Abstract
Background:
Coronal incision is a popular and versatile surgical approach to the anterior cranial vault and upper and middle third facial skeleton. The flap itself permits widespread exposure of the fractures in this region. The bicoronal flap was first described by Hartley and Kenyon (neurosurgeons) to gain access to the anterior cranium in 1907. It extension as an access flap to the upper and lateral aspect of the face was pioneered by Tessier (1971). Esthetically, it is pleasing as the surgical scar is hidden within the hair.
Aims:
To evaluate the versatility of coronal incision using various modifications advocated in incision, exposure to fractured site, and closure of flap in treating the upper and middle third facial fractures.
Materials and Methods:
A total of ten patients diagnosed with upper and middle third facial fractures requiring open reduction and internal fixation/correction of contour defect were selected after preoperative clinical and radiographic (computed tomography scan) evaluation. All the cases were operated by coronal approach to gain the access to the fracture/defect site for reduction/correction of the defect. Advantages and complication are evaluated.
Results:
Excellent access and anatomical reduction by this approach with least number of complications; if it is performed with healthy knowledge of anatomy of the scalp and temporal region. Certain minimal complications have also been noted using various modifications used in the procedure.
Conclusion:
Despite of prolonged surgical time for the exposure, it is very advantages in treating upper and middle third facial fractures due to wide access and discreet scar (minimal).
Keywords: Complications, coronal incision, open reduction and internal fixation, upper and middle third facial fracture
Introduction
Maxillofacial trauma is an important field of study in plastic and reconstructive procedure. The most significant recent advancement made in the treatment of facial trauma is the rigid internal fixation and surgical approaches allowing wide exposure of the affected area. Access to the site of affected area may be made either through laceration associated with the injuries or by elective incision. The main goal in the treatment of facial fractures is healing without postoperative morbidity or long-term deformities. The coronal incision was initially used in the treatment of nasofrontal injuries for its wide visualization of the operative field. Later, it was being used in cases of fractures involving frontal, nasoorbitoethmoid (NOE), severely comminuted or displaced zygomatic arch and its components; reduction and fixation to reestablish the facial contour is required.
The flap itself permits widespread exposure of the skull and upper and lateral midfacial skeleton, with minimal morbidity.[1] In treating fractures of the zygomatic complex, various approaches, and surgical incisions have been described (Michelet et al., 1973), the coronal being one of them. Traditional closed techniques still compete with total exposure of all the fracture lines by multiple incisions (Manson et al., 1985), or routine coronal incisions (Gruss et al., 1990).[2] The bicoronal flap is arguably the most versatile of their surgical access technique. While there is no doubt due to this wide exposure of the cranial and facial skeleton obtained, a balance has to be maintained between exposure and flap-associated morbidity.[3] The purpose of this study was aimed to overcome this morbidity using various modifications reviewed in literature.
Materials and Methods
A prospective study was conducted on ten patients above 10 years of age who required open reduction and internal fixation (ORIF) of the upper and middle third facial fractures with or without other associated fractures of the facial skeleton.
Inclusion criteria
(1) Patients with well-defined hairline, (2) age above 10 years, (3) patients diagnosed with fracture of frontal bone, nasal, NOE, supraorbital, lateral orbital, comminuted zygomatic complex fracture, grossly displaced zygomatic arch fractures and residual defect due to trauma and other associated midface fractures and (4) clearance from the neurosurgeon.
Exclusion criteria
(1) Preoperative facial nerve palsy, (2) previously operated by the coronal incision, (3) mentally retarded patients, (4) patients who have fear of scar, and (5) medically compromised patients.
Mode of injury, age, gender, and social habits is all recorded. In this study group, seven patients were operated immediately after facial trauma (within a period of 10 days from trauma), three patients had posttraumatic residual defect due to trauma (who underwent primary treatment and operated for the correction of residual defect after a period of above 10 days). Among the study group, seven patients (four frontal bone and three zygomatic complex fractures) were planned for the ORIF and three patients (two frontal bone and one zygomatic bone fractures) were planned for reconstruction of the primary defect to maintain the anatomical contour. Case details are shown in Table 1.
Table 1.
Case details
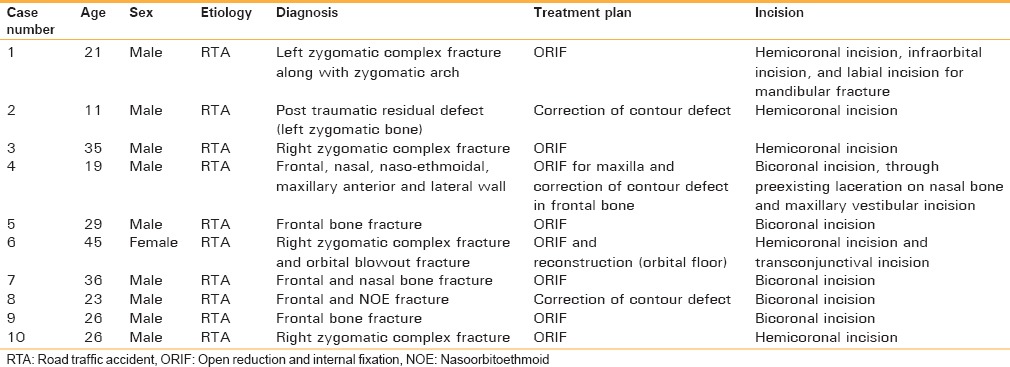
Parameters evaluated were Site of fracture – Assessed with any of the following computed tomography scan, orthopantomogram, paranasal sinus and submentovertex skull radiographs and intraoperative clinical examination. Time taken to expose the fracture: By the coronal incision from the moment incision placed to complete exposure of the fracture. Access to the fracture site: Assessed by surgeon subjectively as excellent, good. Anatomic reduction of fracture: Assessed with postoperative radiographs as excellent (no visible radiographic gap between fracture fragments postoperatively) and good (<7 mm of visible radiographic gap between fracture fragments). Postoperative hemorrhage/hematoma: Assessed clinically. Infection: Assessed by swelling, pain, tenderness, wound dehiscence, or pus discharge at the operated site. Temporal branch of facial nerve weakness: Assessed clinically by examination of frontal wrinkling, tight closure of the eyes. Duration of postoperative hospitalization: Calculated from the day of operation until the day of discharge (in days). Temporal fossa hollowing: Assessed by clinical examination only (concavity) has present and not present. Alopecia: Assessed by clinical examination. Scar at the operated site: Assessed by clinical examination as discreet (thin incision line without fibrosis) and hypertrophic (with wide fibrosis).
All of the patients were followed for minimum of 12th postoperative weeks, with a regular interval of follow-up at 1st, 2nd, 4th, 8th, and 12th to evaluate prognoses and frequency of complication.
Surgical Technique
All cases were treated under general anesthesia either with nasotracheal intubation, submental intubation, or oral intubation. Initially, line of incision is marked with gentian violet; incision site is infiltrated by 10–12 ml of local anesthesia with adrenaline 1:100,000 along the marked incision line.
Bicoronal incision
Begins at the upper attachment of the helix extending transversely over the vault of the skull crossing the midline and extending to the helix of the opposite side (used in upper one-third facial fractures where access is required for frontal bone)[4] [Figures 1 and 2].
Figure 1.
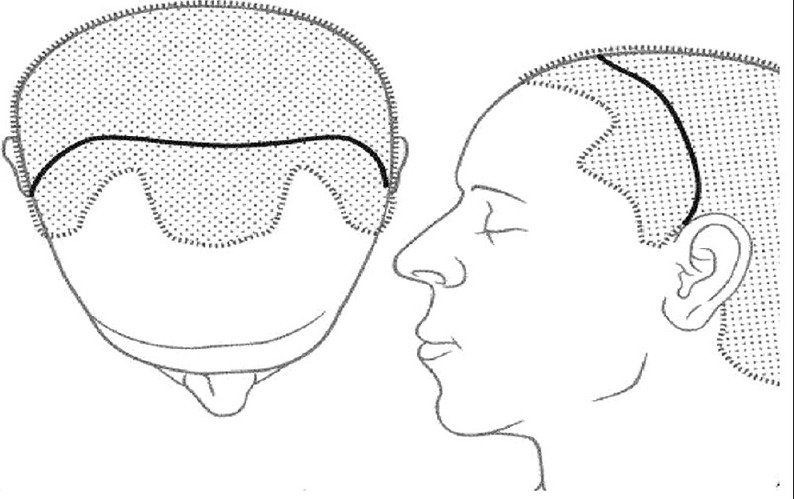
Line diagram of bicoronal incision (note the relationship of the incision to the hair line)
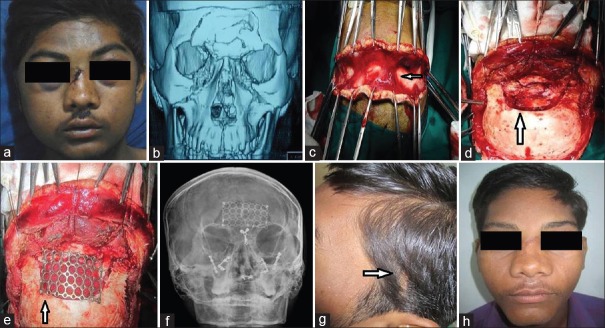
Figure 2.
Clinical case: (a) Preoperative profile, (b) preoperative computed tomography scan, (c) layer by layer incision, (d) exposure of the fractured, (e) mesh was used to restore contour, (f) postoperative X-ray, (g) discreet scar, (h) postoperative profile
Hemicoronal incision
Begins at the preauricular region in front of the tragus of the ear or little below till the ear lobe attachment[5] and extending transversely over the vault of the skull to the midline (used in middle facial fractures where access is required for zygoma, zygomatic arch, and lateral orbital rim) [Figures 3 and 4].
Figure 3.

Line diagram of hemicoronal incision. (a) Incision with preauricular extension, (b) relation between incision and superficial temporal vessel
Figure 4.
Clinical case: (a) Preoperative, (b) residual defect in lateral orbital rim, (c) preoperative computed tomography scan, (d) exposure of the fractured site, (e) graft fixation done (f) postoperative X-rays, (g) discreet scar, (h) correction of contour defect
Linear incision with slight forward curvature at the vertex of the skull following the hairline, but 2–3 cm posterior to it was given in nine cases except in one case were the incision was curvilinear.[6] The flap is raised along with the periosteum. Continuous locking sutures at the flap margin (or) hemostats were used as an aid to achieve hemostasis. Hemostatic clips (Raney's) were avoided in our study to minimize hair loss.[7] The flap is raised to gain exposure of the fractured site. If supraorbital margins had to be exposed neurovascular bundles were released from the supraorbital notch/foramen and reflected along with the flap.[6] In nine cases, lateral dissection was carried out on the outer surface of the temporalis fascia to approximately 2 cm above the zygomatic arch. At that point where the temporalis fascia splits into two layers, an incision running anteriosuperiorly at 45° was made through the superficial layer of the temporalis fascia to spare the frontal branches of facial nerve.[4,2] In one case, the lateral incision was carried till subperiosteal layer (Dual plane dissection) by incising the temporalis muscle to expose the lateral orbital rim.[8] Once the plane of dissection was established deep to the superficial layer of the temporal fascia, the dissection was continued inferiorly until the periosteum of the zygomatic arch.[4,6] It was then incised and reflected laterally over the arch, the body of the zygoma, and the lateral orbital rim. It provided excellent exposure of the frontal bone, the upper part of the nose and nasoethmoidal region, the roof, medial and lateral walls of the orbit, the zygomatic bone, and the entire zygomatic arch[9,10,11] [Figure 5]. Other incisions such as intraoral vestibular and the infraorbital were added for further exposure when necessary.[12] After reduction and fixation, double relaxation suturing was done for periosteum and the temporal fascia sutured with 2°-3° vicryl, galea, and skin were closed in layers with 2–3° proline.[13] Pressure dressing was applied for 48 h in all patients and in five cases where the chance of hematoma is expected, there suction drain was used to minimize the postoperative complication of hematoma.[14]
Figure 5.
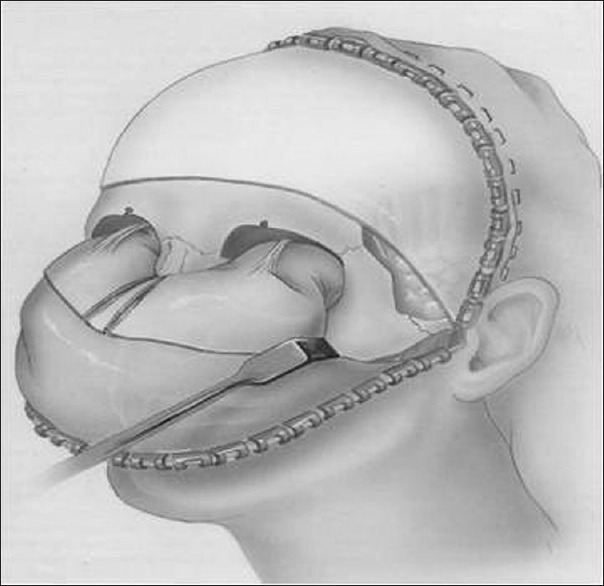
Dissection exposing the upper & middle third and anterolateral part of skull
Results
The etiologies of the fractures were primarily because of road traffic accidents. Of 10 patients, 9 patients were male and 1 female, with a male:female ratio of 9:1. All the patients ranged from 11 to 45 years with the mean age of 27.1 years. Seventy percent (7 cases) pre- and post-operative radiographs were compared to check for proper reduction and fixation. Among them, 20% (2 cases) were assessed as good reduction, 50% (5 Cases) as excellent. In the remaining 30% (3 cases), this surgical incision was performed to maintain the facial contour, which was achieved excellently.
The average time taken for exposure of the fracture site by the hemicoronal incision was 27 min with values ranging from 25 min to 30 min. In case of bicoronal incision, the average time for exposure of fracture is 41 min with values ranging from 35 to 45 min. Surgical access was good in 10% of (1 case) cases and excellent in 90% of cases (9 cases).
None of the cases in this study encountered any form of infection, except for one patient (Case 3), who had swelling with abscess for almost 8 weeks postoperatively. It subsided on taking oral medication but recurred once the medication was discontinued and swelling completely subsided after the plate removal on the 12th postoperative week. However, facial asymmetry in the region of middle one-third of zygomatic arch is persistent till date.
In this study, 30% (3 cases) were reported with transient deficit of temporal branch of facial nerve. Out of which, 20% (2 cases) recovered within 2nd postoperative week, whereas in 10% (1 case) facial nerve palsy recovered by the end of 12th postoperative week. The average duration of postoperative hospitalization in 50% (5 cases) with suction drains was 4 days and in 50% (5 cases) without suction drains was 3 days. The surgeon was comfortable in gaining access to fractured site in all the cases. In 90% (9 cases), patients were satisfied with the esthetics due to minimal or invisible scar within the hairline. Except in 10% (1 case), where there is persistent facial asymmetry till date even after removal of the plate at 8th postoperative week [Table 2].
Table 2.
Result

In this study, no cases of postoperative hemorrhage, hematoma, permanent facial nerve palsy (temporal branch), alopecia, hypertrophic scar or temporal fossa hollowing were reported.
Discussion
Patients with a severe comminution and displacement of the facial skeleton have been treated conventionally through small local incisions with the wiring of bone fragments in position, immobilization of jaws with arch bars, and occasional use of immediate bone grafting for the restoration of facial buttresses. In selected patients, the coronal approach provides wide exposure and direct availability of calvarial bone grafts and enables the surgeon to accurately reconstruct the shattered face (multiple fractures) with intact bone of similar shape and consistency. Large areas of shattered bone can be easily replaced with intact segments of calvarial bone graft and are subsequently immobilized accurately through the widely exposed operative field. This technique provides for reconstruction of all fractures or missing bony fragments under direct vision. It has a great advantage over the conventional techniques of reduction and fixation while treating upper and middle facial fractures.[3]
Out of ten patients, there was high male predominance to female with ratio of 9:1, which correlates with various studies by Nysing, Lundin et al.[15] and Adam et al.[16] who, had a male to female ratio of 4:1 and study conducted on coronal approach for zygomatic complex fracture by Shetty et al.,[17] who had a male to female ratio of 12:0. Road traffic accidents are the major cause of fractures of the upper and middle third facial region (100%).[11,12] The age groups of patients ranged from 11 years to 45 years with an average 27.1 years, correlates with results published by Zhang et al.,[18] who had a mean age of 35 years, Adam et al.,[16] who had a mean age of 32.33 years and also as reported by Ellis et al., who reported their peak in the second and third decades of life.[15]
In nine cases, the classical coronal incision was used as advocated by Abubaker et al.[4] in their study on the coronal incision for craniomaxillofacial injuries. In one case, curvilinear skin incision was placed till helix and extended to traditional preauricular incision, which was advocated by Ramon et al.[6] and Munro and Fearon.[19] Five cases were operated by hemicoronal incision with preauricular extension, and five cases were treated with bicoronal approach, whereas in four cases, additional local incisions were used to gain access for fractured site. In one case, dual plane dissection (temporal region) was used as advocated by Srinivasan et al.[8] Extended coronal incision into preauricular region with traditional coronal incision will give access to temporomandibular joint (TMJ) and zygomatic arch as advocated by Dunaway and Trott.[9] The finding of this study correlated with above reported findings during incision placement.
Shepherd et al.[20] and Marschall et al.[3] have all reported excellent access to the upper midfacial skeleton,[7,10] Lefort III fracture,[7] supraorbital margin,[7] frontonasal suture,[21] nasoethmoidal suture, lateral orbital region,[8] zygomatic complex fracture,[18] zygomatic arch, and TMJ[9] by the coronal surgical incision. The finding of our study correlates with the above findings, with excellent access. Even reconstruction of supraorbital,[21] frontal,[21] nasal,[22] and nasoethmoidal[23] region can be done with minimal scar. The finding of this study correlated with the above findings.
In 7 cases, 6 cases achieved excellent reduction and 1 case achieved good reduction. In the remaining 3 cases, anatomical correction was evaluated esthetically by correcting contour defect which is caused due to trauma, with autografts (iliac bone) in one case (lateral orbital rim) and alloplast (titanium mesh) in two cases (frontal bone). The finding of this study correlates with studies of Abubaker et al.,[4] who reported that this approach allows for accurate anatomic reduction and fixation of fractures; Marschall et al.[3] reported that reduction of displaced fragments under direct vision and replacement of missing bone with a required material can be best achieved by coronal approach.
No evidence of hematoma was recorded. Suction drains were used in 5 cases along with double-layered suturing for incision closure (galea to galea and skin to skin), and pressure dressing for 48 h was applied for all cases in our study. No significant difference was noticed on using suction drains among the study group. Shepherd et al.[20] reported just one case of hematoma formation in a series of 24 cases. Abubaker et al.[4] reported two cases (repeated episodes of hypertension) out of 28 patients with hematoma. Shetty et al.[17] reported no case of hematoma in his study of coronal approach for the treatment of the zygomatic complex fractures. Hodges and Altman[14] reported that the use of stabilize drains while closing coronal flap will minimize the complication of hematoma. This technique was used in five cases in this study, and findings were correlated.
No cases of flap infection were reported in the study group. Only one case reported with an abscess which resolved on the removal of mini plate in F–Z region of lateral orbital rim by giving a local incision and antibiotic therapy. The findings are similar to various studies of Frodel et al.,[24] who reported no cases of flap infection, whereas just four cases of stitch abscess, which resolved on the removal of sutures; Mitchell et al.[25] reported wound infection in six cases who were operated for primary facial trauma due to secondary infection.
Three patients had reported with transient deficit of temporal branch of facial nerve. Out of which two cases recovered within 2nd postoperative week while in one case, facial nerve palsy recovered by the end of 12th postoperative week. Shepherd et al.[20] had 3 cases of facial nerve weakness, out of which two resolved within 9 months and one case persisted till 2 years. In the retrospective study by Zhang et al.,[18] Six out of 69 cases had facial nerve weakness, and one case had a permanent palsy. Frodel et al.[24] had reported nine patients with temporary motor weakness and two patients with permanent facial nerve weakness. Mitchell et al.[25] reported 6 cases of transient deficit of the temporal branch which had resolved within the follow-up period. Dunaway and Trott[9] reported three cases with mild temporary facial palsy, which resolved by 6th postoperative week. The finding of this study correlated with above studies.
All the ten cases had negligible scar formation. None of the cases reported with the problem of alopecia by the end of 12th postoperative week. Frodel et al.[24] reported five cases with telogen phenomenon for 0.5–1 cm around the scar, which was till 2–3 months. In one patient, this was permanent. In the patients with hair loss, it was noted that operative time was over 12 h, suggesting prolonged ischemia secondary to the application of raney clips, as a cause for alopecia. For this reason, we avoided usage of raney clips in the study. Burm and Oh[13] reported a surgical procedure to minimize the scar formation and alopecia, by 30° beveling to incision and double relaxation of galeal suturing, as performed on two patients. The finding of this study correlated with above studies.
Surgeon comfort for reduction and fixation of fracture along with correction of contour defect was excellent in all the cases. Findings of this study correlated with the various studies conducted by Hartley and Kenyon (1907), who first reported that these approach will give a good access to anterior cranial vault.[1,2,10,20,24] Abubaker et al.[4] reported that it is the widely accepted approach for the reduction of upper and middle facial fractures along with reconstruction of this area because of its direct accessibility to the fractured site.[3,7,10,15,26]
All the patients were satisfied with this surgical approach except one patient (Case 3). It is esthetically also excellent because most of the surgical scar is hidden within the hairline; even if the incision is extended into the preauricular region, it was not clearly visible.[3,4,7,2,21,23,24,25,26] The duration of postoperative hospitalization, which was to be considered as disadvantage was evaluated. Instead of giving multiple incisions for exposing the fracture site in the upper and middle third region of the face which will cause an esthetically unpleasant appearance with minimal hospitalization, a single incision with hidden scar with mild extended postoperative hospitalization is better.
In this study, we have encountered a new complication of facial asymmetry (Case 3) at the operated site of temporal region, which might probably be due to fibrosis of temporalis muscle because of dual plane dissection which was advocated by Srinivasan et al.[8] This finding has proved that classical coronal incision advocated by Abubaker et al.[4] is better than dual plane dissection.
Conclusion
Coronal incisions have advantages such as giving excellent access to the upper and middle third and lateral side till TMJ for exact anatomical reduction of fractures along with reconstruction of residual defects. On the other hand, it has few disadvantages which can be minimized by having a thorough knowledge of the anatomy of related structures involving the surgical site with various modifications in surgical method. The coronal approach advocated by Abubaker et al. is superior than Srinivasan et al. Even though the time taken for exposure of the fracture site is more by this approach, multiple fractures (least number of complications) can be reduced and fixed with a single incision with a relatively good anatomical reduction. This incision should not be misused in cases of isolated facial fracture, fractures that can be treated by closed reduction and the fractures that can be corrected with preexisting laceration.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kerawala CJ, Grime RJ, Stassen LF, Perry M. The bicoronal flap (craniofacial access): An audit of morbidity and a proposed surgical modification in male pattern baldness. Br J Oral Maxillofac Surg. 2000;38:441–4. doi: 10.1054/bjom.2000.0315. [DOI] [PubMed] [Google Scholar]
- 2.Gruss JS, Van Wyck L, Phillips JH, Antonyshyn O. The importance of the zygomatic arch in complex midfacial fracture repair and correction of posttraumatic orbitozygomatic deformities. Plast Reconstr Surg. 1990;85:878–90. doi: 10.1097/00006534-199006000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Marschall MA, Cohen M, Garcia J, Schafer ME. Craniofacial approach for the reconstruction of severe facial injuries. J Oral Maxillofac Surg. 1988;46:305–10. doi: 10.1016/0278-2391(88)90014-6. [DOI] [PubMed] [Google Scholar]
- 4.Abubaker AO, Sotereanos G, Patterson GT. Use of the coronal surgical incision for reconstruction of severe craniomaxillofacial injuries. J Oral Maxillofac Surg. 1990;48:579–86. doi: 10.1016/s0278-2391(10)80470-7. [DOI] [PubMed] [Google Scholar]
- 5.Netscher DT, Stal S, Peterson R. A critical analysis of coronal incisions. Plast Reconstr Surg. 1990;86:167–9. doi: 10.1097/00006534-199007000-00051. [DOI] [PubMed] [Google Scholar]
- 6.Ruiz RL, Pattisapu JV, Costello BJ, Golden B. The coronal scalp flap: Surgical technique. Atlas Oral Maxillofac Surg Clin North Am. 2010;18:69–75. doi: 10.1016/j.cxom.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Frodel JL, Mabrie D. Optimal elective scalp incision design. Otolaryngol Head Neck Surg. 1999;121:374–7. doi: 10.1016/S0194-5998(99)70223-8. [DOI] [PubMed] [Google Scholar]
- 8.Srinivasan D, White N, Rodrigues D, Solanki G, Dover MS, Nishikawa H. Dual-plane approach for calvarial exposure. J Craniofac Surg. 2010;21:506–7. doi: 10.1097/SCS.0b013e3181d02328. [DOI] [PubMed] [Google Scholar]
- 9.Dunaway DJ, Trott JA. Open reduction and internal fixation of condylar fractures via an extended bicoronal approach with a masseteric myotomy. Br J Plast Surg. 1996;49:79–84. doi: 10.1016/s0007-1226(96)90077-6. [DOI] [PubMed] [Google Scholar]
- 10.Godhi SS, Kukreja P, Singh V, Goyal S. Versatility of the coronal approach in maxillofacial surgery. J Oral Health Community Dent. 2010;4:16–21. [Google Scholar]
- 11.Luo W, Wang L, Jing W, Zheng X, Long J, Tian W, et al. A new coronal scalp technique to treat craniofacial fracture: The supratemporalis approach. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;20:1–6. doi: 10.1016/j.tripleo.2011.01.037. [DOI] [PubMed] [Google Scholar]
- 12.Babu A, Varghese J, Jose M. Coronal and midfacial degloving approach for panfacial trauma. Kerala Dent J. 2011;34:437–9. [Google Scholar]
- 13.Burm JS, Oh SJ. Prevention and treatment of wide scar and alopecia in the scalp: Wedge excision and double relaxation suture. Plast Reconstr Surg. 1999;103:1143–9. doi: 10.1097/00006534-199904040-00007. [DOI] [PubMed] [Google Scholar]
- 14.Hodges S, Altman K. Simple manoeuvre to help stabilize drains when closing a coronal flap. Br J Oral Maxillofac Surg. 2009;47:162. doi: 10.1016/j.bjoms.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 15.Raymond JF, Walter RV. Oral and Maxillofacial Trauma. 2nd ed. Vol. 1. Pennsylvania: W.B. Saunders Company; 2005. pp. 569–642. [Google Scholar]
- 16.Adam AA, Zhi L, Bing LZ, Zhong Xing WU. Evaluation of treatment of zygomatic bone and zygomatic arch fractures: A retrospective study of 10 years. J Maxillofac Oral Surg. 2012;11:171–6. doi: 10.1007/s12663-011-0294-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shetty SK, Saikrishna D, Kumaran S. A study on coronal incision for treating zygomatic complex fractures. J Maxillofac Oral Surg. 2009;8:160–3. doi: 10.1007/s12663-009-0039-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang QB, Dong YJ, Li ZB, Zhao JH. Coronal incision for treating zygomatic complex fractures. J Craniomaxillofac Surg. 2006;34:182–5. doi: 10.1016/j.jcms.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Munro IR, Fearon JA. The coronal incision revisited. Plast Reconstr Surg. 1994;93:185–7. doi: 10.1097/00006534-199401000-00031. [DOI] [PubMed] [Google Scholar]
- 20.Shepherd DE, Ward-Booth RP, Moos KF. The morbidity of bicoronal flaps in maxillofacial surgery. Br J Oral Maxillofac Surg. 1985;23:1–8. doi: 10.1016/0266-4356(85)90072-5. [DOI] [PubMed] [Google Scholar]
- 21.Poole MD, Briggs M. Cranio-orbital trauma: A team approach to management. Ann R Coll Surg Engl. 1989;71:187–94. [PMC free article] [PubMed] [Google Scholar]
- 22.Atlan G, Jammet P, Schmitt-Bernard CF, Dupoirieux L, Souyris F. Bicoronal incision for nasal bone grafting. Int J Oral Maxillofac Surg. 1994;23:2–5. doi: 10.1016/s0901-5027(05)80316-9. [DOI] [PubMed] [Google Scholar]
- 23.Ellis E., 3rd Sequencing treatment for naso-orbito-ethmoid fractures. J Oral Maxillofac Surg. 1993;51:543–58. doi: 10.1016/s0278-2391(10)80512-9. [DOI] [PubMed] [Google Scholar]
- 24.Frodel JL, Marentette LJ. The coronal approach. Anatomic and technical considerations and morbidity. Arch Otolaryngol Head Neck Surg. 1993;119:201–7. doi: 10.1001/archotol.1993.01880140091014. [DOI] [PubMed] [Google Scholar]
- 25.Mitchell DA, Barnard NA, Bainton R. An audit of 50 bitemporal flaps in primary facial trauma. J Craniomaxillofac Surg. 1993;21:279–83. doi: 10.1016/s1010-5182(05)80347-6. [DOI] [PubMed] [Google Scholar]
- 26.Shaw RC, Parsons RW. Exposure through a coronal incision for initial treatment of facial fractures. Plast Reconstr Surg. 1975;56:254–9. doi: 10.1097/00006534-197509000-00002. [DOI] [PubMed] [Google Scholar]