Abstract
Context:
Evaluation of Maxillofacial fractures in hilly region of Garhwal Himalyas and its relation with age, gender, anatomical location, seasonal variation and treatment provided.
Aims:
The aim of the present study is to analyze the pattern of maxillofacial fractures in the Garhwal Himalayan region of India and to compare the results with similar studies in India and the rest of the world.
Settings and Design:
This was a prospective study conducted on 102 patients with 128 facial fractures.
Materials and Methods:
This study was conducted on 102 patients who were admitted for the treatment of maxillofacial fractures in the Department of Dentistry at Government Medical College, Srinagar, Uttarakhand, India.
Statistical Analysis Used:
All analyses were performed using Chi-square test and level of significance.
Results:
Peak incidence was noted in the second to fourth decades of life. Male: female ratio was 4:1. Road traffic accident was the main etiology (42.2%), followed by fall (37.2%) and assault (11.8%). Among other etiology of injury, distinguishing feature was bear bite, which was only seen in winters causing 5.9% of total injury. Fall was reported high in females whereas road traffic accident in males. Mandible was fractured in 73.5% of patients while mid-face in 26.5% of patients. Open reduction with internal fixation was the choice of treatment in 60.8% of cases. Nearly 79.4% of patients were treated under local anesthesia. The mean duration of hospitalization was (standard deviation 5.2 days) 5.3 days.
Conclusions:
Road traffic accidents still remain the main cause of maxillofacial fractures in developing countries such as India. In hilly area, road traffic accident can be minimized by better wide roads with guide walls/parapet, strict law enforcement for overspeed, overload, and to use seat belts while driving, and use of helmet while riding two-wheeler. Open reduction internal fixation remains the first choice of treatment in facial fractures due to early return of function with minimal morbidity and better nutritional status in patients compared to closed reduction.
Keywords: Mandibular fractures, maxillofacial fractures, mid-face trauma, open reduction internal fixation, road traffic accident
Introduction
In surgical terms, trauma may be defined as a physical force which results in injury.[1] Maxillofacial injury simply means trauma to the middle third of facial skeleton and/or mandible including soft-tissue injury. The maxillofacial region is the most exposed part of the body and is prone to injury.[2] Maxillofacial injuries can occur as an isolated injury or may be associated with multiple injuries to the head, chest, abdominal, spinal, and extremities,[3,4] along with psychological trauma.[5,6,7] There are many reports about pattern of facial fractures in the literature from different countries[8] such as England,[9] Finland,[10] Italy,[11] India,[2,12,13,14,15,16,17,18,19] Japan,[20,21] Nigeria,[22] New Zealand,[23] Poland,[24] Pakistan,[25] Bulgaria,[26] and the United States.[27] Maxillofacial injuries vary between and within countries and depend on socioeconomic status, traffic standards, and topography of that area. Etiology of facial injury changed from the last four decades.[2] In Europe, assault and fall were the main causes of facial fractures,[28] while in Asia and Africa, still road accidents are the main cause.[12,13,20,21,22,25,29] Indian studies from various states show road traffic accident being the leading cause,[2,12,13,14,15,16,17,18] except a study from New Delhi showed the assault.[19] Due to different Terrain in Himalayan region, maxillofacial injuries are predominately due to road traffic accident (mainly vehicle fall from hill not collision). Assault, fall from cliff or tree while gathering firewood or grass for cattle, animal bite (mainly bear bite and leopard bite) less commonly are due to sports injury and least due to industrial or war injury. Regional data collection on maxillofacial fracture is important as it allows the better management and prevention measures on that region.[30] No prospective study has ever been reported about general maxillofacial complex fracture from this region. The purpose of this article was to analyze the pattern of maxillofacial fractures in this part of India and compare the results with similar studies in India and the rest of the world.
Materials and Methods
Hemwati Nandan Bahuguna is a base teaching hospital for Veer Chandra Singh Garhwali Government Medical College, Srinagar, Uttarakhand. It is the only government tertiary care referral hospital covering greater part of Garhwal Himalayan region. All 102 patients who were admitted for the treatment of facial fracture from February 2013 to June 2016 in the Department of Dentistry were included in this study. Patients with soft-tissue injury, patients with neurosurgical component who were referred by emergency department to higher center, and patients who refused treatment at our center were excluded from the study. Patients who were dead before treatment were not included. Diagnosis was made clinically and confirmed radiographically and finding at surgery. Facial fractures were classified as panfacial, Le Fort for midfacial region, and according to Ivy for mandibular fracture.[31,32] Data about age, gender, etiology, anatomical location, seasonal variation, mode of treatment, type of anesthesia, duration of stay, and X-ray advised were recorded from inpatient department case sheet. Significance of finding was statically evaluated by Chi-square test.
Results
A total of 102 patients with 128 facial fractures were studied. In the present study, the age distribution of the patients ranged from 1.5 to 83 years (mean age in years 29.7 [standard deviation (SD) ±13.9]). Among these, majority cases 59 (57.8%) were in the second to fourth decades of life. About 80.4% of males and 19.6% of females constituted the study population. The majority of the patients 34 (33.3%) admitted in the year 2013. The maximum number of patients 30 (29.4%) seeked health care in April to June.
By etiology of injury, maximum number of patients injured due to road traffic accident, i.e., 43 patients (42.2%). Among road traffic accidents, two-wheeler was more common injuring 32 patients. Fall injuring 38 patients (37.3%) and assault 12 patients (11.8%) followed this. Among other etiology of injury, distinguishing feature was bear bite, which was only seen on winters causing 5.9% of total injury [Figure 1]. Among those who had bear bite injury, 4 (4.9%) patients were male whereas 2 (10.0%) were female. In males, the common cause of injury was road traffic accidents 37 (35.1%); whereas in females, it was fall 10 (50.0%). In patients aged 20–40 years, the common cause of injury was a road traffic accident 29 (37.3%). Compared to inpatients, less than 20 and more than 40 years reported fall 11 (50.0%) and 10 (47.6%), respectively, as the cause of injury. No significant difference of diagnosis of study patients by etiology of injury (P = 0.095), month of diagnosis (P = 0.280), and year of diagnosis (P = 0.269) was observed. There was no significant trend in the burden of patient accordingly to time in years in the present study.
Figure 1.
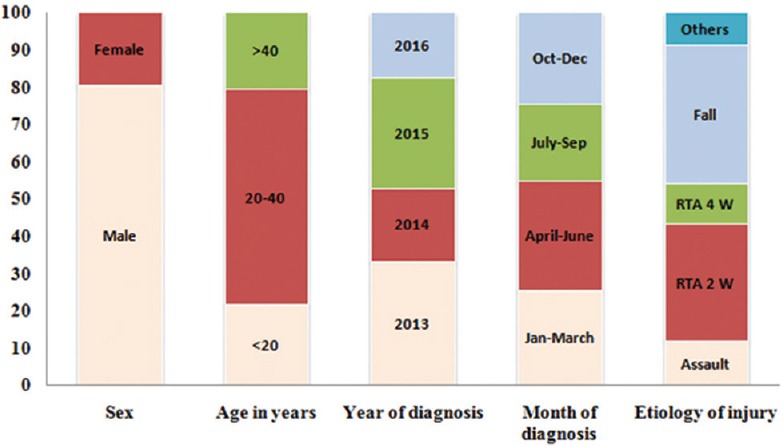
Demographic and presentation details of the study patients (n = 102)
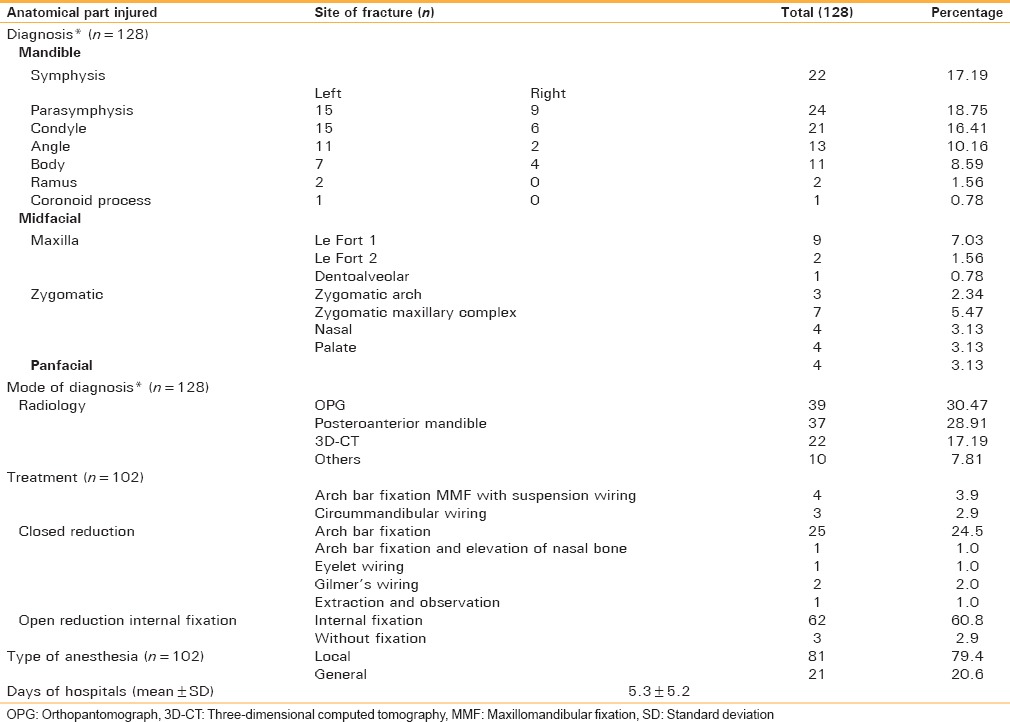
The majority of the patients presented with injury involving one or other part of the mandible. The most common diagnosis was fracture parasymphysis seen in 24 patients (18.75%), followed by fracture symphysis in 22 patients (17.19%), condyle 21 (16.41%), fracture angle 13 (10.16%). In mid-face region, maxillary Le Fort I (7.03%) was followed by zygomatic maxillary complex (5.47%) and others. Panfacial injury was present in 4 (3.13%) patients. The primary modality of diagnosis was radiology. Orthopantomograph and posterior-anterior view of the mandible X-ray were most common, comprising 39 (30.4%) and 37 (28.9%) patients, respectively. This was followed by three-dimensional computed tomography in 22 (17.2%) patients. Most of the study patients had undergone open reduction with internal fixation 62 (60.8) as the treatment modality followed by closed reduction with arch bar fixation 25 (24.5). Nearly 79.4% of patients were treated under local anesthesia. The mean duration of hospitalization was 5.3 (SD 5.2) days [Table 1].
Table 1.
Details of presenting diagnosis and treatment of the study patient (n=102) and site of fracture (n=128)
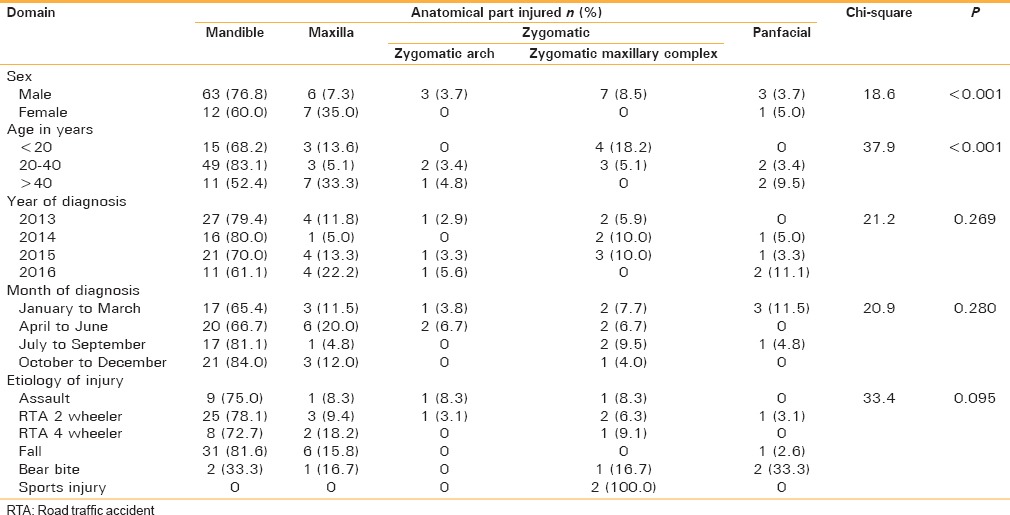
In males, most common diagnosis was fracture-involving mandible 63 (76.8%). In mandible, the most common involved site of injury was parasymphysis 18 (30.5%) Similarly, in females, the most commonly involved site was mandible 12 (60.0%), with the most common site of injury being condyle 6 (42.8%). There was a significant difference in morbidity pattern between adult males and females (P < 0.001). In adults (20–40 years), the most common diagnosis was fracture-involving mandible 49 (83.1%). The most common site of injury was parasymphysis in 16 (33.3%) patients. Among patients <20 years of age and more than 40 years of age, the commonly involved site of injury in the mandible was condyle 4 (44.4%) and angle 7 (43.7%), respectively. There was significant difference of diagnosis between >20, 20–40, and >40 years of age among study patients (P < 0.001) [Table 2].
Table 2.
Distribution of patients gender, age, year, month, and etiology of injury by primary diagnosis
Discussion
Epidemiologic survey will vary with geographical region, population density, socioeconomic status, culture, and regional government era in the time and type of facility, in which study was conducted.[13,30,33] In the present study, most commonly affected age group was between 20 and 40 years, whereas studies from other states of India such as Gujarat[2] Karnataka,[15,16] Haryana,[17] and Delhi[19] mentioned the age group between 21 and 30 years. International studies show the second to fourth decades life more commonly involved.[20,22,24,25,34] Age group of 20–40 years is the active phase of working life which demands to stay out of house for longer duration, travel more often, take more risks, indulge in interpersonal violence and adventure activity due to intense social interaction.
Demographic data of this region showed male predominance (ratio 4:1) which is near about similar to other studies from India.[2,12,13,14,15,16,17] Male predominance depends on the culture and socioeconomic status of that country. Studies from developed countries have lower ratio near about 2.1:1.[20,24,26,30] It can be explained due to females participating in social activities and are more susceptible to road traffic accident and violence.[33] Males were more commonly affected by road traffic accident (35.1%) whereas females fall from height (50%).
Road traffic accident is the major cause of maxillofacial injury in Himalayan region which accounts for 42.2%, which is slightly less compared to other states of India: Gujarat[2] 53%, Tamil Nadu[12] 62%, Goa[13] 76%, Karnataka[16] 74.7%, and Haryana[17] 71.8%. It is due to less vehicles and less traffic congestion in Himalayan region which leads to slightly less percentage road traffic accidents. In this terrain, road traffic accidents are due to poor road condition that is blind curves, slippery muddy road, in which driver lose control, and it accounts for fall of vehicle from mountain rather than collision. Some other causes of these accidents are overload, overspeed, and vehicles not up to date which causes brake fail and steering lock. Among road traffic accidents, two-wheeler is more common injuring 31% of patients as there is no strict law for helmet wearing in this region. In a study conducted in India, the highest incidence of 2-wheeled drive in road traffic accident is because young adults favor speedy bikes which run on poor roads without wearing helmet, leading to maxillofacial injury and head injury.[2] Age group from 20 to 40 years were more commonly affected by road traffic accident (37.3%).
In Garhwal Himalayan region, fall from height appears to be the second most etiological factor for maxillofacial fracture comprising 37.3%. This is similar to other studies from India.[12,15,17] Few international studies also reported fall as the second etiological factor.[20,22,25,34] Females were more prone to fall injury (50%) as they have to gather woods for cooking and grass for cattle, so they climb trees and cliff. Fall also showed bimodal age distribution less than 20 years and more than 40 years. It was high in the first decade of life as this group falls from roof, trees, and cliff while playing.
Assault in our study accounts for 11.8% only whereas a study from Delhi reported it the most common cause.[19] Other etiological factor bear bite (5.9%), which is mainly seen in this region of India during winter season, causes massive disfigurement of face and panfacial fractures; these encounters occur due to less food in winter when bear often visit the residential area of local inhabitants.
Most frequently, facial bone involved was the mandible which is similar to various studies across India;[2,12,13,15,16] this preponderance is due its anatomical position which is the most prominent, only movable facial bone, and inherent structural weakness, leading to greater chance of being fractured.[2,13] Parasymphysis fracture was the most common mandibular fracture accounting for 18.7%, which is similar to other Indian studies.[12,13,16,17] In our study, next common anatomical site involved was symphysis (17.9%). In midface, maxillary bone (9.3%) was more frequently involved than zygomatic bone (7.8%) similar to studies,[20,29] whereas other studies show zygomatic bone to be more frequently involved than maxilla.[12,13,15,16] Panfacial injury constitutes 3.9% only. Midfacial fractures are often associated with head injury and polytrauma which are treated or referred to higher centers; therefore, less incidence of midfacial fracture reported in our study.
In the past 15 years, treatment modality is influenced by innovation of new materials and technology which focus on early recovery, segment stability, and patient comfort.[33] Open reduction internal fixation is preferred than closed reduction in various centers in India.[15,16,17] Earlier studies from other countries preferred closed reduction.[20,22,34] The study from Nigeria states that developing countries still prefer closed reduction despite advantage of open fixation due to its cost-effectiveness.[22] In our center, 60.8% fractures were treated with open reduction internal fixation, followed by closed reduction with arch bar fixation (24.5%). Nearly 79.4% of patients were treated under local anesthesia which also includes open reduction, without any discomfort to patient, as local anesthesia is safer than general anesthesia. The mean duration of hospitalization was 5.3 (SD 5.2) days as patient kept on intravenous antibiotics and analgesics and sutures and intermaxillary fixation removed after 1 week as stated by Steinhauser.[35] The use of miniplate in our center is facilitated by the government providing the material to the poor patients.
Higher incidence of maxillofacial fracture was reported during April to June due to tourist visit, pilgrimage travels take place for Hindus and Sikh going to their shrines. People in Himalayan region are indulged in various activities such as farming, wood chopping, and grass and herb gathering in this season as this is the cessation of winter which limits the activities. Other Indian study from Goa reported higher incidence in April to June and October to December due to tourist season.[13] Tamil Nadu state reported higher incidence in September and October, the monsoon season, due to poor visibility.[12] International studies from Poland[24] reported spring whereas study from Austria[30] reported winters for higher incidence. Seasonal variation can be seen due to different demographic location and even within the same country.
Conclusions
In India, road traffic accident still remains the major causes of facial fractures. Two-wheeler road traffic accidents affect mainly young males. In hilly terrain, road traffic accidents can be minimized by better wide roads, use of parapet or guide walls, modern technology in vehicles on hill roads such as antilock braking system and hill assist to prevent slipping on roads. Strict laws for overspeed and overload and to use seat belts while driving and use of helmet while riding two-wheeler are required. Fall, the second most cause, in Garhwal Himalayan region which mainly affects female population, can be reduced only when better facility will be available to villages, such as use of cooking gas rather than wood, establishment of government fodder shops for cattle rather than grass fetching from the jungle.
In the present scenario, open reduction internal fixation remains the choice of treatment considering good fracture reduction and early functional outcomes, promotes the patient's oral health-related quality of life, and minimizes any masticatory disability resulting from prolonged immobilization of the jaws, thus better nutritional status compared to closed reduction.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Thomas DW, Hill CM. In: Etiology and changing patterns of maxillofacial trauma. Maxillofacial Surgery. 1st ed. Ward Booth P, editor. Vol. 1. London: Churchill Livingstone; 1999. pp. 1–10. [Google Scholar]
- 2.Weihsin H, Thadani S, Agrawal M, Tailor S, Sood R, Langalia A, et al. Causes and incidence of maxillofacial injuries in India: 12-year retrospective study of 4437 patients in a tertiary hospital in Gujarat. Br J Oral Maxillofac Surg. 2014;52:693–6. doi: 10.1016/j.bjoms.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 3.Akama MK, Chindia ML, Macigo FG, Guthua SW. Pattern of maxillofacial and associated injuries in road traffic accidents. East Afr Med J. 2007;84:287–95. doi: 10.4314/eamj.v84i6.9539. [DOI] [PubMed] [Google Scholar]
- 4.Morris LM, Kellman RM. Complications in facial trauma. Facial Plast Surg Clin North Am. 2013;21:605–17. doi: 10.1016/j.fsc.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 5.De Sousa A. Psychological issues in oral and maxillofacial reconstructive surgery. Br J Oral Maxillofac Surg. 2008;46:661–4. doi: 10.1016/j.bjoms.2008.07.192. [DOI] [PubMed] [Google Scholar]
- 6.Auerbach SM, Laskin DM, Kiesler DJ, Wilson M, Rajab B, Campbell TA. Psychological factors associated with response to maxillofacial injury and its treatment. J Oral Maxillofac Surg. 2008;66:755–61. doi: 10.1016/j.joms.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Glynn SM, Shetty V, Elliot-Brown K, Leathers R, Belin TR, Wang J. Chronic posttraumatic stress disorder after facial injury: A 1-year prospective cohort study. J Trauma. 2007;62:410–8. doi: 10.1097/01.ta.0000231556.05899.b0. [DOI] [PubMed] [Google Scholar]
- 8.Afzelius LE, Rosén C. Facial fractures. A review of 368 cases. Int J Oral Surg. 1980;9:25–32. doi: 10.1016/s0300-9785(80)80003-2. [DOI] [PubMed] [Google Scholar]
- 9.Down KE, Boot DA, Gorman DF. Maxillofacial and associated injuries in severely traumatized patients: Implications of a regional survey. Int J Oral Maxillofac Surg. 1995;24:409–12. doi: 10.1016/s0901-5027(05)80469-2. [DOI] [PubMed] [Google Scholar]
- 10.Lindqvist C, Sorsa S, Hyrkäs T, Santavirta S. Maxillofacial fractures sustained in bicycle accidents. Int J Oral Maxillofac Surg. 1986;15:12–8. doi: 10.1016/s0300-9785(86)80005-9. [DOI] [PubMed] [Google Scholar]
- 11.Gerbino G, Roccia F, Benech A, Caldarelli C. Analysis of 158 frontal sinus fractures: Current surgical management and complications. J Craniomaxillofac Surg. 2000;28:133–9. doi: 10.1054/jcms.2000.0134. [DOI] [PubMed] [Google Scholar]
- 12.Subhashraj K, Nandakumar N, Ravindran C. Review of maxillofacial injuries in Chennai, India: A study of 2748 cases. Br J Oral Maxillofac Surg. 2007;45:637–9. doi: 10.1016/j.bjoms.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 13.Kumar GB, Dhupar V, Akkara F, Kumar SP. Patterns of maxillofacial fractures in Goa. J Oral Maxillofac Surg. 2015;14:138–41. doi: 10.1007/s12663-013-0583-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garg V, Singh H, Vij K. Trends of maxillofacial trauma at tertiary care hospital in rural area of Southern Punjab. J Indian Acad Forensic Med. 2012;34:49–51. [Google Scholar]
- 15.Naveen Shankar A, Naveen Shankar V, Hegde N, Sharma S, Prasad R. The pattern of the maxillofacial fractures – A multicentre retrospective study. J Craniomaxillofac Surg. 2012;40:675–9. doi: 10.1016/j.jcms.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 16.Kamath RA, Bharani S, Hammannavar R, Ingle SP, Shah AG. Maxillofacial trauma in central Karnataka, India: An outcome of 95 cases in a regional trauma care centre. Craniomaxillofac Trauma Reconstr. 2012;5:197–204. doi: 10.1055/s-0032-1322536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bali R, Sharma P, Garg A, Dhillon G. A comprehensive study on maxillofacial trauma conducted in Yamunanagar, India. J Inj Violence Res. 2013;5:108–16. doi: 10.5249/jivr.v5i2.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guruprasad Y, Hemavathy O, Giraddi G, Shetty JN. An assessment of etiological spectrum and injury characteristics among maxillofacial trauma patients of Government Dental College and Research Institute, Bangalore. J Nat Sci Biol Med. 2014;5:47–51. doi: 10.4103/0976-9668.127285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kapoor P, Kalra N. A retrospective analysis of maxillofacial injuries in patients reporting to a tertiary care hospital in East Delhi. Int J Crit Illn Inj Sci. 2012;2:6–10. doi: 10.4103/2229-5151.94872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tanaka N, Tomitsuka K, Shionoya K, Andou H, Kimijima Y, Tashiro T, et al. Aetiology of maxillofacial fracture. Br J Oral Maxillofac Surg. 1994;32:19–23. doi: 10.1016/0266-4356(94)90166-x. [DOI] [PubMed] [Google Scholar]
- 21.Iida S, Kogo M, Sugiura T, Mima T, Matsuya T. Retrospective analysis of 1502 patients with facial fractures. Int J Oral Maxillofac Surg. 2001;30:286–90. doi: 10.1054/ijom.2001.0056. [DOI] [PubMed] [Google Scholar]
- 22.Adebayo ET, Ajike OS, Adekeye EO. Analysis of the pattern of maxillofacial fractures in Kaduna, Nigeria. Br J Oral Maxillofac Surg. 2003;41:396–400. doi: 10.1016/s0266-4356(03)00165-7. [DOI] [PubMed] [Google Scholar]
- 23.Kieser J, Stephenson S, Liston PN, Tong DC, Langley JD. Serious facial fractures in New Zealand from 1979 to 1998. Int J Oral Maxillofac Surg. 2002;31:206–9. doi: 10.1054/ijom.2002.0208. [DOI] [PubMed] [Google Scholar]
- 24.Malara P, Malara B, Drugacz J. Characteristics of maxillofacial injuries resulting from road traffic accidents – A 5 year review of the case records from department of maxillofacial surgery in Katowice, Poland. Head Face Med. 2006;2:27. doi: 10.1186/1746-160X-2-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheema SA, Amin F. Incidence and causes of maxillofacial skeletal injuries at the Mayo Hospital in Lahore, Pakistan. Br J Oral Maxillofac Surg. 2006;44:232–4. doi: 10.1016/j.bjoms.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 26.Deliverska E, Rubiev M. Patterns of maxillofacial injuries in University Hospital ‘St. Anna’, Sofia. J IMAB. 2012;18:150–2. [Google Scholar]
- 27.Laski R, Ziccardi VB, Broder HL, Janal M. Facial trauma: A recurrent disease. The potential role of disease prevention? J Oral Maxillofac Surg. 2004;62:685–8. doi: 10.1016/j.joms.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 28.Boffano P, Roccia F, Zavattero E, Dediol E, Uglešic V, Kovacic Ž, et al. European Maxillofacial Trauma (EURMAT) project: A multicentre and prospective study. J Craniomaxillofac Surg. 2015;43:62–70. doi: 10.1016/j.jcms.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 29.Bamjee Y, Lownie JF, Cleaton-Jones PE, Lownie MA. Maxillofacial injuries in a group of South Africans under 18 years of age. Br J Oral Maxillofac Surg. 1996;34:298–302. doi: 10.1016/s0266-4356(96)90006-6. [DOI] [PubMed] [Google Scholar]
- 30.Gassner R, Tuli T, Hächl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: A 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003;31:51–61. doi: 10.1016/s1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 31.Banks P. Killey's Fractures of the Middle Third of the Facial Skeleton. 4th ed. Mumbai: Varghese Publishing House; 1993. [Google Scholar]
- 32.Banks P. Killey's Fractures of the Mandible. 4th ed. Mumbai: Varghese Publishing House; 1993. [Google Scholar]
- 33.Brasileiro BF, Passeri LA. Epidemiological analysis of maxillofacial fractures in Brazil: A 5-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:28–34. doi: 10.1016/j.tripleo.2005.07.023. [DOI] [PubMed] [Google Scholar]
- 34.Motamedi MH. An assessment of maxillofacial fractures: A 5-year study of 237 patients. J Oral Maxillofac Surg. 2003;61:61–4. doi: 10.1053/joms.2003.50049. [DOI] [PubMed] [Google Scholar]
- 35.Steinhauser EW. Bone screws and plates in orthognathic surgery. Int J Oral Maxillofac Surg. 1982;11:573. doi: 10.1016/s0300-9785(82)80069-0. [DOI] [PubMed] [Google Scholar]


