Abstract
Genome-wide transcriptional analysis in intestinal epithelial cells (IEC) can aid in elucidating the impact of single versus multi-strain probiotic combinations on immunological and cellular mechanisms of action. In this study we used human expression microarray chips in an in vitro intestinal epithelial cell model to investigate the impact of three probiotic bacteria, Lactobacillus helveticus R0052 (Lh-R0052), Bifidobacterium longum subsp. infantis R0033 (Bl-R0033) and Bifidobacterium bifidum R0071 (Bb-R0071) individually and in combination, and of a surface-layer protein (SLP) purified from Lh-R0052, on HT-29 cells’ transcriptional profile to poly(I:C)-induced inflammation. Hierarchical heat map clustering, Set Distiller and String analyses revealed that the effects of Lh-R0052 and Bb-R0071 diverged from those of Bl-R0033 and Lh-R0052-SLP. It was evident from the global analyses with respect to the immune, cellular and homeostasis related pathways that the co-challenge with probiotic combination (PC) vastly differed in its effect from the single strains and Lh-R0052-SLP treatments. The multi-strain PC resulted in a greater reduction of modulated genes, found through functional connections between immune and cellular pathways. Cytokine and chemokine analyses based on specific outcomes from the TNF-α and NF-κB signaling pathways revealed single, multi-strain and Lh-R0052-SLP specific attenuation of the majority of proteins measured (TNF-α, IL-8, CXCL1, CXCL2 and CXCL10), indicating potentially different mechanisms. These findings indicate a synergistic effect of the bacterial combinations relative to the single strain and Lh-R0052-SLP treatments in resolving toll-like receptor 3 (TLR3)-induced inflammation in IEC and maintaining cellular homeostasis, reinforcing the rationale for using multi-strain formulations as a probiotic.
Introduction
In the past decade a number of studies have established important beneficial effects of probiotics that include alteration of gut microbiota, competitive adherence to gut epithelium, enhancement of the intestinal epithelial barrier function and immune modulation of various cell types of the gut-associated lymphoid tissue (GALT) [1,2]. One of the core properties of probiotic bacteria is their capacity to modulate innate and adaptive immune responses of different cell types of the GALT that include intestinal epithelial cells (IEC), mast cells (M cells), dendritic cells (DC), macrophages, T-cells and B-cells [3,4]. Several key immune pathways such as Jak/STAT, mitogen-activated protein kinase (MAPK) and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) signaling cascades have been implicated as possible sources behind the mechanism(s) of action of probiotics [5,6]. However, the elucidation of the exact mechanism(s) underlying how probiotic bacteria direct their beneficial effects on the host are not entirely understood [7].
Interestingly, studies have also established strain specific effects of probiotic bacteria on immune modulation and barrier function [8,9]. Moreover, a few studies that have compared single strains to multi-strain combinations have revealed, in some cases synergistic and in other situations antagonist, effects [9,10]. Preclinical assessment of blood samples from two distinct rat models of infection (TH1 and TH2) using single strains of Lh-R0052, Bl-R0033 and Bb-R0071 and the multi-strain probiotic combination of all 3 reported that the multi-strain synergistically benefited both TH1 and TH2 responses, but the mechanism(s) and the contribution of each strain was not elucidated [11].
Components of bacteria such as surface layer proteins (SLP) also influence several mechanisms including adhesion and are expressed by several probiotics including lactobacilli [12]. The receptor-binding region of the SLP from L. brevis adheres to gut epithelial cells, is transferrable to other non-adhesive LAB [13] and can also bind to blood type A-antigen found in the gut, aiding in intestinal colonization in humans [14]. In addition, in vitro application of SLP extracted from L. helveticus to epithelial cells (Hep-2 and T84) helps decrease adherence of E. coli O157:H7 [15]
Evidence from various studies suggests probiotics and SLP interact with pattern recognition receptors (PRRs) that include Toll-like receptors(TLR), nucleotide-binding oligomerization-like receptors (NOD-like receptors), adhesion molecules and lectins, in turn directing the modulation of key signaling pathways such as MAPK and NF-κB [1,4,16]. Studies of immune-modulation of TLR-mediated responses have mainly focused on the effects of different strains of Lactobacillus rhamnosus and include the differential expression of TLR genes in human primary macrophages [17], polarization of human monocyte-derived dendritic cells via TLR2 [18] and the attenuation of TLR4-induced signaling in Escherichia coli-challenged immune cells [19,20]. L. helveticus SLP acting through TLR2 in macrophages stimulates a pro-inflammatory response, while dampening NF-κB activation in intestinal epithelial cells [16], illustrating a different effect by bacterial components compared to whole bacteria at an immunological level on different cell types.
Relatively few studies have examined the effect probiotic strains have on TLR3-mediated immune responses. While most TLR primarily act through the MYD88-dependent pathway, TLR3, which detects dsRNA, triggers the MYD88-independent pathway. TLR3 activation does not involve the Toll/Interleukin 1-MYD88 interaction, but instead utilizes the adaptor protein TRIF (Toll/Interleukin 1 domain containing adaptor inducing IFN-β),-leading to IRF3-mediated transcriptional events. The MYD88-independent pathway also leads to the transcription of IFN-βinducible genes such as CXCL10 [21]. This difference in signaling from other TLR makes TLR3 an attractive PRR through which to study probiotic activity.
We have previously demonstrated through a custom-designed immune microarray analysis a multi-strain (Bl-R0033, Lh-R0052 and Bb-R0071) probiotic combination (PC) on TLR3-induced immune activation by polyinosinic:polycytidylic acid (poly(I:C)) in human intestinal epithelial cells attenuated TH1 pro-inflammatory response through the TLR3-TRIF, MAPK and NF-KB signaling pathways [22]. However, recent evidence also indicates a single probiotic strain, L. rhamnosus GG, can increase the expression of TLR3, specifically, in murine intestinal organoids [23], indicating a potential difference between single versus multi-strain probiotic combination on TLR3-related immune activity at the intestinal epithelial level.
The aim of this study was to elucidate the impact of the probiotic bacterial strains (Bl-R0033, Lh-R0052 and Bb-R0071) individually and in combination, and a specific surface-layer protein purified from Lh-R0052 (Lh-R0052-SLP), in response to TLR3-engagement in an in vitro IEC model. Genome-wide human expression microarrays were utilized to evaluate other cellular pathways beyond the immune-related pathways, especially in light of the benefits associated with probiotics on nervous, endocrine, stress-related behavior [24] and various gut inflammatory or autoimmune disorders [25,26].
Materials and Methods
Intestinal Epithelial Cell Culture
Human colon adenocarcinoma (HT-29) cells were purchased from American Type Culture Collection (ATCC #HTB-38, Cedarlane, Canada), and cultured in a suspension of RPMI-1640 media (HyClone, Logan, UT, USA) supplemented with 5% bovine calf serum, 5% fetal bovine serum and 2 mM L-glutamine (Invitrogen, Life Technologies). Cell cultures were grown in T75-cm2 tissue culture flasks (Corning Life Sciences, Acton, MA) at 37°C in a humidified, 5% CO2 incubator (Steri-cycle, ThermoFisher Scientific). Cultures were routinely passaged when they reached a confluence ~75–90% and used for subsequent challenge experiments between passages 8–22. For all challenge experiments, HT-29 cells were seeded at 2.5 x 106 cells and grown for 48 h in standard tissue-culture T25-cm2 flasks to reach a final total cell count of ~5 x 106 cells. Cells were washed with Dulbecco’s Phosphate Buffered Saline (DPBS) (HyClone, Logan, UT, USA) and incubated 30 min in serum-free RPMI prior to challenge assays.
Bacteria and Culture Conditions
Laboratory blend of the multi-strain bacteria referred to as multi-strain or probiotic combination, PC, was prepared using industrially prepared lyophilized bacterial powders (Lallemand Health Solutions Inc., Montreal, QC, Canada) of B. longum subsp. infantis R0033, B. bifidum R0071 and L. helveticus R0052 in a ratio of 20:20:60; respectively, and as described in MacPherson et al. [22]. To rehydrate the lyophilized bacteria for both single and multi-strain blend, 1 g was mixed for 15 min at room temperature (RT) in 99 mL of phosphate buffer [0.1% soy peptone (w/v), 0.121% K2HPO4 (w/v), 0.034% KH2PO4 (w/v)] as described in MacPherson et al. and Audy et al. [22,27]. Briefly, bacterial pellet from 1 ml of this bacterial suspension was washed in PBS after centrifugation at 12800 x g for 10 min at room temperature (RT) and then re-suspended in serum-free RPMI-1640 media. Individual bacteria and the multi-strain probiotic combination (PC) suspension was added to the culture flask (T25-cm2 flasks containing HT-29 cells) to have a multiplicity of infection (MOI) of 100:1 for bacteria to HT-29 cell ratio. Viable counts using reinforced clostridial agar (Oxoid) were performed on the bacterial suspension and incubated 48 h anaerobically at 37°C to confirm the calculated ratio.
Surface Layer Protein Extraction from L. helveticus R0052
Extraction of surface-layer protein from Lh-R0052 was performed with LiCl based extraction method as described in Johnson-Henry et al [15] and Taverniti et al [16]. Briefly, Lh-R0052 culture was grown overnight (16~18 hours) in anaerobic jars in 9 mL of MRS broth at 37°C. Overnight culture was transferred to 500 mL MRS broth and again incubated overnight in the same conditions. Bacterial culture (500 ml) was harvested in 50 mL Falcon tubes by centrifugation at 7,000 rpm for 10 min at 4°C, washed once with 1 volume of cold sterile distilled H2O and centrifuged again in same conditions. Bacterial cell pellet was re-suspended with 1M LiCl solution, incubated for 30 min at RT in the presence of protease inhibitor cocktail (0.001%; Sigma-Aldrich, St. Louis, MO) with slight agitation and centrifuged at 10,000 x g for 20 minutes at RT. The supernatant was discarded and the cell pellet was extracted for surface-layer protein with 5M LiCl solution for 1h at RT in the presence of protease inhibitor cocktail (0.001%) and centrifuged at 10,000 x g for 20 minutes at RT. The supernatant (containing surface-layer protein) was filtered through a 0.22 μm-pore-size filter and dialyzed for 24 h at 4°C against distilled H2O using 12 kDa cutoff membranes (Sigma-Aldrich). Dialysis tubing was prepared by boiling for 10 min in 2% NaHCO3 and 1mM EDTA solution. Dialysis tubing of ~20 cm in length was filled with ~20 mL of collected protein extract supernatant to dialyze sample in 4 L beaker filled with sterile distilled H2O to remove 5M LiCl at 4°C with periodic changing of the water. At each water change, 0.001% protease inhibitor cocktail was added. Once the dialysis was completed the samples were collected from the tubing and freeze-dried. Samples were stored at -20°C until later use. Protein concentration of extracted surface-layer protein from Lh-R0052 was determined by measuring on the Direct Detect® (EMD Millipore, Billerica, MA) spectrometer.
1D-SDS-PAGE and 2D-gel Analyses
LiCl extracted Lh-R0052-SLP preparations were assessed for correct molecular weight by running protein preparations on 15% SDS-PAGE precast Mini-Protean TGX gels (Bio-Rad; Cat. 456–1083). Briefly, 2, 4, and 8 μg of Lh-R0052-SLP preparation were added to 1X SDS loading dye, and incubated at 100°C for 10 min before loading on gel. SDS-PAGE gel was run for 1.5 hr at 120 volts, stained overnight with Bio-SafeTM Coomassie G-250 stain (Bio-Rad; Cat. 101–0786) and destained with distilled water. Aliquoted samples of Lh-R0052-SLP were also sent to Applied Biomics (www.appliedbiomics.com/) for 2D-difference gel electrophoresis (DIGE) to determine the isoelectric point and purity of the Lh-R0052-SLP. Both 1D SDS-PAGE and 2D-gel analysis showed that the Lh- R0052-SLP migrated to the expected molecular weight and isoelectric point of 48 kDa and 9.34; respectively, (S1 Fig) and was consistent with what was reported in Johnson-Henry et al. [15]. The purity of the LiCl extracted Lh-R0052-SLP preparation was further assessed on 2D-gel by probing with rabbit polyclonal antibody specific for Lh-R0052-SLP (available from Lallemand Health Solutions). The protein purity was calculated to be 99.12%. The equivalent amount of surface layer protein to be used in challenges with IEC was also determined by loading a known amount of bacterial cells onto 2D-gel and probing with the same rabbit polyclonal antibody that is specific for Lh-R0052-SLP (available from Lallemand Health Solutions Inc., Montreal). An equivalent amount of Lh-R0052-SLP protein based on 5 x 10E8 bacteria cells to have an equivalent MOI 100:1 was calculated to be 38μg/ml in a 5 ml culture of HT-29 cells.
HT-29 Cell Challenges
Cell challenges were performed as explained previously in MacPherson et al. and Audy et al. [22,27]. Briefly, HT-29 cells were co-challenged for 3h with either the single strains (Bl-R0033, Lh-R0052 or Bb-R0071) or probiotic combination (PC) alone or in combination with poly(I:C) at 10 μg/mL (Sigma; Cat. P1530). Lh-R0052-SLP challenges used alone or in combination with poly(I:C) were performed as previously described [22]. Challenges for cytokine and chemokine profiling were performed over 6h to allow for the accumulation of protein levels as described previously [27].
RNA Extraction and Dye-labeling
Total RNA isolation was performed on HT-29 cells using a phenol-based extraction method as described previously [22,27]. 15 μg of control and treated RNA was used for reverse transcription to cDNA and direct method of dye-labeling using Cy3-dCTP and Cy5-dCTP as described in MacPherson et al. [22].
Hybridization and Scanning
Genome-wide human expression microarrays version 2 were purchased from Agilent Technologies Inc. (GE 4x44K; G2519F). Briefly, Agilent array pre-hybridization, hybridization and post-hybridization were performed as previously described [22]. After post-hybridization, slides were scanned using ScanArray 5000 instrument from Perkin-Elmer (Waltham, MA) and spot intensities were quantified using ImaGene® version 9.0 (BioDiscovery).
Microarray Statistical Analysis
Global LOWESS normalization was conducted with ImaGene® microarray analysis software. Statistical analyses and two-dimensional hierarchical clustering analyses were performed with Multi-Experiment Viewer (MeV, version 4.9), a freely available bioinformatics analyses tool of the TM4 microarray software suite from the J. Craig Venter Institute [28]. Genes with changes in transcript abundance were selected on the basis of two criteria: (i) a t-test p-value of less than 0.05, which was considered statistically significant, and (ii) a cut-off in transcript abundance of least 1.5-fold change. Information regarding the microarray platform and the expression data files can be found on the NCBI Gene Expression Omnibus (GEO; http://www.ncbi.nlm.nih.gov/geo/) under GEO platform no. GPL10332 and GEO series no. GSE71515.
Set Distiller and String Analyses
Enrichment analyses of the genes modulated by each challenge or co-challenges were done using Set Distiller from GeneDecks version 3 [29] which ranks gene sets into attribute types (e.g., super pathways, KEGG pathways, compounds, phenotypes, expression and disorders) and descriptors (pathways) that best characterize the entire gene set. A p-value <0.05 was considered to be statistically significant for enrichment of pathways in Set Distiller (Bonferroni corrected). Interaction network maps were constructed using String version 9.1 [30] for selected pathways and disorders from the Set Distiller analyses to determine functional links between genes, verify the Set Distiller analyses and discover new relevant biological insights that had been overlooked.
Cytokine and Chemokine Profiling
Bio-Plex ProTM human cytokine and chemokine standards were serially diluted for the establishment of calibration curves for the determination of protein concentration as per the manufacturer’s instructions (Bio-Rad, Richmond, CA). All experiments were conducted with 4 biological replicates with 2 technical replications per biological replicate. All cytokine and chemokine measurements (TNF-α, IL-1β, IL-6, IL-8, CXCL1, CXCL2 and CXCL10) were multiplexed in the same 96-well plate. Bio-Plex ProTM software was used to determine the protein concentration using concentration in range and represented in pg/ml. Results were presented as the means ± SD of the replicate experiments. One-way ANOVA using Dunnett’s multiple comparisons test was performed with GraphPad version 6 to determine the statistical significance with the poly(I:C)-only challenge, compared to the co-challenges of Bl-R0033, Lh-R0052, Bb-R0071, Lh-R0052-SLP and PC. P-value <0.05 was considered to be statistically significant for each of the co-challenges and controls compared to the poly(I:C)-only challenge.
Results
Heat-map Analyses
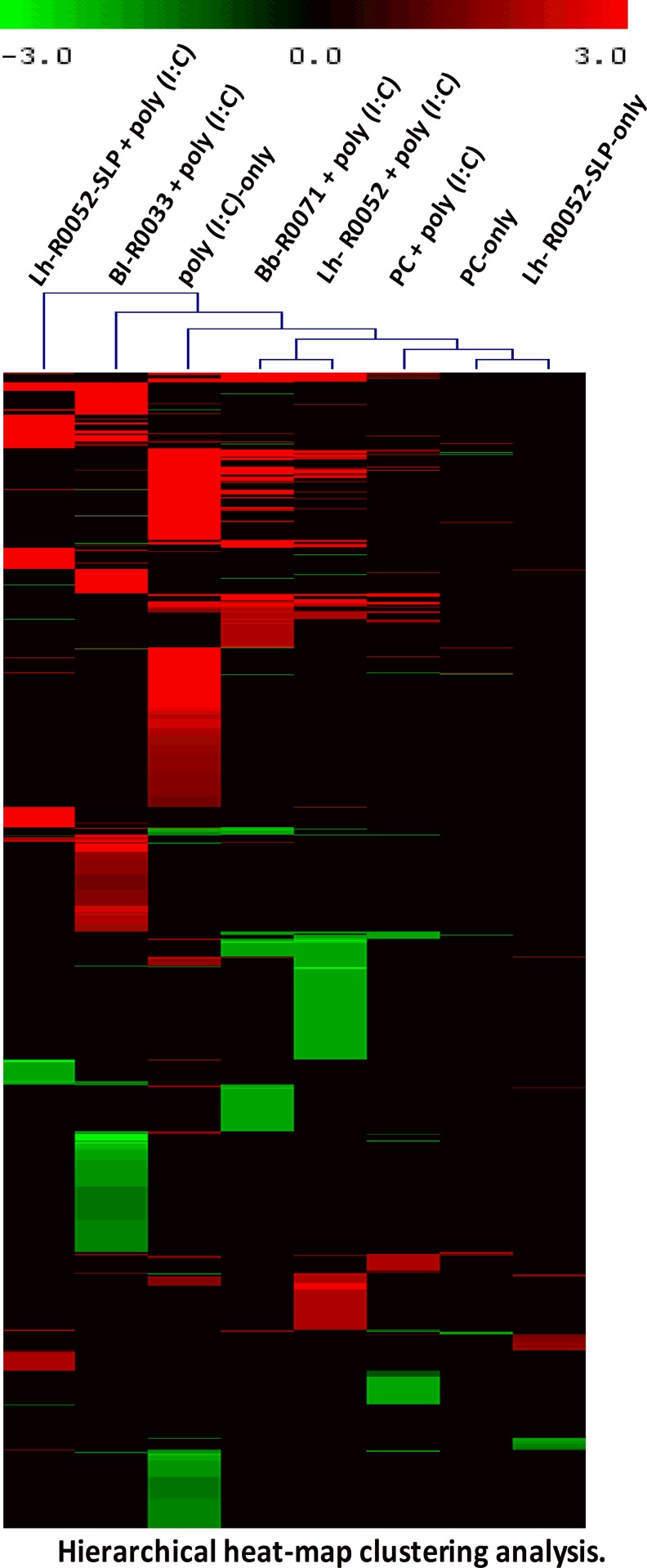
Genome-wide transcriptional analysis was used to investigate the transcriptional response of HT-29 cells co-challenged with individual bacterial strains (Bl-R0033, Lh-R0052 and Bb-R0071), probiotic combination (PC) and a purified Lh-R0052-SLP in the presence of the TLR3 inducer poly(I:C). Two-dimensional hierarchical clustering grouped individual challenges and differentially modulated genes into a clustering tree with similar expression profiles as depicted in Fig 1. The heat map analysis revealed a number of global observations from each of the challenges and co-challenges (Fig 1). The poly(I:C)-only challenge had the greatest impact on differential gene expression by modulating 607 genes, whereas the co-challenge with Bl-R0033, Lh-R0052, Bb-R0071, Lh-R0052-SLP or PC with poly(I:C) had a lower impact of modulating 467, 368, 293, 219 and 131 genes respectively (Table 1). The results indicated that the large number of genes that were differentially modulated by the poly(I:C)-only challenge were either attenuated or turned off by the probiotic co-challenges.
Fig 1. Two-dimensional hierarchical heat-map clustering analysis showing differentially modulated genes for each challenge and co-challenge of HT-29 cells.
Genes included in the heat map analysis were statistically significant with a p-value of <0.05 and a cut-off of 1.5-fold change in differential gene expression. Genes that were up-regulated are shown in red and down-regulated in green.
Table 1. Total number of up-regulated and down-regulated genes for each challenge and co-challenge.
All genes modulation are statistically significant with a p-value <0.05 and a cut-off of transcript abundance of 1.5-fold.
| Number of Genes Modulated | |||
|---|---|---|---|
| Challenges/Co-challenges | Up-regulated | Down-regulated | Total |
| poly(I:C)-only | 469 | 138 | 607 |
| Lh-R0052-SLP + poly(I:C) | 175 | 44 | 219 |
| Bl-R0033 + poly(I:C) | 268 | 199 | 467 |
| Bb-R0071 + poly(I:C) | 170 | 123 | 293 |
| Lh-R0052 + poly(I:C) | 167 | 200 | 367 |
| PC + poly(I:C) | 60 | 71 | 131 |
| PC-only | 7 | 10 | 17 |
| R0052-SLP-only | 30 | 18 | 48 |
The individual bacterial co-challenges had strain specific effects on gene modulation. Each single strain induced unique gene modulation not observed with the other co-challenges (Fig 1). Co-challenge with Lh-R0052-SLP also had a unique impact on gene modulation compared to the other co-challenges. Although each of the individual bacteria and Lh-R0052-SLP had a positive effect on attenuating global gene expression, the multi-strain PC had the greatest impact. The PC reduced the number of modulated genes from 607 to 131 genes (Table 1). Without prior poly(I:C) stimulation, the PC-only and Lh-R0052-SLP-only challenges modulated only 17 and 47 genes; respectively.
Set Distiller Enrichment Analysis
In order to have a better understanding of what pathways were modulated and what genes were implicated, enrichment analysis was performed using the bioinformatics tool Set Distiller from GeneDeck. As previously explained, Set Distiller takes gene sets and categorizes descriptors (pathways) that best characterize a particular gene set [29]. The results of the enrichment analyses for each of the challenges were placed into pathways that corresponded to immune, cellular signaling, compound, virus, endocrine/nervous and disorder related (Tables 2 and 3). The enrichment analyses illustrated that there were numerous pathways associated with cellular signaling. Notable pathways related to cellular signaling included homeostasis/metabolism, PAK pathway, focal adhesion, and apoptosis signaling pathway (Table 2). Overall, results revealed that the poly(I:C)-only challenge had a greater impact on this model system, as evident by the larger number of pathways and the total number of genes modulated. For example, the poly(I:C)-only challenge exhibited a greater impact on gene modulation for immune related pathways such as TNF-α (16), Jak-STAT (7), MAPK (21), NF-κB family pathway (17), cytokine-cytokine receptor interaction (16) and chemokine (13), Immune response IL23 (12), IL-17 family (9) and Toll-like receptor (8) signaling pathways. Examples of pro-inflammatory genes that were up-regulated by poly (I:C)-only in these immune pathways included TNF-α (32.4-fold), RELB (11.3-fold), IL-8 (7.2-fold), CXCL1, (5.7-fold) CXCL2 (4.6-fold), CXCL3 (4.2-fold), CXCL10 (2.6-fold) and LIF (2.0-fold) (S1 Table). The up-regulation of these genes confirmed previously reported data using a customized Immune Array [22]. Furthermore, there was a progressive reduction in the total number of genes for a number of pathways for the single strains and Lh-R0052-SLP; with the multi-strain PC showing the greatest impact at reducing the number of genes induced by poly(I:C)-only (Tables 2 and 3; S1 Table).
Table 2. Enrichment analysis using Set Distiller analysis from GeneDecks (version 3) showing descriptors/pathways and the number of genes modulated for immune, compound and cellular related pathways.
Enrichment analysis of pathways are statistically significant with a p-value <0.05 (Bonferroni corrected).
| GeneDecks Set Distiller Analysis | Attribute Type | poly(I:C) | Lh-R0052 | Bb-R0071 | Bl-R0033 | Lh-R0052-SLP | PC | PC | Lh-R0052-SLP |
|---|---|---|---|---|---|---|---|---|---|
| only | poly(I:C) | poly(I:C) | poly(I:C) | poly (I:C) | poly(I:C) | only | only | ||
| Immune Related | Number of Genes Modulated | ||||||||
| Immune System Phenotype | PHENOTYPE | 88 | 85 | 77 | 59 | 32 | 22 | - | - |
| TNF Signaling Pathway | KEGG_PATHWAY | 16 | 12 | 14 | - | - | - | - | - |
| MAPK Signaling Pathway | SUPER_PATHWAY | 21 | 16 | 14 | 6 | - | 4 | - | - |
| NF-KappaB Signaling Pathway | KEGG_PATHWAY | 13 | 14 | 12 | 4 | 3 | 7 | - | - |
| NF-KappaB Family Pathway | SUPER_PATHWAY | 17 | 13 | 11 | - | - | 1 | - | - |
| Jak-STAT Signaling Pathway | SUPER_PATHWAY | 7 | 1 | 2 | - | 3 | 1 | - | - |
| Immune response IFN Alpha/Beta Signaling Pathway | SUPER_PATHWAY | 8 | - | - | - | - | - | - | - |
| Cytokine-cytokine Receptor Interaction | KEGG _PATHWAY | 16 | 16 | 12 | 8 | 7 | 7 | - | - |
| Chemokine Signaling | KEGG_PATHWAY | 13 | 14 | 6 | - | 6 | 6 | - | - |
| Toll-like receptor Signaling Pathway | KEGG_PATHWAY | 8 | 12 | 11 | 2 | 2 | 4 | - | - |
| IL-17 Family Signaling Pathways | SUPER_PATHWAY | 9 | 2 | 4 | - | - | - | - | - |
| Immune Response IL-23 Signaling Pathway | SUPER_PATHWAY | 12 | 3 | 5 | - | - | 3 | - | - |
| NOD-like Receptor Signaling Pathway | SUPER_PATHWAY | 16 | 3 | 4 | 2 | 2 | 5 | - | - |
| RIG-I-like Receptor Signaling Pathway | KEGG_PATHWAY | 6 | 4 | 4 | - | - | 4 | - | - |
| Inactivation of MAPK Activity | GO_MOLEC_FUNC | - | 6 | - | - | - | - | - | - |
| BAFF in B-Cell Signaling | SUPER_PATHWAY | 4 | 9 | 8 | - | - | - | - | - |
| Immune Response MIF-mediated Glucocorticoid Regulation | PATHWAY_MLPR | 6 | 6 | 8 | - | - | 3 | - | - |
| Immune Response IL-2 Activation and Signaling Pathway | SUPER_PATHWAY | 7 | 9 | 7 | - | - | - | - | - |
| Compound/Immune Related | |||||||||
| VEGF | COMPOUND | 34 | 41 | 38 | 36 | 12 | 14 | - | - |
| Rantes | COMPOUND | 18 | - | 15 | - | - | 8 | - | - |
| Nitric Oxide | COMPOUND | 33 | 36 | 29 | 29 | - | 11 | - | - |
| H2O2 | COMPOUND | 32 | 11 | 27 | 22 | - | 10 | - | - |
| Progesterone | COMPOUND | 33 | 10 | - | 25 | 14 | 8 | - | - |
| Superoxide | COMPOUND | 18 | - | - | 20 | 3 | 6 | - | - |
| Histamine | COMPOUND | 13 | - | - | 16 | - | - | - | - |
| Cellular/Signaling Related | |||||||||
| Homeostasis/Metabolism Phenotype | PHENOTYPE | 107 | 100 | 80 | 74 | 37 | 24 | - | - |
| Signal Transduction | GO_BIOL_PROC | 51 | - | 24 | 30 | - | 13 | - | - |
| PAK Pathway | SUPER_PATHWAY | 37 | - | 19 | - | - | - | - | - |
| Focal Adhesion | PATHWAT_KEGG | 10 | - | 12 | 9 | - | - | - | - |
| Cell Adhesion | GO_BIOL_PROC | 20 | 19 | - | 18 | - | - | - | - |
| p53 Signaling Pathway | SUPER_PATHWAY | 7 | - | 10 | - | - | - | - | - |
| Apoptosis Signaling | SUPER_PATHWAY | 20 | 9 | 6 | - | - | 4 | - | - |
| Integrin Pathway | SUPER_PATHWAY | 15 | 20 | 17 | - | - | - | - | - |
| EGFR1 Signaling Pathway | SUPER_PATHWAY | - | 11 | - | - | - | - | - | - |
| PI3K-Akt signaling Pathway | SUPER_PATHWAY | 12 | 16 | 6 | 10 | 3 | 1 | - | - |
Table 3. Enrichment analysis using Set Distiller analysis from GeneDecks (version 3) showing descriptors/pathways and the number of genes modulated for virus, nervous and disorder related pathways.
Enrichment analysis of pathways are statistically significant with a p-value <0.05 (Bonferroni corrected).
| GeneDecks Set Distiller Analysis | Attribute Type | poly(I:C) | Lh-R0052 | Bb-R0071 | Bl-R0033 | Lh-R0052-SLP | PC | PC | Lh-R0052-SLP |
|---|---|---|---|---|---|---|---|---|---|
| only | poly(I:C) | poly(I:C) | poly(I:C) | poly(I:C) | poly(I:C) | only | only | ||
| Virus Related | Number of Genes Modulated | ||||||||
| Influenza | DISORDER | 11 | 27 | - | 8 | - | - | - | - |
| Virus infection | DISORDER | 24 | 20 | 20 | - | - | 8 | - | - |
| Defense Response to Virus | GO_BIOL_PROC | 13 | - | - | - | - | - | - | - |
| Influenza A | SUPER_PATHWAY | 20 | 15 | - | - | - | - | - | - |
| Response to Virus | GO_BIOL_PROC | 14 | - | - | - | - | - | - | - |
| Type 1 Interferon Signaling Pathway | GO_BIOL_PROC | 8 | - | - | - | - | - | - | - |
| poly I:C | COMPOUND | 8 | 8 | 6 | - | - | - | - | - |
| Interferon-alpha | COMPOUND | 7 | - | - | - | - | - | - | - |
| 2,5-oligoadenylate | COMPOUND | 7 | - | - | - | - | - | - | - |
| Nervous/Endocrine Related | |||||||||
| Nervous System Phenotype | PHENOTYPE | 66 | 83 | 59 | 66 | 37 | - | - | - |
| Behavior/Neurological Phenotype | PHENOTYPE | 61 | 57 | 48 | 49 | 28 | - | - | - |
| Endocrine/Exocrine Gland Phenotype | PHENOTYPE | 47 | 55 | 33 | 37 | 15 | 12 | - | - |
| Disorder Related | |||||||||
| Necrosis | DISORDER | 70 | 67 | 56 | 53 | 20 | 23 | - | - |
| Inflammation | DISORDER | 60 | 53 | 49 | 40 | 21 | 22 | - | - |
| Inflammatory Bowel Disease | DISORDER | 15 | 26 | 20 | 10 | 9 | - | - | - |
| Rheumatoid Arthritis | DISORDER | 27 | 62 | 53 | - | - | - | - | - |
| Multiple Sclerosis | DISORDER | 15 | 39 | 35 | - | 8 | - | - | - |
| Obesity | DISORDER | 14 | 36 | - | - | - | - | - | - |
| Autoimmune Disease | DISORDER | 15 | - | - | 15 | - | - | - | - |
| Gastritis | DISORDER | 9 | - | 18 | - | - | - | - | - |
A secondary aim of this study was to evaluate other potentially interesting genes and go beyond the immune-related pathways that were previously reported in MacPherson et al. [22] by using genome-wide microarrays. Of particular interest was the capacity of Set Distiller enrichment to integrate gene function into disorder-related pathways. Examples included inflammation, inflammatory bowel disease, rheumatoid arthritis, multiple sclerosis, obesity and autoimmune diseases (Table 3). The enrichment analyses also revealed that there were a number of shared genes found in many of the disorder pathways (Table 3). The majority of these shared genes were associated with pro-inflammatory substances such as cytokines and chemokines that were also present in immune and inflammatory responses. Examples of such substances included chemokine (C-X-C motif) ligand 1 (CXCL1), CXCL2, CXCL3, CXCL10, CXCL11, intercellular adhesion molecule 1 (ICAM1), interleukin 23 alpha subunit (IL-23A), IL-17C, IL-26, IL-8, interferon receptor 2 (IFNAR2), leukemia inhibitory factor (LIF) and tumor necrosis factor-alpha (TNF-α).
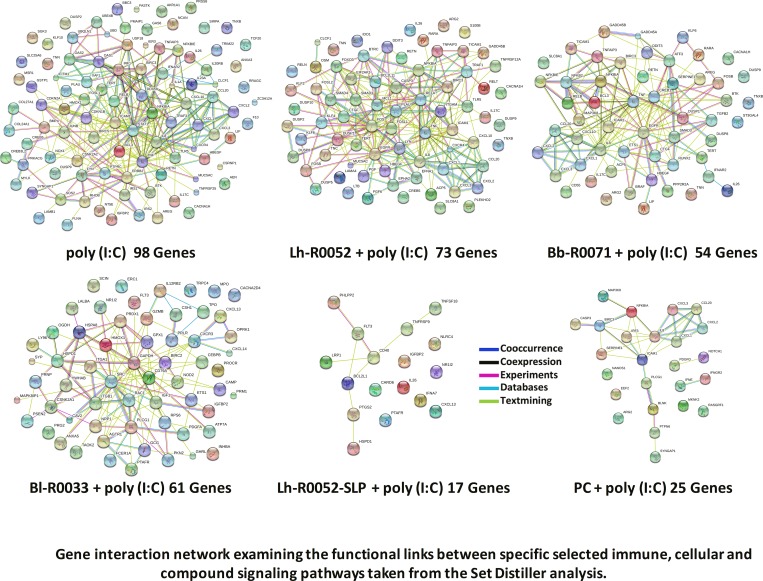
Gene Interaction Network: String Analysis
Enrichment was followed up for selected immune pathways, compound and cellular pathways to construct a gene interaction network map. String 9.1 was used to build this map and to determine functional links between genes. It was also used to confirm the Set Distiller analyses and elucidate potentially interesting functional links of genes that may have been previously overlooked. The String analysis was specified to look at the functional links of pathways involved in innate immunity and inflammation with a few cellular and compound pathways. This was done in order to make the functional link between innate immunity, inflammation, cellular signaling and compound to better elucidate, in part, the complex probiotic gene modulation that is exhibited by the single strains, multi-strain, PC, and Lh-R0052-SLP (Fig 2). It was evident from the analysis that there was, in fact, much overlap between genes in different pathway attributes. Many genes found in these respective linked pathways were also found in the disorders (Table 3) that are characterized by inflammation. The inflammation and inflammatory bowel disease (IBD) disorders had many commonly modulated genes that were also found in the String analysis that were common with the disorders which included IL-8, ICAM1, RELB, NFκBIA, TNFAIP3, LIF, CXCL1, CXCL2, CXCL3, CXCL10, and TNF-α.
Fig 2. Gene interaction network map (String 9.1) examining the functional links between genes in specific immune, cellular and compound signaling pathways taken from the Set Distiller analysis.
Selected pathways included apoptosis, NF-κB, MAPK, Jak-STAT, immune response IFN-alpha/beta, toll-like receptor, IL-17 family, immune response IL-23, RIG-I-like receptor, cytokine-cytokine receptor interaction, NOD-like signaling, nitric oxide, superoxide and histamine.
One particular gene that stood out in the String analyses was IL-17C in the inflammation disorder (Table 3) that does not show up in the TNF, MAPK and NF-κB signaling pathways. In the Set Distiller analyses, IL-17C was only present in the immune system phenotype and IL-17 family signaling pathway (Table 2). When gene sets were analyzed with Set Distiller there was no other placement of this particular gene. Through the String analyses, IL-17C has functional links (Fig 2) to a key pro-inflammatory gene TNF-α, in turn having functional links to CXCL1 and IL-23A (Fig 2), which are associated with the majority of disorder-related pathways. The use of complementary cross-enrichment analysis tools (Set Distiller and String) can be applied to extract useful functional insights or links of genes such as IL-17C and IL-23A that are important in the pro-inflammatory response of immunity and autoimmune or metabolic disorders. Another notable cytokine that was found was IL-26, which has a functional link to IFNAR2, in turn having a functional link with IL-23A (Fig 2). IL-26 may also prove to be an important marker to monitor in immunity and inflammation as revealed in these results.
Cytokine and Chemokine Profiling
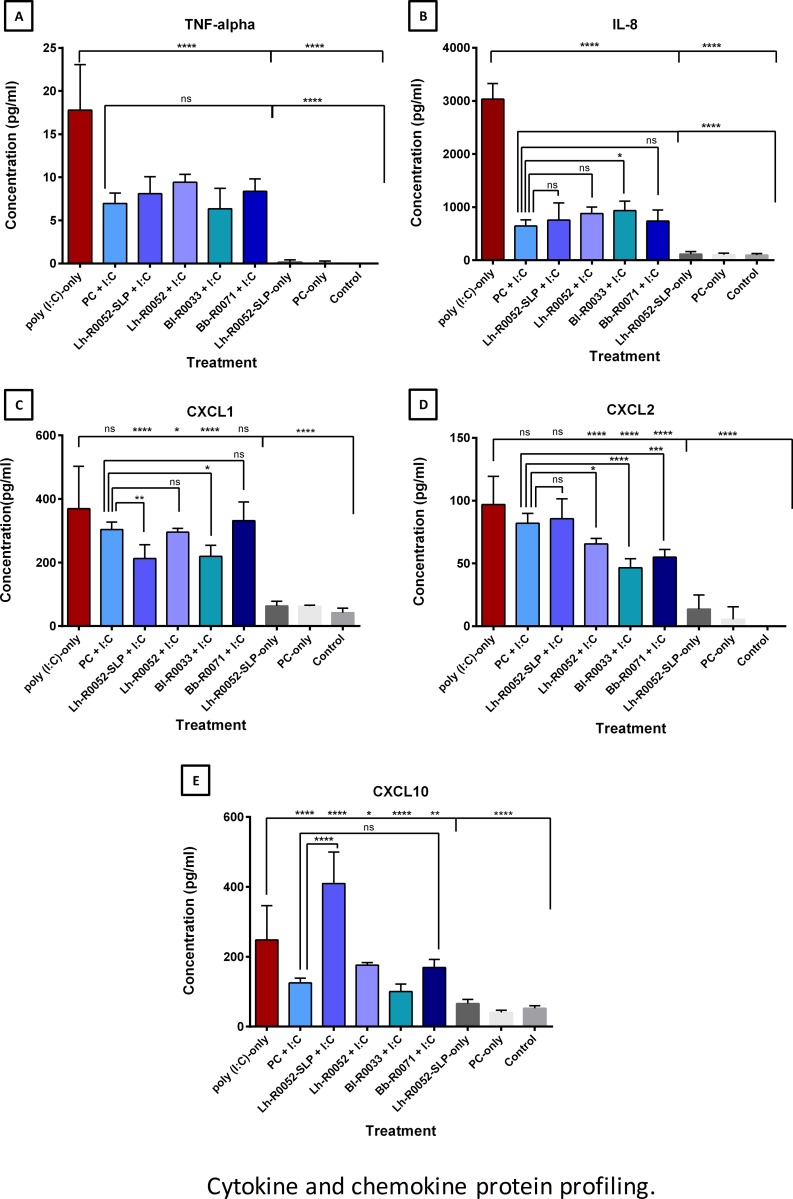
Mapping out specifically where gene modulation lies in the TNF and NF-κB signaling pathway allowed a rational approach to selecting endpoints or markers to measure at the protein level. A core set of chemokines and cytokines were chosen as end points. This included CXCL1, CXCL2, CXCL10 and TNF-α from the TNF pathway and IL-8 from the NF-κB signaling pathway. Protein levels of selected pro-inflammatory markers were analyzed using a fluorescent-magnetic-bead-based multiplex immunoassay. The results of Fig 3A and 3B for TNF-α, a key pro-inflammatory marker, and IL-8, a potent chemotactic factor that attracts neutrophils, basophils and T cells, showed a statistically significant (p<0.001) attenuation for each single strain, Lh-R0052-SLP and multi-strain PC co-challenges compared to poly(I:C)-only. Although there was more attenuation in the PC co-challenge for TNF-α and IL-8 compared to the single strains and Lh-R0052-SLP, the difference was not statistically significant. However, for IL-8 there was more attenuation for PC co-challenge compared to Bl-R0033 co-challenge (Fig 3B; p<0.05).
Fig 3.
Cytokine and chemokine protein profiling for HT-29 cells challenges and co-challenges for (A) TNF-α, (B) IL-8, (C) CXCL1, (D) CXCL2 and (E) CXCL10. Results were presented as the means ± SD of the replicate experiments (biological replicates n = 4; with 2 technical replicates each). One-way ANOVA using Dunnett’s multiple comparisons test was performed with GraphPad version 6 to determine the statistical significance with the pro-inflammatory stimulus, poly(I:C)-only and PC plus poly(I:C), p-values: *: p<0.05, **:p<0.01, ***: p<0.001, **** p<0.0001 and ns = not statistically significant.
The chemokine markers CXCL1, CXCL2 and CXCL10, that are involved in leukocyte recruitment, revealed strain, PC and Lh-R0052-SLP specific attenuation (Fig 3C, 3D and 3E). For example, PC and Bb-R0071 did not significantly attenuate CXCL1 compared to the poly(I:C)-only; whereas the co-challenge of Lh-R0052-SLP (p<0.0001), Lh-R0052 (p<0.05) and Bl-R0033 (p<0.0001) did (Fig 3C). The results of CXCL2 revealed that PC and Lh-R0052-SLP co-challenges did not significantly attenuate CXCL2 protein levels compared to the poly(I:C)-only challenge; whereas Lh-R0052 (p<0.05), Bl-R0033 (p<0.001) and Bb-R0071 (p<0.001) co-challenges were all significantly attenuated (Fig 3D). All three single strains and the PC significantly attenuated CXCL10 compared to poly(I:C)-only (Fig 3E), while Lh-R0052-SLP co-challenge significantly increased CXCL10 levels compared to poly(I:C)-only. Protein measured for the negative control markers IL-1β and IL-6 revealed no detectable protein modulation for all the challenges, confirming, as expected, the microarray expression data.
Discussion
IEC act as a physical barrier and the first line of defense against pathogens and pathogen-associated molecular patterns (PAMPs) at the gut mucosal level and are an active participant in the host-microbiota cross-talk [31]. Recognition of potential threats and communication with the microbiota can occur via varied IEC signaling receptors [32]. Immune responses to PAMPs initiated at the IEC level activate immune cells, including macrophages, dendritic cells and B cells in the underlying gut associated-lymphoid tissues [33], leading to resolution of inflammation and the return to homeostasis. Intake of a specific strain or combination of bacteria and/or metabolic activity linked to these bacteria can attenuate TLR-activated innate immune responses by IEC [34]. However, few studies have established the efficacy of single strain versus multi-strain combinations on modulating TLR-induced inflammation in IEC. In this study, we utilized genome-wide microarray analysis to expand upon our previous findings with the custom-made immune array [22,27,35] and demonstrate distinct mechanistic differences at the expression level between single and the multi-strain probiotic combination on a broad range of immune and cellular pathways in poly(I:C)-challenged IEC.
The heat map and Set Distiller analyses revealed a number of key insights on the global impact of single strain (Bl-R0033, Lh-R0052 or Bb-R0071), probiotic combination (PC), and surface layer protein (Lh-R0052-SLP) on TLR-3 induced activation in IEC by poly(I:C). Both analyses reinforced that the strain specific and Lh-R0052-SLP effects differed from PC co-challenge. The effects of Lh-R0052 and Bb-R0071 diverged from that of Bl-R0033 and Lh-R0052-SLP, while PC modulation contrasted sharply with either grouping (Fig 1; Tables 2 and 3). Although the heat map analysis showed strain-based clustering, overall the effect of each probiotic treatment was quite different. It was evident from the global analyses with respect to the immune, cellular and homeostasis related pathways that there was a reduction in the total number of genes and pathways modulated by the single strains or Lh-R0052-SLP (Table 2). More specifically, the co-challenge with PC resulted in a substantial decrease in modulated genes and pathways, suggesting that the bacterial combination had a synergistic effect. Work performed by Chapman et al. [9] which investigated in vitro models of single and multi-strain probiotics on pathogen inhibition found that combinations had significantly greater inhibition of pathogens (e.g., Clostridium difficile, Escherichia coli and Salmonella typhimurium). The authors concluded that multi-strain formulations may be more effective at reducing gastrointestinal infections than single strain components [9]. Although the work by Chapman and co-workers used different in vitro models and pathogens, the results support the positive benefit of using multi-strain versus single strain preparations.
The enrichment analyses of the expression data using Set Distiller (Tables 2 and 3) in conjunction with String analysis (Fig 2) highlighted the overlap and functional connections between immune and cellular pathways. The findings demonstrated differences in the potential mechanisms by which single strain, Lh-R0052-SLP or PC co-challenge affected poly(I:C)-mediated inflammation in IEC. For example, the expression of TLR5 and the mucin gene MUC5AC increased in poly(I:C)-challenged IEC and their expression was unaffected by the presence of Lh-R0052. Increased TLR5 expression in TLR3-activated IEC is indicative of PRR cross-activation. The MYD88-TRIF adaptor cross-talk has been shown to synergize the immune response in the presence of TLR3 and TLR4 or TLR9 ligands and can act as a secondary signal to help the host evaluate an appropriate response to an immune challenge [36,37]. In contrast to Lh-R0052, Lh-R0052-SLP co-challenge increased the expression of the inflammasome component NLRC4 (NLR family, CARD domain containing 4), demonstrating purified components from a probiotic strain can differ in their mechanism of action from whole bacteria.
The effect on gene expression in single strain Bl-R0033 co-challenged IEC was uniquely different from the other probiotic treatments. Firstly, Bl-R0033 up-regulated expression of genes LY96 HSPA8 and NOD2, all of which assist with LPS-mediated inflammation. LY96 encodes for a protein which associates with TLR4, while HSPA8, a heat-shock protein, binds to LPS [38]. NOD-2 is a pattern recognition receptor found in the cytoplasm and recognizes peptidoglycans from both Gram positive and Gram negative bacteria [39]. Bifidobacteria can bind to LPS and while certain strains can inhibit LPS-induced NF-κB activation [40], this inhibitory effect is not universal across all strains [41]. However, as LPS was not used as a stimulant in the current study, the increased expression of LPS-associated genes indicates Bl-R0033 may precondition IEC to LPS presence during TLR3 activation.
In addition to the overlap in expression of genes involved in innate immune signaling, Bl-R0033 co-challenge also up-regulated CD79, which encodes for a B cell receptor component, and CXCL13, known to induce B cell homing to lymph nodes [38]. Although co-challenge with Bl-R0033 did not modulate B cell activating factor (BAFF) pathway genes, studies have shown B. animalis lactis Bb12 along with L. rhamnosus GG to secrete A Proliferation-Inducing Ligand (APRIL) from IEC [42]. APRIL and BAFF are cytokines that stimulate B cells to produce IgA in a T cell-independent manner [43]. Taken together, these findings suggest Bl-R0033 may, in TLR3-activated IEC, promote IEC-B cell communication at the gut mucosal level.
Genes involved in the attenuation of inflammatory signals were differentially expressed in single strain, PC and Lh-R0052-SLP co-challenge IEC. Both Lh-R0052 and Bb-R0071 co-challenge increased the expression of DUSP9, which encodes for a MAP kinase inhibitor, while Lh-R0052-SLP up-regulated BCL2L11, which inhibits NLRC4 inflammasome activation [38]. Taverniti et al. showed that L. helveticus MIMLh5 surface-layer protein (SLP) induced anti-inflammatory effects by attenuating NF-κB activation in IEC, specifically Caco-2 cells [16]. These findings highlight that the effect of SLP is not only strain-specific, but that the possible mechanisms involved in dampening inflammation differ between probiotic components and whole bacteria.
The PC co-challenge gene expression profile demonstrated potential cross-inhibitory activity. The probiotic combination possibly attenuated TLR3-mediated inflammation in IEC by down regulating genes IRF3 (downstream marker of TRIF), while up regulating genes NFκBIA (inhibitor of NF-κB/REL complex) and SYNGAP1 (inhibitory regulator of Ras-cAMP pathway) [38]. Multiple ligand engagement induces signals that cross-inhibit, leading to dampening of the inflammatory response [44] and may explain the PC effect on gene modulation. We also noted a significant decrease in protein levels of pro-inflammatory cytokine TNF-α and chemokines IL-8 and CXCL10 relative to poly(I:C)-challenged IEC and these possibly reflect PC-induced changes to the inflammation-associated gene expression profile. These findings agree with a previous preclinical assessment of the single strains and multi-strain combinations using two distinct rat models (TH1 and TH2) of infection which concluded that immune-modulation of TH1 and TH2 responses favored homeostatic rebalancing [11].
Further to attenuating inflammation, the PC co-challenge also modulated apoptosis-associated genes in our IEC model. Expression of CASP3, which initiates apoptosis, was down-regulated, while the gene BIRC3, an inhibitor of apoptosis, was up-regulated in PC co-challenged IEC. These genes were also modulated in the same manner in Lh-R0052 co-challenged IEC. In contrast, Lh-R0052-SLP down-regulated CARD6, which stimulates inflammasome-mediated apoptosis. Apoptosis can result from high levels of nitric oxide production [45] and TLR-mediated inflammation in IEC have been noted to be pro-oxidative, with TLR3 activation reducing the activity of super oxide dismutase [46]. However, the expression of the gene ARG2 was down-regulated; indicating possible suppression of nitric oxide synthesis in Lh-R0052, Bb-R0071 and PC co-challenged IEC. In contrast, the expression of PTAFR, which is important for superoxide formation, increased in Bl-R0033 and Lh-R0052-SLP co-challenged IEC. Although Bl-R0033 co-challenge did not modulate the expression of genes in the apoptosis pathway, the increased expression of PTFAR highlights the complexity of the interaction of differing probiotic treatments at the cellular and immune level. Overall the functional link analysis (Fig 2) of immune and cellular gene pathways suggest that PC may attenuate TLR3-activated inflammation in IEC in a multi-pronged fashion, an approach that differed completely from single strains and Lh-R0052-SLP co-challenges.
The transcriptional analyses also revealed other cellular signaling, nervous and endocrine related disorders (Table 3). It has been widely reported in the literature that many cytokine and chemokine genes (e.g., TNF-a, IL-8, CXCL2, CXCL3, CXCL10, LIF, IL-17C and IL-23A) are the basis of autoimmune disorder pathways that are characterized by inflammation. For example, Yamaguchi et al. reported that IL-17C stimulates the production of TNF-α, in turn increasing inflammatory rheumatoid arthritis, and suggested that IL-17C may have a key role in the pathogenesis of arthritis [47]. Other reports have implicated IL-17 in various autoimmune diseases such as multiple sclerosis and inflammatory bowel diseases [48]. In addition, other studies have also reported that IL-17C and IL-23A are key cytokines of TH17 responses that are involved in regulating innate immune functions and gut inflammation of IEC [49,50]. The fact that these particular cytokines were induced by the poly(I:C)-only challenge, and attenuated or turned off with the multi-strain PC, implies that these may be potential markers to follow in future probiotic clinical studies of these disorder-related diseases.
Overall the findings reveal a distinct pattern of gene modulation by single strains and Lh-R0052-SLP compared to the probiotic combination in TLR3-activated IEC. The genome-wide expression analysis demonstrated the probiotic combination modulated the least number of genes and through a highly regulated process attenuated TLR3-mediated inflammation in IEC, implying a synergistic effect at the expression level. Our findings highlight potential immune-modulatory mechanisms and biomarkers to follow in the rational design of future pre-clinical and clinical probiotic studies.
Supporting Information
(TIF)
All genes were statistically significant with a p-value<0.05 and a cut-off fold change in transcript abundance of 1.5-fold.
(XLSX)
All genes were significant with a p-value <0.05 and cut-off fold change in transcript abundance of 1.5-fold.
(XLSX)
Acknowledgments
The authors would like to thank Dr. Andre Nantel for his expertise and input in data mining analyses of the human genome-wide microarray analyses.
Data Availability
Information regarding the microarray platform and the expression data files can be found on the NCBI Gene Expression Omnibus (GEO; http://www.ncbi.nlm.nih.gov/geo/) under GEO platform no. GPL10332 and GEO series no. GSE71515.
Funding Statement
This project was funded in its entirety by Lallemand Health Solutions Inc. The funding organization did not play a role in the study design, data collection and analysis, decision to publish or preparation of the manuscript and only provided financial support in the form of authors’ salaries and/or research materials. Moreover, all final research decisions were made by the Research Director of Lallemand Health Solutions Inc., Dr. Thomas Allan Tompkins, one of the author(s) of this manuscript. The funder Lallemand Health Solutions Inc. only provided financial support in the form of authors’ salaries and/or research materials.
References
- 1.Plaza-Diaz J, Gomez-Llorente C, Fontana L, Gil A (2014) Modulation of immunity and inflammatory gene expression in the gut, in inflammatory diseases of the gut and in the liver by probiotics. World J Gastroenterol 20: 15632–15649. 10.3748/wjg.v20.i42.15632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wan LY, Chen ZJ, Shah NP, El-Nezami H (2015) Modulation of Intestinal Epithelial Defense Responses by Probiotic Bacteria. Crit Rev Food Sci Nutr: 0. [DOI] [PubMed] [Google Scholar]
- 3.O'Flaherty S, Klaenhammer TR (2012) Influence of exposure time on gene expression by human intestinal epithelial cells exposed to Lactobacillus acidophilus. Appl Environ Microbiol 78: 5028–5032. 10.1128/AEM.00504-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gomez-Llorente C, Munoz S, Gil A (2010) Role of Toll-like receptors in the development of immunotolerance mediated by probiotics. Proc Nutr Soc 69: 381–389. 10.1017/S0029665110001527 [DOI] [PubMed] [Google Scholar]
- 5.Thomas CM, Versalovic J (2010) Probiotics-host communication: Modulation of signaling pathways in the intestine. Gut Microbes 1: 148–163. 10.4161/gmic.1.3.11712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bermudez-Brito M, Plaza-Diaz J, Munoz-Quezada S, Gomez-Llorente C, Gil A (2012) Probiotic mechanisms of action. Ann Nutr Metab 61: 160–174. 10.1159/000342079 [DOI] [PubMed] [Google Scholar]
- 7.Sherman PM, Ossa JC, Johnson-Henry K (2009) Unraveling mechanisms of action of probiotics. Nutr Clin Pract 24: 10–14. 10.1177/0884533608329231 [DOI] [PubMed] [Google Scholar]
- 8.Presti I, D'Orazio G, Labra M, La Ferla B, Mezzasalma V, et al. (2015) Evaluation of the probiotic properties of new Lactobacillus and Bifidobacterium strains and their in vitro effect. Appl Microbiol Biotechnol. [DOI] [PubMed] [Google Scholar]
- 9.Chapman CM, Gibson GR, Rowland I (2012) In vitro evaluation of single- and multi-strain probiotics: Inter-species inhibition between probiotic strains, and inhibition of pathogens. Anaerobe 18: 405–413. 10.1016/j.anaerobe.2012.05.004 [DOI] [PubMed] [Google Scholar]
- 10.Chapman CM, Gibson GR, Rowland I (2011) Health benefits of probiotics: are mixtures more effective than single strains? Eur J Nutr 50: 1–17. 10.1007/s00394-010-0166-z [DOI] [PubMed] [Google Scholar]
- 11.Cazzola M, Tompkins TA, Matera MG (2010) Immunomodulatory impact of a synbiotic in T(h)1 and T(h)2 models of infection. Ther Adv Respir Dis 4: 259–270. 10.1177/1753465810379009 [DOI] [PubMed] [Google Scholar]
- 12.Kahala M, Savijoki K, Palva A (1997) In vivo expression of the Lactobacillus brevis S-layer gene. J Bacteriol 179: 284–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avall-Jaaskelainen S, Lindholm A, Palva A (2003) Surface display of the receptor-binding region of the Lactobacillus brevis S-layer protein in Lactococcus lactis provides nonadhesive lactococci with the ability to adhere to intestinal epithelial cells. Appl Environ Microbiol 69: 2230–2236. 10.1128/AEM.69.4.2230-2236.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uchida H, Kinoshita H, Kawai Y, Kitazawa H, Miura K, et al. (2006) Lactobacilli binding human A-antigen expressed in intestinal mucosa. Res Microbiol 157: 659–665. 10.1016/j.resmic.2006.03.001 [DOI] [PubMed] [Google Scholar]
- 15.Johnson-Henry KC, Hagen KE, Gordonpour M, Tompkins TA, Sherman PM (2007) Surface-layer protein extracts from Lactobacillus helveticus inhibit enterohaemorrhagic Escherichia coli O157:H7 adhesion to epithelial cells. Cell Microbiol 9: 356–367. 10.1111/j.1462-5822.2006.00791.x [DOI] [PubMed] [Google Scholar]
- 16.Taverniti V, Stuknyte M, Minuzzo M, Arioli S, De Noni I, et al. (2013) S-layer protein mediates the stimulatory effect of Lactobacillus helveticus MIMLh5 on innate immunity. Appl Environ Microbiol 79: 1221–1231. 10.1128/AEM.03056-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miettinen M, Veckman V, Latvala S, Sareneva T, Matikainen S, et al. (2008) Live Lactobacillus rhamnosus and Streptococcus pyogenes differentially regulate Toll-like receptor (TLR) gene expression in human primary macrophages. J Leukoc Biol 84: 1092–1100. 10.1189/jlb.1206737 [DOI] [PubMed] [Google Scholar]
- 18.Konieczna P, Schiavi E, Ziegler M, Groeger D, Healy S, et al. (2015) Human dendritic cell DC-SIGN and TLR-2 mediate complementary immune regulatory activities in response to Lactobacillus rhamnosus JB-1. PLoS One 10: e0120261 10.1371/journal.pone.0120261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu M, Wu Q, Wang M, Fu Y, Wang J (2016) Lactobacillus rhamnosus GR-1 Limits Escherichia coli-Induced Inflammatory Responses via Attenuating MyD88-Dependent and MyD88-Independent Pathway Activation in Bovine Endometrial Epithelial Cells. Inflammation 39: 1483–1494. 10.1007/s10753-016-0382-7 [DOI] [PubMed] [Google Scholar]
- 20.Bermudez-Brito M, Munoz-Quezada S, Gomez-Llorente C, Romero F, Gil A (2014) Lactobacillus rhamnosus and its cell-free culture supernatant differentially modulate inflammatory biomarkers in Escherichia coli-challenged human dendritic cells. Br J Nutr 111: 1727–1737. 10.1017/S0007114513004303 [DOI] [PubMed] [Google Scholar]
- 21.Takeda K, Akira S (2004) TLR signaling pathways. Semin Immunol 16: 3–9. [DOI] [PubMed] [Google Scholar]
- 22.Macpherson C, Audy J, Mathieu O, Tompkins TA (2014) Multistrain probiotic modulation of intestinal epithelial cells' immune response to a double-stranded RNA ligand, poly(i.c). Appl Environ Microbiol 80: 1692–1700. 10.1128/AEM.03411-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aoki-Yoshida A, Saito S, Fukiya S, Aoki R, Takayama Y, et al. (2016) Lactobacillus rhamnosus GG increases Toll-like receptor 3 gene expression in murine small intestine ex vivo and in vivo. Benef Microbes 7: 421–429. 10.3920/BM2015.0169 [DOI] [PubMed] [Google Scholar]
- 24.Ait-Belgnaoui A, Colom A, Braniste V, Ramalho L, Marrot A, et al. (2014) Probiotic gut effect prevents the chronic psychological stress-induced brain activity abnormality in mice. Neurogastroenterol Motil 26: 510–520. 10.1111/nmo.12295 [DOI] [PubMed] [Google Scholar]
- 25.Bonaz BL, Bernstein CN (2013) Brain-gut interactions in inflammatory bowel disease. Gastroenterology 144: 36–49. 10.1053/j.gastro.2012.10.003 [DOI] [PubMed] [Google Scholar]
- 26.Dinan TG, Stanton C, Cryan JF (2013) Psychobiotics: a novel class of psychotropic. Biol Psychiatry 74: 720–726. 10.1016/j.biopsych.2013.05.001 [DOI] [PubMed] [Google Scholar]
- 27.Audy J, Mathieu O, Belvis J, Tompkins TA (2012) Transcriptomic response of immune signalling pathways in intestinal epithelial cells exposed to lipopolysaccharides, Gram-negative bacteria or potentially probiotic microbes. Benef Microbes 3: 273–286. 10.3920/BM2012.0027 [DOI] [PubMed] [Google Scholar]
- 28.Saeed AI, Sharov V, White J, Li J, Liang W, et al. (2003) TM4: a free, open-source system for microarray data management and analysis. Biotechniques 34: 374–378. [DOI] [PubMed] [Google Scholar]
- 29.Stelzer G, Inger A, Olender T, Iny-Stein T, Dalah I, et al. (2009) GeneDecks: paralog hunting and gene-set distillation with GeneCards annotation. OMICS 13: 477–487. 10.1089/omi.2009.0069 [DOI] [PubMed] [Google Scholar]
- 30.Franceschini A, Szklarczyk D, Frankild S, Kuhn M, Simonovic M, et al. (2013) STRING v9.1: protein-protein interaction networks, with increased coverage and integration. Nucleic Acids Res 41: D808–815. 10.1093/nar/gks1094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Neish AS (2002) The gut microflora and intestinal epithelial cells: a continuing dialogue. Microbes Infect 4: 309–317. [DOI] [PubMed] [Google Scholar]
- 32.Wells JM, Rossi O, Meijerink M, van Baarlen P (2011) Epithelial crosstalk at the microbiota-mucosal interface. Proc Natl Acad Sci U S A 108 Suppl 1: 4607–4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abreu MT (2010) Toll-like receptor signalling in the intestinal epithelium: how bacterial recognition shapes intestinal function. Nat Rev Immunol 10: 131–144. 10.1038/nri2707 [DOI] [PubMed] [Google Scholar]
- 34.de Kivit S, Tobin MC, Forsyth CB, Keshavarzian A, Landay AL (2014) Regulation of Intestinal Immune Responses through TLR Activation: Implications for Pro- and Prebiotics. Front Immunol 5: 60 10.3389/fimmu.2014.00060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ho NK, Hawley SP, Ossa JC, Mathieu O, Tompkins TA, et al. (2013) Immune signalling responses in intestinal epithelial cells exposed to pathogenic Escherichia coli and lactic acid-producing probiotics. Benef Microbes 4: 195–209. 10.3920/BM2012.0038 [DOI] [PubMed] [Google Scholar]
- 36.Suet Ting Tan R, Lin B, Liu Q, Tucker-Kellogg L, Ho B, et al. (2013) The synergy in cytokine production through MyD88-TRIF pathways is co-ordinated with ERK phosphorylation in macrophages. Immunol Cell Biol 91: 377–387. 10.1038/icb.2013.13 [DOI] [PubMed] [Google Scholar]
- 37.Liu Q, Zhu Y, Yong WK, Sze NS, Tan NS, et al. (2015) Cutting Edge: Synchronization of IRF1, JunB, and C/EBPbeta Activities during TLR3-TLR7 Cross-Talk Orchestrates Timely Cytokine Synergy in the Proinflammatory Response. J Immunol 195: 801–805. 10.4049/jimmunol.1402358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stelzer G, Dalah I, Stein TI, Satanower Y, Rosen N, et al. (2011) In-silico human genomics with GeneCards. Hum Genomics 5: 709–717. 10.1186/1479-7364-5-6-709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tlaskalova-Hogenova H, Tuckova L, Mestecky J, Kolinska J, Rossmann P, et al. (2005) Interaction of mucosal microbiota with the innate immune system. Scand J Immunol 62 Suppl 1: 106–113. [DOI] [PubMed] [Google Scholar]
- 40.Riedel CU, Foata F, Philippe D, Adolfsson O, Eikmanns BJ, et al. (2006) Anti-inflammatory effects of bifidobacteria by inhibition of LPS-induced NF-kappaB activation. World J Gastroenterol 12: 3729–3735. 10.3748/wjg.v12.i23.3729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Park MS, Kim MJ, Ji GE (2007) Assessment of lipopolysaccharide-binding activity of Bifidobacterium and its relationship with cell surface hydrophobicity, autoaggregation, and inhibition of interleukin-8 production. J Microbiol Biotechnol 17: 1120–1126. [PubMed] [Google Scholar]
- 42.Kandasamy S, Chattha KS, Vlasova AN, Rajashekara G, Saif LJ (2014) Lactobacilli and Bifidobacteria enhance mucosal B cell responses and differentially modulate systemic antibody responses to an oral human rotavirus vaccine in a neonatal gnotobiotic pig disease model. Gut Microbes 5: 639–651. 10.4161/19490976.2014.969972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cerutti A (2008) The regulation of IgA class switching. Nat Rev Immunol 8: 421–434. 10.1038/nri2322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thaiss CA, Levy M, Itav S, Elinav E (2016) Integration of Innate Immune Signaling. Trends Immunol 37: 84–101. 10.1016/j.it.2015.12.003 [DOI] [PubMed] [Google Scholar]
- 45.Dijkstra G, van Goor H, Jansen PL, Moshage H (2004) Targeting nitric oxide in the gastrointestinal tract. Curr Opin Investig Drugs 5: 529–536. [PubMed] [Google Scholar]
- 46.Latorre E, Mendoza C, Layunta E, Alcalde AI, Mesonero JE (2014) TLR2, TLR3, and TLR4 activation specifically alters the oxidative status of intestinal epithelial cells. Cell Stress Chaperones 19: 289–293. 10.1007/s12192-013-0461-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yamaguchi Y, Fujio K, Shoda H, Okamoto A, Tsuno NH, et al. (2007) IL-17B and IL-17C Are Associated with TNF- Production and Contribute to the Exacerbation of Inflammatory Arthritis. The Journal of Immunology 179: 7128–7136. [DOI] [PubMed] [Google Scholar]
- 48.Shabgah AG, Fattahi E, Shahneh FZ (2014) Interleukin-17 in human inflammatory diseases. Postepy Dermatol Alergol 31: 256–261. 10.5114/pdia.2014.40954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Monteleone I, Pallone F, Monteleone G (2009) Interleukin-23 and Th17 cells in the control of gut inflammation. Mediators Inflamm 2009: 297645 10.1155/2009/297645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ramirez-Carrozzi V, Sambandam A, Luis E, Lin Z, Jeet S, et al. (2011) IL-17C regulates the innate immune function of epithelial cells in an autocrine manner. Nat Immunol 12: 1159–1166. 10.1038/ni.2156 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
All genes were statistically significant with a p-value<0.05 and a cut-off fold change in transcript abundance of 1.5-fold.
(XLSX)
All genes were significant with a p-value <0.05 and cut-off fold change in transcript abundance of 1.5-fold.
(XLSX)
Data Availability Statement
Information regarding the microarray platform and the expression data files can be found on the NCBI Gene Expression Omnibus (GEO; http://www.ncbi.nlm.nih.gov/geo/) under GEO platform no. GPL10332 and GEO series no. GSE71515.