Abstract
Five hundred five blood cultures collected through a peripheral intravenous catheter (PIV) in an emergency department were matched to cultures obtained by dedicated venipuncture from the same patient within 10 minutes. The relative risk of contamination for cultures collected through PIVs compared with dedicated venipuncture was 1.83 (95% confidence interval, 1.08–3.11).
False-positive blood cultures due to specimen contamination with skin bacteria are common problems that lead to substantial patient morbidity, overuse of antibiotics, and increased costs.1–4 Blood culture specimens are frequently collected through peripheral intravenous catheters (PIVs).4,5 However, collecting cultures through PIVs rather than by dedicated venipuncture may lead to higher contamination rates due to the difficulty of adequately sterilizing a collection site in the presence of a catheter.6 The purpose of this study was to assess the risk of blood culture contamination associated with collecting specimens through PIVs compared with dedicated venipuncture in adult emergency department patients.
METHODS
We conducted a matched historical cohort study of blood cultures collected for clinical purposes between January 1 and December 31, 2009, in the adult emergency department of a university-affiliated hospital. The local institutional review board approved the study.
Throughout the study period, nurses and paramedics collected blood cultures by 2 methods—dedicated venipuncture and through PIVs. Dedicated venipuncture involved skin antisepsis with 2% chlorhexidine gluconate/70% isopropyl alcohol and specimen obtainment by placing a needle directly into a patient’s vein. Collection through a PIV involved skin antisepsis with 2% chlorhexidine gluconate/70% isopropyl alcohol prior to PIV placement, antisepsis of the catheter with 70% isopropyl alcohol, and drawing blood through the PIV. Blood was inoculated into aerobic and anaerobic bottles and processed on a BD BACTEC instrument. Nurses and paramedics were instructed not to use the needle-change technique.4 There were no systematic changes in specimen collection techniques during the study period.
Clinical personnel obtaining each culture determined which collection technique to use and documented it in the medical record. Using electronic medical record queries, we identified cultures obtained via a PIV in the emergency department and searched for cultures collected from the same patient within 10 minutes by dedicated venipuncture. Matched pairs of cultures—one collected by PIV and one by dedicated venipuncture—were used as the unit of analysis.
Results of each culture were classified as no growth, truly positive, or contaminated. Cultures without growth of bacteria or fungi were classified as no growth. Cultures that grew identical organisms compared with their matched partner were classified as true positives.
Cultures with results not identical to their matched partner were individually reviewed. Cultures growing organisms that do not typically cause skin contamination—gram-negative bacteria, anaerobic bacteria, fungi, Actinomyces species, Streptococcus pneumoniae, and β-hemolytic Streptococcus species—were classified as true positives.7
Cultures growing any of the skin contaminant organisms—Aerococcus species, Bacillus species, Clostridium species, Corynebacterium species, diphtheroids, Enterococcus species, Micrococcus species, Propionibacterium species, viridans group Streptococcus species, and Staphylococcus species—underwent a standardized chart review for classification.7 The chart abstraction instrument we used has been described elsewhere.1 Blinded to the method of culture collection, 2 infectious disease (ID) specialists reviewed the abstracted data and independently classified culture results as contaminated, truly positive, or indeterminate. A third ID specialist evaluated cultures classified differently by the initial 2 reviewers. Final classification was determined by consensus of 2 reviewers.
The outcome variable was the category of blood culture result: no growth, contaminated, or truly positive. Concordant pairs were defined as matched cultures with results in the same category, regardless of specific organisms that grew. Discordant pairs were matched pairs with results in different categories. McNemar’s test was used to compare the number of discordant pairs consisting of a contaminated PIV culture and a noncontaminated dedicated venipuncture culture versus the number of pairs with a noncontaminated PIV culture and contaminated dedicated venipuncture culture. We calculated the relative risk of contamination among PIV cultures using dedicated venipuncture as a referent. Similarly, we used McNemar’s test and relative risk calculations to compare the number of truly positive cultures collected by PIV and dedicated venipuncture. Interrater reliability of reviewers was calculated using Cohen’s κ.
RESULTS
During the study period, 8,254 blood cultures were collected in the emergency department; 1,909 cultures (23.1%) were collected through PIVs, and 508 of these PIV cultures were matched to cultures collected by dedicated venipuncture from the same patient within 10 minutes. Sixty-three cultures underwent review by ID specialists with agreement between the initial 2 reviewers in 56 cultures (88.9%; κ = 0.64; standard error, 0.11). Three cultures were classified as indeterminate and excluded, leaving 505 pairs for analyses.
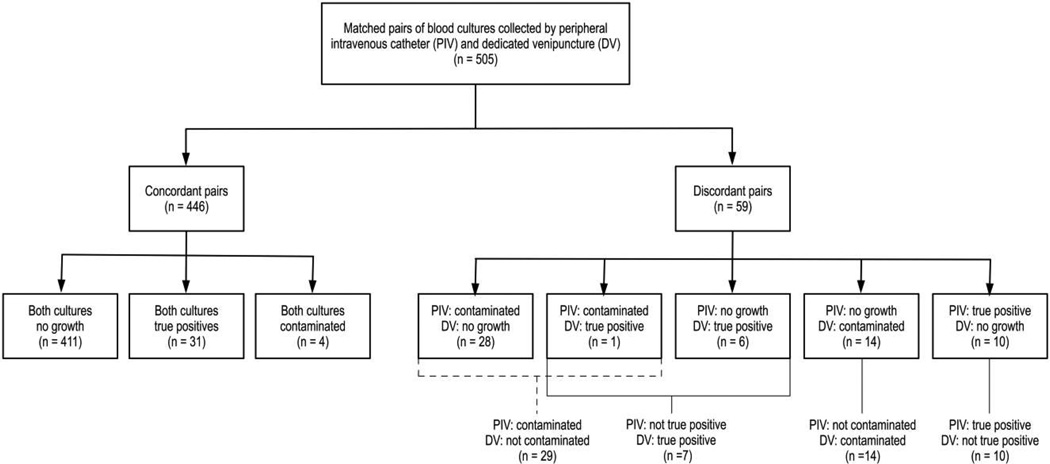
Discordant results were obtained in 59 pairs (11.7%; Figure 1). These discordant pairs included 43 pairs in which one culture was contaminated and its partner was not, including 29 with a contaminated PIV culture and 14 with a contaminated dedicated venipuncture culture (P = .022; Table 1). Overall, 33 of 505 PIV cultures (6.53%) and 18 of 505 dedicated venipuncture cultures (3.56%) were contaminated (relative risk of contamination, 1.83; 95% confidence interval [CI], 1.08–3.11). There were 10 discordant pairs in which the PIV culture grew a true positive but the dedicated venipuncture culture did not, and 7 pairs in which the dedicated venipuncture culture grew a true positive but the PIV culture did not (P = .47). Of 505 cultures collected, 41 PIV cultures (8.12%) and 38 dedicated venipuncture cultures (7.52%) were true positives (relative risk of a true positive culture, 1.08; 95% CI, 0.88–1.32).
FIGURE 1.
Blood culture results of 505 matched pairs of cultures collected by peripheral intravenous catheter (PIV) and dedicated venipuncture (DV) from the same patient within 10 minutes.
TABLE 1.
Organisms Responsible for Contaminated Cultures
| Study category and organisms | No. of pairs |
|---|---|
| PIV contaminated/DV not contaminated | 29 |
| Coagulase-negative Staphylococcus | 16 |
| Diphtheroids | 2 |
| Micrococcus species | 2 |
| Propionibacterium acnes | 2 |
| α-hemolytic Streptococcus | 2 |
| Aerococcus species | 1 |
| Bacillus species | 1 |
| Staphylococcus aureus | 1 |
| Micrococcus species | 1 |
| α-hemolytic Streptococcus and diphtheroids | 1 |
| PIV not contaminated/DV contaminated | 14 |
| Coagulase-negative Staphylococcus | 6 |
| Propionibacterium species | 3 |
| α-hemolytic Streptococcus | 3 |
| Diphtheroids | 1 |
| Micrococcus species | 1 |
| Both PIV and DV contaminated | 4 |
| PIV: coagulase-negative Staphylococcus/DV: Micro- coccus species |
1 |
| PIV: Diphtheroids/DV: coagulase-negative Staphylococcus |
1 |
| PIV: Micrococcus species/DV: Propionibacterium acnes | 1 |
| PIV: Propionibacterium acnes/DV: coagulase-negative Staphylococcus |
1 |
NOTE. DV, dedicated venipuncture; PIV, peripheral intravenous catheter.
On the basis of these results, obtaining blood cultures through PIVs instead of by dedicated venipuncture resulted in 2.97 (95% CI, 0.29–7.51) additional contaminated cultures per 100 cultures collected without a significant change in the number of true positives.
DISCUSSION
Our study suggests that collecting blood culture specimens through PIVs increases the risk of contamination compared with dedicated venipuncture. This is consistent with previous work demonstrating increased contamination associated with specimen collection through central venous catheters.8 Three previous studies evaluating the association between PIV collection and contamination have focused on pediatric patients and yielded conflicting results.6,9,10 Isaacman and Karasic9 found no association between PIV collection and contamination, whereas Norberg et al6 and Ramsook et al10 suggested that PIV collection does increase contamination.
Our study had limitations. Although matching cultures based on patient and time reduced the risk of patient-level confounding, unmeasured factors may have confounded the association between PIV collection and contamination. The decision to collect cultures via a PIV was determined by clinical providers; we did not explore why some patients had PIV cultures while others did not. We selected cultures that were explicitly labeled as collected through PIVs and by dedicated venipuncture in the medical record. We suspect the accuracy of the medical record to be high for these data but did not perform a validation study. Although we classified culture results on the basis of review by ID specialists, misclassification was possible. This was a single site study, and its findings may not be generalizable to other settings with different culturing practices.
Our study suggests that collecting specimens by dedicated venipuncture rather than through PIVs may help minimize contamination. Collecting cultures through catheters has several advantages associated with avoidance of additional venipuncture during the index encounter, including improved patient comfort, reduced needle stick risks, and less time spent obtaining cultures.2 Furthermore, for some patients, such as those who are obese, dehydrated, or edematous, specimen collection through a catheter may be the only available method for rapidly obtaining cultures. Clinicians and policy makers developing protocols for blood culturing practices must weigh the elevated risk of contamination associated with PIV-drawn specimens against the advantages of collecting specimens through catheters.
Acknowledgments
We would like to thank Carlos G. Grijalva, MD, MPH, and Tyler W. Barrett, MD, MSCI, for their thoughtful reviews of the manuscript.
Financial support. This work was supported by the Office of Academic Affiliations, Department of Veterans Affairs, VA National Quality Scholars Program, with resources and the use of facilities at VA Tennessee Valley Healthcare System, Nashville, Tennessee (W.H.S. and C.D.M.).
W.H.S. reports receiving research grants from the Emergency Medicine Patient Safety Foundation, Society for Academic Emergency Medicine, bioMérieux, and CareFusion. J.G.J. reports receiving salary support from Sanofi Pasteur. T.R.T. reports being a consultant for the Joint Commission and Community Health Systems.
Footnotes
Potential conflicts of interest. All other authors report no conflicts of interest relevant to this article. All authors submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and the conflicts that the editors consider relevant to this article are disclosed here.
REFERENCES
- 1.van der Heijden YF, Miller G, Wright PW, Shepherd BE, Daniels TL, Talbot TR. Clinical impact of blood cultures contaminated with coagulase-negative staphylococci at an academic medical center. Infect Control Hosp Epidemiol. 2011;32:623–625. doi: 10.1086/660096. [DOI] [PubMed] [Google Scholar]
- 2.Bates DW, Goldman L, Lee TH. Contaminant blood cultures and resource utilization: the true consequences of false-positive results. JAMA. 1991;265:365–369. [PubMed] [Google Scholar]
- 3.Gander RM, Byrd L, DeCrescenzo M, Hirany S, Bowen M, Baughman J. Impact of blood cultures drawn by phlebotomy on contamination rates and health care costs in a hospital emergency department. J Clin Microbiol. 2009;47:1021–1024. doi: 10.1128/JCM.02162-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hall KK, Lyman JA. Updated review of blood culture contamination. Clin Microbiol Rev. 2006;19:788–802. doi: 10.1128/CMR.00062-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smart D, Baggoley D, Head J, Noble D, Wetherall B, Gordon DL. Effect of needle changing and intravenous cannula collection on blood culture contamination rates. Ann Emerg Med. 1993;22:1164–1168. doi: 10.1016/s0196-0644(05)80983-7. [DOI] [PubMed] [Google Scholar]
- 6.Norberg A, Christopher NC, Ramundo ML, Bower JR, Berman SA. Contamination rates of blood cultures obtained by dedicated phlebotomy vs intravenous catheter. JAMA. 2003;289:726–729. doi: 10.1001/jama.289.6.726. [DOI] [PubMed] [Google Scholar]
- 7.Weinstein MP, Towns ML, Quartey SM, et al. The clinical significance of positive blood cultures in the 1990s: a prospective comprehensive evaluation of the microbiology, epidemiology, and outcome of bacteremia and fungemia in adults. Clin Infect Dis. 1997;24:584–602. doi: 10.1093/clind/24.4.584. [DOI] [PubMed] [Google Scholar]
- 8.Falagas ME, Kazantzi MS, Bliziotis IA. Comparison of utility of blood cultures from intravascular catheters and peripheral veins: a systematic review and decision analysis. J Med Microbiol. 2008;57:1–8. doi: 10.1099/jmm.0.47432-0. [DOI] [PubMed] [Google Scholar]
- 9.Isaacman DJ, Karasic RB. Utility of collecting blood cultures through newly inserted intravenous catheters. Pediatr Infect Dis J. 1990;9:815–818. doi: 10.1097/00006454-199011000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Ramsook C, Childers K, Cron SG, Nirken M. Comparison of blood culture contamination rates in a pediatric emergency room: newly inserted intravenous catheters versus venipuncture. Infect Control Hosp Epidemiol. 2000;21:649–651. doi: 10.1086/501708. [DOI] [PubMed] [Google Scholar]