Abstract
Purpose:
The aim of this systematic review was to assess the efficacy of low-level laser therapy (LLLT) in patients with temporomandibular disorders (TMDs).
Methods:
Medline search was done from 1997 to 2011 using search terms appropriate to establishing a relation between LLLT and TMD. Only randomized controlled trials were included in this study. Outcome variables related to pain, muscle tenderness, mandibular movements, and Electromyographic (EMG) activity were considered. Of the 242 articles examined, 13 were finally included in the critical analysis conducted as a part of the present systematic review.
Results:
Of the 242 titles reviewed, only 13 articles were considered eligible. 7 articles showed significant improvement in the study group, whereas 5 showed no significant improvement between the study and control groups. The primary outcome of most of the studies was pain. Other variables considered were muscle tenderness, mandibular movements; EMG activity was considered.
Conclusion:
Our results have shown that LLLT seems to be effective in reducing pain in TMD's. It may be a treatment option for patients with an interest in a noninvasive, complementary therapy.
Keywords: Low-level laser therapy, mandibular movements, temporomandibular disorders
Introduction
Temporomandibular disorder (TMD) or craniomandibular disorders is a collective term embracing a number of clinical problems that involve the masticatory muscles, the temporomandibular joint and associated structures, or both.[1] There are different types of treatments for TMDs. Low-level laser therapy (LLLT) (a form of physical therapy) has been used to reduce signs and symptoms of patients with TMDs, but the effectiveness has still not been totally explained. The basic effects of (LLLT) are biostimulative, regenerative, analgesic, and anti-inflammatory. Thus, the purpose of this systematic review was to evaluate the efficacy of LLLT, and summarize the evidence from, randomized controlled trials (RCTs) that examined the effectiveness of LLLT intervention in the management of TMD.
Methods
Search strategy for identification of the studies
This search strategy was in accordance with the Cochrane guidelines for systemic review. For identification of studies included or considered for this review, MEDLINE search was done using the combination of controlled vocabulary and free text terms. RCTs of LLLT for treating TMDs were included from January 1997 to December 2010. Studies carried out in animal models and studies other than RCT's were excluded. Primary outcome was pain relief with laser therapy in all the articles was assessed using visual analog scale.
Study selection
Titles and abstracts of identified studies were assessed independently to judge if the studies match the inclusion criteria. If it was clear that the study did not refer to an RCT on the treatment of TMD, we excluded it. If it was unclear, then we obtained the full text of the study for assessment.
Data extraction and management
Data were abstracted on first author, year of publication, number of cases, study design, outcomes, and results. The data were extracted and double-checked.
Results
The search identified 242 publications, of which 204 were excluded after reviewing the title or abstract. 33 studies were retrieved for further detailed evaluation resulting in the exclusion of another 20 studies as they did not fulfill the requirement for the inclusion criteria. In the end, 13 studies were considered potentially appropriate to be considered for this review [Figure 1]. Out of the selected 13 studies, 7 indicated the superiority of LLLT over placebo, whereas remaining 6 had no significant differences between real and placebo groups in relation to pain. This review found that there was some evidence supporting that LLLT is effective in reducing pain due to TMDs.
Figure 1.
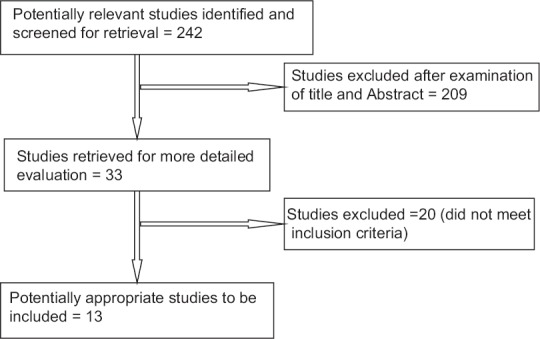
Flow diagram of the selection data process
Discussion
This systematic review examines the evidence from RCTs regarding the efficacy of LLLT for TMDs. Only 13 RCT of LLLT for TMDs met the inclusion criteria for this review [Table 1]. However, the risk of bias in these studies was unclear across several of the domains assessed. In four studies, the number of patients was considered too low to allow generalized result out of which three showed that LLLT is efficacious in significant reduction of pain which was the primary outcome. In the study by Katsoulis et al.,[2] sample size was 11. The authors have justified the low number of participants included in the study explaining that many patients seen at the clinic were referred patients who have already been treated had to be excluded from his study. He has concluded that low-level laser has no detrimental effect on the patients and could be an option for patients interested in noninvasive therapy. Carrasco et al.[3] divided 14 patients into two groups (active and placebo) and concluded that low-intensity laser application is effective in reducing TMD symptoms, and also has influence over masticatory efficiency. Shirani et al.[4] conducted the study on 16 patients and concluded that LLLT is an effective treatment for pain reduction. Conti[5] too had only 20 patients as sample and his conclusion was no significant differences between real and placebo groups.
Table 1.
Characteristics and details of included studies
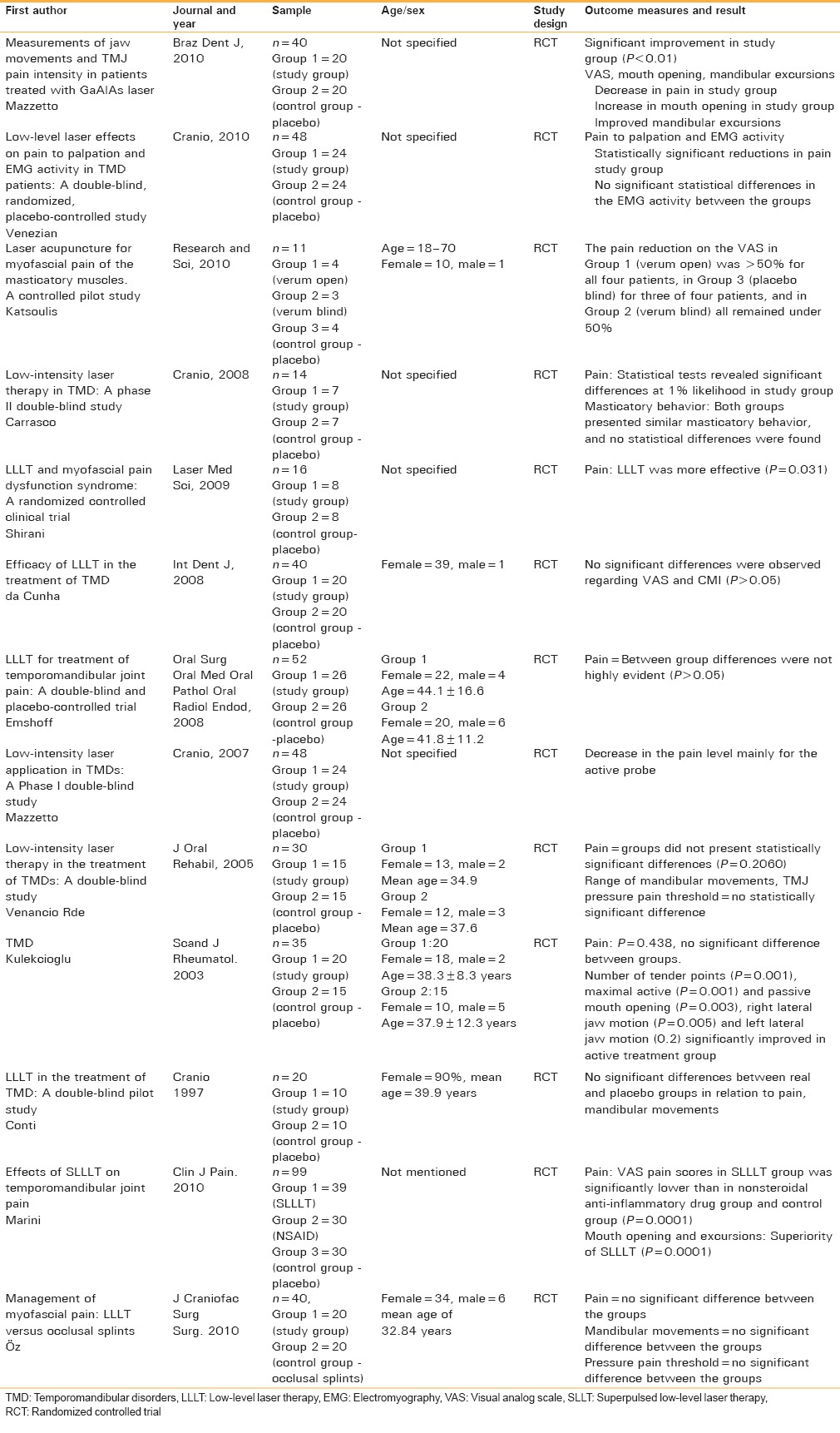
Out of the remaining nine studies, four showed significant improvements in the study groups regarding pain. In the study by Mazzetto et al. (2010),[6] LLLT was effective in the improvement of the range of mandibular lateral movements and caused a significant reduction of pain symptoms. In the study by Venezian et al.[7], LLLT was effective in reducing the pain, but no differences were found when electromyography activity was. Mazzetto et al.[8] found that LLLT effectively promoted significant reduction in the pain. A study by Marini et al.[9] proved the effectiveness of LLLT in the treatment of pain, which was demonstrated by a significant improvement in clinical signs and symptoms of temporomandibular joint disc displacement without reduction and osteoarthritis at the end of treatment. In the studies by da Cunha et al., Emshoff et al. and Venancio et al.,[10,11,12] laser therapy was not better than placebo at reducing TMJ pain. Öz et al.[13] demonstrated that low-level laser therapy is as effective as occlusal splint in pain release and mandibular movement improvement. A study by Kulekcioglu et al.[14] reported significant improvement in mandibular functions in comparison to placebo group. The weakest point of this review is the heterogeneity in the procedures of the treatment and within the patient sample. Heterogeneity may also increase with the differences in numbers and frequencies of the treatment sessions. However, the majority of trials involved treatment for 3–4 weeks, and only two trial treated for 2 weeks and measured the effect of LLLT,[7,9] whereas there were two studies which involved treatment till 8 weeks.[8,11] The literature on LLLT is full of reports that are conflicting, and much of this is caused by the lack of dosage consensus.[15]
Conclusion
Implications for practice
LLLT seemed to be effective in reduction of pain in TMDs. The hypothesis that LLLT acts through a dose-specific anti-inflammatory effect in the irradiated joint capsule is a possible explanation of the positive results. However, due to the limitations of this review, findings must be interpreted with caution.
Implications for research
There is a need for more well-conducted RCTs examining LLLT as interventions for TMDs. These studies need to be clear in the reporting of allocation, blinding, sequence generation, withdrawals, intention-to-treat analysis, and any other potential source of bias in the study. In addition, there should be use of well-validated standardized outcomes so that the RCTs could be compared with other similar trials. The sample size of the RCTs should also be calculated beforehand so that the study has adequate statistical power.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Dias FJ, Issa JP, Vicentini FT, Fonseca MJ, Leão JC, Siéssere S, et al. Effects of low-level laser therapy on the oxidative metabolism and matrix proteins in the rat masseter muscle. Photomed Laser Surg. 2011;29:677–84. doi: 10.1089/pho.2010.2879. [DOI] [PubMed] [Google Scholar]
- 2.Katsoulis J, Ausfeld-Hafter B, Windecker-Gétaz I, Katsoulis K, Blagojevic N, Mericske-Stern R. Laser acupuncture for myofascial pain of the masticatory muscles. A controlled pilot study. Schweiz Monatsschr Zahnmed. 2010;120:213–25. [PubMed] [Google Scholar]
- 3.Carrasco TG, Mazzetto MO, Mazzetto RG, Mestriner W., Jr Low intensity laser therapy in temporomandibular disorder: A phase II double-blind study. Cranio. 2008;26:274–81. doi: 10.1179/crn.2008.037. [DOI] [PubMed] [Google Scholar]
- 4.Shirani AM, Gutknecht N, Taghizadeh M, Mir M. Low-level laser therapy and myofacial pain dysfunction syndrome: A randomized controlled clinical trial. Lasers Med Sci. 2009;24:715–20. doi: 10.1007/s10103-008-0624-5. [DOI] [PubMed] [Google Scholar]
- 5.Conti PC. Low level laser therapy in the treatment of temporomandibular disorders (TMD): A double-blind pilot study. Cranio. 1997;15:144–9. doi: 10.1080/08869634.1997.11746005. [DOI] [PubMed] [Google Scholar]
- 6.Mazzetto MO, Hotta TH, Pizzo RC. Measurements of jaw movements and TMJ pain intensity in patients treated with GaAlAs laser. Braz Dent J. 2010;21:356–60. doi: 10.1590/s0103-64402010000400012. [DOI] [PubMed] [Google Scholar]
- 7.Venezian GC, da Silva MA, Mazzetto RG, Mazzetto MO. Low level laser effects on pain to palpation and electromyographic activity in TMD patients: A double-blind, randomized, placebo-controlled study. Cranio. 2010;28:84–91. doi: 10.1179/crn.2010.012. [DOI] [PubMed] [Google Scholar]
- 8.Mazzetto MO, Carrasco TG, Bidinelo EF, de Andrade Pizzo RC, Mazzetto RG. Low intensity laser application in temporomandibular disorders: A phase I double-blind study. Cranio. 2007;25:186–92. doi: 10.1179/crn.2007.029. [DOI] [PubMed] [Google Scholar]
- 9.Marini I, Gatto MR, Bonetti GA. Effects of superpulsed low-level laser therapy on temporomandibular joint pain. Clin J Pain. 2010;26:611–6. doi: 10.1097/AJP.0b013e3181e0190d. [DOI] [PubMed] [Google Scholar]
- 10.da Cunha LA, Firoozmand LM, da Silva AP, Camargo SE, Oliveira W. Efficacy of low-level laser therapy in the treatment of temporomandibular disorder. Int Dent J. 2008;58:213–7. doi: 10.1111/j.1875-595x.2008.tb00351.x. [DOI] [PubMed] [Google Scholar]
- 11.Emshoff R, Bösch R, Pümpel E, Schöning H, Strobl H. Low-level laser therapy for treatment of temporomandibular joint pain: A double-blind and placebo-controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:452–6. doi: 10.1016/j.tripleo.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 12.Venancio Rde A, Camparis CM, Lizarelli Rde F. Low intensity laser therapy in the treatment of temporomandibular disorders: A double-blind study. J Oral Rehabil. 2005;32:800–7. doi: 10.1111/j.1365-2842.2005.01516.x. [DOI] [PubMed] [Google Scholar]
- 13.Öz S, Gökçen-Röhlig B, Saruhanoglu A, Tuncer EB. Management of myofascial pain: Low-level laser therapy versus occlusal splints. J Craniofac Surg. 2010;21:1722–8. doi: 10.1097/SCS.0b013e3181f3c76c. [DOI] [PubMed] [Google Scholar]
- 14.Kulekcioglu S, Sivrioglu K, Ozcan O, Parlak M. Effectiveness of low-level laser therapy in temporomandibular disorder. Scand J Rheumatol. 2003;32:114–8. doi: 10.1080/03009740310000139. [DOI] [PubMed] [Google Scholar]
- 15.Bjordal JM, Couppé C, Chow RT, Tunér J, Ljunggren EA. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother. 2003;49:107–16. doi: 10.1016/s0004-9514(14)60127-6. [DOI] [PubMed] [Google Scholar]


