Abstract
Background
Among former prisoners, a high rate of death has been documented in the early postrelease period, particularly from drug-related causes. Little is known about risk factors and trends in postrelease mortality in the past decade, especially given general population increases in overdose deaths from pharmaceutical opioids.
Objective
To determine postrelease mortality between 1999 and 2009; cause-specific mortality rates; and whether sex, calendar year, and custody factors were risk factors for all-cause, overdose, and opioid-related deaths.
Design
Cohort study.
Setting
Prison system of the Washington State Department of Corrections.
Participants
76 208 persons released from prison.
Measurements
Identities were linked probabilistically to the National Death Index to identify deaths and causes of death, and mortality rates were calculated. Cox proportional hazards regression estimated the effect of age, sex, race or ethnicity, whether the incarceration resulted from a violation of terms of the person’s community supervision, length of incarceration, release type, and calendar year on the hazard ratio (HR) for death.
Results
The all-cause mortality rate was 737 per 100 000 person-years (95% CI, 708 to 766) (n = 2462 deaths). Opioids were involved in 14.8% of all deaths. Overdose was the leading cause of death (167 per 100 000 person-years [CI, 153 to 181]), and overdose deaths in former prisoners accounted for 8.3% of the overdose deaths among persons aged 15 to 84 years in Washington from 2000 to 2009. Women were at increased risk for overdose (HR, 1.38 [CI, 1.12 to 1.69]) and opioid-related deaths (HR, 1.39 [CI, 1.09 to 1.79]).
Limitation
The study was done in only 1 state.
Conclusion
Innovation is needed to reduce the risk for overdose among former prisoners.
Primary Funding Source
National Institute on Drug Abuse and the Robert Wood Johnson Foundation.
Among former prisoners, many studies have shown an increased risk for death, particularly from drug-related causes and in the early postrelease period (1–12). Over the past decade, scientific, public health, and policy efforts have been directed at improving prisoner reentry (13, 14). Yet, over the same period physicians in the United States have substantially increased prescription of pharmaceutical opioids for noncancer pain (15). In addition, nonmedical use of pharmaceutical opioids has increased, with 4.6% of persons aged 12 years or older reporting nonmedical use in 2010 to 2011 (16). As a result, substantial increases in fatal overdose from opioids are being seen in the U.S. population. Overdose is now the leading cause of unintentional injury-related death, surpassing motor vehicle accidents, and pharmaceutical opioids are the leading cause of overdose death (17–20). Little is known about whether these trends have affected criminal justice populations. Thus, we sought to examine changes in postrelease mortality in the past decade, with an emphasis on overdose and opioids.
Although women represent a relatively small proportion of the total U.S. prison population (6.7% in 2011), the growth of the female prisoner population has exceeded that of the male population in the past decade (21). Women are more likely than men to be imprisoned for drug-related offenses (21), and many chronic medical and mental health conditions are more prevalent in this group (22). After release, female former prisoners have higher rates of overdose and suicide than noninstitutionalized women (1, 5, 11), so we have also examined sex differences in postrelease mortality.
Little is known about the association between custody characteristics and risk for postrelease mortality. Custody characteristics include whether a person is incarcerated for a violation of the terms of community supervision, known as parole or probation in many other states. These generally brief incarcerations are commonly due to drug use violations. Other custody characteristics are length of incarceration and type of release. Increasing incarceration length has been associated with a mildly protective effect on all-cause postrelease mortality, independent of age (23, 24). Nonetheless, the relationship may differ for opioid-related deaths because it has been hypothesized that reduced physiologic tolerance after a period of relative abstinence in prison may increase risk for overdose (4). Finally, release followed by community supervision generally involves criminal justice monitoring and may include social or substance dependence services, which could affect postrelease behavior and health outcomes (25).
Methods
Study Design and Setting
We conducted a cohort study of prisoners released from the Washington State Department of Corrections (WA DOC) between 1999 and 2009. The WA DOC is a state prison system that had 15 full-confinement and 15 partial-confinement (for example, work release) facilities and 16 812 male and 1387 female prisoners at year-end 2009 (26). Prisons are run by states or the federal government, whereas jails are run by local governments and generally hold persons who have not been sentenced (that is, remanded) or have been sentenced to short terms (for example, <1 year) (27). The WA DOC was also responsible for most of the state’s community supervision of felons. In 1999, the state legislature passed the Offender Accountability Act (E2SSB 5421, Chapter 196, Laws of 1999), which took effect in 2001. As a result, persons who violated their community supervision terms were increasingly incarcerated in prisons rather than jails and thus were increasingly included in our study population after 2001.
Study Cohort
We obtained data on all 192 944 releases (76 461 persons) between 1 July 1999 and 31 December 2009. This included 30 237 persons from our Washington State prison cohort released from July 1999 to December 2003 (11) and 46 224 persons released from January 2004 through December 2009. We created a new combined cohort that spanned 10.5 years.
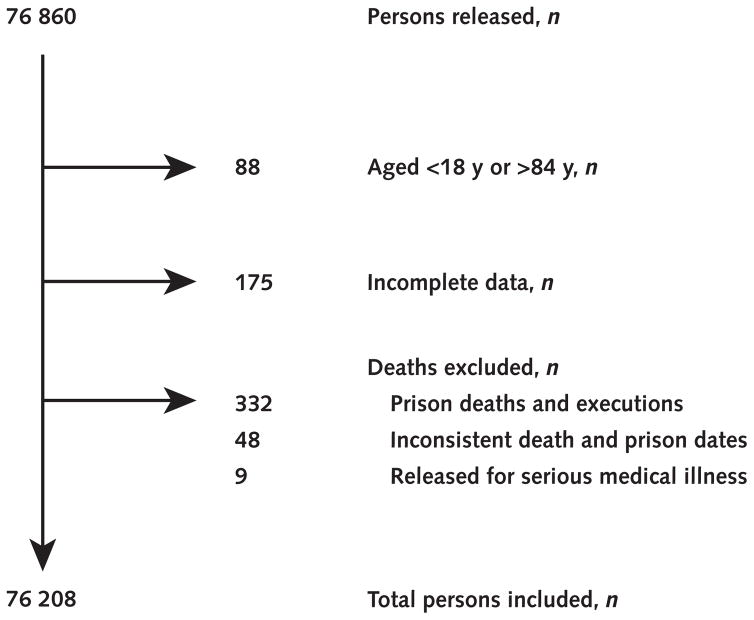
Identifiers from all released persons from 1999 to 2009 were sent to the National Death Index (NDI) to identify deaths though 31 December 2009. The NDI provided new matches for cohort members released from 1999 to 2003 (the previous NDI match only went through 31 December 2003) and from 2004 to 2009. Our methods for matching records to the NDI have been previously described (11). Briefly, data sent to the NDI included Social Security number, aliases, date of birth, sex, and race. Deaths were identified by using the NDI’s probability scoring system (28). Demographic (sex, race or ethnicity, and age) and custody (whether the incarceration was due to a violation of the person’s community supervision terms, length of incarceration, release type, and release date) characteristics were obtained from the administrative records of the WA DOC. Release type was classified as discharged with no supervision (that is, sentence expired), release followed by supervision by community supervision staff, and other (including partial confinement and sentence vacated). The WA DOC also provided a list of persons who died in prison and those placed on medical parole. Exclusion criteria were similar to those previously described (Appendix Figure, available at www.annals.org) (11).
Appendix Figure.
Exclusion criteria.
For comparisons with the general, noninstitutionalized population using standardized mortality ratios (SMRs), we used data from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) (29). For these comparisons, we restricted the time frame from 2000 to 2009 because there were too few deaths from some causes in 1999 when stratified by sex, race, and age (CDC WONDER suppresses death counts when there are fewer than 10 for a given cause). Releases from 1999 or for which race did not match the CDC WONDER race categories (n = 5171; 2.7% of the cohort) were not included in the SMR analysis, which was done on 187 340 releases (73 614 persons). Deaths of former prisoners that occurred in Washington State and time spent in the community before death were deducted from the comparison population. The NDI provided International Classification of Diseases, 10th Revision, codes for the underlying cause of death and several contributing causes of death (if applicable). We first classified deaths into mutually exclusive underlying causes (for example, unintentional injuries) and mutually exclusive subclassifications (for example, overdose or accidental poisoning as a subcategory of unintentional injuries). We use the term “overdose” for deaths in which accidental poisoning was the underlying cause of death (Appendix Table, available at www.annals.org).
Appendix Table.
ICD-10 Codes Used in the Classification of Deaths
| Classification | ICD-10 Codes |
|---|---|
| Unintentional injuries | V01-X59, Y85-Y86 |
| Overdose (accidental poisoning) | X40-X49 |
| Opioid-related | T40.1, T40.2, T40.3, T40.4 |
| Pharmaceutical opioid–related | T40.2–T40.4 |
| Opioids | T40.0–T40.4 |
| Pharmaceutical opioids | T40.2–T40.4 |
| Methadone | T40.3 |
| Heroin | T40.1 |
| Cocaine | T40.5 |
| Other and unspecified narcotics | T40.6 |
| Psychostimulants | T43.6 |
| Alcohol | T51.0–T51.9 |
| Antidepressants | T43.0–T43.2 |
| Benzodiazepines | T42.4 |
| Neuroleptics | T43.3–T43.5 |
| Barbiturates | T42.3 |
| Cannabis | T40.7 |
| Other psychotropics | T43.8–T43.9 |
ICD-10 = International Classification of Diseases, 10th Revision.
Context
Former prisoners are at increased risk for death, particularly from drug-related causes. Over the past decade, increased mortality related to pharmaceutical opioids has been observed in the general population.
Contribution
From 1999 to 2009 in the state of Washington, the leading cause of death after prison release was drug overdose, especially from pharmaceutical opioids. Female former prisoners were at increased risk for overdose and opioid-related death compared with men.
Caution
Data may not be generalizable to other areas.
Implication
Current efforts to reduce drug overdose, including from pharmaceutical opioids, should involve interventions for released prisoners.
—The Editors
More than 1 substance can contribute to death; therefore, we identified the most common combinations of substances listed among substance-related deaths. If the substance was listed among the multiple causes of death, it was classified as “substance-related” regardless of the underlying cause. Thus, “opioid-related deaths” included deaths for which opioids contributed to the death alone as well as when they were combined with other substances. We use the broad term “opioids” to include both “pharmaceutical opioids” (manufactured by pharmaceutical companies), which are commonly prescribed for pain and generally in Drug Enforcement Administration Schedule II or III (for example, hydrocodone or oxycodone), as well as Schedule I opioids, such as heroin.
This study was approved by the Colorado Multiple Institutions Review Board with a waiver of consent, the National Death Index, and the WA DOC. We received a Federal Certificate of Confidentiality.
Statistical Analysis
Descriptive statistics for releases and individuals were calculated by inclusion of means and SDs or medians with interquartile ranges (25th, 75th percentiles). Mortality rates (deaths per 100 000 person-years) were calculated with 95% CIs, in which time at risk included time after release and excluded time in prison during any subsequent incarcerations. Mortality rates were calculated for all-cause death, 11 causes of death and their subcauses, substance-related causes, and the most common substance combinations. Mortality rates were calculated by cause for men and women and tested to determine whether they differed statistically by sex.
We estimated crude in-prison mortality rates from 2004 to 2009 to compare with published in-prison death rates from 1999 to 2003. With NDI linkage, we confirmed 234 in-prison deaths reported by the WA DOC. An additional 11 deaths had potential matches in the NDI but did not meet our requirements for probability matching. One additional in-prison death had no matches in the NDI. We summed the midyear populations from 2004 to 2009 for the population denominator.
The SMRs, adjusted for sex, race, and age, were computed to compare the observed number of deaths in the cohort with the expected number of deaths based on the mortality rates for the noninstitutionalized population of Washington State.
For our risk factor analysis, we examined time to death for 4 outcomes of particular clinical and public health importance: all-cause, nonoverdose, overdose, and opioid-related events. Cox proportional hazards regression was used to investigate whether the survival experience was associated with demographic (sex, race or ethnicity, and age) or custody (whether the incarceration was due to a violation of community supervision terms, length of incarceration, release type, and release year) characteristics. We modeled custody characteristics as separate variables because they are applications of distinct legal policies. In checking the independent variables for collinearity, the largest variance inflation factor among all variables was 1.66 and within acceptable limits in which remedial action was not needed. Release year was modeled as a categorical variable because the hazard of death varied in a nonlinear pattern across calendar time.
It was reasonable to assume that there was a correlation among releases for an individual with multiple releases, and 45% of the cohort members had 2 or more releases. This correlation was accounted for by using the options available in SAS, version 9.3 (SAS Institute, Cary, North Carolina), which sum the score residuals for each participant in the computation of the Lin and Wei robust sandwich estimate of the covariance matrix. Data on 220 releases (0.1%) were not included in the Cox analyses because of missing data for covariates. We explored the effect of each risk factor on the hazard for death in 3 clinically important periods of risk after release from prison: the first month, months 2 to 12, and subsequent months. The hazard ratios (HRs) for risk factors did not differ significantly in these periods, except for age, which was significantly different in the third period compared with the 2 previous periods. The final analyses thus included interaction terms to model the effect of age on mortality separately for each period. For covariates other than age, the assumption of proportional hazards was tested and satisfied by using the methods of Lin and coworkers (30), which compare the observed score process with simulated score processes for each covariate. The P value for the test of proportional hazards is based on the results of a Kolmogorov-type supremum test. We did 1000 simulations for these tests (31).
Data were analyzed by using SAS, version 9.3.
Role of the Funding Source
Funding for this study was provided by the National Institute on Drug Abuse (grant R21DA031041) and the Robert Wood Johnson Foundation. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Results
This cohort included 76 208 released prisoners from 1999 to 2009, with 192 511 releases (Table 1) and 334 238 person-years. The mean length of follow-up by person was 4.4 years (SD, 2.7). Most (55%) had 1 release, and 29% had 3 or more releases. The mean age at release was 34.5 years (SD, 9.9). Incarcerations due to violations of community supervision terms were shorter (mean, 0.1 year [SD, 0.1]) than standard incarcerations (mean, 1.9 years [SD, 2.8]).
Table 1.
Demographic and Custody Characteristics of Persons Released and Corresponding Prison Releases, July 1999–December 2009
| Variable | Individuals or Releases, n (%) |
|---|---|
| Demographic characteristic | |
|
| |
| Released individuals/releases, n/N | 76 208/192 511 |
|
| |
| Age at each release | |
| 18–24 y | 39 363 (20.4) |
|
| |
| 25–34 y | 65 828 (34.2) |
|
| |
| 35–44 y | 57 052 (29.6) |
|
| |
| 45–54 y | 25 517 (13.3) |
|
| |
| 55–64 y | 4096 (2.1) |
|
| |
| 65–74 y | 575 (0.3) |
|
| |
| 75–84 y | 80 (0.0) |
| Sex | |
|
| |
| Male | 63 979 (84.0) |
|
| |
| Female | 12 229 (16.0) |
| Race/ethnicity | |
|
| |
| White, non-Hispanic | 49 206 (64.6) |
|
| |
| African American, non-Hispanic | 13 173 (17.3) |
|
| |
| Hispanic | 8797 (11.5) |
|
| |
| Asian, non-Hispanic | 1902 (2.5) |
|
| |
| Other | 3037 (4.0) |
|
| |
| Missing | 93 (0.1) |
| Number of releases during study | |
|
| |
| 1 | 41 565 (54.5) |
|
| |
| 2 | 12 446 (16.3) |
|
| |
| 3 | 6701 (8.8) |
|
| |
| 4 | 4511 (5.9) |
|
| |
| 5 | 3103 (4.1) |
|
| |
| 6 | 2088 (2.7) |
|
| |
| 7 | 1461 (1.9) |
|
| |
| 8 | 1057 (1.4) |
|
| |
| 9 | 787 (1.0) |
|
| |
| ≥10 | 2489 (3.3) |
| Custody characteristic | |
|
| |
| Entire cohort | 192 511 |
|
| |
| Incarceration due to violation of community supervision terms | 43 321 (22.5) |
| Length of incarceration | |
|
| |
| 0–6 mo | 126 182 (65.5) |
|
| |
| 6–12 mo | 27 390 (14.2) |
|
| |
| 12–24 mo | 18 737 (9.7) |
|
| |
| ≥24 mo | 20 202 (10.5) |
| Release type | |
|
| |
| With community supervision | 167 290 (86.9) |
|
| |
| Without community supervision | 22 827 (11.9) |
|
| |
| Other | 2342 (1.2) |
|
| |
| Missing | 52 (0.03) |
| Release year | |
|
| |
| 1999* | 3236 (1.7) |
|
| |
| 2000 | 6719 (3.5) |
|
| |
| 2001 | 7331 (3.8) |
|
| |
| 2002 | 9106 (4.7) |
|
| |
| 2003 | 12 408 (6.4) |
|
| |
| 2004 | 17 988 (9.3) |
|
| |
| 2005 | 23 667 (12.3) |
|
| |
| 2006 | 25 951 (13.5) |
|
| |
| 2007 | 29 401 (15.3) |
|
| |
| 2008 | 29 050 (15.1) |
|
| |
| 2009 | 27 654 (14.4) |
1 July–31 December 1999.
A total of 2462 persons died after release from prison: 18.0% of deaths (n = 443) were previously identified between 1999 and 2003 (11), 30.6% (n = 754) occurred between 2004 and 2009 among persons released from 1999 to 2003, and 51.4% (n = 1265) occurred among persons released from 2004 to 2009. The median age at death was 45 years (interquartile range, 35 to 53 years). The median time from release to death was 1.7 years (range, 1 day to 10.2 years): 194 persons (7.8%) died in the first month, 742 (30.1%) died in months 2 to 12, and 1526 (62.0%) died after 1 year.
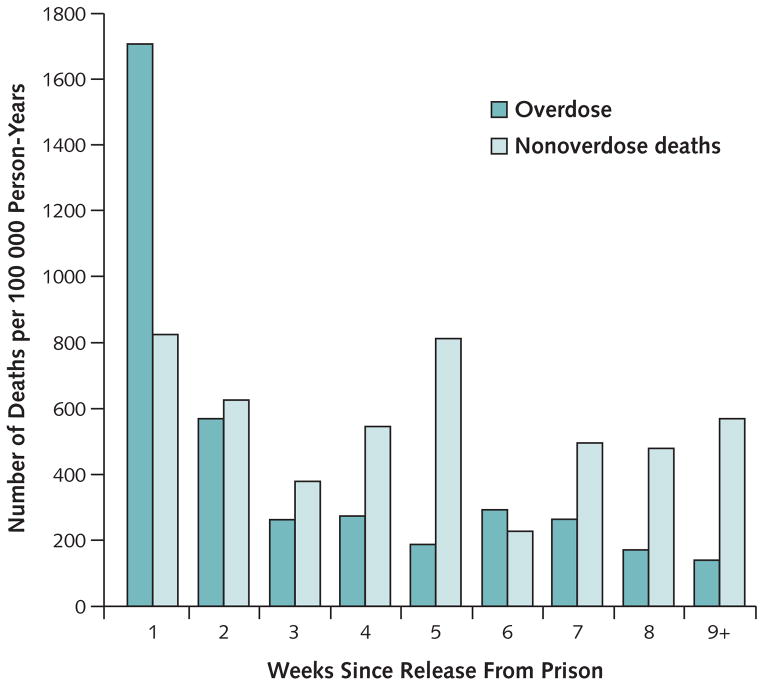
The all-cause mortality rate was 737 per 100 000 person-years (95% CI, 708 to 766) (Table 2). The leading cause of death was unintentional injuries (n = 828; 248 per 100 000 person-years [CI, 231 to 265]), which were driven by overdose (n = 558; 167 per 100 000 person-years [CI, 153 to 181]). The overdose mortality rate was higher in women than in men (236 vs. 154 per 100 000 person-years; P < 0.001). We saw an increased mortality rate in the first week after release relative to subsequent weeks for overdoses but not for nonoverdose deaths (Figure). The second leading cause of death was cardiovascular disease (95 per 100 000 person-years [CI, 85 to 106]), followed by cancer (71 per 100 000 person-years [CI, 62 to 80]). Lung cancer had the highest cancer mortality rate (26 per 100 000 person-years [CI, 20 to 31]), followed by liver cancer (10 per 100 000 person-years [CI, 6 to 13]). Among infectious causes of death, the mortality rate from viral hepatitis (21 per 100 000 person-years [CI, 16 to 26]) exceeded that of HIV (11 per 100 000 person-years [CI, 8 to 15]). The crude in-prison mortality rate from 2004 to 2009 was estimated at 245 per 100 000 person-years.
Table 2.
Deaths After Release From Prison by Leading Causes, Overall and by Sex
| Variable | Overall (n = 76 208)
|
Men (n = 63 979)
|
Women (n = 12 229)
|
|||
|---|---|---|---|---|---|---|
| Deaths, n | Deaths per 100 000 Person-Years (95% CI) | Deaths, n | Deaths per 100 000 Person-Years (95% CI) | Deaths, n | Deaths per 100 000 Person-Years (95% CI) | |
| All-cause death | 2462 | 737 (708–766) | 2124 | 752 (720–784) | 338 | 653 (583–722) |
|
| ||||||
| Unintentional injuries | 828 | 248 (231–265) | 683 | 242 (224–260) | 145 | 280 (234–326) |
|
| ||||||
| Overdose | 558 | 167 (153–181) | 436 | 154 (140–169) | 122 | 236 (194–277) |
|
| ||||||
| Motor vehicle accidents | 183 | 55 (47–63) | 168 | 60 (50–68) | 15 | 29 (14–44) |
|
| ||||||
| Drowning | 23 | 7 (4–10) | 22 | 8 (5–11) | 1 | 2 (0–11) |
|
| ||||||
| Cardiovascular diseases | 319 | 95 (85–106) | 290 | 103 (91–114) | 29 | 56 (36–76) |
|
| ||||||
| Ischemic heart | 170 | 51 (43–59) | 159 | 56 (48–65) | 11 | 21 (9–34) |
|
| ||||||
| Cerebrovascular | 39 | 12 (8–15) | 30 | 11 (7–14) | 9 | 17 (8–33) |
|
| ||||||
| Hypertensive heart | 36 | 11 (7–14) | 33 | 12 (8–16) | 3 | 6 (1–17) |
|
| ||||||
| Cancer | 238 | 71 (62–80) | 205 | 73 (63–83) | 33 | 64 (42–85) |
|
| ||||||
| Lung | 86 | 26 (20–31) | 72 | 25 (20–31) | 14 | 27 (13–41) |
|
| ||||||
| Liver | 32 | 10 (6–13) | 29 | 10 (7–14) | 3 | 6 (1–17) |
|
| ||||||
| Blood/lymph | 21 | 6 (4–9) | 19 | 7 (4–10) | 2 | 4 (0–14) |
|
| ||||||
| Esophagus/stomach | 18 | 5 (3–8) | 17 | 6 (3–9) | 1 | 2 (0–11) |
|
| ||||||
| Pancreas | 10 | 3 (1–5) | 8 | 3 (1–6) | 2 | 4 (0–14) |
|
| ||||||
| Homicide | 219 | 66 (57–74) | 213 | 75 (65–86) | 6 | 12 (4–25) |
|
| ||||||
| By firearm | 163 | 49 (41–56) | 159 | 56 (48–65) | 4 | 8 (2–20) |
|
| ||||||
| Suicide | 212 | 63 (55–72) | 191 | 68 (58–77) | 21 | 41 (23–58) |
|
| ||||||
| By firearm | 43 | 13 (9–17) | 41 | 15 (10–19) | 2 | 4 (0–14) |
|
| ||||||
| Infectious disease | 158 | 47 (40–55) | 136 | 48 (40–56) | 22 | 42 (25–60) |
|
| ||||||
| Viral hepatitis | 69 | 21 (16–26) | 59 | 21 (16–26) | 10 | 19 (7–31) |
|
| ||||||
| HIV | 37 | 11 (8–15) | 31 | 11 (7–15) | 6 | 12 (4–25) |
|
| ||||||
| Septicemia | 21 | 6 (4–9) | 17 | 6 (3–9) | 4 | 8 (2–20) |
|
| ||||||
| Pneumonia | 19 | 6 (3–8) | 17 | 6 (3–9) | 2 | 4 (0–14) |
|
| ||||||
| Liver disease | 73 | 22 (17–27) | 66 | 23 (18–29) | 7 | 14 (5–28) |
|
| ||||||
| Alcoholic | 58 | 17 (13–22) | 53 | 19 (14–24) | 5 | 10 (3–23) |
|
| ||||||
| Respiratory disease | 67 | 20 (15–25) | 52 | 18 (13–23) | 15 | 29 (14–44) |
|
| ||||||
| Lower respiratory disease | 42 | 13 (9–16) | 35 | 12 (8–16) | 7 | 14 (5–28) |
|
| ||||||
| Diabetes mellitus | 49 | 15 (11–19) | 46 | 16 (12–21) | 3 | 6 (1–17) |
|
| ||||||
| Kidney disease | 12 | 4 (2–6) | 12 | 4 (2–7) | 0 | 0 (0–7) |
|
| ||||||
| Other | 287 | 86 (76–96) | 230 | 81 (71–92) | 57 | 110 (82–130) |
Figure.
Mortality rate, by week since release, for overdose and all other (nonoverdose) causes of death.
Opioids were involved in 14.8% (n = 365) of all deaths (Table 3) and 58.6% (n = 327) of overdose deaths. Specifically, pharmaceutical opioids were involved in 10.5% (n = 259) of all deaths and 40.5% (n = 226) of overdose deaths. Overdose was the underlying cause of death in 90% (n = 327) of opioid-related deaths, whereas other underlying causes, such as suicide (n = 12), were listed for the remainder. Cocaine was involved in the second highest number (n = 209) of substance-related deaths. Women had higher mortality rates than men for the following substance-related causes of death: pharmaceutical opioids (135 vs. 67; P < 0.001), cocaine (100 vs. 56; P < 0.001), antidepressants (73 vs. 23; P < 0.001), benzodiazepines (33 vs. 15; P = 0.016), and other and unspecified narcotics (81 vs. 50; P = 0.011). Of the 632 substance-related deaths, 355 (56.2%) had several substances involved, generally including opioids. The most common combinations were opioids and cocaine (n = 37) and cocaine and other narcotics (n = 36) (Table 4).
Table 3.
Deaths and Mortality Rates for Substance-Related Deaths After Release, Overall and by Sex*
| Substance Involved† | Overall (n = 76 208)
|
Men (n = 63 979)
|
Women (n = 12 229)
|
|||
|---|---|---|---|---|---|---|
| Deaths, n | Deaths per 100 000 Person-Years (95% CI) | Deaths, n | Deaths per 100 000 Person-Years (95% CI) | Deaths, n | Deaths per 100 000 Person-Years (95% CI) | |
| Opioids | 365 | 109 (98–120) | 283 | 100 (89–112) | 82 | 158 (124–193) |
|
| ||||||
| Pharmaceutical opioids | 259 | 77 (68–87) | 189 | 67 (57–76) | 70 | 135 (104–167) |
|
| ||||||
| Methadone | 176 | 53 (45–60) | 130 | 46 (38–54) | 46 | 89 (63–115) |
|
| ||||||
| Heroin | 123 | 37 (30–43) | 107 | 38 (31–45) | 16 | 31 (16–46) |
|
| ||||||
| Cocaine | 209 | 63 (54–71) | 157 | 56 (47–64) | 52 | 100 (73–128) |
|
| ||||||
| Other and unspecified narcotics | 184 | 55 (47–63) | 142 | 50 (42–59) | 42 | 81 (57–106) |
|
| ||||||
| Psychostimulants | 136 | 41 (34–48) | 109 | 39 (31–46) | 27 | 52 (32–72) |
|
| ||||||
| Alcohol | 93 | 28 (22–33) | 77 | 27 (21–33) | 16 | 31 (16–46) |
|
| ||||||
| Antidepressants | 103 | 31 (25–37) | 65 | 23 (17–29) | 38 | 73 (50–97) |
|
| ||||||
| Benzodiazepines | 60 | 18 (13–22) | 43 | 15 (11–20) | 17 | 33 (17–48) |
|
| ||||||
| Neuroleptics | 26 | 8 (5–11) | 20 | 7 (4–10) | 6 | 12 (4–25) |
|
| ||||||
| Barbiturates | 4 | 1 (0–3) | 3 | 1 (0–3) | 1 | 2 (0–11) |
|
| ||||||
| Cannabis | 2 | 1 (0–2) | 2 | 1 (0–3) | 0 | 0 (0–7) |
|
| ||||||
| Other psychotropics | 2 | 1 (0–2) | 2 | 1 (0–3) | 0 | 0 (0–7) |
Overdose may not be listed as the underlying cause of death for the deaths listed. For example, of the 259 deaths where pharmaceutical opioids were involved, 33 (12.7%) listed an underlying cause other than overdose.
Not mutually exclusive as each substance may be listed more than once among the multiple cause-of-death listings per individual.
Table 4.
Most Common Substance Combinations Listed in Substance-Related Deaths and Associated Mortality Rates
| Combination | Deaths, n | Deaths per 100 000 Person-Years (95% CI) |
|---|---|---|
| Opioid and cocaine | 37 | 11 (8–15) |
| Cocaine and other narcotics | 36 | 11 (7–14) |
| Opioid and psychostimulants | 24 | 7 (4–10) |
| Opioid and other narcotics | 18 | 5 (3–8) |
| Opioid and benzodiazepines | 16 | 5 (2–7) |
| Opioid and antidepressants | 14 | 4 (2–6) |
| Opioid, cocaine, and other narcotics | 13 | 4 (2–6) |
| Opioid and alcohol | 11 | 3 (1–5) |
| Opioid, cocaine, and alcohol | 10 | 3 (1–5) |
| Opioid, other narcotics, and alcohol | 9 | 3 (1–5) |
Compared with the noninstitutionalized population, the adjusted risk for all-cause death was 3.61-fold higher among former prisoners (CI, 3.48 to 3.73) and higher for every main cause of death except for diabetes (Table 5). Former prisoners had a 10.33-fold increased risk for overdose (SMR, 10.33 [CI, 9.61 to 11.10]). Overdose deaths among former prisoners in Washington State from 2000 to 2009 accounted for 8.3% (n = 533) of the total overdoses among state residents aged 15 to 84 years (n = 6434).
Table 5.
Observed and Expected Deaths and Standardized Mortality Ratios Among Prisoners Released From 2000 to 2009*
| Variable | Observed Deaths, n | Expected Deaths, n | SMR (95% CI) | Median Age at Death (IQR), y |
|---|---|---|---|---|
| All-cause death | 2324 | 645 | 3.61 (3.48–3.73) | 44.7 (34.6–52.8) |
| Unintentional injuries | 793 | 134 | 5.91 (5.57–6.26) | 39.9 (31.1–47.6) |
| Overdose | 533 | 52 | 10.33 (9.61–11.10) | 41.6 (33.7–48.4) |
| Cardiovascular disease | 298 | 120 | 2.49 (2.26–2.74) | 52.0 (46.4–59.6) |
| Cancer | 224 | 121 | 1.85 (1.65–2.07) | 54.8 (47.8–62.7) |
| Homicide | 202 | 24 | 8.47 (7.52–9.52) | 31.5 (26.1–39.0) |
| Suicide | 197 | 61 | 3.23 (2.86–3.63) | 36.0 (28.6–44.9) |
| Infectious disease | 149 | 36 | 4.12 (3.58–4.71) | 48.0 (42.1–55.0) |
| Liver disease | 67 | 21 | 3.26 (2.63–3.99) | 50.4 (45.0–56.7) |
| Respiratory disease | 61 | 20 | 3.11 (2.48–3.85) | 54.8 (49.5–64.1) |
| Diabetes | 48 | 123 | 0.39 (0.30–0.50) | 53.6 (43.3–59.9) |
| Kidney disease | 11 | 4 | 2.83 (1.59–4.69) | 57.5 (50.6–63.8) |
| Other death | 274 | 75 | 3.66 (3.31–4.05) | 44.6 (36.4–50.7) |
IQR = interquartile range; SMR = standardized mortality ratio.
Compared with other state residents and adjusted for age, sex, race, and median age at death by cause (187 340 releases from 73 614 persons). Deaths excluded from SMR calculations if race did not match the groups in the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research (white, black, Asian, or American Indian). Deaths outside of Washington state are excluded.
In adjusted analyses, the strongest risk factor for all-cause, overdose, and opioid-related deaths was increased age (Table 6). Each decade increase in age was associated with an increased risk for all-cause death during the first month after release (HR, 1.67 [CI, 1.46 to 1.91]) and months 2 through 12 (HR, 1.71 [CI, 1.59 to 1.84]) and an even greater increase in subsequent months (HR, 1.94 [CI, 1.86 to 2.03]). Although women had a reduced risk for all-cause death (HR, 0.85 [CI, 0.75 to 0.95]) and nonoverdose deaths (HR, 0.70 [CI, 0.60 to 0.80]), they were at greater risk for overdose death (HR, 1.38 [CI, 1.12 to 1.69]) and opioid-related death (HR, 1.39 [CI, 1.09 to 1.79]) than men. African Americans, Hispanic persons, and Asian persons had a statistically significant reduced risk for all-cause, overdose, and opioid-related death compared with white persons. Incarcerations due to violations of community supervision terms were associated with an increased risk for all-cause death after release (HR, 1.28 [CI, 1.15 to 1.42]). Increasing length of incarceration was associated with a small but statistically significant reduction in the risk for all-cause and overdose death. Being released without community supervision was associated with an increased risk for all-cause death (HR, 1.13 [CI, 1.02 to 1.26]) compared with release with supervision.
Table 6.
Multivariable Models of Potential Risk Factors for Time to Death After Release for All-Cause, Nonoverdose, Overdose, and Opioid-Related Deaths
| Variable | Adjusted HR (95% CI)
|
|||
|---|---|---|---|---|
| All-Cause | Causes Other Than Overdose | Overdose | Opioid-Related | |
| Age* | ||||
|
| ||||
| Months 0–1 after release | 1.67 (1.46–1.91) | 1.79 (1.46–2.20) | 1.58 (1.33–1.88) | 1.71 (1.36–2.15) |
|
| ||||
| Months 2–12 after release | 1.71 (1.59–1.84) | 1.77 (1.63–1.93) | 1.53 (1.35–1.74) | 1.53 (1.28–1.83) |
|
| ||||
| Months 13 or more after release | 1.94 (1.86–2.03) | 2.03 (1.93–2.13) | 1.56 (1.42–1.72) | 1.57 (1.41–1.75) |
|
| ||||
| Sex | ||||
| Male | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
|
| ||||
| Female | 0.85 (0.75–0.95) | 0.70 (0.60–0.80) | 1.38 (1.12–1.69) | 1.39 (1.09–1.79) |
|
| ||||
| Race/ethnicity | ||||
| White, non-Hispanic | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
|
| ||||
| African American, non-Hispanic | 0.82 (0.74–0.91) | 0.93 (0.82–1.04) | 0.53 (0.41–0.68) | 0.32 (0.22–0.47) |
|
| ||||
| Hispanic | 0.65 (0.56–0.76) | 0.74 (0.62–0.88) | 0.38 (0.25–0.57) | 0.30 (0.17–0.51) |
|
| ||||
| Asian, non-Hispanic | 0.61 (0.42–0.88) | 0.80 (0.55–1.17) | 0.08 (0.01–0.56) | 0.00 (0.00–0.00) |
|
| ||||
| Other | 1.02 (0.84–1.25) | 1.16 (0.93–1.46) | 0.64 (0.40–1.03) | 0.85 (0.51–1.40) |
| Type of incarceration | ||||
|
| ||||
| Standard incarceration | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
|
| ||||
| Incarceration due to violation of terms of community supervision | 1.28 (1.15–1.42) | 1.27 (1.13–1.43) | 1.24 (0.96–1.60) | 1.16 (0.85–1.58) |
|
| ||||
| Length of incarceration† | 0.98 (0.96–0.99) | 0.99 (0.97–1.00) | 0.91 (0.84–1.00) | 0.93 (0.84–1.03) |
|
| ||||
| Release type | ||||
| With community supervision | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
|
| ||||
| Without community supervision | 1.13 (1.02–1.26) | 1.11 (0.98–1.25) | 1.21 (0.96–1.52) | 1.10 (0.83–1.47) |
|
| ||||
| Other | 0.77 (0.56–1.08) | 0.73 (0.50–1.07) | 0.92 (0.49–1.75) | 1.14 (0.56–2.30) |
| Calendar year of release | ||||
|
| ||||
| 1999 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
|
| ||||
| 2000 | 1.08 (0.88–1.34) | 1.11 (0.88–1.41) | 0.96 (0.59–1.57) | 1.08 (0.58–2.03) |
|
| ||||
| 2001 | 1.07 (0.86–1.32) | 1.11 (0.87–1.40) | 0.92 (0.57–1.51) | 1.04 (0.55–1.97) |
|
| ||||
| 2002 | 0.95 (0.76–1.18) | 0.94 (0.73–1.20) | 0.98 (0.61–1.57) | 1.08 (0.58–2.01) |
|
| ||||
| 2003 | 0.95 (0.77–1.18) | 0.98 (0.77–1.25) | 0.85 (0.53–1.37) | 1.10 (0.59–2.04) |
|
| ||||
| 2004 | 0.92 (0.74–1.14) | 0.93 (0.73–1.19) | 0.87 (0.54–1.39) | 1.22 (0.67–2.23) |
|
| ||||
| 2005 | 0.90 (0.72–1.12) | 0.92 (0.71–1.18) | 0.82 (0.51–1.33) | 1.04 (0.56–1.94) |
|
| ||||
| 2006 | 0.85 (0.67–1.06) | 0.91 (0.70–1.17) | 0.66 (0.41–1.08) | 0.98 (0.53–1.81) |
|
| ||||
| 2007 | 0.69 (0.54–0.88) | 0.69 (0.52–0.91) | 0.67 (0.40–1.11) | 0.84 (0.43–1.62) |
|
| ||||
| 2008 | 0.88 (0.68–1.12) | 0.85 (0.63–1.13) | 0.91 (0.55–1.51) | 1.19 (0.62–2.28) |
|
| ||||
| 2009 | 0.80 (0.59–1.08) | 0.81 (0.57–1.16) | 0.74 (0.41–1.32) | 1.20 (0.58–2.48) |
HR = hazard ratio.
Each decade increase in age was associated with an increased risk for all-cause death during the first month after release and a greater increase in subsequent months.
Increasing length of incarceration was associated with a small but statistically significant reduction in the risk for all-cause and overdose deaths.
Discussion
The leading cause of death in former prisoners was overdose. Pharmaceutical opioids were the most common substances involved in these deaths. From 1999 to 2003, cocaine was involved in the largest number of deaths (11), but in later years opioids were more commonly involved. We also found that multiple substances, often in conjunction with opioids, were involved in more than half of substance-related deaths.
Our findings that women leaving prison were at higher risk for opioid-related death than men may indicate evolving demographic patterns of complications from opioid use. Women also had higher mortality rates from overdose of other substances, including cocaine and antidepressants. For the pharmaceutical substances contributing to deaths in this cohort, we cannot determine whether the medications were prescribed or diverted or whether use was for medical or nonmedical reasons even if prescribed. Nonetheless, our findings suggest that improved overdose education, monitoring for medication problems, and drug treatment are needed in prison- and community-based mental and health care systems. Effective, patient-centered interventions to prevent substance-related death are needed to address these risks in former prisoners.
Our study supports the need for careful consideration of the overdose risks associated with transition from prison to the community. Legal policies, such as incarceration for violations of community supervision terms, may have unanticipated health effects. For drug-dependent persons, transitions, such as hospital discharge and discontinuation of drug treatment, have been associated with increased mortality (32, 33). Enforced abstinence may be associated with counterintuitive effects on future mortality (34). Persons receiving methadone or buprenorphine before incarceration frequently do not continue treatment in prison because of administrative prohibitions. Promising interventions for this population include broader access to these evidence-based treatments of opioid dependence in prison and after release. In addition, publicly funded overdose education and naloxone (an opioid antidote) distribution programs may help reduce the risk for death in former prisoners. For example, Scotland distributes naloxone to prisoners as part of a national program (35). Finally, agencies that provide postrelease housing and reentry social services should consider how to reduce social exposures, which can trigger drug use among former prisoners with a history of drug dependence (25).
Increased attention to the complex health needs of this vulnerable population is also warranted because of the risk for cardiovascular disease, cancer, homicide, and suicide. The combined risk for death from liver disease and liver cancer may be partially related to the elevated prevalence of hepatitis C in prisoners.
This study was limited by exclusions resulting from inconsistencies in administrative data. We applied stringent requirements for probabilistic matching with the NDI, which probably excluded actual deaths and may have reduced the observed rates of death. Conversely, some deaths classified as occurring after release may have occurred in jails, federal facilities, or facilities in other states or countries. The classification scheme for underlying and contributing causes of death is subject to some limitations, particularly with regard to specific substances contributing to death (17). Cause of death determinations may be affected by whether an autopsy was done, differing metabolism of substances, and variability in testing methods used across coroner and medical examiner systems. Despite these limitations, the longer study duration and larger cohort gave us the ability to examine risk factors, such as sex differences, with greater power and precision than in previous studies (24). New data on custody characteristics increased understanding of postrelease mortality.
Innovative health care, public health, and policy efforts are needed to reduce the risk for death after release from prison. In 2010, the World Health Organization issued policy and treatment recommendations on drug-related deaths after prison release (36), which may serve as an initial guide. Former prisoners should be included in broader strategic efforts to reduce overdose from pharmaceutical opioids in the United States.
Acknowledgments
The authors thank Washington State Department of Corrections, especially Kathryn Lundy, RHIT; Mike Evans; and David Daniels, Traci E. Yamashita, MS, Rick Whisenhunt, Melanie Arndt, and Marcy Fulmer for their assistance in the execution of this study; and Jean Kutner, MD, MSPH, and John F. Steiner, MD, MPH, for their thoughtful comments on the design and implementation of this study.
Grant Support: By the National Institute on Drug Abuse of the National Institutes of Health (R21DA031041) and the Robert Wood Johnson Foundation.
Footnotes
Current author addresses and author contributions are available at www.annals.org.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Robert Wood Johnson Foundation.
Potential Conflicts of Interest: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M13-0979.
Reproducible Research Statement: Study protocol: Not applicable. Statistical code: Portions of the code are available from Dr. Blatchford (Patrick.Blatchford@ucdenver.edu). Data set: Not available.
Author Contributions: Conception and design: I.A. Binswanger, M.F. Stern.
Analysis and interpretation of the data: I.A. Binswanger, P.J. Blatchford, M.F. Stern.
Drafting of the article: I.A. Binswanger, P.J. Blatchford.
Critical revision of the article for important intellectual content: S.R. Mueller, M.F. Stern.
Final approval of the article: P.J. Blatchford, S.R. Mueller, M.F. Stern.
Statistical expertise: P.J. Blatchford.
Obtaining of funding: I.A. Binswanger, P.J. Blatchford, M.F. Stern.
Administrative, technical, or logistic support: S.R. Mueller.
Collection and assembly of data: I.A. Binswanger, P.J. Blatchford, S.R. Mueller.
References
- 1.Kariminia A, Butler T, Corben S, Levy M, Grant L, Kaldor J, et al. Extreme cause-specific mortality in a cohort of adult prisoners—1988 to 2002: a data-linkage study. Int J Epidemiol. 2007;36:310–6. doi: 10.1093/ije/dyl225. [DOI] [PubMed] [Google Scholar]
- 2.Bird SM, Hutchinson SJ. Male drugs-related deaths in the fortnight after release from prison: Scotland, 1996–99. Addiction. 2003;98:185–90. doi: 10.1046/j.1360-0443.2003.00264.x. [DOI] [PubMed] [Google Scholar]
- 3.Seaman SR, Brettle RP, Gore SM. Mortality from overdose among injecting drug users recently released from prison: database linkage study. BMJ. 1998;316:426–8. doi: 10.1136/bmj.316.7129.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krinsky CS, Lathrop SL, Brown P, Nolte KB. Drugs, detention, and death: a study of the mortality of recently released prisoners. Am J Forensic Med Pathol. 2009;30:6–9. doi: 10.1097/PAF.0b013e3181873784. [DOI] [PubMed] [Google Scholar]
- 5.Pratt D, Piper M, Appleby L, Webb R, Shaw J. Suicide in recently released prisoners: a population-based cohort study. Lancet. 2006;368:119–23. doi: 10.1016/S0140-6736(06)69002-8. [DOI] [PubMed] [Google Scholar]
- 6.Rosen DL, Schoenbach VJ, Wohl DA. All-cause and cause-specific mortality among men released from state prison, 1980–2005. Am J Public Health. 2008;98:2278–84. doi: 10.2105/AJPH.2007.121855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stewart LM, Henderson CJ, Hobbs MS, Ridout SC, Knuiman MW. Risk of death in prisoners after release from jail. Aust N Z J Public Health. 2004;28:32–6. doi: 10.1111/j.1467-842x.2004.tb00629.x. [DOI] [PubMed] [Google Scholar]
- 8.Lim S, Seligson AL, Parvez FM, Luther CW, Mavinkurve MP, Binswanger IA, et al. Risks of drug-related death, suicide, and homicide during the immediate post-release period among people released from New York City jails, 2001–2005. Am J Epidemiol. 2012;175:519–26. doi: 10.1093/aje/kwr327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zlodre J, Fazel S. All-cause and external mortality in released prisoners: systematic review and meta-analysis. Am J Public Health. 2012;102:e67–75. doi: 10.2105/AJPH.2012.300764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merrall EL, Kariminia A, Binswanger IA, Hobbs MS, Farrell M, Marsden J, et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010;105:1545–54. doi: 10.1111/j.1360-0443.2010.02990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, et al. Release from prison—a high risk of death for former inmates. N Engl J Med. 2007;356:157–65. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spaulding AC, Seals RM, McCallum VA, Perez SD, Brzozowski AK, Steenland NK. Prisoner survival inside and outside of the institution: implications for health-care planning. Am J Epidemiol. 2011;173:479–87. doi: 10.1093/aje/kwq422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system: improving public health and safety. JAMA. 2009;301:183–90. doi: 10.1001/jama.2008.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nunn A, Zaller N, Dickman S, Nijhawan A, Rich JD. Improving access to opiate addiction treatment for prisoners [Letter] Addiction. 2010;105:1312–3. doi: 10.1111/j.1360-0443.2010.03000.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Campbell CI, Weisner C, Leresche L, Ray GT, Saunders K, Sullivan MD, et al. Age and gender trends in long-term opioid analgesic use for noncancer pain. Am J Public Health. 2010;100:2541–7. doi: 10.2105/AJPH.2009.180646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Substance Abuse and Mental Health Services Administration and Center for Behavioral Health Statistics and Quality. The NSDUH Report: State Estimates of Nonmedical Use of Prescription Pain Relievers. Rockville, MD: Center for Behaviorial Health Statistics and Quality; Jan 8, 2013. [on 30 August 2013]. Accessed at www.samhsa.gov/data/2k12/NSDUH115/sr115-nonmedical-use-pain-relievers.htm. [Google Scholar]
- 17.Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. JAMA. 2013;309:657–9. doi: 10.1001/jama.2013.272. [DOI] [PubMed] [Google Scholar]
- 18.Calcaterra S, Glanz J, Binswanger IA. National trends in pharmaceutical opioid related overdose deaths compared to other substance related overdose deaths: 1999–2009. Drug Alcohol Depend. 2013;131:263–70. doi: 10.1016/j.drugalcdep.2012.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC) Vital signs: overdoses of prescription opioid pain relievers—-United States, 1999—2008. MMWR Morb Mortal Wkly Rep. 2011;60:1487–92. [PubMed] [Google Scholar]
- 20.Warner M, Chen LH, Makuc DM, Anderson RN, Miniño AM. Drug poisoning deaths in the United States, 1980–2008. Hyattsville, MD: National Center for Health Statistics; Dec, 2011. [on 30 August 2013]. Accessed at www.cdc.gov/nchs/data/databriefs/db81.htm. [Google Scholar]
- 21.Carson EA, Sabol WJ. Prisoners in 2011. Washington, DC: U.S. Department of Justice; Dec, 2012. [on 30 August 2013]. Bureau of Justice Statistics. Accessed at www.bjs.gov/content/pub/pdf/p11.pdf. [Google Scholar]
- 22.Binswanger IA, Merrill JO, Krueger PM, White MC, Booth RE, Elmore JG. Gender differences in chronic medical, psychiatric, and substance-dependence disorders among jail inmates. Am J Public Health. 2010;100:476–82. doi: 10.2105/AJPH.2008.149591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kariminia A, Law MG, Butler TG, Corben SP, Levy MH, Kaldor JM, et al. Factors associated with mortality in a cohort of Australian prisoners. Eur J Epidemiol. 2007;22:417–28. doi: 10.1007/s10654-007-9134-1. [DOI] [PubMed] [Google Scholar]
- 24.Binswanger IA, Blatchford PJ, Lindsay RG, Stern MF. Risk factors for all-cause, overdose and early deaths after release from prison in Washington state. Drug Alcohol Depend. 2011;117:1–6. doi: 10.1016/j.drugalcdep.2010.11.029. [DOI] [PubMed] [Google Scholar]
- 25.Binswanger IA, Nowels C, Corsi KF, Glanz J, Long J, Booth RE, et al. Return to drug use and overdose after release from prison: a qualitative study of risk and protective factors. Addict Sci Clin Pract. 2012;7:3. doi: 10.1186/1940-0640-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guerino PM, Harrison PM, Sabol WJ. Prisoners in 2010. Washington, DC: U.S. Department of Justice; Dec, 2011. [on 30 August 2013]. Bureau of Justice Statistics. Accessed at www.bjs.gov/content/pub/pdf/p10.pdf. [Google Scholar]
- 27.Bureau of Justice Statistics. What is the difference between jails and prisons? Washington, DC: U.S. Department of Justice; 2010. [on 30 August 2013]. Accessed at www.bjs.gov/index.cfm?ty=qa&iid=322. [Google Scholar]
- 28.Bilgrad R. NDIPlus: coded causes of death: supplement to the NDI user’s manual. Hyattsville, MD: National Center for Health Statistics; 1999. National Death Index. [Google Scholar]
- 29.Centers for Disease Control and Prevention. Wide-ranging online data for epidemiologic research (WONDER) Atlanta, GA: Centers for Disease Control and Prevention; Mar 1, 2012. [Google Scholar]
- 30.Lin D, Wei LJ, Ying Z. Checking the Cox model with cumulative sums of martingale-based residuals. Biometrika. 1993;80:557–72. [Google Scholar]
- 31.Lin DY, Wei LJ. The robust inference for the proportional hazards model. JASA. 1989;84:1074–8. [Google Scholar]
- 32.Cornish R, Macleod J, Strang J, Vickerman P, Hickman M. Risk of death during and after opiate substitution treatment in primary care: prospective observational study in UK General Practice Research Database. BMJ. 2010;341:c5475. doi: 10.1136/bmj.c5475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Merrall EL, Bird SM, Hutchinson SJ. A record-linkage study of drug-related death and suicide after hospital discharge among drug-treatment clients in Scotland, 1996–2006. Addiction. 2013;108:377–84. doi: 10.1111/j.1360-0443.2012.04066.x. [DOI] [PubMed] [Google Scholar]
- 34.Strang J, McCambridge J, Best D, Beswick T, Bearn J, Rees S, et al. Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow up study. BMJ. 2003;326:959–60. doi: 10.1136/bmj.326.7396.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McAuley A, Best D, Taylor A, Hunter C, Robertson R. From evidence to policy: The Scottish national naloxone programme. Drugs (Abingdon Engl) 2012;19:309–19. [Google Scholar]
- 36.World Health Organization. Prevention of acute drug-related mortality in prison populations during the immediate post-release period. Geneva: World Health Organization; 2010. p. 33. [Google Scholar]