthews, & Keefe, 2007). By necessity, family members’ roles shift across the care journey—from more diverse and intensive primary caring activities in the home, to a range of secondary caring activities on institutionalization (Gaugler, 2005; Moon, 2016). But these shifts can result in increased stress, and burn out, financial strain, social isolation, and reduced quality of life (Gaugler, Kane, Kane, Clay, & Newcomer, 2005; McCabe et al., 2016; Rosenthal et al., 2007). Finally, it is long recognized that LTC does a poor job of integrating family members sufficiently into the interdisciplinary care team thereby heightening their stress, and promoting negative outcomes especially around care transitions and trajectories (Dilworth-Anderson et al., 2011).
Design and Methods
In this article, we triangulate two sources of data: quantitative data from our funded research program, with our personal narratives about the experiences of our mothers who lived with dementia, and who received both home care and residential care in the later years of their lives. The descriptive, quantitative data explore LTC service use pathways and predictors among clients living in the small but populous health region of Fraser Health (FH) in British Columbia, Canada. We link data from client management files, clinical and functional assessments (obtained using the Resident Assessment Instrument—Minimum Data Set for Residential Care [RAI-MDS 2.0] and for Home/Community Care [RAI-HC], Canadian Versions), and hospital discharge data files. The RAI assessment instruments have been extensively tested and validated in more than 30 countries worldwide, including the United States and Canada (Hirdes, Mitchell, Maxwell, & White, 2011).
Our study cohort includes all female LTC clients aged 65 and older as of January 1, 2008 who received publicly subsidized home care (i.e., home support, day programs, other home, and community care services), professional direct care services (e.g., home nursing, occupational therapy, physiotherapy, nutritional services), assisted living or long-term “residential care” (i.e., the term used in British Columbia for nursing home care), with an initial service start in the 2008 calendar year. Only those who had a diagnosis of dementia at some point in their care trajectories between January 1, 2008 and March 31, 2012 were included (n = 3,717). We were particularly interested in women who made the transition from home care to residential care (HC > RC; n = 1,340, 36.1%) because this pathway matched our mothers’ experiences. (Only 761 (56.8%) of these women had valid RAI assessments completed at both entry into HC and entry into RC, thereby limiting our final study sample to this latter group. A comparative analysis of the missing data revealed few significant differences between those who had assessments and those who did not.)
Our analyses focused on the prevalence of common LTC pathways (home care only [HC], HC to residential care [HC > RC], and RC only [RC]) and the impact of sociodemographic/economic variables (age, marital status, education, income, living alone, and residence), health variables (falls risk, activities of daily living [ADLs], cognitive performance [CPS], depression, medical frailty [CHESS Score], pain, chronic conditions, incontinence, aggression, and mortality), the availability of a primary caregiver (type and hours of care per week), and service use variables (days in LTC, number of hospitalizations and days in hospital). We then undertook a second descriptive analysis to examine the HC > RC group comparing the characteristics of women with dementia on entry into HC (Time 1) and on the transition into RC (Time 2).
Following our analyses of this transition, we proceed to a consideration of our mothers’ stories, analyzing our transcripts by reading and re-reading the written vignettes and hand coding them for recurring, converging, and diverging themes, patterns, and concepts (Boyatzis, 1998; Braun & Clarke, 2012), paying close attention to the methods of narrative analysis (Riessman, 2008). To address our research questions, we consider core concepts from the life-course perspective that exemplify the heterogeneity and variability of human lives (age, gender, marital and health status), and care contexts, but we were also able to examine the range of care options that were both needed and available, linked lives (role of family), and issues of human agency and personal control.
Results
The Pathways and Characteristics of Women With Dementia Transitioning Through LTC
Table 1 presents the descriptive characteristics of our sample of women with dementia who received some form of LTC from 2008 to 2012. Movement from HC to RC was the most common trajectory for these women (36.1%), followed by HC only (31.7%) and RC only (27.3%). Only a small proportion used various other form(s) of care.
Table 1.
Characteristics of Women With Dementia in Long-term Care in a Canadian Context (2008–2011)a
| All women with dementia (N = 3,717) | Care pattern HC onlyb (N = 1,179; 31.7%) | Care pattern HC > RC (N = 1,340; 36.1%) | Care pattern RC only (N = 1,014; 27.3%) | Other care pattern (N = 184; 5.0%) | p Valuec | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | N/mean | Percentage/(CI) | N/mean | Percentage/(CI) | N/mean | Percentage/(CI) | N/mean | Percentage/(CI) | N/mean | Percentage/(CI) | |
| Demographic | |||||||||||
| Aged | 83.5 | (83.3, 83.7) | 83.1 | (82.7, 83.4) | 83.3 | (82.9, 83.7) | 84.4 | (84.0, 84.8) | 83.5 | (82.5, 84.4) | <.001 |
| % 85 or olderd | 1,728 | 46.5% | 518 | 43.9% | 599 | 44.7% | 533 | 52.6% | 78 | 42.4% | <.001 |
| High school or higher | 1,656 | 46.7% | 511 | 44.8% | 611 | 47.1% | 453 | 48.7% | 81 | 45.0% | .325 |
| Low income (supplement)e | 1,642 | 44.9% | 599 | 52.5% | 606 | 45.5% | 329 | 32.8% | 108 | 59.3% | <.001 |
| Living alone | 1,454 | 39.6% | 445 | 38.2% | 547 | 40.9% | 354 | 35.9% | 108 | 59.3% | <.001 |
| Marital status | <.001 | ||||||||||
| Married | 972 | 26.5% | 333 | 28.6% | 404 | 30.2% | 208 | 21.1% | 27 | 14.9% | |
| Widowed | 2,319 | 63.2% | 707 | 60.7% | 809 | 60.5% | 669 | 67.8% | 134 | 74.0% | |
| Separated | 49 | 1.3% | 20 | 1.7% | 15 | 1.1% | 12 | 1.2% | 2 | 1.1% | |
| Divorced | 215 | 5.9% | 69 | 5.9% | 67 | 5.0% | 65 | 6.6% | 14 | 7.7% | |
| Never married | 107 | 2.9% | 32 | 2.7% | 40 | 3.0% | 31 | 3.1% | 4 | 2.2% | |
| Other | 7 | 0.2% | 4 | 0.3% | 2 | 0.1% | 1 | 0.1% | 0 | 0.0% | |
| Location of residencef | <.001 | ||||||||||
| Rural | 399 | 10.7% | 156 | 13.2% | 157 | 11.7% | 73 | 7.2% | 13 | 7.1% | |
| Suburban | 1,336 | 35.9% | 408 | 34.6% | 501 | 37.4% | 367 | 36.2% | 60 | 32.6% | |
| Urban | 1,982 | 53.3% | 615 | 52.2% | 682 | 50.9% | 574 | 56.6% | 111 | 60.3% | |
| Health | |||||||||||
| Falls riskg | .023 | ||||||||||
| Low | 2,003 | 54.4% | 647 | 55.5% | 755 | 56.3% | 501 | 50.3% | 100 | 54.9% | |
| Medium | 881 | 23.9% | 293 | 25.2% | 292 | 21.8% | 253 | 25.4% | 43 | 23.6% | |
| High | 799 | 21.7% | 225 | 19.3% | 293 | 21.9% | 242 | 24.3% | 39 | 21.4% | |
| ADLh | 1.4 | (1.4, 1.5) | 0.9 | (0.9, 1.0) | 1.1 | (1.0, 1.1) | 2.6 | (2.5, 2.7) | 0.6 | (0.4, 0.7) | <.001 |
| CPSi | 2.4 | (2.4, 2.5) | 2.1 | (2.1, 2.2) | 2.3 | (2.2, 2.4) | 3.1 | (3.0, 3.1) | 1.7 | (1.6, 1.8) | <.001 |
| Depressionj | 1.7 | (1.6, 1.8) | 1.6 | (1.5, 1.8) | 1.9 | (1.7, 2.0) | 1.6 | (1.4, 1.7) | 1.7 | (1.3, 2.0) | .016 |
| Medical frailty (CHESS score)k | 1.3 | (1.3, 1.4) | 1.2 | (1.1, 1.3) | 1.4 | (1.3, 1.4) | 1.5 | (1.4, 1.5) | 1.2 | (1.1, 1.4) | <.001 |
| PAINl | 0.9 | (0.9, 1.0) | 1.0 | (1.0, 1.1) | 0.9 | (0.9, 1.0) | 0.8 | (0.7, 0.9) | 1.0 | (0.8, 1.1) | <.001 |
| Number of chronic conditionsm | 2.7 | (2.6, 2.7) | 2.8 | (2.7, 2.9) | 2.6 | (2.5, 2.7) | 2.5 | (2.4, 2.6) | 3.2 | (2.9, 3.4) | <.001 |
| Incontinencen | 1,423 | 38.7% | 380 | 32.6% | 439 | 32.8% | 559 | 56.2% | 45 | 24.7% | <.001 |
| Aggressiono | 600 | 16.3% | 135 | 11.6% | 220 | 16.4% | 238 | 23.9% | 7 | 3.8% | <.001 |
| Died within study period | 1,116 | 30.0% | 251 | 21.3% | 420 | 31.3% | 409 | 40.3% | 36 | 19.6% | <.001 |
| Primary caregiverp | <.001 | ||||||||||
| Spouse | 685 | 18.8% | 224 | 19.2% | 311 | 23.2% | 137 | 14.4% | 13 | 7.1% | |
| Child/child-in-law (live with) | 893 | 24.5% | 358 | 30.7% | 318 | 23.8% | 181 | 19.0% | 36 | 19.8% | |
| Child/child-in-law (not live with) | 1,588 | 43.7% | 439 | 37.7% | 538 | 40.2% | 497 | 52.2% | 114 | 62.6% | |
| Other (relative, friend, neighbor) | 437 | 12.0% | 136 | 11.7% | 160 | 12.0% | 122 | 12.8% | 19 | 10.4% | |
| No primary caregiver | 35 | 1.0% | 8 | 0.7% | 11 | 0.8% | 16 | 1.7% | 0 | 0.0% | |
| Hours of informal care weeklyp | 19.4 | (18.7, 20.1) | 21.8 | (20.6, 23.0) | 22.5 | (21.2, 23.8) | 13.3 | (12.0, 14.5) | 12.0 | (10.3, 13.6) | <.001 |
| Service use | |||||||||||
| Total days in long-term care | 752.5 | (738.0, 767.1) | 624.9 | (600.6, 649.3) | 923.7 | (900.8, 946.6) | 654.2 | (626.6, 681.8) | 866.0 | (807.7, 924.3) | <.001 |
| Total hospitalizationsq | 2.1 | (2.0, 2.1) | 1.9 | (1.8, 2.0) | 2.3 | (2.2, 2.4) | 1.8 | (1.7, 1.9) | 2.8 | (2.5, 3.2) | <.001 |
| 0 | 843 | 22.7% | 341 | 28.9% | 283 | 21.1% | 180 | 17.8% | 39 | 21.2% | <.001 |
| 1 | 1,020 | 27.4% | 299 | 25.4% | 324 | 24.2% | 363 | 35.8% | 34 | 18.5% | |
| 2 | 671 | 18.1% | 198 | 16.8% | 241 | 18.0% | 204 | 20.1% | 28 | 15.2% | |
| 3+ | 1,183 | 31.8% | 341 | 28.9% | 492 | 36.7% | 267 | 26.3% | 83 | 45.1% | |
| Total hospital days | 40.1 | (38.5, 41.7) | 25.4 | (23.2, 27.7) | 43.4 | (40.6, 46.2) | 52.6 | (49.5, 55.7) | 41.6 | (33.8, 49.3) | <.001 |
Note: ANOVA = analysis of variance; CI = confidence interval; HC = home care; LTC = long-term care; RC = residential care.
aBased on demographic and RAI assessment values closest to the start of LTC—baseline.
bCare patterns based on first and last service records.
cSignificance testing (p value) compares differences across all pattern groups using either chi square or one-way ANOVA, as appropriate.
dAge as of the start of initial long-term care service.
eReceipt of Guaranteed Income Supplement provided to older adults below minimum income threshold.
fBased on geocoded location of first three digits of residential postal code. For residential care clients, this should represent last known home address.
gClinical Assessment Protocol to represent risk of future falls.
hActivities of Daily Living based on ADL Self-Performance Hierarchy Scale; range 0 = independent to 6 = total dependence.
iCognitive Performance Scale; range 0 = intact to 6 = very severe impairment.
jDepression Rating Scale, range 0–14, with higher values indicating more numerous and/or frequent symptoms of depression.
kChanges in Health, End-Stage Disease and Signs and Symptoms (CHESS), range 0 = no instability to 5 = highest level of instability.
lPain scale, range 0 = no pain to 3 = severe daily pain.
mBased on chronic conditions common to both the home care and residential care assessment instruments, range 0–10.
nEvidence of either bladder and/or bowel incontinence.
oEvidence of minimum one item associated with Aggressive Behaviour Scale, including verbal abuse, physical abuse, inappropriate behavior, and resisting care.
pPrimary caregiver and informal care information is included on the RAI-HC instrument only. Clients without a home care assessment will be missing for these items.
qHospitalizations with a discharge date more than 365 days prior to the start of LTC have been excluded from the analysis of hospital variables.
Sources: Analysis utilized anonymized linked administrative data from long-term care clients in the Fraser Health Authority in British Columbia, Canada, including client demographic and service utilization records, Resident Assessment Instruments (inter-RAI) for Residential Care (RAI-MDS 2.0) and for Home/Community Care (RAI-HC), Canadian Versions, and Discharge Abstract Database (DAD) hospital discharge records. All clients received long-term care services between January 1, 2008 and December 31, 2011.
A comparison of the women making the HC > RC transition to those experiencing the other two common pathways (HC only or RC only), revealed both commonalities and differences. Although the majority of women were widowed, there was also a high proportion of married and living alone individuals. Geographically, although all groups lived predominantly in urban areas, HC > RC clients were more likely to be living in suburban areas compared to the other groups. The HC > RC transition group was situated between the other two groups in terms of most health measures: risk of falls (high), ADL dependency, cognitive performance, frailty, pain, chronic conditions, aggression, and mortality. Notably, the transitional group had higher levels of depression. Though primary caregiver data was limited, women making this transition were proportionally more likely to be supported by a spouse, consistent with their greater likelihood of being married. Adult children were most likely to not live with the care recipient. Hours of weekly informal care were highest among the HC > RC group. Finally, relative to formal service use, the HC > RC group spent a longer period of time in LTC (as clients of both HC and RC), and their total number of hospitalizations was also the greatest.
Table 2 reports on the HC > RC transitional group, comparing their characteristics at time of entry into HC and RC. At the time of RC admission, women were less likely to be married or living alone. They were also in poorer health based on ADL impairments, cognitive performance, incontinence, and aggression. Conversely, assessed depression, medical frailty, pain, chronic conditions, and falls risk were lower at RC entry. Finally, with regard to service use, older women with dementia in the transitional group experienced significantly fewer hospitalizations after RC admission. Accordingly, the number of days spent in hospital was considerably reduced reflecting the management of care within the RC facility rather than in the acute care setting.
Table 2.
Characteristicsa of Women With Dementia in Long-term Care Who Transition From Home Care to Residential Care in a Canadian Context (N = 759; 2008–2011)b
| Start of home care | Start of residential care | p Valuec | |||
|---|---|---|---|---|---|
| Characteristics | N/mean | Percentage/(CI) | N/mean | Percentage/CI | |
| Demographicd | |||||
| Age | 83.2 | (82.8, 83.7) | 84.4 | (83.9, 84.8) | <.001 |
| % 85 or older | 335 | 44.1% | 376 | 49.5% | <.001 |
| Married | 234 | 30.9% | 208 | 27.5% | <.001 |
| High school or higher | 341 | 46.4% | — | — | — |
| Low income (supplement) | 351 | 46.6% | — | — | — |
| Living alone | 300 | 39.5% | 177 | 24.0% | <.001 |
| Location of residence | |||||
| Rural | 122 | 16.1% | — | — | — |
| Suburban | 257 | 33.9% | — | — | — |
| Urban | 380 | 50.1% | — | — | — |
| Health | |||||
| Falls risk | <.001 | ||||
| Low | 404 | 53.2% | 595 | 78.4% | |
| Medium | 182 | 24.0% | 133 | 17.5% | |
| High | 173 | 22.8% | 31 | 4.1% | |
| ADL | 1.1 | (1.0, 1.2) | 2.5 | (2.3, 2.6) | <.001 |
| CPS | 2.3 | (2.2, 2.4) | 3.0 | (2.9, 3.1) | <.001 |
| Depression | 1.9 | (1.7, 2.1) | 1.3 | (1.2, 1.5) | <.001 |
| Medical frailty (CHESS score) | 1.4 | (1.3, 1.5) | 0.7 | (0.6, 0.7) | <.001 |
| PAIN | 1.0 | (0.9, 1.0) | 0.6 | (0.5, 0.6) | <.001 |
| Number of chronic conditions | 2.7 | (2.6, 2.8) | 2.5 | (2.4, 2.6) | <.001 |
| Incontinence | 262 | 34.6% | 353 | 46.5% | <.001 |
| Aggression | 142 | 18.7% | 322 | 42.4% | <.001 |
| Died within study period | 223 | 29.4% | |||
| Age at death | 86.4 | (85.4, 87.3) | |||
| Service use | |||||
| Days in HC/RC | 402.7 | (377.7, 427.6) | 545.0 | (518.0, 572.0) | |
| Hospitalizations in HC/RC | 1.2 | (1.1, 1.3) | 0.4 | (0.4, 0.5) | <.001 |
| Hospital days in HC/RC | 31.2 | (28.1, 34.2) | 3.5 | (2.6, 4.4) | <.001 |
Note: CI = confidence interval; HC = home care; LTC = long-term care.
aBased on demographic and RAI assessment values closest to the start of HC/RC.
bOnly includes women with at least one valid home care and residential care assessment (n = 759).
cSignificance testing (p value) compares differences between clients at start of HC and start of RC using paired t test.
dSee Table 1 for further notes on specific variable definitions.
eVariable was not measured on RAI assessments and only captured once (time invariant).
Personal Journeys
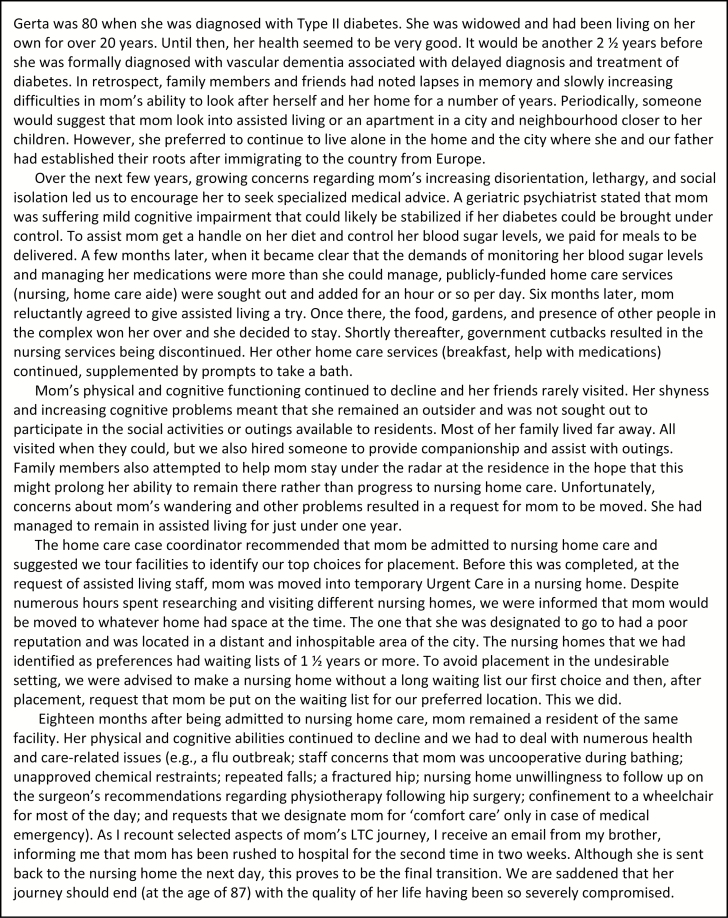
The narrative stories of our mothers (Sheila and Gerta) are presented in Figures 1 and 2, respectively, in simplified textual form. Consistent with our quantitative analyses, both Sheila and Gerta made the HC > RC transition, and each of them died while in RC. Both had unique biographical characteristics and experienced multiple transitions and relocations in their care trajectories.
Figure 1.
Sheila’s story.
Figure 2.
Gerta’s story.
In terms of social location, both similarities and differences were evident in their experiences. Sheila was initially married, and over the course of her LTC journey, became widowed, and then moved in with her sister before entering hospital and finally residential (nursing home) care. In contrast, Gerta was widowed and had lived alone for a long period of time prior to admission to home care, followed by assisted living and then residential care. Sheila had an average income, whereas Gerta had above-average income, and each of them lived in the suburban areas of larger urban centers. In addition, both were embedded in family support systems composed of proximate and distal caregivers—adult children for the most part, but also Sheila’s husband (Denise’s father), and her older sister at different points in time.
Our mothers’ stories underscore the influence of timing on lives and reflect heterogeneity and variability in their individual experience. The ages at which they were widowed, and the nature and timing of their diagnoses of dementia were further marks of difference. As their health declined, both increasingly relied on family members living inside or outside the household for assistance. The unique comorbid conditions of our mothers also had a large impact on their health and care trajectories over time. For example, Sheila’s health trajectory began with a history of hypertension, leading to a stroke that went undiagnosed for a period of time. Although her formal LTC journey was shaped more by diagnoses of Alzheimer’s and vascular dementia, these were amplified by a later diagnosis of lung cancer while she was undergoing testing in hospital. In contrast, Gerta suffered for an unknown period of time from Type II diabetes, also undiagnosed. Like Sheila, her formal LTC journey was initiated in relation to her diagnosis of vascular dementia.
Eventually, following sequences of formal and informal care and hospitalizations, and through formal service providers’ recommendations, both were admitted into residential care. In both cases, hospitalizations were an important feature of the care journey, albeit in somewhat different ways—acute, episodic care for Gerta, and a prolonged stay in acute care for Sheila before transitioning into an alternative level of care bed in hospital while she waited for placement in a residential care facility. Throughout their care trajectories, both of our mothers relied on both publicly and privately funded forms of mostly home-based care with paid companions and meal services being especially important sources of support and social engagement.
Over time, we witnessed the ways our mothers’ identity and autonomy were being altered within specific care contexts. A striking example of this was the characterization of our moms as uncooperative and “problematic” (aggressive) in the RC setting, which led to them being restricted from social activities. At the same time, their limited access to various medical and therapeutic forms of care (e.g., social stimulation, pain management, and ambulation devices) affected both quality of life and quality of care. Additionally, at many points along the care trajectory, family members experienced feelings of confusion and frustration with the information and communication between formal service providers and family members, challenging rather than promoting decision making.
Implications
This article set out to address two research questions: (a) How do our quantitative data map onto our mothers’ experiences? (b) What lessons do our mothers’ experiences convey about the care of older women with dementia? To address these questions, we drew on a life-course perspective that enabled us to reflect on the connections between our quantitative and qualitative data and our mothers’ experiences. Key concepts of the heterogeneity and variability of individual lives, timing and sequencing of health and care trajectories and service contexts, linked lives (family ties), and issues of agency and personal control were important for our moms and our families. Reflecting on these concepts, we explore the overall implications of our findings for policy and practice, theory development and future research.
Heterogeneity and Variability of Individual Lives
Our quantitative analyses highlighted the major pathways that older women with dementia take through the LTC system. HC > RC emerged as the most common trajectory and was also the trajectory experienced by our mothers. This transitional group is around 83 years of age on average, more likely to be widowed (60%) and more likely to be living alone (40%). From our personal narratives, our mom’s characteristics were not only broadly similar (HC > RC transition, widowhood, suburban residence) but also unique from each other in terms of their age and income status, living arrangements, and nature and types of comorbid conditions and LTC services used.
Health and Care Trajectories and Service Contexts
Both data sets paint a picture of increasing frailty on entry into residential care as measured by ADLs, cognitive performance, incontinence, and aggression. Falls risk, depression, medical frailty, and pain were lower at this time perhaps in part reflecting the timing of the RAI assessment after entry into care. In cases where assessment is delayed, chemical and physical restraint policies, and changing medication regimes postresidential care placement may reduce risk of falls, while the use of antipsychotics may alter mood and behavior (e.g., reducing depression), which would give the appearance of improved rates with entry.
Our mothers’ experiences also revealed the more complex, less linear nature of their pathways. Specifically, health trajectories were gradual at some points and sharper at other intervals. Both Sheila and Gerta became clients of LTC (HC), shortly after their diagnoses of dementia. Later on, Sheila spent a prolonged amount of time in hospital waiting for a residential care placement, whereas Gerta spent more time in the LTC system overall as someone who transitioned from HC to assisted living, and then RC. Both Sheila and Gerta also appeared to experience greater declines in physical and cognitive health after entering residential care:
…we had to deal with numerous health and care-related issues…; unapproved chemical restraints; repeated falls; a fractured hip; facility unwillingness to follow up on the surgeon’s recommendations regarding physiotherapy following surgery; confinement to a wheelchair for most of the day; and requests that we designate mom for ‘comfort care’ only in case of medical emergency). As I recount selected aspects of mom’s LTC journey, I receive an email from my brother, informing me that mom has been rushed to hospital for the second time in two weeks.…this proves to be the final transition. (Gerta’s story)
As family members and researchers, we were sensitized to the manner in which our mothers’ specific comorbid health conditions influenced their care journeys. Moreover, their conditions appeared to be amplified by associated contextual factors and events such as policies and procedures around falls and chemical and physical restraints that seemed to alter the nature and speed of the health and care trajectories of our moms in substantial ways. For Sheila, increasing medical frailty (vascular and Alzheimer type dementia and a lung cancer diagnosis at a younger age) appears to have accelerated her rate of decline in residential care. Her family noted, “We had little information about where she was at with her dementia and, with the added diagnosis of lung cancer, we felt overwhelmed when thinking about what her likely prognosis and journey would be given both of these conditions” (Sheila’s story). Although health status is commonly linked to heightened frailty and increased vulnerability to poor transitions, there is limited research on the specific ways that comorbidity interacts with other contextual factors to influence trajectories and quality of life (Chen, Chan, Kiely, Morris, & Mitchell, 2007; Kellett, Moyle, McAllister, King, & Gallagher, 2010; Moorhouse & Mallery, 2012; Sivananthan, 2015; Wysocki et al., 2014).
Reducing unnecessary transitions is a recognized solution supporting quality of life and minimizing the likelihood of negative health outcomes (Manderson et al., 2012). It is difficult to quantify whether our mothers experienced more care-related transitions than other women with dementia. Much depends on how we delineate exact transition points within the care journey (i.e., whether they are focused on health trajectories such as changing cognitive status, on moves from one form of care to another, or on significant life-course transitions such as the transition into widowhood). What we can say is that many of these facets are reflected in the quantitative data and explained more fully in qualitative studies that elaborate on the nuances of points of change. We also believe that virtually every transition in our mothers’ care journeys prompted a corresponding trickle-down effect in terms of care regimes, medications, restraints, social engagement, spirit, mood, identity, family responsibility, decision making, and ultimately quality of life. In the months before their deaths, these processes were experienced as destabilizing and often heartbreaking events for our moms and our families, on a seesaw between too little information on the one hand and too few care options on the other hand.
Hospitalization trends were a key part of the LTC journeys in both the quantitative and qualitative data. Our qualitative analyses highlighted the importance of the timing and duration of hospital care, not only sequentially in influencing whether and when transitions would occur from home to residential care, but also, as an influence on the nature of HC and RC experiences. Our mothers’ experiences reinforced our interest in exploring and understanding hospitalization patterns (when and how often they occur, how many days people spend in care) as a piece of the puzzle within LTC trajectories for women with dementia (Chen et al., 2007).
Our personal narratives confirmed that an exclusive focus on formal, publicly funded services provides only part of the complex story of individual care journeys through the LTC system. For both of our mothers, a reliance on paid companions was particularly notable, underscoring an important area of need within the continuum of care. To illustrate, when formal care is more task focused (e.g., baths, meals) than person centered (e.g., social activities), and when family members face challenges in care provision (related to geographic distance, inflexible jobs, or the competing demands of younger children), the quality of life of frail older adults may be substantively improved by the supportive services offered by paid companions.
Linked Lives
The quantitative data revealed that the hours of weekly care provided by family members was highest for this HC > RC transitional group, perhaps reflecting the progressive frailty of these care recipients, and their greater length of time in LTC. These data revealed high levels of reliance on spouses, and family members as caregivers, with adult children tending not to live with the care recipient.
A life-course perspective underscores the complicated nature of family roles and dynamics in the care of loved ones with dementia (McCabe et al., 2016; Phillipson, Jones, & Magee, 2014). Our personal data revealed family members’ concerns about the quality of care received, rather than the amount of care, focusing, for example, on how Sheila’s pain was not being effectively managed, influenced to some degree by the vastly different care philosophies of the two doctors responsible for her treatment. In hindsight, greater communication among formal care providers and family members about her potential “palliative status” after her entry into RC, may have resulted in different responses to her care (e.g., improved pain and symptom management is key emphasis within palliative approaches; Covinsky et al., 2003; Kane & West, 2005). Even telling family members that the pathways ahead will be rocky and unpredictable would be more helpful than silence or limited guidance, education, or instruction (Gitlin & Wolff, 2011). Though not without its own challenges, a palliative designation may have helped her family to better prepare for the future, rather than existing in a state of limbo between expecting the worst while hoping for the best. Ultimately, these crucial conversations are necessary and beneficial at multiple stages throughout the care journey in the interests of quality of care and quality of life (Bergum & Dossetor, 2005).
Witnessing our moms’ increasing frailty, our families were often caught between in situations characterized by equal parts vigilance and helplessness (Kane & West, 2005). For health care providers and decision makers, improved access to information about family circumstances (ranging from the size of the support network, proximity of caregivers, levels of expertise of secondary as well as primary caregivers, nature of relationships among family members, health of the spouse and other caregivers) and recognition of family roles may help to smooth out some of these rough edges and support better relationships and more effective care planning (Dilworth-Anderson et al., 2011). Despite their overall importance in characterizing broad patterns and aggregate trends, quantitative data cannot help as much with this level of understanding.
Agency and Personal Control
Tied to linked lives, issues of agency and personal control also emerged in the qualitative data regarding the care of older women with dementia. Common to our families’ experiences of the HC > RC trajectory was the shift in our moms’ identities from independent to highly dependent, frail people. Within families, this growing awareness of frailty, whether sharp or smooth, propels adult children headlong into the role of primary carers for their parents. In Gerta’s case, family tried to reinforce Gerta’s independence by enabling her to remain in her own home, and working actively to keep her in the assisted living facility for as long as possible. “Family members attempted to help mom stay under the radar at the residence in the hope that this might prolong her ability to remain there rather than progress to RC” (Gerta’s story). Thus, critical issues of personhood, identity, agency, and control were embedded in our moms’ experiences and reflected in our experiences as families as we struggled to “do what was right.” In hindsight, our academic experience as social gerontologists seemed to have little impact on the everyday challenges and experiences of our moms within the LTC system. And profoundly, through our personal experiences, we felt that we lost more faith than we gained, about how the system actually operates and functions.
Qualitatively, the relationship between identity and social engagement for women with dementia is also an important area for research. This relationship could be further theorized using a life-course perspective. For example, our personal narratives reflected how the broader care system (re)-identified our moms as problematic in terms of their behaviors (aggression and wandering) even though as family members, we knew our moms throughout their lives as shy and gentle women, who we believe would still have benefited from more social engagement rather than less. Over time, we watched them become stigmatized and more isolated by their newly acquired, negative residential care identities.
Although our academic backgrounds contributed to our knowledge and potential ability to navigate the formal LTC system, other factors were constraining. For example, living in different provinces from where our mothers were cared for reduced our knowledge of local service contexts and also relegated us (within both the family and service delivery environments) to the position of long-distance secondary, rather than primary caregivers. As a result, we were not necessarily included in day-to-day decision making with regard to our mothers’ care but were often engaged in short and intensive bursts of involvement in decision making and caring activities that afforded respite for other local family members when we were home (Lewis, 2008). As elder daughters, we had both contemplated moving our moms closer to us for care purposes, but the delicate state of their health at the point in their care trajectories where they may have been open to such a move, a lack of portability in provincial health care plans, dynamics linked to their current geographical residency, and concerns about relocation prevented this from being a real possibility. Both the quantitative and qualitative data emphasized an opportunity for further research in this area around the impact of “relocation” on frail individuals, particularly those with dementia (Cohen & Pushkar, 1999). Our personal experiences suggest that relocation, particularly into residential care influenced levels of anxiety, agitation, aggression, falls risk, and wandering behaviors for our moms, in tandem with the progression of their disease states. Keeping the most frail individuals where they are rather than subjecting them to multiple dislocations and relocations based on policy (e.g., first available bed criterion, pressures on limited bed supply) must be considered more fully from the standpoints of quality of life and quality of care. Such stability is supported by research that argues that “wandering” is not a random or purposeless behavior for persons with dementia but is a responsive behavior triggered by environmental and social factors (Sadowsky & Galvin, 2012). Ultimately, personhood and identity may be fostered through the establishment of stable and familiar environments, as well as by maintaining and promoting, rather than reducing social activities and contacts (Brooker, 2003).
Limitations
Several research limitations should be noted. Quantitatively, we had only 4 years of data with which to understand the experiences of women with dementia moving through the LTC system. Further, we had to restrict our sample to only those women who had valid RAI assessments at entry into both HC and RC, which reduced the final sample size. Although comparative analysis revealed few significant differences between those who had assessments and those who did not, this remains a concern for future analyses. Another challenge in using the RAI data was that some variables are defined differently in each of the two instruments (e.g., incontinence, chronic conditions). Consistency in how variables are measured and incorporation of comparable data on informal care providers such as the number and gender of adult children, their geographic proximity and ability to provide care, and their own health status and concerns, especially for spousal caregivers would be meaningful (Gaugler, 2005). Because health sector reforms will continue to put different pressures on family caregivers, understanding both their capacities and limitations will remain critically important (Dilworth-Anderson et al., 2011; McCabe et al., 2016).
We have already noted the importance of incorporating hospitalization trends into research on LTC service use trajectories, as are algorithms for linking quantitative data sets together for longitudinal analyses. Such information is beneficial to enhance our understanding service use trajectories and their causal patterns and predictors. This knowledge will also be meaningful for resource allocation decisions; local, national, and international comparisons; and in promoting the care of frail individuals under a philosophy of “continuous care” rather than discharge management (Butz & Torrey, 2006; Dilworth-Anderson et al., 2011).
Our personal narratives add critical dimension and depth to our quantitative analyses. Writing our mothers’ stories was challenging to say the least as we aimed for authenticity and representativeness, but we were challenged to illuminate such complexity in a concise and condensed format. We consulted with family members to assist with our recall of the timing and import of reported events; however, the interpretation of the stories is ours alone and likely reflects our particular viewpoints, biases, and emphases.
Finally, though a life-course perspective emphasizes the need to locate individual trajectories in a macrostructural and sociohistorical context, our analyses were necessarily confined to the micro-level. Extensive multilevel health sector restructuring initiatives in recent decades throughout Canada, are expected to continue to erode public-sector home care services and nursing home bed supply in ways that are unique and distinct from the United States, or other service contexts. To illustrate, in Canada, it is common for older persons to occupy more costly alternative care (ALC) beds or transitional beds in hospital while they await placement in a nursing home/residential care facility (Banerjee, 2007; Sivanthan, Doupe, & McGregor, 2015), a facet of Sheila’s experience. Similarly, the broader health service context influenced the range of available health care options for Gerta and Sheila, notably: reduced access to home nursing services; increased need for private pay services such as meals and companions; and reduced access to specialized dementia care units, assisted living and residential care facilities. Research should continue to examine individual diversity, linked lives and family dynamics, alongside these shifting social, historical, and organizational contexts (Dannefer, 2011; McDaniel & Bernard, 2011).
Conclusions
In this article, a life-course perspective was a highly relevant framework for helping us to organize, integrate, and synthesize the lessons learned from our quantitative and qualitative data. It also enriched our understanding of the diverse and complex transitions and trajectories experienced by women with dementia and their families. Allen, Griffiths, and Lyne (2004) caution that residents’ journeys and experience often reflect a series of false starts, blind alleys, and changes in direction. Notwithstanding our quantitative data that suggest a limited number of fairly clearly defined and predictable care trajectories, as families, we often experienced the system in this unpredictable and nonlinear way. Sadly, the wisdom of Kane and West in 2005 feels true to us today. More than a decade on, we have still not made substantial progress in the provision of person- and family-centered LTC. Ultimately, the individual person, and the family, still get lost in a cracked and broken system.
Finally, just as we began, we return once again to the metaphor of Janus, god of births and journeys, beginnings, and transitions. Janus has two faces: looking back into the past, it is evident that we have only a limited knowledge of the combination of services (community based and institutional, public and private, formal and informal) that people rely on as they navigate through the “continuum” of care (Karmel et al., 2012). Looking forwards, attending to the care needs of older women with dementia and other frail older adults compels an ongoing engagement with longitudinal quantitative and qualitative studies. A life-course perspective offers insights into the development and delivery of more inspired, compassionate, and continuous care for frail older persons with dementia and their families.
Funding
The BC Transitions in Care Study, 2012–2015, funded by the Canadian Institutes of Health Research (CIHR) and the BC Michael Smith Foundation for Health Research (MSFHR). The co-PIs are: M. J. Penning and D. S.
Conflict of Interest
No conflicts of interest.
Acknowledgments
The research on which some of this work was based was undertaken in partnership with the Fraser Health (FH) region, Province of British Columbia. Their support is gratefully acknowledged as is that provided by the seniors, family members, practitioners, and advocates who participated in the research. We also express our deep thanks and appreciation for the data tables generated by our project coordinator, Ms. Kim Nuernberger. The interpretations expressed herein are those of the authors and do not necessarily represent those of the FH or other participants.
References
- Allen D. Griffiths L., & Lyne P (2004). Understanding complex trajectories in health and social care provision. Sociology of Health and Illness, 26, 1008–1030. doi:10.1111/j.0141-9889.2004.00426.x [DOI] [PubMed] [Google Scholar]
- Alzheimer Society of Canada (2010). Rising tide: The impact of dementia on Canadian Society. Toronto, Ontario, Canada: Alzheimer Society of Canada; Retrieved from http://www.alzheimer.ca/~/media/Files/national/Advocacy/ASC_Rising_Tide_Full_Report_e.pdf (June 14, 2006) [Google Scholar]
- Banerjee A. (2007). An overview of long-term care in Canada and selected provinces and territories. Toronto, Ontario, Canada: Women and Health Care Reform Group, Health Canada; http://www.womenandhealthcarereform.ca/publications/banerjee_overviewLTC.pdf (accessed June 14, 2016). [Google Scholar]
- Bergum V., & Dossetor J (2005). Relational ethics: The full meaning of respect. Hagerstown, MD: University Publishing Group. [Google Scholar]
- Braun V., & Clarke V (2012). Thematic analysis. In Harris C. (Ed.), APA handbook of research methods in psychology: Research designs: Quantitative, qualitative, neuropsychological, and biological (Vol. 2, pp. 57–71). Washington, DC: American Psychological Association. doi:10.1037/13620-004 [Google Scholar]
- Boyatzis R. E. (1998). Transforming qualitative information: Thematic analysis and code development. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Brooker D. (2003). What is person-centred care in dementia? Reviews in Clinical Gerontology, 13, 215–222. doi:10.1017/S095925980400108X [Google Scholar]
- Butz W. P., & Torrey B. B (2006). Some frontiers in social science. Science, 312, 1898–1900. doi:10.1126/science.1130121 [DOI] [PubMed] [Google Scholar]
- Callahan C. M. Arling G. Tu W. Rosenman M. B. Counsell S. R. Stump T. E., & Hendrie H. C (2012). Transitions in care for older adults with and without dementia. Journal of the American Geriatrics Society, 60, 813–820. doi:10.1111/j.1532-5415.2012.03905.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J. H. Chan D. C. Kiely D. K. Morris J. N., & Mitchell S. L (2007). Terminal trajectories of functional decline in the long-term care setting. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 62, 531–536. doi:10.1093/gerona/62.5.531 [DOI] [PubMed] [Google Scholar]
- Cohen C. A., & Pushkar D (1999). Transitions in care: Lessons learned from a longitudinal study of dementia care. American Journal of Geriatric Psychiatry, 7, 139–146. doi:10.1097/00019442-199921720-00007 [PubMed] [Google Scholar]
- Coleman E. A., & Boult C (2003). Improving the quality of transitional care for persons with complex care needs. Journal of the American Geriatrics Society, 51, 556–557. doi:10.1046/j.1532-5415.2003.51186.x [DOI] [PubMed] [Google Scholar]
- Coleman E. A. Min S. Chomiak A., & Kramer A. M (2004). Post-hospital care transitions: Patterns, complications, and risk identification. Health Services Research, 39, 1449. doi:10.1111/j.1475-6773.2004.00298.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covinsky K. E. Eng C. Lui L. Sands L. P., & Yaffe K (2003). The last 2 years of life: Functional trajectories of frail older people. Journal of the American Geriatrics Society, 51, 492–498. doi:10.1046/j.1532-5415.2003.51157.x [DOI] [PubMed] [Google Scholar]
- Dannefer D. (2011). Age, the life course, and the sociological imagination: Prospects for theory. In Binstock R., George L. (Eds.), Handbook of aging and the social sciences (Chapter 1, pp. 3–16). New York: Academic Press. doi:10.1016/B978-0-12-380880-6.00001-0 [Google Scholar]
- Dilworth-Anderson P. Hilliard T. S. Williams S., & Palmer M. H (2011). A contextual conceptualization on transitions of care for older persons. Annual Review of Gerontology and Geriatrics, 31, 1–14. doi:10.1891/0198-8794.31.1 [Google Scholar]
- Elder G. H., Jr (1985). Life course dynamics: Trajectories and transitions: 1968–90. Ithaca, NY: Cornell University Press. [Google Scholar]
- Eska K. Graessel E. Donath C. Schwarzkopf L. Lauterberg J., & Holle R (2013). Predictors of institutionalization of dementia patients in mild and moderate stages: A 4-year prospective analysis. Dementia and Geriatric Cognitive Disorders, 3, 426–445. doi:10.1159/000355079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler J. (2005). Family Involvement in residential long-term care: A synthesis and critical review. Aging and Mental Health, 9, 105–118. doi:10.1080/13607860412331310245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler J. Kane R. L., & Kane R. A. Clay T., & Newcomer R. C (2005). The effects of duration of caregiving on institutionalization. The Gerontologist, 45, 78–89. doi:10.1093/geront/45.1.78 [DOI] [PubMed] [Google Scholar]
- Gitlin L. N., & Wolff J (2011). Family involvement in care transitions of older adults: What do we know and where do we go from here? Annual Review of Gerontology and Geriatrics, 31, 31–64. doi:10.1891/0198-8794.31.31 [Google Scholar]
- Hirdes J. P. Mitchell L. Maxwell C. J., & White N (2011). Beyond the ‘iron lungs of gerontology’: Using evidence to shape the future of nursing homes in Canada. Canadian Journal on Aging, 30, 371–390. doi:10.1017/S0714980811000304 [DOI] [PubMed] [Google Scholar]
- Kane R. L., & West J. C (2005). It shouldn’t be this way: The failure of long-term care. Nashville, TN: Vanderbilt University Press. [Google Scholar]
- Karmel R. Gibson D. Anderson P. Wells Y., & Duckett S (2012). Care trajectories through community and residential aged care services: Disease effects. Ageing and Society, 32, 1428–1445. doi:10.1017/S0144686X11001231 [Google Scholar]
- Kellett U. Moyle W. McAllister M. King C., & Gallagher F (2010). Life stories and biography: A means of connecting family and staff to people with dementia. Journal of Clinical Nursing, 19, 1707. doi:10.1111/j.1365-2702.2009.03116.x [DOI] [PubMed] [Google Scholar]
- Lewis L. (2008). Long-distance caregiving. American Journal of Nursing, 108(Suppl), 49. doi:10.1097/01.NAJ.0000336416.68119.a2 [DOI] [PubMed] [Google Scholar]
- Luppa M. Luck T. Weyerer S. König H.-H. Brähler E., & Riedel-Heller S. G (2010). Prediction of institutionalization in the elderly. A systematic review. Age and Ageing, 39, 31–38. doi:10.1093/ageing/afp202 [DOI] [PubMed] [Google Scholar]
- Manderson B. Mcmurray J. Piraino E., & Stolee P (2012). Navigation roles support chronically ill older adults through healthcare transitions: A systematic review of the literature. Health & Social Care in the Community, 20, 113–127. doi:10.1111/j.1365-2524.2011.01032.x [DOI] [PubMed] [Google Scholar]
- Mayer K. U. (2009). New directions in life course research. Annual Review of Sociology, 35, 413–433. doi:10.1146/annurev.soc.34.040507.134619 [Google Scholar]
- McCabe M. You E., & Tatangelo G (2016). Hearing their voice: A systematic review of dementia family caregivers’ needs. The Gerontologist, 56, e70–e88. doi:10.1093/geront/gnw078 [DOI] [PubMed] [Google Scholar]
- McDaniel S., & Bernard P (2011). Life course as a policy lens: Challenges and opportunities. Canadian Public Policy, 37(Special Issue), S1–S13. doi:10.1353/cpp.2011.0005 [Google Scholar]
- Menec V. H. Nowicki S. Blandford A., & Veselyuk D (2009). Hospitalizations at the end of life among long-term care residents. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 64, 395–402. doi:10.1093/gerona/gln034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon M. (2016). The unprepared caregiver. The Gerontologist. doi:10.1093/geront/gnw080 [DOI] [PubMed] [Google Scholar]
- Moorhouse P., & Mallery L. H (2012). Palliative and therapeutic harmonization: A model for appropriate decision-making in frail older adults. Journal of the American Geriatrics Society, 60, 2326–2332. doi:10.1111/j.1532-5415.2012.04210.x [DOI] [PubMed] [Google Scholar]
- Murtaugh C. M., & Litke A (2002). Transitions through postacute and long-term care settings: Patterns of use and outcomes for a national cohort of elders. Medical Care, 40, 227–236. doi:10.1097/00005650-200203000-00006 [DOI] [PubMed] [Google Scholar]
- Phillipson L. Jones S. C., & Magee C (2014). A review of the factors associated with the non-use of respite services by carers of people with dementia: Implications for policy and practice. Health and Social Care in the Community, 22, 1–12. doi:10.1111/hsc.12036 [DOI] [PubMed] [Google Scholar]
- Riessman C. K. (2008). Narrative methods for the human sciences. Los Angeles, CA: Sage Publications. [Google Scholar]
- Rosenthal C. J. Martin-Matthews A., & Keefe J. M (2007). Care management and care provision for older relatives amongst employed informal caregivers. Ageing and Society, 27, 755–778. doi:10.1017/s0144686x07005995 [Google Scholar]
- Sadowsky C. H., & Galvin J. E (2012). Guidelines for the management of cognitive and behavioral problems in dementia. Journal of the American Board of Family Medicine, 25, 350–366. doi:10.3122/jabfm.2012.03.100183 [DOI] [PubMed] [Google Scholar]
- Sivananthan S. N. (2015). Diagnosis and disruption: Understanding guideline-consistent dementia care and patterns of transitions experienced by individuals with dementia (PhD dissertation). Retrieved from University of British Columbia https://circle.ubc.ca/bitstream/handle/2429/52306/ubc_2015_may_sivananthan_saskia.pdf?sequence=4 [Google Scholar]
- Sivanthan S. N., Doupe M., , &, McGregor M. J. (2015). Exploring the ecology of Canada’s publicly funded residential long-term care bed supply. Canadian Journal on Aging, 34, 60–74. doi:10.1017/s071498081400052x [DOI] [PubMed] [Google Scholar]
- WHO. (2015). World Health Organization – World report on ageing and health (p. 260). Retrieved from http://www.who.int/ageing/events/world-report-2015-launch/en/ [Google Scholar]
- Wysocki A. Kane R. L. Dowd B. Golberstein E. Lum T., & Shippee T (2014). Hospitalization of elderly Medicaid long-term care users who transition from nursing homes. Journal of the American Geriatrics Society, 62, 71–78. doi:10.1111/jgs.12614 [DOI] [PubMed] [Google Scholar]