Abstract
Background
Microvascular complications of diabetes mellitus can cause retinopathy and maculopathy, which can irreversibly damage vision and lead to blindness. The prevalence of retinopathy is 9–16% in patients with type 2 diabetes and 24–27% in patients with type 1 diabetes. 0.2–0.5% of diabetics are blind.
Methods
The National Disease Management Guideline on the prevention and treatment of retinal complications in diabetes was updated according to recommendations developed by seven scientific medical societies and organizations and by patient representatives and then approved in a formal consensus process. These recommendations are based on international guidelines and systematic reviews of the literature.
Results
Regular ophthalmological examinations enable the detection of retinopathy in early, better treatable stages. The control intervals should be based on the individual risk profile: 2 years for low-risk patients and 1 year for others, or even shorter depending on the severity of retinopathy. General risk factors for retinopathy include the duration of diabetes, the degree of hyperglycemia, hypertension, and diabetic nephropathy. The general, individually adapted treatment strategies are aimed at improving the risk profile. The most important specifically ophthalmological treatment recommendations are for panretinal laser coagulation in proliferative diabetic retinopathy and, in case of clinically significant diabetic macular edema with foveal involvement, for the intravitreal application of medications (mainly, vascular endothelial growth factor [VEGF] inhibitors), if an improvement of vision with this treatment is thought to be possible.
Conclusion
Regular, risk-adapted ophthalmological examinations, with standardized documentation of the findings for communication between ophthalmologists and the patients’ treating primary care physicians/diabetologists, is essential for the prevention of diabetic retinal complications, and for their optimal treatment if they are already present.
Diabetic retinopathy and maculopathy are microvascular complications of diabetes that can permanently damage vision, potentially leading to blindness. In Germany, the age- and sex-standardized prevalence of diabetes among persons covered by statutory health insurance is nearly 10% (e1).
In German population-based health care studies, the prevalence of diabetic retinopathy has been found to be
Between 0.2% and 0.5% of diabetics are blind (3, 8). Many more have impaired vision because of diabetic retinopathy, although retinopathy does not cause subjective worsening of vision in every case. Any subjectively noticeable impairment of vision may be very significant to the patient. No data are available on the prevalence of impaired or worsened vision, and the available data on retinopathy and blindness can only be considered rough estimates, since all of the underlying studies have methodological limitations.
A National Disease Management Guideline (NDMG) on the prevention and treatment of retinal complications in diabetes was developed in the framework of the national disease management guidelines program of the German Medical Association (Bundesärztekammer, BÄK), the National Association of Statutory Health Insurance Physicians (Kassenärztlicher Bundesvereinigung, KBV), and the Association of the Scientific Medical Societies in Germany (Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften, AWMF), with the purposes of
improving the care of patients with impending or already existing retinal damage due to diabetes,
defining suitable evidence-based methods of prevention, diagnosis, and treatment, and
optimizing the flow of information among all physicians involved.
A further goal of the NDMG is to heighten diabetics’ awareness of their risk of retinal damage and to encourage them to have regular ophthalmological examinations. The second, comprehensively updated version of the NDMG will be in effect until the next update, or until the end of September 2020, whichever comes first.
Methods
NDMGs are created in accordance with the principles of the G-I-N (Guidelines International Network), the guideline assessment criteria of the BÄK and KBV (e2), the regulatory framework for guidelines of the AWMF (e3), and the German Guideline Assessment Instrument (Deutsches Leitlinienbewertungsinstrument, DELBI) (e4). The basic underlying method is described in a general method report (e5), and the specific method by which this guideline was created is described in the report on this particular NDMG (29).
The first version of this NDMG concerning the prevention and treatment of retinal complications in type 2 diabetes was issued in 2007 (e6). The creation of the second, updated version was organized by the German Agency for Quality in Medicine (Ärztliches Zentrum für Qualität in der Medizin, ÄZQ) and took place from November 2013 to September 2015. The guideline was created by a multidisciplinary group (ebox).
eBOX. Editors and authors of the National Disease Management Guideline on the prevention and treatment of retinal complications in diabetes.
Editors
German Medical Association (Bundesärztekammer, BÄK), Conference of German State Medical Associations (Arbeitsgemeinschaft der Deutschen Ärztekammern)
National Association of Statutory Health Insurance Physicians (Kassenärztliche Bundesvereinigung, KBV)
Association of Scientific Medical Societies in Germany (Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften, AWMF)
and
Drug Commission of the German Medical Association (Arzneimittelkommission der deutschen Ärzteschaft, AkdÄ)
German College of General Practitioners and Family Physicians (Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin, DEGAM)
German Diabetes Society (Deutsche Diabetes Gesellschaft, DDG)
German Society for Internal Medicine (Deutsche Gesellschaft für Innere Medizin, DGIM)
German Ophthalmological Society (Deutsche Ophthalmologische Gesellschaft, DOG)
Association of Diabetes Counseling and Training Professions in Germany (Verband der Diabetesberatungs- und Schulungsberufe in Deutschland, VDBD)
National Association of Self-Help Groups (Bundesarbeitsgemeinschaft Selbsthilfe e. V., BAG Selbsthilfe)
Authors of the second edition
Prof. Dr. med. Ulrich A. Müller (AkdÄ)
Dr. med. Til Uebel, Prof. Dr. med. Heinz Harald Abholz (DEGAM)
Prof. Dr. med. Rüdiger Landgraf, Prof. Dr. med. Hans-Peter Hammes (DDG)
Prof. Dr. med. Hans-Peter Hammes (DGIM)
Prof. Dr. med. Bernd Bertram, Prof. Dr. med. Hansjürgen Agostini, PD Dr. med. Klaus-Dieter Lemmen (DOG)
Dr. rer. medic. Nicola Haller (VDBD)
Hannelore Loskill (BAG Selbsthilfe) – patient representative
Methodological supervision and coordination
Dr. Susanne Schorr, Corinna Schaefer, Dr. med. Carmen Khan, Peggy Prien, Prof. Dr. rer. nat. Dr. med. Günter Ollenschläger (ÄZQ)
Prof. Dr. med. Ina Kopp, Dr. med. Monika Nothacker (AWMF)
ÄZQ, German Agency for Quality in Medicine (Ärztliches Zentrum für Qualität in der Medizin)
Conflicts of interest
The potential conflicts of interest of all participants were determined in a structured procedure specified by the AWMF and published in the guideline report (29). These potential conflicts of interest were openly discussed, and it was not felt that any of the participants needed to be excluded.
Search strategy
In accordance with the basic general procedures of the NDMG program (e5), the guideline-developing group decided to make use of existing evidence-based guidelines from Germany and abroad as the evidence base for this guideline. To identify such guidelines, a search was carried out in the Medline database (via PubMed) and in multiprofessional and mono-disciplinary guideline databases of different guideline providers. Pertinent guidelines were assessed with domains 3 and 6 of the DELBI (e4). Guidelines with a standardized domain value greater than 0.33 were considered in the consensus process. The search strategies, an overview of the process of guideline screening, and the DELBI evaluation are all discussed in the guideline report (9).
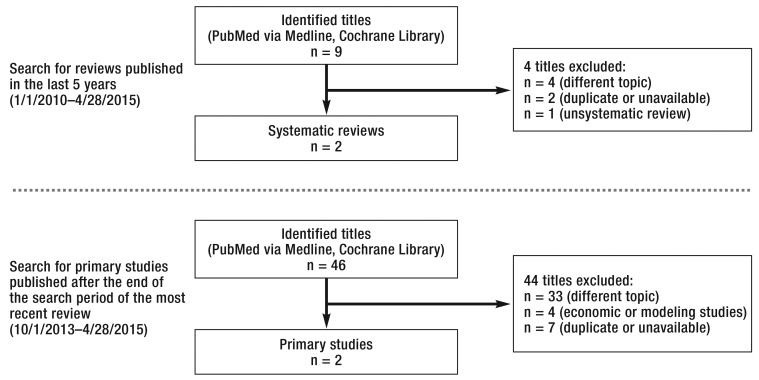
Moreover, systematic searches were carried out for aggregated evidence and primary studies on the topics of optical coherence tomography (OCT), intervals between examinations, and special ophthalmological treatments. A three-step procedure was used to search for studies on intervals between examinations (efigure 3). In the first step, relevant information from the identified guidelines was summarized; in the second step, a search was carried out in Medline (via PubMed) and in the Cochrane Library for systematic reviews; in the third step, the same search strategy was used to find primary studies published after the end of the search period of the most recent, relevant systematic review. All hits were inspected in a two-step procedure, and the identified studies were summarized and assessed in evidence tables. These steps were all carried out by the ÄZQ. Search strategies, an overview of the screening of retrieved literature, and the evidence tables have all been published in the guideline report (29). Further selective literature searches were performed on the epidemiology of retinal complications and the general risk factors for them.
eFigure 3.
Search strategy for studies on the interval between ophthalmological examinations
Evidence levels and recommendation grades
The evidence underlying the recommendations in the guideline was graded according to the scheme of the Scottish Intercollegiate Guidelines Network (e7). The grading of the recommendations themselves was loosely based on the GRADE procedure (Grading of Recommendations, Assessment, Development and Evaluation) (e8, e9). Two arrows indicate a strong recommendation, a single arrow indicates a weak recommendation, and a double arrow with arrowheads pointing in both directions indicates an open recommendation. Recommendation grades were assigned in consideration of the strength of the underlying evidence, ethical obligations, the clinical relevance of the effect strengths indicated by the studies, the applicability of the study findings to the target group of patients, patient preferences, and the implementability of the recommendations in everyday clinical practice given the existing care structures in Germany.
Formal consensus procedure
In a formal procedure to reach a consensus on the recommendations, consensus conferences took place in which nominal group processes were carried out (e10– e12) under the moderation of the AWMF and the ÄZQ. Of the 32 recommendations, 31 were issued with a strong consensus. The remaining recommendation was issued with 75% agreement and a particular objection from the scientific medical society that voted against it (29). The most important recommendations are reported and explained in the text of this article in the Results section, below. Further recommendations are listed in Table 1.
Table 1. Summary of important recommendations.
| No. | Recommendation | GoR | Consensus (source) |
| Symptoms and risk factors | |||
| 2–1 | The patient should have regular ophthalmological examinations, because:
|
↑↑ | expert consensus |
| 2–2 | The following are warning signs of retinal complications:
|
statement | expert consensus |
| 2–3 | Important general risk factors for the appearance or progression of diabetic retinopathy and/or maculopathy are:
|
statement | expert consensus (9– 15) |
| Clinical examination and general treatment strategies | |||
| 3–2 | On referral to the ophthalmologist, the patient should be told not to drive a motor vehicle for a few hours after the ophthalmological examination because the pupils must be dilated as part of the procedure. | ↑↑ | expert consensus |
| 3–3 | The ophthalmological examination for the detection of retinopathy and/or maculopathy and the determination of its severity should include the following:
|
↑↑ | expert consensus |
| 3–4 | The intraocular pressure should be measured in patients with advanced retinopathy. In certain clinical situations, fluorescein angiography is indicated. |
↑↑ | expert consensus (16, 17) |
| Interval between ophthalmological examinations | |||
| 4–1 | The regular ophthalmological examination of diabetics enables the early diagnosis of pathological changes so that the patient‘s treatment can be adjusted as needed and any indicated ophthalmological treatments can be provided. | statement | expert consensus |
| 4–2 | Ophthalmological screening should be performed
|
↑↑ | |
| 4–6 | Patients should be seen promptly by an ophthalmologist if they develop any of the following new symptoms:
|
↑↑ | expert consensus |
| Treatment by the primary care physician/diabetologist | |||
| 5–2 | The patient should be told that the presence of retinopathy is not a contraindication for cardioprotective ASA treatment, as the latter does not elevate the risk of retinal hemorrhage. | ↑ | expert consensus (18– 20) |
| 5–7 | If both focal and panretinal laser coagulation are indicated in a patient with combined proliferative diabetic retinopathy and diabetic macular edema without foveal involvement, the maculopathy should be treated first. | ↑ | expert consensus |
| Severe complications of proliferative diabetic retinopathy | |||
| 5–8 | Vitrectomy should be offered to patients who have a non-resorbing vitreal hemorrhage or a present or impending central traction retinal detachment. | ↑↑ | expert consensus (21– 23) |
| Treatment of clinically significant diabetic macular edema | |||
| …without foveal involvement | |||
| 5–9 | Focal laser coagulation can be offered to patients with clinically significant diabetic macular edema that spares the fovea but threatens to impair visual acuity. | ↔ | (24– 27) |
| … with foveal involvement | |||
| 5–11 | Intravitreal steroid therapy can be offered to patients with an inadequate or absent response to intravitreal therapy with VEGF inhibitors. | ↔ | expert consensus (28) |
| Provision of magnifying visual aids | |||
| 5–14 | Patients who lose the ability to read despite best refractive correction and whose blood glucose levels and ophthalmological findings are stable should be offered magnifying visual aids (either optical or electronic). | ↑ | expert consensus |
Recommendations are numbered as in the guideline. ↑↑ strong recommendation, ↑ weak recommendation, ↔ open recommendation.
ASA, acetylsalicylic acid; GoR, grade of recommendation; PDR, proliferative diabetic retinopathy; VEGF, vascular endothelial growth factor
External review
In July 2015, a draft of the guideline was made available on a publicly accessible website (www.versorgungsleitlinien.de) so that comments could be made on it. The start of this external evaluation process was announced in a statement to the press. The assembled comments were considered anonymously. These comments and the resulting decisions and changes are documented in the guideline report (29).
Results
Ophthalmological examinations and general treatment strategies
The goal of screening for diabetic retinal changes and treating them is essentially to limit or prevent subjectively noticeable visual loss. Regular examinations should make it possible to detect retinal complications of diabetes in an early, often asymptomatic stage. Nonetheless, screening for diabetic retinal changes, like all types of screening for the early detection of disease, carries with it a risk of overtreatment, i.e., the treatment of patients whose abnormal ophthalmological findings would never have led to any relevant visual impairment. This fact should be disclosed to patients both in medical consultations and in diabetes training.
The ophthalmological examination is intended to detect diabetic retinopathy and determine its severity. It involves measurement of visual acuity, split-lamp microscopy, and ophthalmoscopy with dilated pupils (30).
Patients with advanced retinopathy may need further tests such as intraocular pressure measurement or fluorescein angiography. Optical coherence tomography (OCT) can be used to diagnose central, clinically relevant macular edema with 78% sensitivity (95% confidence interval [CI]: [72%; 83%]) and 86% specificity (95% CI: [76%; 93%]) (16). The guideline therefore contains an open recommendation for OCT for the differential-diagnostic assessment of maculopathy potentially requiring treatment. However, OCT should always be used to establish the indication for intravitreal drug administration and to monitor the response to such treatment, as OCT was used for this purpose in all of the pertinent drug-approval studies.
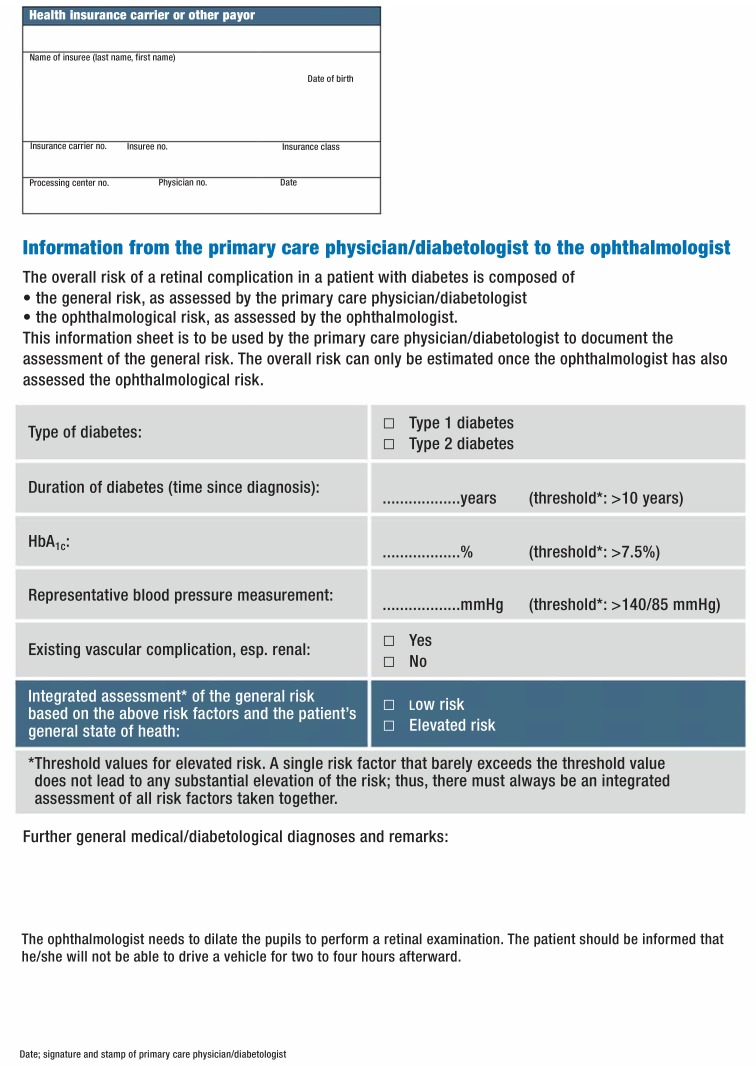
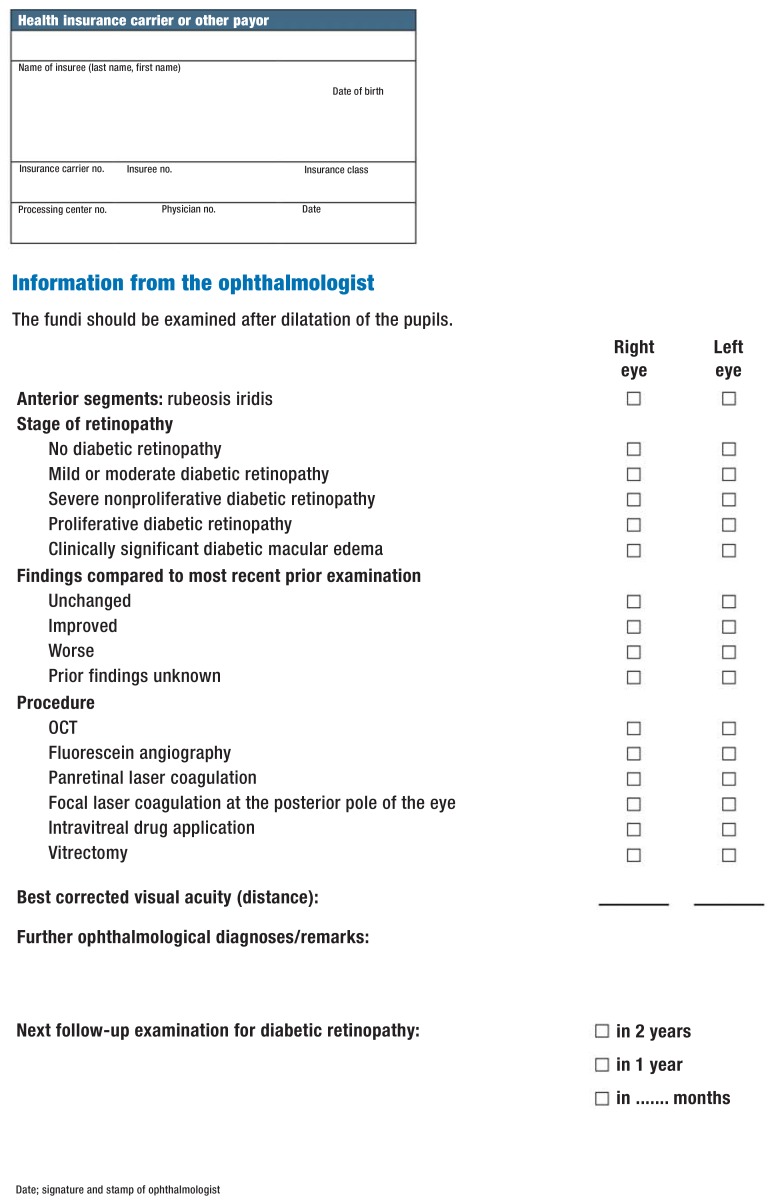
The communication and transmission of findings among primary care physicians/diabetologists and ophthalmologists need to be improved. To this end the authors of the guideline recommend the use of the structured documentation forms developed specifically in the framework of this NDMG (eFigures 1, 2).
eFigure 1.
Documentation form for communication from the primary care physician/diabetologist to the ophthalmologist
The interval between examinations
The patient may have diabetic retinal complications even before receiving the diagnosis of diabetes. Therefore, the international guidelines that were identified and evaluated as methodologically sound all contain a recommendation for an ophthalmological examination as soon as possible after type 2 diabetes is diagnosed (e13– e19). Patients with overt retinopathy should have further examinations at intervals of one year or less (e13– e19). As for the interval between examinations in diabetics without retinopathy, some guidelines recommend examinations once a year (e17, e20) or every two years (e18, e19), while others recommend adjusting the interval to the individual risk (e13– e16).
A systematic literature search revealed no randomized, controlled, prospective trials on the benefits and harms of different intervals between ophthalmological examinations. The best available evidence is derived from two systematic reviews of observational and modeling studies (31, 32) and two subsequently published observational studies (33, 34).
These studies are of limited informational value for the development of recommendations on intervals between examinations because they were characterized by a wide diversity of intervals, examination techniques, and indications for treatment and referral—and because they also differed in these important respects from the system of ophthalmological care in Germany. These studies also have a risk of bias because of drop-outs in the screening groups.
Because of these considerations, the authors of the guidelines recommend that the primary care physician/diabetologist should base the determination of the patient‘s so-called general risk on the following risk factors, as well as on the patient’s overall state of health:
Type of diabetes
Duration of diabetes
Nephropathy
HbA1c value
Hypertension.
The patient‘s general risk status is then documented on a form specially developed for this guideline (efigure 1) to facilitate communication among primary care physicians/diabetologists and ophthalmologists.
In addition to the general risk, each patient has an individual ophthalmological risk that is assessed on the basis of the previous fundoscopic findings, above all any pre-existing retinopathy or maculopathy and their degree of severity. Both of these types of risk are components of the general risk that determines whether the patient should be re-examined by an ophthalmologist once a year (or more often) or once every two years (table 2).
Table 2. The interval between ophthalmological examinations.
| General risk | Ophthalmological risk | Interval | |
| Low general risk | low | no | 2 years |
| Other risk constellations | high | no | 1 year |
| Unknown general risk | unknown | no | 1 year |
| Diabetic retinal changes | yes | 1 year or less | |
| Diagnosis of type 2 diabetes after the age of 10, or 5 years after the onset of type 1 diabetes | short-term | ||
| Visual worsening, distorted vision, blurry vision, spots before the eyes | short-term | ||
Treatment
Medical treatment by the primary care physician or diabetologist
The primary care physician or the diabetologist is responsible for the treatment of risk factors for retinal complications, including diabetes, arterial hypertension, and renal disease. It was concluded in a recent review that intense antihyperglycemic therapy in patients with type 2 diabetes leads to an approximately 3% absolute reduction of the risk of retinopathy. Intensified antihyperglycemic therapy (e21) was associated with a higher risk of hypoglycemia. Patients with high HbA1c values stand to benefit more from such therapy; for patients with low HbA1c values, whose risk of diabetic complications is significantly lower, the benefits and risks of treatment intensification must be jointly discussed by the patient and the physician. The effect of intensified treatment of either diabetes or hypertension on retinal complications is but one of many factors (some of them still inadequately defined) to be considered in weighing its benefits against its risks. More information on this topic can be found in the evidence-based guidelines on the individualized treatment of diabetes and its complications (www.diabetes.versorgungsleitlinien.de, www.awmf.org/leitlinien/detail/ll/057–013.html).
Special ophthalmological treatment
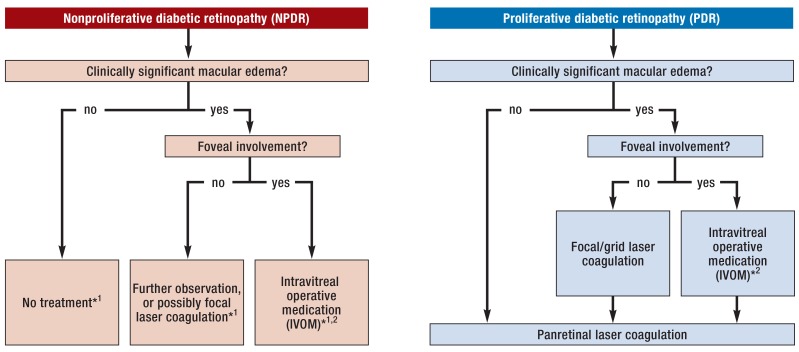
The ophthalmologist is responsible for appropriate diagnostic evaluation and treatment corresponding to the patient’s stage of disease, and for monitoring the course of diabetic retinopathy and/or maculopathy. The treatment options for diabetic retinal complications include laser therapy and intravitreal operative medication (IVOM). The most important considerations for the choice of treatment are the distinction between proliferative and nonproliferative retinopathy and the presence or absence of clinically significant macular edema, with or without foveal involvement (figure).
Figure.
Treatment options for diabetic retinopathy and maculopathy
*1 in advanced nonproliferative retinopathy, panretinal laser coagulation may be useful
*2 possibly, focal laser coagulation in addition or as an alternative
For the comparison of laser treatment versus no treatment or delayed treatment, the literature search revealed a review article (35) that was based, in particular, on the ETDR study (24). No improvement was found in the primary endpoint, moderate worsening of vision (relative risk [RR] 0.99 [0.89; 1.11]), but there was a marked, statistically significant reduction of the risk of severe worsening of vision (RR 0.46 [0.24; 0.86]), progression of diabetic retinopathy (RR 0.49 [0.37; 0.64]), and vitreal hemorrhage (RR: 0.56 [0.37; 0.85]) (35). A differential analysis of proliferative and nonproliferative diabetic retinopathy (PDR and NPDR) was not possible because of the mixed populations in the studies that were included in the analysis. The authors of the review estimate that, in one year, ten of 1000 untreated patients with moderate or severe NPDR will suffer a severe worsening of vision, and that laser coagulation reduces this number to five (95% CI [2; 9], number needed to treat [NNT] 200). For patients with PDR, they estimate that 50 of 1000 untreated patients will suffer severe worsening of vision in one year, and that laser coagulation reduces this number to 23 (95% CI [12; 43], NNT 37) (35). In view of its risk–benefit profile, laser therapy is unrestrictedly recommended only for patients with PDR. Panretinal laser coagulation can, however, be considered for certain patients with severe NPDR who are at high risk.
Foveal involvement is the key factor determining the proper mode of treatment for clinically significant macular edema (figure). Focal laser therapy is an option if there is no foveal damage, particularly if the patient still has good vision (27). Two review articles were identified in which IVOM with vascular endothelial growth factor (VEGF) inhibitors was compared to laser therapy or placebo for the treatment of clinically significant macular edema with foveal involvement. These studies showed the superiority of VEGF inhibitor treatment to placebo with respect to the number of patients who sustained either a moderate improvement or a moderate worsening of vision (28, 36). The NNT for moderate improvement of vision with VEGF inhibitor treatment, compared to laser treatment alone, was five (RR 3.6 [2.7; 4.8]), while that for the avoidance of moderate worsening of vision was ten (RR 0.11 [0.05; 0.24]) (36). Depending on the specific findings and individual risk–benefit considerations, IVOM may be necessary at once, or a period of further observation may be indicated. The authors of the guideline therefore issued a weak recommendation for the administration of VEGF inhibitors if the morphology of the macular findings suggests that such treatment will improve vision. Nonetheless, the German College of General Practitioners and Family Physicians (Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin, DEGAM) disagreed and preferred to restrict this recommendation to patients with current, subjectively symptomatic loss of vision. IVOM should be terminated when no benefit for vision is to be expected (37, 38). If IVOM is not indicated or cannot be performed, laser therapy can be offered instead, despite its low benefit (39, 40).
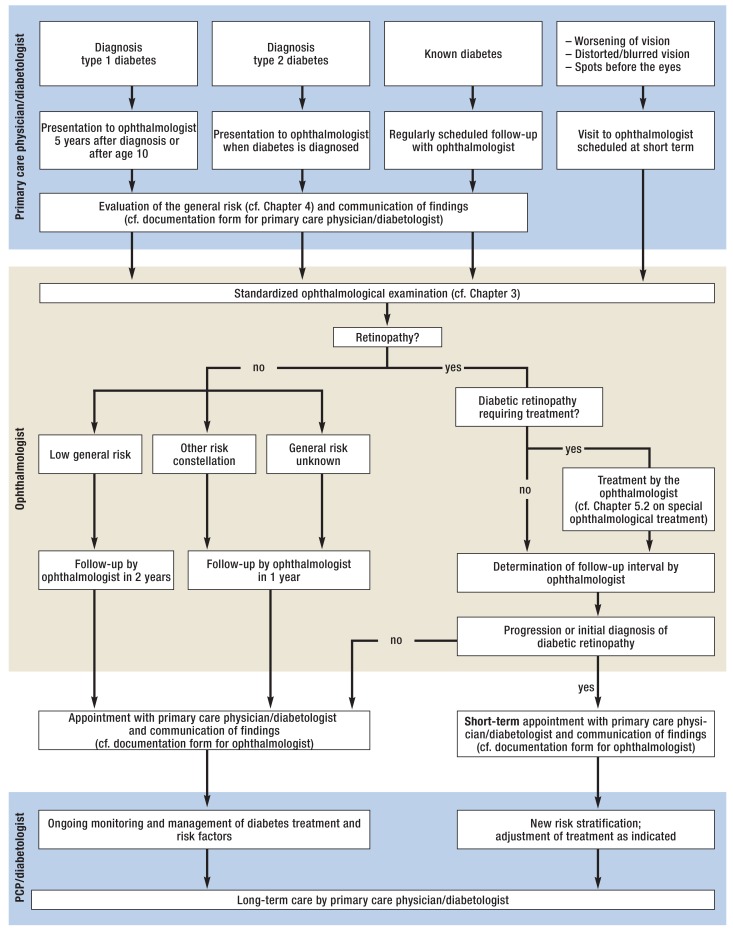
The coordination of care
The treating primary care physicians/diabetologists are responsible for coordinating the treatment of their diabetic patients (efigure 4). Ophthalmologists are involved in the treatment of diabetics by providing regular ophthalmological examinations to detect potential retinal damage. Furthermore, they perform ophthalmological examinations as soon as any visual complication arises; whenever necessary (as determined by the ophthalmologists) for closer monitoring; or for ophthalmological treatments or follow-ups after treatment.
eFigure 4.
Care coordination flowchart. The chapter references are to the corresponding chapters in the long version of the National Disease Management Guideline.
PCP, primary care physician
The primary care physician/diabetologist also bears the primary responsibility for ensuring that regular ophthalmological examinations are actually performed, particularly in their patients who do not (yet) have diabetic retinopathy.
Key Messages.
All diabetics should undergo ophthalmological screening, because diabetic retinal changes can cause significant loss of vision.
In patients who do not have diabebetic retinopathy, the interval between ophthalmological examinations should be set according to the individual risk profile (2 years for low-risk patients, otherwise 1 year).
The ophthalmological examination includes measurement of visual acuity, split-lamp microscopy, ophthalmoscopy with dilated pupils, and further tests in certain situations.
Diabetic retinal changes should be monitored and treated by an ophthalmologist as appropriate for their stage and according to the proper indications.
Standardized documentation forms should be used for communication between the primary care physician/diabetologist and the ophthalmologist.
eFigure 2.
Documentation form for communications from the ophthalmologist
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
Prof. Hammes has served as a paid consultant for Bayer and Boehringer Ingelheim and has received lecture honoraria and reimbursement of travel expenses from Bayer and Novartis. He has received financial support for research (third-party funding) from Boehringer Ingelheim and Sanofi.
Prof. Müller has received financial support for research (third-party funding) from Novo Nordisk, Haemopharm, Abbott, and Pfizer.
Prof. Landgraf has received consultant‘s fees or lecture honoraria from Lilly Deutschland, MSD, Novo Nordisk Pharma, and Roche Diagnostics.
The other authors state that they have no conflicts of interest.
References
- 1.Hagen B, Altenhofen L, et al. DMP. Düsseldorf: 2014. Nordrheinische Gemeinsame Einrichtung Disease-Management-Programme Qualitätssicherungsbericht 2013. Disease-Management-Programme in Nordrhein. Brustkrebs, Diabetes mellitus Typ 1/Typ 2, Koronare Herzkrankheit, Asthma/COPD Nordrheinische Gemeinsame Einrichtung. [Google Scholar]
- 2.Hesse L, Grusser M, Hoffstadt K, Jorgens V, Hartmann P, Kroll P. Population-based study of diabetic retinopathy in Wolfsburg. Ophthalmologe. 2001;98:1065–1068. doi: 10.1007/s003470170026. [DOI] [PubMed] [Google Scholar]
- 3.Blum M, Kloos C, Müller N, et al. Prevalence of diabetic retinopathy Check-up program of a public health insurance company in Germany 2002-2004. Ophthalmologe. 2007;104:499–500. 502–504. doi: 10.1007/s00347-007-1522-0. [DOI] [PubMed] [Google Scholar]
- 4.Icks A, Rathmann W, Haastert B, et al. Quality of care and extent of complications in a population-based sample of patients with type 2 diabetes mellitus The KORA Survey 2000. Dtsch Med Wochenschr. 2006;131:73–78. doi: 10.1055/s-2006-924927. [DOI] [PubMed] [Google Scholar]
- 5.Huppertz E, Pieper L, Klotsche J, et al. Diabetes mellitus in German primary care: quality of glycaemic control and subpopulations not well controlled—results of the DETECT study. Exp Clin Endocrinol Diabetes. 2009;117:6–14. doi: 10.1055/s-2008-1073127. [DOI] [PubMed] [Google Scholar]
- 6.Böhler S, Pittrow D, Pieper L, et al. Diabetes mellitus in der primärärztlichen Versorgung: Häufigkeit von mikro- und makrovaskulären Komplikationen - Ergebnisse der DETECT Studie 41 Jahrestagung der Deutschen Diabetes-Gesellschaft. Diabet Stoffw. 2006;1 (S1):A1–A315. [Google Scholar]
- 7.Hammes HP, Kerner W, Hofer S, Kordonouri O, Raile K, Holl RW. Diabetic retinopathy in type 1 diabetes-a contemporary analysis of 8,784 patients. Diabetologia. 2011;54:1977–1984. doi: 10.1007/s00125-011-2198-1. [DOI] [PubMed] [Google Scholar]
- 8.Nordrheinische Gemeinsame Einrichtung Disease-Management-Programme. Nordrheinische Gemeinsame Einrichtung DMP. Düsseldorf; 2008. Qualitätssicherungsbericht 2007. Disease Management Programme in Nordrhein. Brustkrebs, Diabetes mellitus Typ 1 / Typ 2, Koronare Herzkrankheit, Asthma / COPD. [Google Scholar]
- 9.Yau JW, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–564. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bundesärztekammer (BÄK) Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF), Kassenärztliche Bundesvereinigung (KBV) Nationale VersorgungsLeitlinie Therapie des Typ-2-Diabetes - Langfassung, 1. Edition. Version 3. http://doi.org/10.6101/AZQ/000203 (last accessed on 5 June 2014) [Google Scholar]
- 11.Bundesärztekammer (BÄK) Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF), Kassenärztliche Bundesvereinigung (KBV) Nationale VersorgungsLeitlinie Nierenerkrankungen bei Diabetes im Erwachsenenalter - Langfassung, 1. Auflage, Version 5. http://doi.org/10.6101/AZQ/000126 (last accessed on 22 June 2015) [Google Scholar]
- 12.Girach A, Vignati L. Diabetic microvascular complications—can the presence of one predict the development of another? J Diabetes Complications. 2006;20:228–237. doi: 10.1016/j.jdiacomp.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 13.DCCT Research Group. Effect of pregnancy on microvascular complications in the diabetes control and complications trial The Diabetes Control and Complications Trial Research Group. Diabetes Care. 2000;23:1084–1091. doi: 10.2337/diacare.23.8.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaaja R, Loukovaara S. Progression of retinopathy in type 1 diabetic women during pregnancy. Curr Diabetes Rev. 2007;3:85–93. doi: 10.2174/157339907780598252. [DOI] [PubMed] [Google Scholar]
- 15.Rasmussen KL, Laugesen CS, Ringholm L, Vestgaard M, Damm P, Mathiesen ER. Progression of diabetic retinopathy during pregnancy in women with type 2 diabetes. Diabetologia. 2010;53:1076–1083. doi: 10.1007/s00125-010-1697-9. [DOI] [PubMed] [Google Scholar]
- 16.Virgili G, Menchini F, Casazza G, et al. Optical coherence tomography (OCT) for detection of macular oedema in patients with diabetic retinopathy. Cochrane Database Syst Rev. 2015;1 doi: 10.1002/14651858.CD008081.pub3. CD008081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Early Treatment Diabetic Retinopathy Study Research Group (ETDRS) Focal photocoagulation treatment of diabetic macular edema. Relationship of treatment effect to fluorescein angiographic and other retinal characteristics at baseline: ETDRS report no. 19. Early Treatment Diabetic Retinopathy Study Research Group. Arch Ophthalmol. 1995;113:1144–1155. [PubMed] [Google Scholar]
- 18.Bergerhoff K, Clar C, Richter B. Aspirin in diabetic retinopathy A systematic review. Endocrinol Metab Clin North Am. 2002;31:779–793. doi: 10.1016/s0889-8529(02)00017-8. [DOI] [PubMed] [Google Scholar]
- 19.American Diabetes Association (ADA) Standards of medical care in diabetes 2014. Diabetes Care. 2014;37:S14–S80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 20.Advani A, Altomare F, Stockl F Canadian Diabetes Association (CDA) Retinopathy - clinical practice guidelines 2013. Can J Diabetes. 2013;37:S137–S141. doi: 10.1016/j.jcjd.2013.01.038. [DOI] [PubMed] [Google Scholar]
- 21.Diabetic Retinopathy Vitrectomy Study Research Group Early vitrectomy for severe vitreous hemorrhage in diabetic retinopathy. Four-year results of a randomized trial: Diabetic Retinopathy Vitrectomy Study Report 5. Arch Ophthalmol. 1990;108:958–964. doi: 10.1001/archopht.1990.01070090060040. [DOI] [PubMed] [Google Scholar]
- 22.Helbig H, Kellner U, Bornfeld N, Foerster MH. Vitrektomie bei diabetischer Retinopathie: Ergebnisse, Risikofaktoren, Komplikationen. Klin Monatsbl Augenheilkd. 1998;212:339–342. [PubMed] [Google Scholar]
- 23.Ostri C. Intraocular surgery in a large diabetes patient population: risk factors and surgical results. Acta Ophthalmol Thesis1. 2014;92:1–13. doi: 10.1111/aos.12364. [DOI] [PubMed] [Google Scholar]
- 24.Early Treatment Diabetic Retinopathy Study Research Group (ETDRS) Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98:766–85. [PubMed] [Google Scholar]
- 25.Early Treatment Diabetic Retinopathy Study Research Group (ETDRS) Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy study report number 2. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1987;94:761–774. doi: 10.1016/s0161-6420(87)33527-4. [DOI] [PubMed] [Google Scholar]
- 26.Early Treatment Diabetic Retinopathy Study Research Group (ETDRS) Techniques for scatter and local photocoagulation treatment of diabetic retinopathy: Early Treatment Diabetic Retinopathy study report no. 3. The Early Treatment Diabetic Retinopathy Study Research Group. Int Ophthalmol Clin. 1987;27:254–64. doi: 10.1097/00004397-198702740-00005. [DOI] [PubMed] [Google Scholar]
- 27.Mohamed QA, Ross A, Chu CJ. Diabetic retinopathy (treatment) BMJ Clin Evid 2011 2011. 0702. [PMC free article] [PubMed] [Google Scholar]
- 28.Ford JA, Lois N, Royle P, Clar C, Shyangdan D, Waugh N. Current treatments in diabetic macular oedema: systematic review and meta-analysis. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2012-002269. e002269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bundesärztekammer (BÄK) Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF), Kassenärztliche Bundesvereinigung (KBV) Nationale VersorgungsLeitlinie Prävention und Therapie von Netzhautkomplikationen bei Diabetes - Leitlinien-Report, Version 2. http://doi.org/10.6101/AZQ/000263 (last accessed on 18 November 2015) (2) [Google Scholar]
- 30.Aiello LP, Gardner TW, King GL, et al. Diabetic retinopathy. Diabetes Care. 1998;21:143–156. doi: 10.2337/diacare.21.1.143. [DOI] [PubMed] [Google Scholar]
- 31.Echouffo-Tcheugui JB, Ali MK, Roglic G, Hayward RA, Narayan KM. Screening intervals for diabetic retinopathy and incidence of visual loss: a systematic review. Diabet Med. 2013;30:1272–1292. doi: 10.1111/dme.12274. [DOI] [PubMed] [Google Scholar]
- 32.Taylor-Phillips S, Mistry H, Leslie R, et al. Extending the diabetic retinopathy screening interval beyond 1 year: systematic review. Br J Ophthalmol. 2001;100:105–114. doi: 10.1136/bjophthalmol-2014-305938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leese GP, Stratton IM, Land M, et al. Progression of diabetes retinal status within community screening programs and potential implications for screening intervals. Diabetes Care. 2015;38:488–494. doi: 10.2337/dc14-1778. [DOI] [PubMed] [Google Scholar]
- 34.Porta M, Maurino M, Severini S, et al. Clinical characteristics influence screening intervals for diabetic retinopathy. Diabetologia. 2013;56:2147–2152. doi: 10.1007/s00125-013-2989-7. [DOI] [PubMed] [Google Scholar]
- 35.Evans JR, Michelessi M, Virgili G. Laser photocoagulation for proliferative diabetic retinopathy. Cochrane Database Syst Rev. 2014;11 doi: 10.1002/14651858.CD011234.pub2. CD011234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Virgili G, Parravano M, Menchini F, Evans JR. Anti-vascular endothelial growth factor for diabetic macular oedema. Cochrane Database Syst Rev. 2014;10 doi: 10.1002/14651858.CD007419.pub4. CD007419. [DOI] [PubMed] [Google Scholar]
- 37.Mitchell P, Bandello F, Schmidt-Erfurth U, et al. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118:615–625. doi: 10.1016/j.ophtha.2011.01.031. [DOI] [PubMed] [Google Scholar]
- 38.Korobelnik JF, Do DV, Schmidt-Erfurth U, et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2014;121:2247–2254. doi: 10.1016/j.ophtha.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 39.Elman MJ, Bressler NM, et al. Diabetic Retinopathy Clinical Research Network, Expanded 2-year follow-up of ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2011;118:609–614. doi: 10.1016/j.ophtha.2010.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Diabetic Retinopathy Clinical Research Network. A randomized trial comparing intravitreal triamcinolone acetonide and focal/grid photocoagulation for diabetic macular edema. Ophthalmology. 2008;115:1447–1459. doi: 10.1016/j.ophtha.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.Tamayo T, Brinks R, Hoyer A, Kuß O, Rathmann W. The prevalence and incidence of diabetes in Germany—an analysis of statutory health insurance data on 65 million individuals from the years 2009 and 2010. Dtsch Arztebl Int. 2016;113:177–182. doi: 10.3238/arztebl.2016.0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E2.Bundesärztekammer (BÄK) Kassenärztliche Bundesvereinigung (KBV) Beurteilungskriterien für Leitlinien in der medizinischen Versorgung - Beschlüsse der Vorstände der Bundesärztekammer und Kassenärztlicher Bundesvereinigung, Juni 1997. Dtsch Arztebl. 1997;94:A2154–###A-2155. [Google Scholar]
- E3.Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF) Zuckschwerdt. München: 2012. Das AWMF-Regelwerk Leitlinien. [Google Scholar]
- E4.Ärztliches Zentrum für Qualität in der Medizin (ÄZQ), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF) Deutsches Instrument zur methodischen Leitlinien-Bewertung (DELBI) Fassung 2005/2006 + Domäne 8. www.leitlinien.de/mdb/edocs/pdf/literatur/delbi-fassung-2005-2006-domaene-8-2008.pdf (last accessed on 20 July 2016) [Google Scholar]
- E5.Bundesärztekammer (BÄK) Kassenärztliche Bundesvereinigung (KBV), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF) Nationales Programm für VersorgungsLeitlinien Methoden-Report 4. Auflage. www.leitlinien.de/mdb/downloads/nvl/methodik/mr-aufl-4-version-1.pdf (last accessed on 20 July 2016) [Google Scholar]
- E6.Bundesärztekammer (BÄK) Kassenärztliche Bundesvereinigung (KBV), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF) Nationale VersorgungsLeitlinie Typ-2-Diabetes Prävention und Therapie von Netzhautkomplikationen - Langfassung, 1. Auflage. Version 2.6. www.leitlinien.de/mdb/downloads/nvl/diabetes-mellitus/archiv/netzhautkomplika tionen/dm-netzhautkomplikationen-vers2.6-lang.pdf (last accessed on 20 July 2016) [Google Scholar]
- E7.Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ. 2001;323:334–336. doi: 10.1136/bmj.323.7308.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E8.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490–1497. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E9.Sackner-Bernstein JD, Kowalski M, Fox M, Aaronson K. Short-term risk of death after treatment with nesiritide for decompensated heart failure: a pooled analysis of randomized controlled trials. JAMA. 2005;293:1900–1905. doi: 10.1001/jama.293.15.1900. [DOI] [PubMed] [Google Scholar]
- E10.Dunham RB. Nominal group technique: A users’ guide Madison. Wisconsin School of Business. 1998 [Google Scholar]
- E11.Stinner B, Bauhofer A, Sitter H, Celik I, Lorenz W. Nominaler Gruppenprozess als Konsensusinstrument zur Einschränkung der Therapieheterogenität in einer komplexen „outcome“-Studie. Intensivmed Notfallmed. 2000;37 [Google Scholar]
- E12.Murphy MK, Black NA, Lamping DL, et al. Consensus development methods, and their use in clinical guideline development. Health Technol Assess. 1998;2 i-88. [PubMed] [Google Scholar]
- E13.American Diabetes Association (ADA) Standards of medical care in diabetes 2014. Diabetes Care. 2014;37:S14–S80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- E14.Advani A, Altomare F, Stockl F Canadian Diabetes Association (CDA) Retinopathy—clinical practice guidelines 2013. Can J Diabetes. 2013;37:S137–S141. doi: 10.1016/j.jcjd.2013.01.038. [DOI] [PubMed] [Google Scholar]
- E15.Hooper P, Cruess A, et al. Canadian Ophthalmological Society, Canadian Ophthalmological Society evidence-based clinical practice guidelines for the management of diabetic retinopathy. Can J Ophthalmol. 2012;47:S1–S54. doi: 10.1016/j.jcjo.2011.12.025. [DOI] [PubMed] [Google Scholar]
- E16.Bundesärztekammer (BÄK) Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF), Kassenärztliche Bundesvereinigung (KBV) Nationale VersorgungsLeitlinie Nierenerkrankungen bei Diabetes im Erwachsenenalter - Kurzfassung, 1. Auflage, Version 5. http://doi.org/10.6101/AZQ/000127 (last accessed on 20 July 2016) [Google Scholar]
- E17.National Institute for Clinical Excellence (NICE) Royal College Of Physicians. London: 2008. Type 2 diabetes National clinical guideline for management in primary and secondary care (update) [PubMed] [Google Scholar]
- E18.Scottish Intercollegiate Guidelines Network (SIGN) SIGN. Edinburgh: 2010. Management of diabetes A national clinical guideline. [Google Scholar]
- E19.Veterans Health Administration and Department of Defense (VADoD) VADoD clinical practice guideline for the management of diabetes mellitus Version 4.0. healthquality.va.gov/guidelines/CD/diabetes/DM2010_FUL-v4e.pdf (last accessed on 20 July 2016) [Google Scholar]
- E20.Ryden L, Grant PJ, Anker SD, et al. ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD) Eur Heart J. 2013;34:3035–3087. doi: 10.1093/eurheartj/eht108. [DOI] [PubMed] [Google Scholar]
- E21.Hemmingsen B, Lund SS, Gluud C, et al. Targeting intensive glycaemic control versus targeting conventional glycaemic control for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2013;11 doi: 10.1002/14651858.CD008143.pub3. CD008143. [DOI] [PubMed] [Google Scholar]