Sir,
As we know that cyanotic congenital heart disease (CHD) comprises up to 25% of cases of all causes of CHD,[1] there is lack of Indian data about the present spectrum of cyanotic CHD. We did a study to determine the spectrum of patients with cyanotic CHD. All patients with suspected cyanotic CHD were provisionally included in this study. This was a prospective observational study conducted in a tertiary cardiac care center in South Rajasthan over a period of 6 months (January 2016 to June 2016). Patients underwent a thorough echocardiographic evaluation and those patients who had definitive diagnosis of cyanotic CHD were included for final analysis. We had excluded those patients who had normal cardiac evaluation with central or peripheral cyanosis, for example, pulmonary arteriovenous fistula, and methemoglobinemia. We had also excluded patients with idiopathic pulmonary hypertension and acquired cyanosis from Eisenmenger's syndrome. After final inclusion in this study, patients were classified according to the cardiac defects and age at presentation. We had arbitrarily divided the children into four groups, namely, neonatal period (0–1 month), infancy (1–12 months), preschool age (>1–6 years), and school age/adolescence (>6–18 years).
Cyanotic CHD could be divided into two groups depending on the pulmonary blood flow. Patients who have congenital cyanotic heart disease with decreased pulmonary blood flow are called as having tetralogy of Fallot (TOF) physiology, and those who have congenital cyanotic heart disease with increased pulmonary blood flow are called as having transposition of great arteries physiology.[2] Echocardiography is the initial diagnostic test of choice to diagnose CHDs, and here, we have used it for diagnostic confirmation of congenital cyanotic heart disease.[3,4]
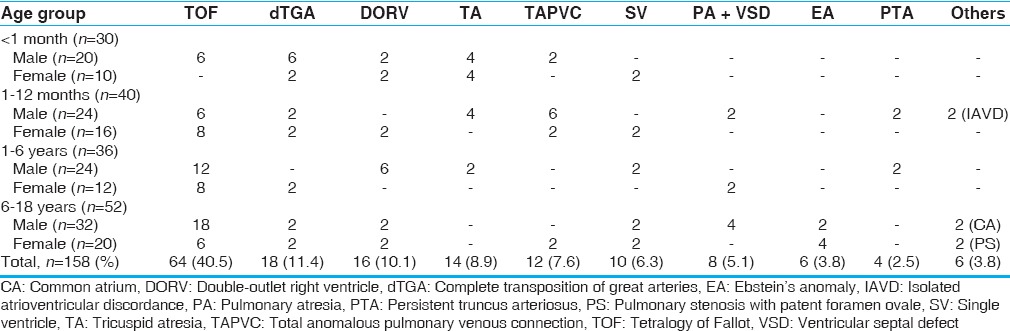
Within the study period, 158 children were diagnosed of having cyanotic CHD through clinical and echocardiographic evaluation. Of the study patients, 100 were male and 58 were female. The various diagnoses of cyanotic CHD in each age group are shown in Table 1. Similar to previous studies, we also found that TOF and its variant were the most common type, with proportion of 40.5% among all congenital cyanotic heart diseases.[5] Complete transposition of great arteries was the next most common cyanotic CHD with the prevalence of 11.4%. Other common malformations included double-outlet right ventricle (10.1%), tricuspid atresia (8.9%), total anomalous pulmonary venous connection (7.6%), single ventricle (6.3%), pulmonary atresia with ventricular septal defect (5%), Ebstein's anomaly (3.8%), truncus arteriosus (2.5%), and other malformations such as common atrium, isolated atrioventricular discordance, and severe pulmonary stenosis with patent foramen ovale.
Table 1.
Distribution of various cyanotic congenital heart disease
This study essentially serves to illustrate the natural history of CHD. The conditions with a relatively poor natural history get eliminated early. Understandably, TOF tends to present later, and because it has the most favorable natural history, it is the most commonly encountered lesion in older children.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mitchell SC, Korones SB, Berendes HW. Congenital heart disease in 56,109 births. Incidence and natural history. Circulation. 1971;43:323–32. doi: 10.1161/01.cir.43.3.323. [DOI] [PubMed] [Google Scholar]
- 2.Humayun KN, Atiq M. Clinical profile and outcome of cyanotic congenital heart disease in neonates. J Coll Physicians Surg Pak. 2008;18:290–3. [PubMed] [Google Scholar]
- 3.Sadoh WE, Uzodimma CC, Daniels Q. Congenital heart disease in Nigerian children: A multicenter echocardiographic study. World J Pediatr Congenit Heart Surg. 2013;4:172–6. doi: 10.1177/2150135112474026. [DOI] [PubMed] [Google Scholar]
- 4.Akhtar K, Ahmed W. Profile of congenital heart disease and correlation to risk adjustment for surgery; an echocardiographic study. J Coll Physicians Surg Pak. 2008;18:334–7. [PubMed] [Google Scholar]
- 5.Waldman JD, Wernly JA. Cyanotic congenital heart disease with decreased pulmonary blood flow in children. Pediatr Clin North Am. 1999;46:385–404. doi: 10.1016/s0031-3955(05)70125-5. [DOI] [PubMed] [Google Scholar]


