Abstract
Background and Purpose
Neonatal hypoxic-ischemic encephalopathy (HIE) is one of the leading causes of neurological handicap in developing countries. Human umbilical cord blood (hUCB) CD34-positive (CD34+) stem cells exhibit the potential for neural repair. We tested the hypothesis that hUCB CD34+ stem cells and other cell types [leukocytes and nucleated red blood cells (NRBCs)] that are up-regulated during the acute stage of perinatal asphyxia (PA) could play a role in the early prediction of the occurrence, severity, and mortality of HIE.
Methods
This case-control pilot study investigated consecutive neonates exposed to PA. The hUCB CD34+ cell count in mononuclear layers was assayed using a flow cytometer. Twenty full-term neonates with PA and 25 healthy neonates were enrolled in the study.
Results
The absolute CD34+ cell count (p=0.02) and the relative CD34+ cell count (CD34+%) (p<0.001) in hUCB were higher in the HIE patients (n=20) than the healthy controls. The hUCB absolute CD34+ cell count (p=0.04), CD34+% (p<0.01), and Hobel risk scores (p=0.04) were higher in patients with moderate-to-severe HIE (n=9) than in those with mild HIE (n=11). The absolute CD34+ cell count was strongly correlated with CD34+% (p<0.001), Hobel risk score (p=0.04), total leukocyte count (TLC) (p<0.001), and NRBC count (p=0.01). CD34+% was correlated with TLC (p=0.02).
Conclusions
hUCB CD34+ cells can be used to predict the occurrence, severity, and mortality of neonatal HIE after PA.
Keywords: full-term neonates, Hobel risk score, mononuclear layer, perinatal asphyxia, stem cells, Thompson score
INTRODUCTION
With a reported incidence of 1.5–6 per 1,000 live births, neonatal hypoxic-ischemic encephalopathy (HIE) remains one of the leading causes of neonatal mortality, morbidity, and permanent neurological and neurodevelopmental disability in developing countries.1,2 Predicting the occurrence and short-term outcome in neonates with HIE is particularly important for initiating and monitoring appropriate management.3 This has become even more important with the current availability of effective neuroprotective strategies such as therapeutic hypothermia and the administration of nerve growth factor.4,5,6 This may prove even more valid with the envisioned use of other, mainly pharmacological neuroprotective agents and strategies.7 Several clinical, laboratory, electrophysiological, and imaging measures have been used to predict the coincident and subsequent potential brain damage with the aim of developing decisive prognostic criteria.8 Scoring systems to help predict death and disability have been subjected to continual stringent assessment and validation.9 However, this has not been the case for acute-stage parameters predictive of occurrence and short-term outcomes.10
Many studies have attempted to assess laboratory markers−alone or in combination with other laboratory and/or clinical parameters−as possibly useful predictors for perinatal asphyxia (PA), HIE, and neurodevelopmental outcomes. However, none of these markers has been demonstrated to be effective in clinical settings.11,12,13
The findings of clinical studies suggest that human umbilical cord blood (hUCB) CD34-positive (CD34+) stem cells could be used in neural repair.14 Since these cells are up-regulated during the acute stage of PA, we hypothesized that they could be utilized in the early prediction of HIE and its severity.
METHODS
Participants
Forty-five singleton full-term neonates with a gestational age of ≥37 weeks and delivered in the Maternity Hospital of Ain Shams University were enrolled from May 2013 to June 2014. Enrollment decisions made for patients who were delivered and required resuscitation that lasted up to 10 minutes, hUCB samples collected.
Risk assessments were performed based on the Hobel score. This score measures morbidity in the normal-weight infant, and consists of 3 components encompassing 126 factors that include morbid conditions or signs and symptoms of morbidity, prenatal, labor/delivery, and neonatal factors, and a total risk score. Each factor is assigned a weight of 1, 5, or 10. The prenatal component consists of 51 items, the labor/delivery component consists of 40 items, and the neonatal component consists of 35 factors.15
Sarnat staging16 was used to classify HIE into stage I (mild) or stages II and III (moderate and severe). Thompson scoring17 was used for grading HIE. This staging scale consists of consecutive daily assessments of neurological features (tone, level of consciousness, seizures, and posture), neonatal reflexes (Moro, sucking, and grasping), respiration, and the anterior fontanel. The maximum score is 22, with scores of 1–10, 11–14, and 15–22 indicating mild, moderate, and severe HIE, respectively.
Eligibility criteria
The study involved term neonates with birth asphyxia that subsequently led to the development of HIE. PA was defined as a pH of ≤7.0 and/or a base deficit of ≥16 mmol/L in a venous or arterial hUCB sample obtained at birth, or in any peripheral (capillary, venous, or arterial) blood sample obtained within the first hour after birth. If the pH was 7.01–7.15 and/or the base deficit was 10–15.9 mmol/L, the following additional criteria were used to define PA: a 10-minute Apgar score of 5 or less, and extended resuscitation with or without assisted ventilation at birth that continued for a minimum of 10 minutes.18
In addition to the electrophysiological signs of encephalopathy (e.g., seizure and/or abnormal amplitude-integrated electroencephalogram),19 clinical signs of encephalopathy needed to be present in at least three of the following six categories: level of consciousness, spontaneous motor activity, tone, posture, primitive reflexes (Moro and sucking), and autonomic nervous system dysfunction.20
The control group comprised 25 healthy term neonates with an appropriate weight for the gestation age who exhibited an Apgar score of ≥8 at 5 minutes, no indication of fetal distress, and normal findings in hUCB gas analysis.
Exclusion criteria
Neonates with congenital (CNS or other) anomalies, or chromosomal abnormalities, multiple pregnancy, or those whose parents refused enrollment were all excluded.
Study design
This is a prospective case-control pilot study aiming to correlate the incidence and severity of disease in HIE patients with hUCB CD34+ cell counts as assessed by flow cytometry, as well as the total leukocyte count (TLC) and nucleated red blood cell (NRBC) count, in comparison with control subjects. The correlation in the HIE patients was assessed based on risk scores (Hobel) and neurological (Sarnat and Thompson) severity scores.
Following delivery and before the placenta was separated, the umbilical cord was double-clamped and dissected. The umbilical vein was disinfected using Betadine solution in vaginal deliveries and then aseptically punctured with a sterile syringe to collect 10 mL of its blood in a 14-mL sterile Falcon tube containing 2 mL of citrate phosphate dextrose as an anticoagulant. Samples were transported to the laboratory within 12 hours.21
The hUCB complete blood count, TLC, NRBC count, and CD34+ cell count were measured using anti-CD34 monoclonal antibodies for all of the included cases. The number of NRBCs per 100 white blood cells (WBCs) was counted in an hUCB smear stained with Wright's stain.22
CD34 assay
Low-density mononuclear (LDMN) cells were extracted using Ficoll-Hypaque density gradient separation. The samples were diluted at a ratio of 1:2 with phosphate-buffered saline (PBS), and then the suspension was laid on Ficoll-Hypaque media (density=1,077 g/mL) at 2:1 and centrifuged for 20 minutes at 1,200 rpm and 28℃. LDMN cells were recovered from the gradient interface, washed twice with PBS, and the pellets were resuspended in 1 mL of PBS.23
A mononuclear layer of CD34+ cells was double stained with anti-CD34 monoclonal antibodies conjugated with phycoerythrin and anti-CD45 (leukocyte common antigen) conjugated with fluorescein isothiocyanate. The number of LDMN cells in each sample was counted using a Coulter automated cell counter, with the cell count adjusted to 5–10×106 cells/mL. Flow cytometric analysis was then performed (EPICS-XL, Coulter, FL, USA).24
Ethical approval
The study was approved by the Ethics Committee of the Pediatric Department, Children's Hospital, Ain Shams University. Informed parental consent was obtained.
Statistical analysis
The SPSS statistical software package (version 18.0, IBM Corporation, Armonk, NY, USA) was used for data analysis. Data are presented as mean±SD, n (%), and median (range) values. The quantitative variables were analyzed using the Mann-Whitney U test for comparisons involving two independent groups of nonparametric data, Student's t-test for comparing two independent parametric samples, and the Spearman correlation test to study the associations between parameters. The cutoff for statistical significance was set at p≤0.05.
RESULTS
The data of 45 full-term neonates were analyzed, of which 20 fulfilled the criteria for PA and HIE (14 males and 6 females, 15 delivered by cesarean section (CS) and 5 delivered vaginally). On the Sarnat staging system, 11 of these 20 neonates were stage I (mild HIE) and 9 were stages II and III (moderate-to-severe HIE). Twenty-five healthy term neonates with appropriate weights for the gestation ages who had not suffered any degree of PA (13 males and 12 females, 13 delivered by CS and 12 delivered vaginally) were recruited as controls. The median Hobel risk scores were higher for the HIE patients than the healthy controls: prenatal (50 vs. 45), labor/delivery (30 vs. 10), neonatal (14 vs. 8), and total (94 vs. 77). The median Thompson score was higher for HIE infants than for the controls (12 vs. 4) (Table 1).
Table 1. Demographic and clinical characteristics in the HIE and control groups.
| Characteristic | HIE (n=20) | Control (n=25) | p |
|---|---|---|---|
| Birthweight (kg) | 3.25±0.52 | 3.21±0.37 | 0.42 |
| Gestational age (weeks) | 40 | 38 (37–41) | 0.6 |
| Sex (%) | 0.22 | ||
| Male | 14 (70) | 13 (52) | |
| Female | 6 (30) | 12 (48) | |
| Mode of delivery (%) | 0.11 | ||
| Vaginal | 5 (25) | 12 (48) | |
| Cesarean section | 15 (75) | 13 (52) | |
| Apgar score | |||
| 1 minute | 2 (0–6) | 7 (6–9) | <0.0001 |
| 5 minutes | 4 (0–6) | 8 (7–10) | <0.0001 |
| 10 minutes | 5 (0–6) | 9 (8–10) | <0.0001 |
| Hobel risk score* | |||
| Prenatal | 55 | 40 | 0.03 |
| Labor/delivery | 30 | 9 | 0.01 |
| Neonatal | 15 | 7 | 0.02 |
| Total | 100 | 56 | 0.001 |
| Thompson score | 12 | 4 | 0.01 |
Data are mean±SD, n (%), or median (range) values.
*chi-sqare test used for comparison.
HIE: hypoxic-ischemic encephalopathy
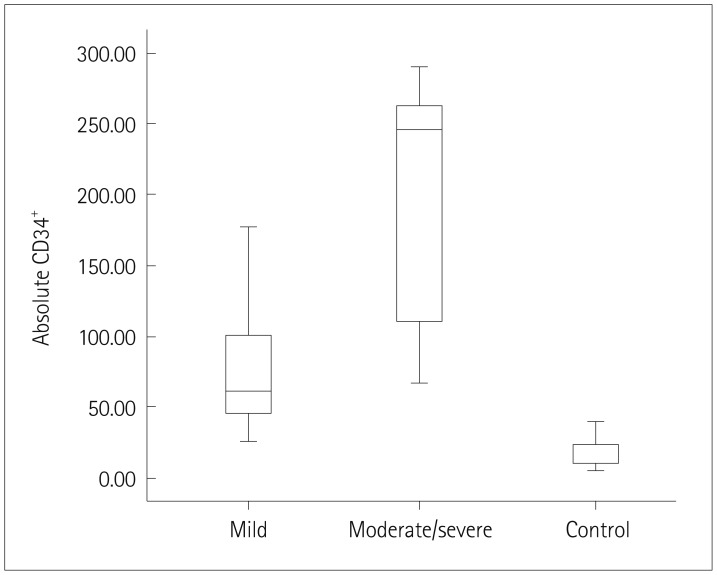
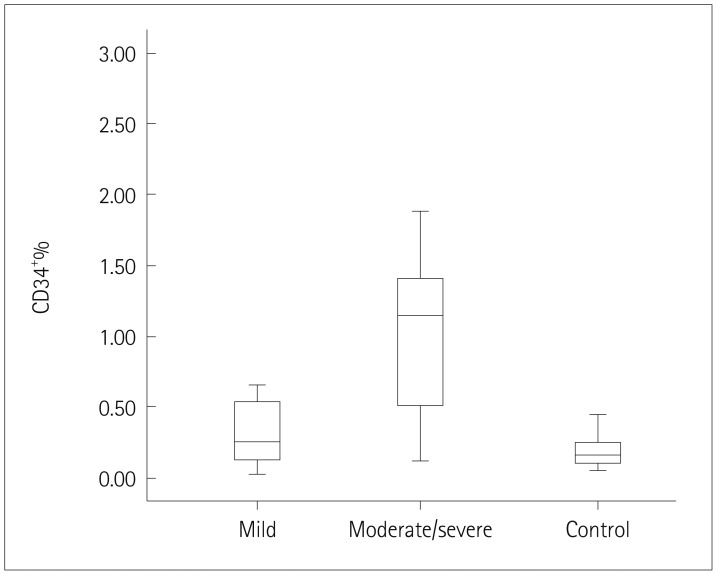
The absolute CD34+ cell count (p=0.02), relative CD34+ cell count (CD34+%) (p<0.001), TLC (p=0.01), and NRBC count (p=0.02) were significantly higher in HIE patients than in healthy controls (Table 2) (Figs. 1 and 2).
Table 2. hUCB parameters in the HIE and control groups.
| Parameter | HIE (n=20) | Control (n=25) | p | ||
|---|---|---|---|---|---|
| Absolute CD34+ cell count (cells/μL) | 95.12±105.26 | 53.00 (45.85, 144.38) | 20.40±27.32 | 10.50 (6.16, 34.64) | 0.02† |
| CD34+% | 0.68±0.71 | 0.49 (0.35, 1.02) | 0.18±0.11 | 0.16 (0.13, 0.23) | <0.001† |
| TLC (×109 cells/L) | 12.12±6.83 | 8.2±3.4 | 0.01* | ||
| NRBCs (cells/100 WBCs) | 30.55±19.34 | 5.70±3.16 | 0.02* | ||
Values are mean±SD or median (confidence interval) values.
*t-test, †Mann-Whitney U test.
CD34+: CD34-positive, CD34+%: relative CD34+ cell count. HIE: hypoxic-ischemic encephalopathy, hUCB: human umbilical cord blood, NRBCs: nucleated red blood cells, TLC: total leukocyte count, WBC: white blood cell.
Fig. 1. hUCB absolute CD34-positive (CD34+) cell count at birth in all of the studied neonates. hUCB: human umbilical cord blood.
Fig. 2. hUCB relative CD34+ cell count (CD34+%) at birth in all of the studied neonates. hUCB: human umbilical cord blood.
Patients with moderate-to-severe HIE had a higher absolute CD34+ cell count (p=0.04), CD34+% (p=0.01). TLC (p=0.02), and NRBC count (p=0.001) compared to those with mild HIE (Table 3). Of the 20 HIE neonates, 5 (25%) died between postnatal days 7 and 38 (moderate-to-severe disease), while 15 (75%) survived. The absolute CD34+ cell count (p<0.0001) and CD34+% (p<0.0001) were significantly higher in the HIE patients who died than in those who survived (Table 4). The Hobel risk score and the Thompson staging score were not correlated with CD34+% (p=0.81 and 0.349, respectively) and were marginal correlated with the absolute CD34+ cell count (p=0.04 for each), whereas the hUCB TLC was correlated with both CD34+% (p=0.02) and the absolute CD34+ cell count (p<0.001), and the hUCB NRBC count was correlated with the absolute CD34+ cell count (p=0.01) but not CD34+% (p=0.187). A statistically significant positive linear correlation was found between the absolute CD34+ cell count and CD34+% (p<0.001) (Table 5).
Table 3. hUCB parameters according to HIE severity.
| Mild HIE (n=11) | Moderate-to-severe HIE (n=9) | p | |||
|---|---|---|---|---|---|
| Absolute CD34+ cell count (cells/μL) | 76.56±42.40 | 60.00 (59.10, 94.10) | 186.43±93.25 | 245.10 (114.76, 258.11) | 0.04† |
| CD34+% | 0.32±0.41 | 0.25 (0.16, 0.47) | 1.13±0.85 | 1.14 (0.84, 1.79) | 0.01† |
| TLC (×109) | 12.17±8.47 | 12.80±6.41 | 0.02* | ||
| NRBCs (cells/100 WBCs) | 14.73±6.91 | 37.56±18.24 | 0.001* | ||
Values are mean±SD or median (confidence interval) values.
*t-test, †Mann-Whitney U test, p is significant if ≤0.05.
CD34+: CD34-positive, CD34+%: relative CD34+ cell count, HIE: hypoxic-ischemic encephalopathy, hUCB: human umbilical cord blood, NRBCs: nucleated red blood cells, TLC: total leukocyte count, WBC: white blood cell.
Table 4. hUCB parameters of HIE patients who died vs. survived.
| Parameter | Died (n=5) | Survived (n=15) | p | ||
|---|---|---|---|---|---|
| Absolute CD34+ cell count (cells/μL) | 263.40±18.12 | 261.8 (240.9, 285.9) | 39.03±38.25 | 14.7 (17.85, 60.22) | <0.0001† |
| CD34+% | 1.69±0.72 | 1.4 (0.79, 2.59) | 0.35±0.24 | 0.33 (0.22, 0.48) | <0.0001† |
| TLC (×109) | 13.02±7.92 | 11.45±6.15 | 0.04* | ||
| NRBCs (cells/100 WBCs) | 3.60±3.05 | 12.87±15.12 | 0.20* | ||
Values are mean±SD or median (confidence interval) values.
*t-test, †Mann-Whitney U test with z, p is significant if ≤0.05.
CD34+: CD34-positive, CD34+%: relative CD34+ cell count, HIE: hypoxic-ischemic encephalopathy, hUCB: human umbilical cord blood, NRBCs: nucleated red blood cells, TLC: total leukocyte count, WBC: white blood cell.
Table 5. Relationship between maternal and neonatal factors and CD34+ cell counts of HIE patients.
| Factor | CD34+% | Absolute CD34+ cell count (cells/μL) |
|---|---|---|
| p | p | |
| Hobel risk score | 0.81 | 0.04 |
| Birthweight (kg)* | 0.08 | 0.21 |
| Thompson score | 0.349 | 0.04 |
| hUCB TLC (×109 cells/L) | 0.02 | <0.001 |
| hUCB NRBCs (cells/100 WBCs) | 0.187 | 0.01 |
| CD34+% | - | <0.001 |
*Spearman's rank-order correlation test, p is significant if ≤0.05.
CD34+: CD34-positive, CD34+%: relative CD34+ cell count, HIE: hypoxic-ischemic encephalopathy, hUCB: human umbilical cord blood, NRBCs: nucleated red blood cells, TLC: total leukocyte count, WBC: white blood cell.
DISCUSSION
This study counted hUCB-derived hematopoietic stem/progenitor CD34+ cells in neonates who had experienced fetal distress and PA that subsequently developing into varying grades of HIE (dichotomized into mild and moderate to severe) and mortality toward the end of the neonatal period. The hUCB absolute CD34+ cell count and CD34+% were strongly correlated with the occurrence, severity, and mortality of HIE, indicating that these cells are useful for predicting the short-term outcome of the disease. hUCB CD34+ cell counts were significantly higher in HIE patients than controls, in moderate-to-severe cases than in mild cases, and in HIE neonates who died during the neonatal period (1–4 weeks after delivery) than in those who survived.
CD34 is a widely used marker of hematopoietic and endothelial progenitor cells. The density of CD34+ mononuclear cells is 10-fold higher in hUCB than in adult peripheral blood.25 The proportion of CD34+ cells in hUCB ranges from 0.3% to 2.4%, which is comparable to that of the bone marrow.26 CD34+ cells are less abundant in neonatal peripheral blood immediately postpartum than in hUCB, and their abundance tends to decrease within the first 48 hours after delivery.27
Apart from their hematopoietic properties, hUCB cells exert myriad effects. Human CD34+ cells secrete numerous cytochemokines and growth factors, including vascular endothelial growth factor.28 The basic concept underlying the intravenous administration of autologous hUCBs for neonatal encephalopathy is to replenish stem cells in the systemic circulation, which may contribute to neuroprotection and/or enhance cerebral plasticity.29,30
The findings of both animal and in vitro studies suggest that intrapartum fetal hypoxia stimulates erythropoiesis by provoking a cascade of events that engage erythropoietic elements, with the ultimate aim of compensating for the diminished oxygen capacity of hemoglobin. This results in the up-regulation of blood-forming cells, including WBCs, immature red blood cells, and hematopoietic CD34+ cells.31 Increases in CD34+ cell counts have been observed on day 7 after both traumatic brain injury and chest trauma.32
The intravenous administration of human hUCB CD34+ cells was found to reduce histological ischemic brain damage in mice after neonatal stroke, with a transient increase in the cerebral blood flow in the peri-infarct area forty-eight hours after permanent occlusion of the left middle cerebral artery.29
In addition, the administration of autologous hUCB cells is feasible in neonates with HIE.33 Aly et al.34 found that neural differentiation was strongest in cells derived from HIE term neonates, of which 69% exhibited complete and 31% exhibited partial neural differentiation.
PA-related stress might trigger mobilization of stem/progenitor-enriched CD34+ cells from the placenta into the hUCB, which could subsequently contribute to the regeneration of damaged tissues.35 Moreover, hypoxia is effective at maintaining the biological characteristics of CD34+ cells through suppressing the level of intracellular reactive oxygen species by regulating NADPH oxidase.36 However, whether asphyxia induces peripheral blood stem cells to differentiate into neural cells has not been reported previously.37 The increased WBC and NRBC counts in our patients are consistent with this. However, there might be a considerable delay between the occurrence of hypoxia and the release of NRBCs, and this might also apply to CD34+ cells.38
We found a significantly higher WBC and NRBC counts in conjunction with hUCB CD34+ cells. Our results add to the growing body of evidence against the predictive value of clinical parameters for short- or even long-term outcomes, especially during the first few hours after birth.
Study limitations
This study represent preliminary research that did not have sufficient statistical power to comprehensively identify mechanisms or assess different variables related to neonatal HIE. One of the main limitations was that the study was not designed to differentiate acute from chronic fetal distress leading to PA/HIE syndrome. This is particularly relevant when commenting on the timing and duration of an insult that could have triggered the cascade leading to encephalopathy.
Like many other markers of PA/HIE, hUCB CD34+ cells are induced after global hypoxia. Although they showed a strong relation with subsequent encephalopathy in our study, whether they are only or mainly induced by cerebral hypoxia remains unclear, and so further studies should investigate this.
Considering that HIE may evolve into further deterioration or improvement, the hUCB CD34+ cell count represents a single-point (snapshot) valuation that cannot be followed up or help in assessing the disease progression. The hUCB WBC count was strongly correlated with CD34+% (p=0.02) and (especially) the absolute CD34+ cell count (p<0.001), while the hUCB NRBC count was correlated with the absolute CD34+ cell count (p<001) but not with CD34+% (p=0.187). Whether utilizing CD34+ cells and NRBCs alone or in combination would provide a better predictor of HIE is a possibility that we did not explore.
Footnotes
Conflicts of Interest: The authors have no conflict of interest to declare.
References
- 1.Lee AC, Kozuki N, Blencowe H, Vos T, Bahalim A, Darmstadt GL, et al. Intrapartum-related neonatal encephalopathy incidence and impairment at regional and global levels for 2010 with trends from 1990. Pediatr Res. 2013;74(Suppl 1):50–72. doi: 10.1038/pr.2013.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Itoo BA, Al-Hawsawi ZM, Khan AH. Hypoxic ischemic encephalopathy, Incidence and risk factors in North Western Saudi Arabia. Neurosciences (Riyadh) 2003;8:113–119. [PubMed] [Google Scholar]
- 3.Dixon BJ, Reis C, Ho WM, Tang J, Zhang JH. Neuroprotective strategies after neonatal hypoxic ischemic encephalopathy. Int J Mol Sci. 2015;16:22368–22401. doi: 10.3390/ijms160922368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.El Shimi MS, Awad HA, Hassanein SM, Gad GI, Imam SS, Shaaban HA, et al. Single dose recombinant erythropoietin versus moderate hypothermia for neonatal hypoxic ischemic encephalopathy in low resource settings. J Matern Fetal Neonatal Med. 2014;27:1295–1300. doi: 10.3109/14767058.2013.855894. [DOI] [PubMed] [Google Scholar]
- 5.Serpero LD, Bellissima V, Colivicchi M, Sabatini M, Frigiola A, Ricotti A, et al. Next generation biomarkers for brain injury. J Matern Fetal Neonatal Med. 2013;26(Suppl 2):44–49. doi: 10.3109/14767058.2013.829688. [DOI] [PubMed] [Google Scholar]
- 6.Hassanein SM, Deifalla SM, El-Houssinie M, Mokbel SA. Safety and efficacy of cerebrolysin in infants with communication defects due to severe perinatal brain insult: a randomized controlled clinical trial. J Clin Neurol. 2016;12:79–84. doi: 10.3988/jcn.2016.12.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chalak LF, DuPont TL, Sánchez PJ, Lucke A, Heyne RJ, Morriss MC, et al. Neurodevelopmental outcomes after hypothermia therapy in the era of Bayley-III. J Perinatol. 2014;34:629–633. doi: 10.1038/jp.2014.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Horn AR, Swingler GH, Myer L, Linley LL, Raban MS, Joolay Y, et al. Early clinical signs in neonates with hypoxic ischemic encephalopathy predict an abnormal amplitude-integrated electroencephalogram at age 6 hours. BMC Pediatr. 2013;13:52. doi: 10.1186/1471-2431-13-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hayakawa M, Ito Y, Saito S, Mitsuda N, Hosono S, Yoda H, et al. Incidence and prediction of outcome in hypoxic-ischemic encephalopathy in Japan. Pediatr Int. 2014;56:215–221. doi: 10.1111/ped.12233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Menticoglou SM. How often do perinatal events at full term cause cerebral palsy? J Obstet Gynaecol Can. 2008;30:396–403. doi: 10.1016/s1701-2163(16)32824-9. [DOI] [PubMed] [Google Scholar]
- 11.Bhongir AV, Yakama AV, Saha S, Radia SB, Pabbati J. The urinary uric acid/creatinine ratio is an adjuvant marker for perinatal asphyxia. Eur J Pharm Med Res. 2015;2:520–528. [PMC free article] [PubMed] [Google Scholar]
- 12.Goel M, Dwivedi R, Gohiya P, Hegde D. Nucleated red blood cell in cord blood as a marker of perinatal asphyxia. J Clin Neonatol. 2013;2:179–182. doi: 10.4103/2249-4847.123097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aly H, Hassanein S, Nada A, Mohamed MH, Atef SH, Atiea W. Vascular endothelial growth factor in neonates with perinatal asphyxia. Brain Dev. 2009;31:600–604. doi: 10.1016/j.braindev.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 14.Reali C, Scintu F, Pillai R, Cabras S, Argiolu F, Ristaldi MS, et al. Differentiation of human adult CD34+ stem cells into cells with a neural phenotype: role of astrocytes. Exp Neurol. 2006;197:399–406. doi: 10.1016/j.expneurol.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 15.Hobel CJ, Youkeles L, Forsythe A. Prenatal and intrapartum high-risk screening. II. Risk factors reassessed. Am J Obstet Gynecol. 1979;135:1051–1056. doi: 10.1016/0002-9378(79)90735-x. [DOI] [PubMed] [Google Scholar]
- 16.Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol. 1976;33:696–705. doi: 10.1001/archneur.1976.00500100030012. [DOI] [PubMed] [Google Scholar]
- 17.Thompson CM, Puterman AS, Linley LL, Hann FM, van der Elst CW, Molteno CD, et al. The value of a scoring system for hypoxic ischaemic encephalopathy in predicting neurodevelopmental outcome. Acta Paediatr. 1997;86:757–761. doi: 10.1111/j.1651-2227.1997.tb08581.x. [DOI] [PubMed] [Google Scholar]
- 18.Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med. 2005;353:1574–1584. doi: 10.1056/NEJMcps050929. [DOI] [PubMed] [Google Scholar]
- 19.Denning-Kendall PA, Horsley H, Donaldson C, Bradley B, Hows JM. Different behaviour of fresh and cultured CD34+ cells during immunomagnetic separation. Br J Haematol. 1999;105:780–785. doi: 10.1046/j.1365-2141.1999.01397.x. [DOI] [PubMed] [Google Scholar]
- 20.van Laerhoven H, de Haan TR, Offringa M, Post B, van der Lee JH. Prognostic tests in term neonates with hypoxic-ischemic encephalopathy: a systematic review. Pediatrics. 2013;131:88–98. doi: 10.1542/peds.2012-1297. [DOI] [PubMed] [Google Scholar]
- 21.Surbek DV, Aufderhaar U, Holzgreve W. Umbilical cord blood collection for transplantation: which technique should be preferred? Am J Obstet Gynecol. 2000;183:1587–1588. doi: 10.1067/mob.2000.108985. [DOI] [PubMed] [Google Scholar]
- 22.Axt R, Ertan K, Hendrik J, Wrobel M, Mink D, Schmidt W. Nucleated red blood cells in cord blood of singleton term and post-term neonates. J Perinat Med. 1999;27:376–381. doi: 10.1515/JPM.1999.051. [DOI] [PubMed] [Google Scholar]
- 23.Mehrishi JN, Bakács T. A novel method of CD34+ cell separation from umbilical cord blood. Transfusion. 2013;53:2675–2680. doi: 10.1111/trf.12123. [DOI] [PubMed] [Google Scholar]
- 24.Sutherland DR, Anderson L, Keeney M, Nayar R, Chin-Yee I. The ISHAGE guidelines for CD34+ cell determination by flow cytometry. International Society of Hematotherapy and Graft Engineering. J Hematother. 1996;5:213–226. doi: 10.1089/scd.1.1996.5.213. [DOI] [PubMed] [Google Scholar]
- 25.Sidney LE, Branch MJ, Dunphy SE, Dua HS, Hopkinson A. Concise review: evidence for CD34 as a common marker for diverse progenitors. Stem Cells. 2014;32:1380–1389. doi: 10.1002/stem.1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al-Deghaither SY. Impact of maternal and neonatal factors on parameters of hematopoietic potential in umbilical cord blood. Saudi Med J. 2015;36:704–712. doi: 10.15537/smj.2015.6.11247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim JP, Lee YH, Lee YA, Kim YD. A comparison of the kinetics of nucleated cells and CD34+ cells in neonatal peripheral blood and cord blood. Biol Blood Marrow Transplant. 2007;13:478–485. doi: 10.1016/j.bbmt.2006.12.446. [DOI] [PubMed] [Google Scholar]
- 28.Liang CC, Liu HL, Chang SD, Chen SH, Lee TH. The protective effect of human umbilical cord blood CD34+ cells and estradiol against focal cerebral ischemia in female ovariectomized rat: cerebral MR imaging and immunohistochemical study. PLoS One. 2016;11:e0147133. doi: 10.1371/journal.pone.0147133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tsuji M, Taguchi A, Ohshima M, Kasahara Y, Sato Y, Tsuda H, et al. Effects of intravenous administration of umbilical cord blood CD34(+) cells in a mouse model of neonatal stroke. Neuroscience. 2014;263:148–158. doi: 10.1016/j.neuroscience.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 30.Boltze J, Reich DM, Hau S, Reymann KG, Strassburger M, Lobsien D, et al. Assessment of neuroprotective effects of human umbilical cord blood mononuclear cell subpopulations in vitro and in vivo. Cell Transplant. 2012;21:723–737. doi: 10.3727/096368911X586783. [DOI] [PubMed] [Google Scholar]
- 31.Haase VH. Regulation of erythropoiesis by hypoxia-inducible factors. Blood Rev. 2013;27:41–53. doi: 10.1016/j.blre.2012.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Elbuken G, Tanriverdi F, Karaca Z, Eser B, Hasdiraz L, Unluhizarci K, et al. Evaluation of peripheral blood CD34+ cell count in the acute phase of traumatic brain injury and chest trauma. Brain Inj. 2016;30:179–183. doi: 10.3109/02699052.2015.1090015. [DOI] [PubMed] [Google Scholar]
- 33.Cotten CM, Murtha AP, Goldberg RN, Grotegut CA, Smith PB, Goldstein RF, et al. Feasibility of autologous cord blood cells for infants with hypoxic-ischemic encephalopathy. J Pediatr. 2014;164:973–979.e1. doi: 10.1016/j.jpeds.2013.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aly H, Mohsen L, Badrawi N, Gabr H, Ali Z, Akmal D. Viability and neural differentiation of mesenchymal stem cells derived from the umbilical cord following perinatal asphyxia. J Perinatol. 2012;32:671–676. doi: 10.1038/jp.2011.174. [DOI] [PubMed] [Google Scholar]
- 35.Baburamani AA, Ek CJ, Walker DW, Castillo-Melendez M. Vulnerability of the developing brain to hypoxic-ischemic damage: contribution of the cerebral vasculature to injury and repair? Front Physiol. 2012;3:424. doi: 10.3389/fphys.2012.00424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fan J, Cai H, Tan WS. Role of the plasma membrane ROS-generating NADPH oxidase in CD34+ progenitor cells preservation by hypoxia. J Biotechnol. 2007;130:455–462. doi: 10.1016/j.jbiotec.2007.05.023. [DOI] [PubMed] [Google Scholar]
- 37.Dong W, Yuwen Z, Xiaohui G. The enhanced ability of peripheral mononuclear cells differentiating into neural cells in term infants with good improvement suffering from severe hypoxic ischemic encephalopathy. Iran J Pediatr. 2014;24:435–440. [PMC free article] [PubMed] [Google Scholar]
- 38.McCarthy JM, Capullari T, Thompson Z, Zhu Y, Spellacy WN. Umbilical cord nucleated red blood cell counts: normal values and the effect of labor. J Perinatol. 2006;26:89–92. doi: 10.1038/sj.jp.7211437. [DOI] [PubMed] [Google Scholar]