Abstract
The purpose of this review is to give a brief background to enable the judicious use of widely performed serum cancer markers. The markers could be product of cancerous cell or as response to cancer. They are usually proteins, which are mainly found in blood or urine. These markers may be employed to predict primary or secondary tumor risk. Sometimes, non-cancerous conditions can also cause elevation of some tumor markers to be higher than normal. Besides, not every cancer patient may have raised level of a tumor marker. For these reasons, knowledge about cancer biomarkers has increased tremendously. Awareness for cancer and related tumor markers providing great opportunities for improving the management of cancer patients by enhancing the efficiency of detection and efficacy of treatment.
Keywords: Biomarkers, cancerous, oral squamous cell carcinoma, tumor markers
Introduction
These are biochemical indicators of presence of a tumor.[1] In clinical practice, it refers to a molecule that can be detected in plasma and body fluids.[2] Tumor markers are measurable biochemicals that are associated with a malignancy. These markers are either produced by tumor cells (tumor-derived) or by the body in response to tumor cell (tumor-associated). They are typically substances that are released into the circulation and thus measured in the blood.[3,4] Tumor markers are not the primary modalities for cancer diagnosis rather they can be used as laboratory test to support the diagnosis.[1]
Cancer is a cluster of diseases involving alterations in the status and expression of multiple genes that confer a survival advantage and undiminished proliferative potential to somatic or germinal cells.[3] Alterations primarily in three main classes of genes, namely (proto) oncogenes, tumor suppressor genes, and DNA repair genes collectively contribute to the development of cancer genotype and phenotype that resists the natural and inherent death mechanism(s) embedded in cells (apoptosis and like processes), coupled with dysregulation of cell proliferation events [Figure 1].[1]
Figure 1.
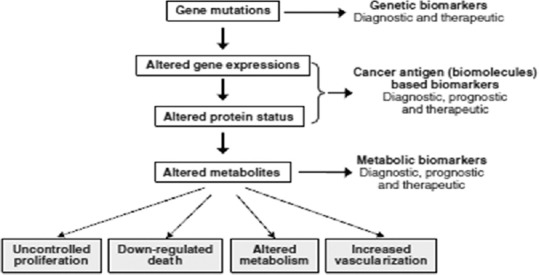
The process of carcinogenesis showing opportunities of identifying biomarkers
Use and Advantages
Although tumor markers are usually imperfect as screening tests for detection of occult (hidden) cancers, once a particular tumor has been found using a marker, the marker may be a way of monitoring the success (or failure) of treatment.
The tumor marker level may also reflect the extent (the stage) of the disease, indicating how quickly the cancer is likely to progress and helping to determine the prognosis (outlook).
Rising levels of tumor markers on test results can be, but are not always worrisome. Although changes in tumor marker levels may be the cause for alarm, other noncancerous diseases can cause test results to vary. Conditions in the laboratory that process tests may also alter the results.[5,6]
Advantages of using tumor markers
Screening and early detection of cancer
Screening refers to looking for cancer in people who have no symptoms of the disease, while early detection is finding cancer at an early stage. Although tumor markers were first developed to test for cancer in people without symptoms, very few tumor markers have been found to be helpful in this way because most tumor markers have not been shown to detect cancer much earlier than they would have been found otherwise.
Aid in the diagnosis of cancer
In most cases, cancer can only be diagnosed by a biopsy and tumor markers are usually not used to diagnose cancer. However, tumor markers can help determine if a cancer is likely in some patients. It can also help diagnose the origin of cancer in patients presenting with advanced widespread disease.
Determine response to therapy
One of the most important uses for tumor markers is to monitor patients being treated for cancer. If the initially raised tumor marker level goes down with treatment, it indicates that the treatment is working and is having a beneficial effect. On the other hand, if the marker level goes up, then the treatment is probably not working and change of treatment should be considered.
Prognostic indicator of disease progression
Some newer tumor markers help to assess how aggressive a cancer is likely to be or even how well it might respond to certain drugs.
Indicate relapse during follow-up period
Indicate relapse during follow-up period. Markers are also used to detect cancers that recur after initial treatment. Some tumor markers can be useful once treatment has been completed and with no evidence of residual cancer left. These include prostate-specific antigen (for prostate cancer), human chorionic gonadotropin (for gestational trophoblastic tumors and germ cell tumors of ovaries and testicles), and cancer 125 (for epithelial ovarian cancer).
Disadvantages
Being able to deduce diagnostic patterns that are unique to specific cancer states is a challenge because of the biological variability in an individual patient's sample, as well as the huge range of biomarker concentrations in all patients compared.
Differences in sample collection, handling or storage, and profiling techniques among various research sites may change the protein profile obtained from a given sample. Therefore, standardization issues regarding biological variation, preanalytical variables, and analytical variability must be tackled before standard values can be established.
A major problem in the identification of cancer biomarkers is the very low concentrations of markers obtained from tissues with small, early-stage cancer lesions.[5,7]
Other problems
Other problems associated with the identification of cancer biomarkers are as follows:
Lack of reliability
Proteins and/or modified proteins may vary among individuals, between cell types, and even within the same cell under different stimuli or different disease states. Hence, it is difficult to know which value obtained from an individual is accurate and what value in different patients indicates a problem
Normal cells as well as cancer cells can produce most tumor markers
Tumor markers are not always present in early-stage cancers
Tumor markers can be present because of noncancerous conditions
People with cancer may never have elevated tumor markers in their blood
Even when tumor marker levels are high, they are not specific enough to confirm the presence of cancer.
Note: A host of tumor markers are identified every year and only a few have stood the test of time and can be used clinically.[8,9]
Examples
-
Carcinoembryonic antigen (CEA)
- It is produced by embryonic tissue of gut, pancreas, and liver
- It is a complex glycoprotein elaborated by many different neoplasms
-
Serum level is positive in:
- 60–90% - Colorectal carcinoma
- 50–80% - Pancreatic carcinoma
- 25–50% - Gastric and breast carcinoma.
-
CEA is elevated in many benign disorders:
- Alcoholic cirrhosis
- Hepatitis
- Ulcerative colitis
- CEA assays lack both sensitivity and specificity required for detection of early cancers.
-
Prostate-specific antigen and prostate-specific membrane antigen
- They detect prostate cancer.
-
Human chronic gonadotropins
- They detect testicular tumors.
-
Cancer 125
- It detects ovarian cancer.
Proteins: Most recently, detection of four proteins in the saliva of cancer patients has been found to be the useful markers of oral cancer with 90% sensitivity and 83% specificity for oral squamous cell carcinoma. These proteins include (i) calcium-binding protein MRP14 implicated in several types of cancer; (ii) CD59 overexpressed on tumor cells that enables them to escape from complement-dependent and antibody-mediated immune responses; (iii) Profilin 1, a protein involved in several signaling pathways with cytoplasmic and nuclear ligands, generally secreted into tumor microenvironments during the early progressive stage of tumorigenesis; and (iv) catalase, a member of the enzymatic antioxidative system, whose level is elevated in many human tumors and involved in carcinogenesis and tumor progression. However, long-term studies employing large number of oral cancer patients as well as subjects at high risk of developing oral cancer are needed to validate these potential biomarkers[1,10]
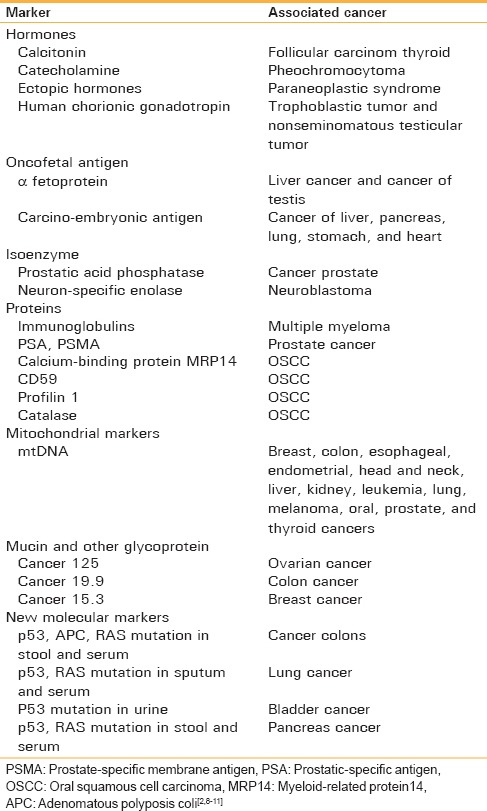
Mitochondrial markers: Mitochondria typically contain multiple haploid copies of their own genome (16.5 kb), including most components of transcription, translation, and protein assembly. mtDNA is present at 1000–10,000 copies/cell, and the vast majority of these copies are identical (homoplasmic) at birth. Several mutations in the mtDNA, particularly in the D-loop region, have been recently found in breast, colon, esophageal, endometrial, head and neck, liver, kidney, leukemia, lung, melanoma, oral, prostate, and thyroid cancers.[11] Brief overview of tumor markers have been listed in Table 1.
Table 1.
Classification scheme of tumor markers
Precautions
There is not a good consensus in the medical community about the value of most tumor or markers
They lack specificity and accuracy
False-positives can cause emotional distress and fear
It is not yet determined if there is savings of life or money with testing
Currently, much controversy surrounds the issue of mass screening for cancer using tumor marker.[8]
Future Scope of Tumor Markers
The future holds great promise for the field of tumor markers. With the advances in genomic and proteomic technology, human diseases will be classified based on molecular rather than morphological analysis. This will occur through techniques such as laser capture micro-dissection for the procurement of tissues and cells, and by combining genomic and proteomic analysis. Early diagnosis of disease is possible by using unique gene or protein profiles consisting of multiple biomarkers. The analysis of panels of protein biomarkers may be performed by using traditional ELISA or antibody-based protein chips for parallel testing. Furthermore, there will be many more diagnostic tests generated as a result of genomic and proteomic discoveries.
In the future, the development of biochips will grow much faster than rest of the diagnostic industry which will include DNA, RNA, and protein chip. All the types of samples will be analyzed including tissues, cells, and body fluids. Integrated diagnostic tools that combine these methods with molecular imaging technique will be used. Finally, bioinformatics will link to scientific data to clinical information to provide and better more comprehensive care of the patient's health. We will witness a rapid translation of new discoveries from the laboratory to patient's bedside. With advances in proteomic, laboratory testing and hence laboratory diagnosis become even more important in the integral health-care delivery system.[12]
Conclusion
A large number of molecular markers are associated with the occurrence, progression, and prognosis of carcinoma. Markers of increased proliferation in oral cancer have been identified and explored for more than a decade. Although a large body of literature exists on the association of these markers with tumor grading and different degrees of dysplasia in premalignant lesions, it is surprising that there are only a few markers that have an impact on prognosis. Nevertheless, markers of cellular proliferation are difficult to interpret as an independent scale for judgment for tumor prognosis.
There is ever-growing number of molecular markers for oral cancer. Nevertheless, a number of studies have shown that it is not the presence of tumor markers as such that make up for the prognosis of the disease, but also the location of these markers within the tumor. In particular, the invasive front of the tumor appears to be of great importance for prognosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bhatt AN, Mathur R, Farooque A, Verma A, Dwarakanath BS. Cancer biomarkers – Current perspectives. Indian J Med Res. 2010;132:129–49. [PubMed] [Google Scholar]
- 2.Virji MA, Mercer DW, Herberman RB. Tumor markers in cancer diagnosis and prognosis. CA Cancer J Clin. 1988;38:104–26. doi: 10.3322/canjclin.38.2.104. [DOI] [PubMed] [Google Scholar]
- 3.Sotiriou C, Lothaire P, Dequanter D, Cardoso F, Awada A. Molecular profiling of head and neck tumors. Curr Opin Oncol. 2004;16:211–4. doi: 10.1097/00001622-200405000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Wu JT. In: Diagnosis and management of cancer using serologic tumor markers. Clinical Diagnosis and Management by Laboratory Methods. 20th ed. Henry JB, editor. Philadelphia, PA: WB Saunders Company; 2001. pp. 1028–42. [Google Scholar]
- 5.Garg A, Ahmed S, Sinha A, Singh HP. Tumor markers – Its advantages and limitations in diagnosis of oral cancer. Univ J Dent Sci. 2015;1:42–45. [Google Scholar]
- 6.Tumuluri V, Thomas GA, Fraser IS. Analysis of the Ki-67 antigen at the invasive tumour front of human oral squamous cell carcinoma. J Oral Pathol Med. 2002;31:598–604. doi: 10.1034/j.1600-0714.2002.00042.x. [DOI] [PubMed] [Google Scholar]
- 7.Matsumoto M, Komiyama K, Okaue M, Shimoyama Y, Iwakami K, Namaki S, et al. Predicting tumor metastasis in patients with oral cancer by means of the proliferation marker Ki67. J Oral Sci. 1999;41:53–6. doi: 10.2334/josnusd.41.53. [DOI] [PubMed] [Google Scholar]
- 8.Eissa S. Tumor Markers. Philadelphia: Lippincot Williams & Wilkins; 1999. [Google Scholar]
- 9.Sharma S. Tumor markers in clinical practice: General principles and guidelines. Indian J Med Paediatr Oncol. 2009;30:1–8. doi: 10.4103/0971-5851.56328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hu S, Arellano M, Boontheung P, Wang J, Zhou H, Jiang J, et al. Salivary proteomics for oral cancer biomarker discovery. Clin Cancer Res. 2008;14:6246–52. doi: 10.1158/1078-0432.CCR-07-5037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jakupciak JP, Wang W, Markowitz ME, Ally D, Coble M, Srivastava S, et al. Mitochondrial DNA as a cancer biomarker. J Mol Diagn. 2005;7:258–67. doi: 10.1016/S1525-1578(10)60553-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rein BJ, Gupta S, Dada R, Safi J, Michener C, Agarwal A. Potential markers for detection and monitoring of ovarian cancer. J Oncol 2011. 2011:475983. doi: 10.1155/2011/475983. [DOI] [PMC free article] [PubMed] [Google Scholar]


