Abstract
Objectives
The aim of this study was to characterize the neuropsychological profile of lifetime traumatic brain injury (TBI) in older Veterans.
Methods
Participants were 169 older Veterans [mean age = 79.1 years (range, 51–97 years), 89% male, 92% Caucasian], 88 with lifetime TBI and 81 without TBI, living in Veterans’ retirement homes in independent residence. TBI history was ascertained with the Ohio State TBI Identification Method structured interview. Cognition was assessed with neuropsychological tests: Raw scores were converted to Z-scores compared to age-corrected normative data and combined into five domain composite Z-scores (attention/working memory, learning/memory, language, processing speed, executive functioning). We investigated the association between TBI and performance in each cognitive domain in linear mixed effects models, with and without adjustment for demographics, medical comorbidities, and psychiatric variables.
Results
Compared to those without TBI, older Veterans with TBI had greater deficits in processing speed (estimate = −.52; p = .01; f2 = .08 in fully adjusted model) and executive functioning (estimate = −.41; p = .02; f2 = .06 in fully adjusted model) but performed similarly in the attention/working memory, learning/memory, and language domains (all p >.05). TBI-associated deficits were most prominent among individuals with multiple mild TBIs and those with any moderate-to-severe TBI, but were not clearly present among those with single mild TBI.
Conclusions
The neuropsychological profile of lifetime TBI in older Veterans is characterized by slowed processing speed and executive dysfunction, especially among those with greater injury burden. This pattern may reflect long-standing deficits or a TBI-associated cognitive decline process distinct from Alzheimer’s disease.
Keywords: Traumatic brain injury, Head injury, Aging, Veterans, Cognition, Cognitive deficits
INTRODUCTION
Epidemiological studies have identified traumatic brain injury (TBI) as a risk factor for dementia (Perry et al., 2015; Plassman & Grafman, 2015). Not only are individuals who sustain TBI in older adulthood at high risk for dementia (Gardner et al., 2014), but there is evidence of long-term associations such that individuals who experienced TBI earlier in life are at increased risk of developing mild cognitive impairment (MCI) (Guskiewicz et al., 2005) and dementia (Barnes et al., 2014; Plassman et al., 2000) in late life. Despite this evidence, the profile of cognitive deficits that may be present among older adults with a lifetime history of TBI remains unclear. Investigation of whether lifetime TBI is associated with deficits in specific cognitive abilities in aging may clarify what type of dementia process is most likely to occur among older adults with TBI, and perhaps elucidate potential targets for intervention or prevention efforts.
Most research examining the effect of TBI on specific cognitive abilities has been conducted among younger to middle-aged adults. From such studies, it is clear that individuals with recent TBI may exhibit deficits in a variety of cognitive domains, including problems with executive functioning (McDonald, Flashman, & Saykin, 2002; Rochat, Ammann, Mayer, Annoni, & Linden, 2009), attention (Chan, 2005), working memory (McAllister, Flashman, McDonald, & Saykin, 2006), processing speed (Mathias, Beall, & Bigler, 2004), and memory (Curtiss, Vanderploeg, Spencer, & Salazar, 2001). In the months to initial years following a TBI, individuals tend to experience at least some cognitive improvement over time (Finnanger et al., 2013; Schretlen & Shapiro, 2003), and some, particularly those with mild TBI, may experience complete cognitive recovery (Karr, Areshenkoff, & Garcia-Barrera, 2014; Schretlen & Shapiro, 2003). These patterns of cognitive stability or improvement following recent TBI contrast with findings of long-term associations between lifetime TBI and the development of dementia in late life.
The few studies (Ashman et al., 2008; Dams-O’Connor et al., 2013; Himanen et al., 2006) that have addressed the effect of lifetime and/or remote TBI on specific cognitive abilities in older adulthood have produced mixed findings and have had important methodological limitations. For example, a study by Dams-O’Connor et al. (2013) compared dementia patients with and without a history of TBI to evaluate differences in the clinical features of dementia between these groups; although this study compared cognitive performance between groups, cognitive results are difficult to interpret as specific to TBI when both groups, by definition, already had cognitive impairment rising to the level of dementia. Other studies have not accounted for medical or psychiatric comorbidities when examining the association between TBI and late-life cognition. This is an important limitation because comorbidities are relatively common in individuals with TBI (Scholten et al., 2016) and are known to have important effects on cognition in aging (Byers & Yaffe, 2011; Qiu & Fratiglioni, 2015; Yaffe et al., 2010).
Our group is conducting the Brain Aging in Veterans (BRAVE) study to investigate the long-term effects of TBI in aging, by comparing groups of older Veterans with and without a lifetime history of TBI (Peltz et al., 2016). TBI is a particularly common injury among military personnel (Okie, 2005; Ommaya, Ommaya, Dannenberg, & Salazar, 1996; Raymont, Salazar, Krueger, & Grafman, 2011; Sayer, 2012); thus older Veterans are an important population among which to investigate this question. For the present study, we aimed to characterize the neuropsychological profile of lifetime TBI in aging, by comparing neuropsychological functioning between older Veterans with and without TBI in the BRAVE study. Because they share many similarities with older Veterans with TBI, older Veterans without TBI serve as an important comparison group for the BRAVE study.
However, it should be noted that this comparison group is not representative of a typical “healthy control” group. Other risk factors for cognitive impairment, such as cardiovascular risk factors and prior psychiatric and substance abuse conditions, are relatively common among older Veterans without TBI (Peltz et al., 2016). Therefore, in the present study, we aimed to first evaluate the extent to which each participant group in the BRAVE study exhibited neuropsychological deficits compared to healthy older adult norms. Then, we examined whether and how neuropsychological profiles differed between groups. Given that cognitive risk factors were present in both groups, we hypothesized that older Veterans with and without TBI would show cognitive deficits compared to normative data, but that older Veterans with TBI would show a different profile of deficits. We also hypothesized that cognitive deficits would be more extensive among older Veterans with greater TBI history burden (i.e., among those with multiple mild TBIs or any moderate or severe TBI).
METHODS
Population
Participants were older Veterans (≥50 years old) with and without a lifetime history of TBI from the Brain Aging in Veterans (BRAVE) study. For the BRAVE study, Veterans were recruited from one of two Veteran’s retirement homes: the Armed Forces Retirement Home in Washington, DC and the Veterans Home of California-Yountville in Yountville, California. Recruitment and eligibility criteria for the BRAVE study have been described previously (Peltz et al., 2016). In brief, to be included in the BRAVE study, individuals were required to score ≥20 on the Mini-Mental State Examination (Folstein, Folstein, & McHugh, 1975) to help ensure they were cognitively capable of providing informed consent. Individuals were also required to be residents of the independent-living sections of their retirement home; to reside in independent-living, the facilities required individuals to be functionally independent and free of active substance abuse.
To be included in the TBI group, participants were required to self-report ≥1 head injury over their lifetime that required medical care, and TBI history was further assessed as detailed below. To be included in the non-TBI group, participants were required to self-report no significant head injury history. Individuals with penetrating TBI, disabling medical or psychiatric conditions, or significant sensory limitations were excluded from the study. The BRAVE study was approved by institutional review boards at each site, all participants provided written informed consent, and all data were obtained in compliance with institutional regulations. All participants were informed during the informed consent process that there would be no direct benefit to them from study participation, other than their contribution to the gain of research knowledge.
Measures
TBI History
Detailed TBI history was ascertained using the Ohio State University TBI Identification Method (OSU TBI-ID) (Bogner & Corrigan, 2009; Corrigan & Bogner, 2007), a structured interview recommended by the National Institute of Neurological Disorders and Stroke (NINDS) as a Common Data Element (CDE) for the retrospective assessment of lifetime TBI in clinical research [National Institute of Neurological Disorders and Stroke (NINDS), 2012]. During the OSU TBI-ID, participants were asked to self-report the TBI(s) they had experienced over their lifetime, including age of injury, injury cause, presence and length of loss of consciousness (LOC), and yes/no response to “were you dazed or did you have a gap in your memory from the injury?” indicating alteration in consciousness or post-traumatic amnesia (PTA).
Each injury was classified as a (1) Mild TBI if an individual experienced an alteration in consciousness or PTA without LOC or LOC <30 min, (2) Moderate TBI if LOC ≥ 30 min but <24 hr, or (3) Severe TBI if LOC ≥ 24 hr (Department of Veterans Affairs & Department of Defense, 2009). Medical charts available at participants’ retirement home were reviewed to corroborate history of TBI to the extent possible. Of individuals in the present study, 41% in the TBI group had TBI documented in their retirement home charts, while none of the individuals in the non-TBI group had TBI in their charts.
Cognitive functioning
Participants completed a comprehensive neuropsychology battery, an expanded version of the Alzheimer’s Disease Centers’ Uniform Data Set battery (Weintraub et al., 2009). This battery was comprised of measures assessing cognitive functioning in five domains: (1) attention/working memory, (2) learning/memory, (3) language, (4) processing speed, and (5) executive functioning. Specifically, measures of attention/working memory included the Wechsler Memory Scale-Revised (WMS-R) Digit Span Forward and Backwards (Wechsler, 1987) and the Working Memory Factor score from the National Institutes of Health - Executive Abilities: Measures and Instruments for Neurobehavioral Evaluation and Research (NIH-EXAMINER) battery (Kramer et al., 2014b). The Auditory Verbal Learning Task (AVLT) (Rey, 1941; Taylor, 1959) was used to assess learning/memory, including AVLT Learning Trials (total trials 1–5), AVLT Delayed Recall, and AVLT Recognition total. Language was assessed using the Boston Naming Test—30 item version (Kaplan, Goodglass, & Weintraub, 1983) and Animal Fluency (Morris et al., 1989). Measures of processing speed included Trail Making Test Part A (Reitan & Wolfson, 1985) and Wechsler Adult Intelligence Scale-Revised (WAIS-R) Digit Symbol (Wechsler, 1981). Executive functioning was assessed with the Trail Making Test Part B (Reitan & Wolfson, 1985), and the NIH-EXAMINER battery Fluency Factor and Cognitive Control Factor scores (Kramer et al., 2014b).
Other variables
Participants self-reported their age, race, sex, education, military service history, and cigarette smoking status. Comorbidities, including hypertension, myocardial infarction, stroke, diabetes, and history of mental health conditions and substance abuse were determined via a combination of participant self-report and chart review. Current psychiatric symptoms were assessed via self-report inventories. Namely, depressive symptoms were assessed with the Geriatric Depression Scale—Short Form (GDS) (Yesavage et al., 1983), a 15-item inventory of yes/no questions with a score >5 being suggestive of clinical depression. Current symptoms of post-traumatic stress disorder (PTSD) were assessed with the PTSD Checklist—Civilian version (PCL-C) (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996), for which a score ≥36 may be suggestive of significant PTSD among Veterans in general settings (U.S. Department of Veterans Affairs & National Center for PTSD, 2014).
Statistical Analysis
We compared participant characteristics between individuals in the TBI group versus the non-TBI group using t tests for continuous variables and chi-square tests or Fisher’s exact tests for categorical variables, as well as Cohen’s d and Phi coefficients as effect size measures in correspondence with these tests. To evaluate whether the TBI and non-TBI groups differed in terms of their neuropsychological profile, we first compared each participant’s raw cognitive test scores to age-corrected normative data for each measure [Mayo’s Older Americans Normative Studies (MOANS) age-corrected norms for AVLT Learning Trials (Ivnik et al., 1990) and Delayed Recall and Recognition (Ivnik et al., 1992); age-corrected norms for the NIH EXAMINER battery (Kramer et al., 2014a); and Alzheimer’s Disease Centers’ Uniform Data Set age-corrected norms (Shirk et al., 2011) for the remaining measures], similar to standard practice in clinical neuropsychological evaluations.
Using these normative data, we converted each individual’s raw test scores into age-corrected Z-scores, reflecting the extent to which an individual’s test performance diverges from that of healthy, age-matched peers. To minimize multiple comparisons, individuals’ Z-scores for individual tests within a cognitive domain were averaged to create five cognitive domain composite scores: attention/working memory, learning/memory, language, processing speed, and executive functioning composites. Thus, these composites reflect the extent to which an individual’s overall performance within a cognitive domain diverges from that of healthy, age-matched peers.
We conducted linear mixed effects model analyses, using SAS PROC MIXED, to investigate the association between TBI and performance on the cognitive domain composite scores. These models accounted for study site (participants nested within site) as a random effect. We conducted these models with and without addition of covariates. We first adjusted for demographics (age, gender, race, education) and a binary variable indicating whether or not participants had any of the following medical comorbidities/health factors (hypertension, myocardial infarction, stroke, diabetes, or current smoking). Then, we additionally adjusted for a binary variable indicating whether or not participants had a history of any of the following psychiatric or substance use conditions (depression, anxiety, PTSD, bipolar disorder, or substance abuse), as well as their current level of psychiatric symptoms (i.e., GDS and PCL-C scores for depressive and PTSD symptoms, respectively). For each of these models, we calculated Cohen’s f2 values from SAS PROC MIXED using procedures outlined in Selya, Rose, Dierker, Hedeker, and Mermelstein (2012), reflecting the effect size for the association between TBI and each cognitive domain composite score, unadjusted or adjusted for covariates.
To explore whether the association between TBI and neuro-psychological functioning differs depending on details of an individual’s injury history, we created a four-level categorical variable to classify participants based on whether they had a single mild TBI, multiple mild TBIs (i.e., individuals who self-reported multiple head injuries that each met criteria for mild TBI as detailed in the “TBI History” section above), or at least one TBI that was moderate-to-severe in severity, compared to individuals without TBI. Using linear trend tests, we investigated the effect of TBI history category (no TBI, single mild TBI, multiple mild TBI, or any moderate-to-severe TBI) on the cognitive domain composite scores. These analyses were conducted by using the ESTIMATE statement in PROC MIXED to specify a test of linear trend across the four-level TBI variable (coefficients: −3 −1 1 3). All analyses were conducted in SAS version 9.4, and p-values <.05 were considered statistically significant.
RESULTS
As previously reported in the BRAVE study (Peltz et al., 2016), Veteran participants with and without lifetime TBI were generally similar in terms of demographics and most medical comorbidities, although Veterans with TBI were more likely to be Caucasian and to have diabetes (see Table 1). Veterans with TBI were also more likely to have a history of depression and substance abuse and endorsed greater current depressive symptoms and current PTSD symptoms compared to those without TBI (see Table 1). Nevertheless, few individuals in either group endorsed current psychiatric symptoms that exceeded clinical cut-offs on the symptom inventory measures [% individuals with GDS >5: TBI = 9.1% (n = 8), non-TBI = 2.5% (n = 2); % individuals with PCL-C ≥ 36: TBI = 6.8% (n = 6), non-TBI = 1.2% (n = 1)]. Regarding details of Veterans’ lifetime exposure to TBI, individuals’ TBI histories were quite heterogeneous.
Table 1.
Demographics and other participant characteristics
| Mean (SD) or % | Non-TBI (n = 81) | TBI (n = 88) | Test statistic | p-Value | Effect size |
|---|---|---|---|---|---|
| Demographics | |||||
| Age, years | 80.3 (8.6) | 77.9 (10.3) | t(167) = 1.63 | .11 | d = .25 |
| Gender, % males | 85.2% | 92.1% | Χ2(1) = 1.99 | .16 | φ = .11 |
| Race, % minority | 13.6% | 2.3% | Fisher’s exact test | .008* | φ = −.21 |
| Education, years | 14.6 (2.6) | 14.4 (2.7) | t(167) = .63 | .53 | d = .08 |
| Military Service, years | 10.7 (8.8) | 10.7 (9.1) | t(162) = −.02 | .98 | d = .00 |
|
| |||||
| TBI history | |||||
| Injury number/severity: | |||||
| Single mild TBI | — | 22.7% | — | — | — |
| Multiple mild TBIs | — | 46.6% | — | — | — |
| Any moderate-to-severe TBI | — | 30.7% | — | — | — |
| Age at first TBI, years | — | 26.2 (21.9) | — | — | — |
| Time since most recent TBI, years | — | 33.0 (24.7) | — | — | — |
|
| |||||
| Medical History | |||||
| Hypertension | 79.0% | 75.6% | Χ2(1) = .28 | .60 | φ = −.04 |
| Myocardial infarction | 10.4% | 11.8% | Χ2(1) = .08 | .78 | φ = .02 |
| Stroke | 11.1% | 14.0% | Χ2(1) = .31 | .58 | φ = .04 |
| Diabetes | 22.2% | 36.8% | Χ2(1) = 4.25 | .04* | φ = .16 |
| Current smoking | 18.5% | 12.6% | Χ2(1) = 1.11 | .29 | φ = −.08 |
|
| |||||
| Psychiatric history/substance abuse history | |||||
| Depression | 20.0% | 43.5% | Χ2(1) = 10.46 | .001* | φ = .25 |
| Anxiety | 15.0% | 23.0% | Χ2(1) = 1.72 | .19 | φ = .10 |
| PTSD | 8.9% | 15.3% | Χ2(1) = 1.58 | .21 | φ = .09 |
| Bipolar disorder | 3.7% | 7.0% | Fisher’s exact test | .50 | φ = .07 |
| Substance abuse | 18.5% | 43.7% | Χ2(1) = 12.30 | <.001* | φ = .27 |
|
| |||||
| Current psychiatric symptoms | |||||
| Depressive symptoms (GDS) | 1.0 (1.5) | 1.9 (2.7) | t(140.7) = −2.66 | .009* | d = −.41 |
| PTSD symptoms (PCL-C) | 19.5 (6.3) | 22.8 (8.3) | t(161.5) = −2.92 | .004* | d = −.45 |
| Global cognition MMSE | 28.3 (1.5) | 27.6 (2.6) | t(143.76) = 2.01 | .046* | d = .33 |
Note. Effect sizes reported are Cohen’s d and phi coefficient (φ) values.
p <.05.
As shown in Table 1, experience of multiple mild TBIs was the most common lifetime injury pattern. The vast majority of Veterans had experienced their TBI(s) many years ago, although some had experienced TBI in more recent years. Namely, 18 TBI participants had sustained TBI within the past 5 years, although 14 of these individuals had had multiple lifetime TBIs with at least one of their injuries occurring >5 years ago. No participant had experienced TBI <1 year ago.
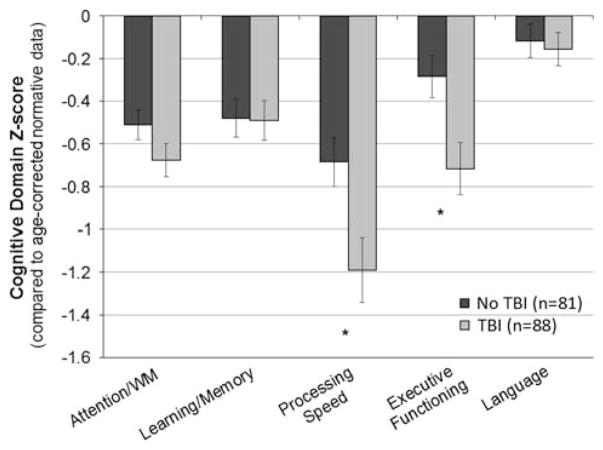
Figure 1 depicts the neuropsychological profile exhibited by older Veterans with and without lifetime TBI compared to age-corrected normative data. On average, older Veterans without TBI performed nearly .7 SD below the mean compared to normative data in the processing speed domain, and approximately .5 SD below the normative mean in the domains of attention/working memory and learning/memory, but performed more similarly to normative data in the executive functioning and language domains. On average, older Veterans with TBI performed nearly 1.2 SD below the normative mean in the processing speed domain, approximately .7 SD below the normative mean in the attention/working memory and executive functioning domains, and nearly .5 SD below the normative mean in the learning/memory domain, but performed more similarly to normative data in the language domain.
Fig. 1.
Neuropsychological profile among older veterans with and without TBI Graph shows mean cognitive domain composite scores with standard error bars by group. *p <.05 in unadjusted and adjusted models (see Table 2).
Results of linear mixed effects models examining the association between TBI and cognitive domain composite scores, with and without adjustment for covariates (demographics, presence of any medical history factor, any psychiatric or substance abuse condition, and current depressive and PTSD symptoms), are detailed in Table 2. There were no significant associations between TBI and performance on the attention/working memory, learning/memory, or language domain scores in any model. Individuals with TBI evidenced greater deficits in processing speed and executive functioning compared to those without TBI, associations which remained statistically significant in the fully adjusted model. Per standard guidelines for interpretation of Cohen’s f2 values (“small”: f2 ≥.02, “medium”: f2 ≥.15, “large”: f2 ≥.35) (Cohen, 1988), these associations (both unadjusted and adjusted for covariates) were in the range of “small” effect sizes.
Table 2.
Association between TBI and cognitive domain composite scores in older veterans
| Cognitive domain | Effect of TBI on cognitive domain composite score
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted model
|
Model adjusted for demographics and presence of any medical history factor
|
Fully adjusted model (+ any history of psychiatric or substance abuse conditions, current depressive and PTSD symptoms)
|
|||||||
| Parameter estimate [95% CI] | p | f2 | Parameter estimate [95% CI] | p | f2 | Parameter estimate [95% CI] | p | f2 | |
| Attention/working memory | −.17 [−.38, .04] | .12 | .01 | −.13 [−.34, .07] | .20 | .01 | −.10 [−.31, .12] | .37 | .00 |
| Learning/memory | −.01 [−.27, .24] | .93 | −.01 | .03 [−.23, .28] | .83 | −.01 | .04 [−.22, .31] | .74 | −.01 |
| Processing speed | −.50 [−.89, − .12] | .01* | .09 | −.54 [−.94, −.14] | .008* | .10 | −.52 [−.94, −.11] | .01* | .08 |
| Executive functioning | −.43 [−.75, −.12] | .007* | .08 | −.46 [−.79, −.14] | .006* | .09 | −.41 [−.75, −.07] | .02* | .06 |
| Language | −.04 [−.26, .18] | .72 | −.01 | −.07 [−.29, .16] | .55 | −.01 | −.02 [−.25, .21] | .86 | −.01 |
Effect sizes reported are Cohen’s f2values.
p <.05.
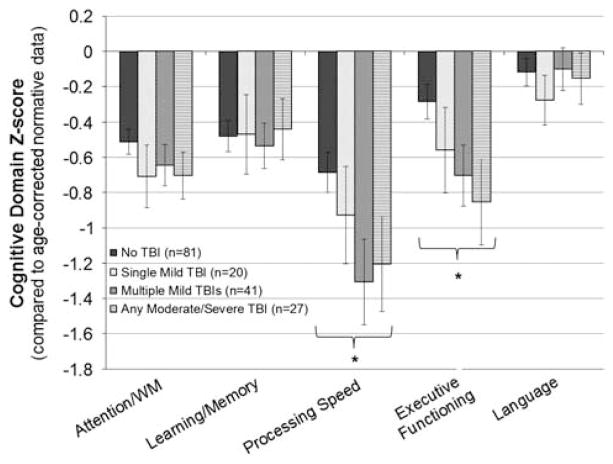
As shown in Figure 2, tests of trend for the four-level TBI variable (no TBI, single mild TBI, multiple mild TBIs, or any moderate-to-severe TBI) indicated that deficits in processing speed and executive functioning were most prominent among individuals with multiple mild TBIs or any moderate-to-severe TBI, while such deficits were not clearly present among those with single mild TBI. Specifically, in the fully adjusted model for processing speed, there was a significant linear trend effect across levels of the four-level TBI variable {parameter estimate for linear trend = −2.21, SE = .99, p = .03; parameter estimate [95% confidence interval (CI)]: no TBI = ref, single mild TBI = −.20 (−.83, .44), multiple mild TBI = −.70 (−1.22, −.18), any moderate-to-severe TBI = −.57 (−1.16, .02)}. Likewise, in the fully adjusted model for executive functioning, there was a significant linear trend effect across levels of the four-level TBI variable [parameter estimate for linear trend = −1.80, SE = .81, p = .03; parameter estimate (95% CI): no TBI = ref, single mild TBI = −.23 (−.75, .29), multiple mild TBI = −.44 (−.87, −.02), any moderate-to-severe TBI = −.53 [−1.02, −.04)]. There were no significant linear trend effects for the remaining cognitive domain composite scores (all p >.05).
Fig. 2.
Neuropsychological profile by TBI history category. Graph shows mean cognitive domain composite scores with standard error bars by group. *p-trend <.05 in unadjusted and adjusted models.
In sensitivity analyses, we re-ran the above models excluding the 18 individuals who had had a TBI within the past 5 years to explore whether findings differed among those whose injuries were exclusively remote TBI(s) rather than most recent injuries. Results remained similar to the above findings.
DISCUSSION
By evaluating the neuropsychological profiles of older Veterans with and without lifetime TBI, we found that both groups evidenced diminished cognitive performance compared to normative data from healthy older adults, but that the two groups had different neuropsychological profiles. On average, older Veterans with TBI (whose injuries were largely remote TBIs) had even greater deficits in processing speed than those without TBI. Older Veterans with TBI also showed evidence of executive dysfunction, whereas executive difficulties were not clearly present among those without TBI. The groups did not differ on measures of attention/working memory, learning and memory, and language.
When examining neuropsychological profiles of Veterans who differed in the number or severity of TBI(s) they had experienced, we found that deficits in speed and executive functioning were most prominent among individuals with more significant TBI injury histories (i.e., those with multiple mild TBIs, or any moderate-to-severe TBI), whereas history of single mild TBI was not clearly associated with greater deficits in these domains. Importantly, the neuropsychological profile differences we observed between groups did not appear to be explained by other factors present in individuals’ medical or psychiatric history, and results were unchanged when excluding the few individuals who sustained a TBI in more recent years. Overall, these results suggest that a lifetime history of multiple mild TBIs or any moderate-to-severe TBI, even when remote, is associated with a unique profile of cognitive deficits in older adulthood, characterized by slowed processing speed and executive dysfunction.
Despite epidemiological evidence that TBI is a risk factor for dementia (Plassman & Grafman, 2015), much remains to be understood regarding how a lifetime history of TBI might influence cognitive aging to ultimately lead to cognitive decline and increase risk for dementia. Our study results provide some clarity among several possibilities that have been raised in the literature. First, it has been suggested that the association between TBI and risk of dementia may simply be contributed to by normal aging processes, such that older adults with a lifetime history of TBI may have long-standing neural and cognitive vulnerabilities that further worsen in aging, eventually resulting in cognitive decline significant enough to meet the clinical threshold for a dementia diagnosis (Moretti et al., 2012).
Our results would be compatible with this hypothesis. Indeed, a common neural sequelae of TBI is diffuse axonal injury (Hayes, Bigler, & Verfaellie, 2016), which is known to be associated with deficits in processing speed and executive functioning (Spitz, Maller, O’Sullivan, & Ponsford, 2013) similar to the neuropsychological profile observed in the present study. It is possible that the processing speed and executive deficits we found among older Veterans with lifetime TBI, particularly among those with greater injury burden, may reflect long-standing deficits these individuals have had since their TBI(s) or deficits in these domains that have been further exacerbated by aging. The latter possibility is supported by a longitudinal study that found that older adults with TBI evidenced significant decline in processing speed over an 8-year follow-up period (executive functioning was not assessed) (Eramudugolla et al., 2014).
Alternatively, it is possible TBI may give rise to neuro-pathologic changes that initiate a neurodegenerative disease process (Johnson, Stewart, & Smith, 2010; Shively, Scher, Perl, & Diaz-Arrastia, 2012; Smith, Johnson, & Stewart, 2013), leading to a particular type of dementia. For example, some studies have identified TBI as a risk factor for Alzheimer’s dementia (AD), particularly among those with moderate or severe TBI (Plassman et al., 2000). Other research suggests repetitive mild TBI in particular may lead to a distinct neuropathology referred to as chronic traumatic encephalopathy (CTE) (Smith et al., 2013; Stern et al., 2013). Our results argue against a specific association between TBI and AD since we did not find prominent memory or language deficits in older Veterans with TBI, as is typical in prodromal AD and mild AD (Bondi et al., 2008; Verma & Howard, 2012). It is possible that our findings are capturing cognitive manifestations of another neurodegenerative process, such as CTE, although much remains to be investigated regarding the prevalence and cognitive profile of CTE. Moreover, it is unclear how likely it is for CTE neuropathology to be present among older Veterans whose TBI exposure may be qualitatively and quantitatively different from populations among whom CTE has been identified to date, namely football players and other athletes with extensive histories of repeated concussive and subconcussive head injuries (Bieniek et al., 2015; Gavett, Stern, & McKee, 2011).
That we found an association between the number/severity of TBIs and the extent to which individuals had cognitive deficits may also inform potential mechanism(s) linking lifetime TBI to cognitive impairment in aging. Namely, it is interesting that older Veterans who differed in the number and/or severity of TBI(s) they had experienced did not differ from each other in which cognitive domains they had deficits. Instead, they differed in the degree to which they had deficits within the same domains of processing speed and executive functioning. This pattern of findings suggests the same mechanism may underlie the association between lifetime TBI and cognition in aging among individuals with diverse TBI histories, but that the effects are more deleterious among those exposed to greater injury burden over their lifetime. Perhaps individuals with a history of multiple mild TBIs or any moderate-to-severe TBI have accumulated more extensive diffuse axonal injury or other neural damage than those with single mild TBI, increasing their vulnerability to cognitive impairment in aging. It is also possible that differences in TBI number and severity may influence whether or what type of neuropathologic cascade may develop to lead to cognitive decline and dementia in aging (Smith et al., 2013).
Strengths of the present study include our ability to investigate functioning in specific cognitive domains among older Veterans with diverse TBI histories, as well as our characterization of neuropsychological profiles among these individuals compared to normative data. Our study also benefits from assessment of participants’ medical comorbidities, psychiatric and substance abuse history, and current psychiatric symptoms, enabling our results to reveal that cognitive profile differences between Veterans with and without TBI remain above and beyond the influence of these other factors. While accounting for these factors as covariates strengthens our conclusions regarding the independent impact of TBI on neuropsychological performance, it is also possible that factors such as psychiatric symptoms may themselves be features of a TBI-related decline process, a possibility that is further discussed in Peltz et al. (2016).
A key limitation of our study is its cross-sectional design, such that we cannot determine whether the deficits we observed may be longstanding or incident in aging. We plan to investigate this in future work as we continue to follow these Veterans over time. We also cannot rule out the potential for reverse causality in this cross-sectional study, for example, perhaps individuals with lower pre-morbid cognitive functioning may be at greater risk for TBI in general, or at greater risk for sustaining repetitive or more severe TBIs. As accuracy of participants’ self-report of their TBI history could not be verified for many individuals, it is unclear how this may have influenced our results, or whether participants’ self-report may have tended to under- versus over-estimate the number or severity of TBI(s) they had experienced.
In defining our TBI group, we required individuals to self-report ≥1 head injury that required medical care, which may have influenced our TBI group to have more significant injury histories than the general population of older Veterans, particularly as a substantial proportion of individuals with TBI do not seek medical attention (Setnik & Bazarian, 2007). Additionally, normative corrections for our neuropsychological test battery necessitated comparisons to different sources of normative data (no one source was available that encompassed all of the tests), which may have introduced an unclear pattern of bias to our results. As this study focused on older, primarily male and caucasian Veterans, a unique population among whom medical and psychiatric comorbidities are common (Kramarow & Pastor, 2012), we cannot be certain how well our results may generalize to non-Veteran populations or to Veterans living in different settings who may differ from our participants in important ways.
Moreover, we cannot be certain of how findings from this research study may diverge from what is seen among patients presenting for neuropsychological evaluations as part of their clinical care, particularly in clinical situations where secondary gain factors may be present. As the associations we observed between TBI and cognitive functioning were in the range suggestive of “small” effect sizes, the extent to which such associations have clear clinical impacts remains unclear, including whether and how these TBI-associated cognitive deficits impact individuals’ daily functioning.
In summary, our findings suggest that the neuropsychological profile of older Veterans with lifetime TBI, even when remote, is characterized by slowed processing speed and executive dysfunction. This pattern of deficits was most prominent among individuals with a history of multiple mild TBIs or any moderate-to-severe TBI, but were not clearly present among those with single mild TBI. Older Veterans with lifetime TBI are appear to be a cognitively vulnerable population, for whom clinical care should include close monitoring and routine assessment to evaluate whether patients need additional resources and care. Future research is needed to understand whether it might be possible to intervene to improve cognitive functioning among older adults with TBI, and whether such interventions might also help to prevent, or at least delay, the development of dementia in this high-risk population. Our results suggest that intervention and prevention research efforts should focus on older Veterans who have had multiple mild TBI or any moderate-to-severe TBI in particular, and that research investigating potential cognitive interventions should emphasize processing speed and executive functioning skills as intervention targets.
Acknowledgments
The authors thank our research participants, the Armed Forces Retirement Home in Washington, DC, the Veterans Home of California in Yountville, CA, and our dedicated study staff including Kim Kelley, Ross Passo, Leah Harburg, Daniel Freimer, and Margaret Gross. This research was supported by Department of Defense grants W81XWH-12-1-0581 and W81XWH-14-2-0132 (awarded to K.Y.); and in part by NIA grant K24AG031155 (awarded to K.Y.). This research was also supported by Career Development Award 1IK2RX001629 (awarded to A.R.K.) from the U.S. Department of Veterans Affairs, Rehabilitation Research and Development Service. The contents of this manuscript do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Footnotes
Disclosures: Dr. Kaup has been given access to cognitive assessment/cognitive training software and tablet devices by Akili Interactive Labs for usage in a related research study. Dr. Yaffe is a consultant for Novartis and Pfizer, serves on DSMBs for Takeda, Inc and an NIA sponsored study, and serves on the Beeson Scientific Advisory Board and the Alzheimer’s Association Medical & Scientific Advisory Council. The remaining authors have no disclosures to report.
References
- Ashman TA, Cantor JB, Gordon WA, Sacks A, Spielman L, Egan M, Hibbard MR. A comparison of cognitive functioning in older adults with and without traumatic brain injury. Journal of Head Trauma Rehabilitation. 2008;23(3):139–148. doi: 10.1097/01.HTR.0000319930.69343.64. [DOI] [PubMed] [Google Scholar]
- Barnes DE, Kaup AR, Kirby K, Byers AL, Diaz-Arrastia R, Yaffe K. Traumatic brain injury and risk for dementia in older veterans. Neurology. 2014;83:312–319. doi: 10.1212/WNL.0000000000000616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieniek KF, Ross OA, Cormier KA, Walton RL, Soto-Ortolaza A, Johnston AE, … Wszolek ZK. Chronic traumatic encephalopathy pathology in a neurodegenerative disorders brain bank. Acta Neuropathologica. 2015;130(6):877–889. doi: 10.1007/s00401-015-1502-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour Research and Therapy. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Bogner J, Corrigan JD. Reliability and predictive validity of the Ohio State University TBI identification method with prisoners. Journal of Head Trauma Rehabilitation. 2009;24(4):279–291. doi: 10.1097/HTR.0b013e3181a66356. [DOI] [PubMed] [Google Scholar]
- Bondi MW, Jak AJ, Delano-Wood L, Jacobson MW, Delis DC, Salmon DP. Neuropsychological contributions to the early identification of Alzheimer’s disease. Neuropsychology Review. 2008;18(1):73–90. doi: 10.1007/s11065-008-9054-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byers AL, Yaffe K. Depression and risk of developing dementia. Nature Reviews. Neurology. 2011;7(6):323–331. doi: 10.1038/nrneurol.2011.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan RC. Sustained attention in patients with mild traumatic brain injury. Clinical Rehabilitation. 2005;19(2):188–193. doi: 10.1191/0269215505cr838oa. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1988. [Google Scholar]
- Corrigan JD, Bogner J. Initial reliability and validity of the Ohio State University TBI identification method. Journal of Head Trauma Rehabilitation. 2007;22(6):318–329. doi: 10.1097/01.HTR.0000300227.67748.77. [DOI] [PubMed] [Google Scholar]
- Curtiss G, Vanderploeg RD, Spencer J, Salazar AM. Patterns of verbal learning and memory in traumatic brain injury. Journal of the International Neuropsychological Society. 2001;7(5):574–585. doi: 10.1017/s1355617701755051. [DOI] [PubMed] [Google Scholar]
- Dams-O’Connor K, Spielman L, Hammond F, Sayed N, Culver C, Diaz-Arrastia R. An exploration of clinical dementia phenotypes among individuals with and without traumatic brain injury. NeuroRehabilitation. 2013;32(2):199. doi: 10.3233/NRE-130838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Veterans Affairs, & Department of Defense. Clinical practice guidelines: Management of concussion/Mild traumatic brain injury. 2009 Retrieved from http://www.healthquality.va.gov/management_of_concussion_mtbi.asp.
- Eramudugolla R, Bielak AA, Bunce D, Easteal S, Cherbuin N, Anstey KJ. Long-term cognitive correlates of traumatic brain injury across adulthood and interactions with APOE genotype, sex, and age cohorts. Journal of the International Neuropsychological Society. 2014;20(04):444–454. doi: 10.1017/S1355617714000174. [DOI] [PubMed] [Google Scholar]
- Finnanger TG, Skandsen T, Andersson S, Lydersen S, Vik A, Indredavik M. Differentiated patterns of cognitive impairment 12 months after severe and moderate traumatic brain injury. Brain Injury. 2013;27(13–14):1606–1616. doi: 10.3109/02699052.2013.831127. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Minimental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gardner RC, Burke JF, Nettiksimmons J, Kaup A, Barnes DE, Yaffe K. Dementia risk after traumatic brain injury vs nonbrain trauma: The role of age and severity. JAMA Neurology. 2014;71(12):1490–1497. doi: 10.1001/jamaneurol.2014.2668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavett BE, Stern RA, McKee AC. Chronic traumatic encephalopathy: A potential late effect of sport-related concussive and subconcussive head trauma. Clinics in Sports Medicine. 2011;30(1):179–188. doi: 10.1016/j.csm.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guskiewicz KM, Marshall SW, Bailes J, McCrea M, Cantu RC, Randolph C, Jordan BD. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery. 2005;57(4):719–726. doi: 10.1093/neurosurgery/57.4.719. [DOI] [PubMed] [Google Scholar]
- Hayes JP, Bigler ED, Verfaellie M. Traumatic brain injury as a disorder of brain connectivity. Journal of the International Neuropsychological Society. 2016;22(02):120–137. doi: 10.1017/S1355617715000740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himanen L, Portin R, Isoniemi H, Helenius H, Kurki T, Tenovuo O. Longitudinal cognitive changes in traumatic brain injury: A 30-year follow-up study. Neurology. 2006;66(2):187–192. doi: 10.1212/01.wnl.0000194264.60150.d3. [DOI] [PubMed] [Google Scholar]
- Ivnik RJ, Malec J, Smith GE, Tangalos EG, Petersen RC, Kokmen E, Kurland LT. Mayo’s older americans normative studies: Updated AVLT norms for ages 56 to 97. Clinical Neuropsychologist. 1992;6:83–104. [Google Scholar]
- Ivnik RJ, Malec JF, Tangalos EG, Petersen RC, Kokmen E, Kurland LT. The Auditory-Verbal Learning Test (AVLT): Norms for ages 55 years and older. Psychological Assessment. 1990;2(3):304. [Google Scholar]
- Johnson VE, Stewart W, Smith DH. Traumatic brain injury and amyloid-β pathology: A link to Alzheimer’s disease? Nature Reviews. Neuroscience. 2010;11(5):361–370. doi: 10.1038/nrn2808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan E, Goodglass H, Weintraub S. The Boston Naming Test. Philadelphia: Lea & Febiger; 1983. [Google Scholar]
- Karr JE, Areshenkoff CN, Garcia-Barrera MA. The neuropsychological outcomes of concussion: A systematic review of meta-analyses on the cognitive sequelae of mild traumatic brain injury. Neuropsychology. 2014;28(3):321. doi: 10.1037/neu0000037. [DOI] [PubMed] [Google Scholar]
- Kramarow EA, Pastor PN. The health of male veterans and nonveterans aged 25–64: United States, 2007–2010 National Center for Health Statistics (NCHS) Data Brief, no 101. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- Kramer JH, Mungas D, Possin KL, Rankin KP, Boxer AL, Rosen HJ, … Widmeyer M. NIH-EXAMINER battery test performances among healthy controls by age group. 2014a. Unpublished raw data. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer JH, Mungas D, Possin KL, Rankin KP, Boxer AL, Rosen HJ, … Widmeyer M. NIH EXAMINER: Conceptualization and development of an executive function battery. Journal of the International Neuropsychological Society. 2014b;20(01):11–19. doi: 10.1017/S1355617713001094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathias JL, Beall JA, Bigler ED. Neuropsychological and information processing deficits following mild traumatic brain injury. Journal of the International Neuropsychological Society. 2004;10(2):286–297. doi: 10.1017/S1355617704102117. [DOI] [PubMed] [Google Scholar]
- McAllister TW, Flashman LA, McDonald BC, Saykin AJ. Mechanisms of working memory dysfunction after mild and moderate TBI: Evidence from functional MRI and neurogenetics. Journal of Neurotrauma. 2006;23(10):1450–1467. doi: 10.1089/neu.2006.23.1450. [DOI] [PubMed] [Google Scholar]
- McDonald BC, Flashman LA, Saykin AJ. Executive dysfunction following traumatic brain injury: Neural substrates and treatment strategies. NeuroRehabilitation. 2002;17(4):333–344. [PubMed] [Google Scholar]
- Moretti L, Cristofori I, Weaver SM, Chau A, Portelli JN, Grafman J. Cognitive decline in older adults with a history of traumatic brain injury. The Lancet Neurology. 2012;11(12):1103–1112. doi: 10.1016/S1474-4422(12)70226-0. [DOI] [PubMed] [Google Scholar]
- Morris J, Heyman A, Mohs R, Hughes J, van B, Fillenbaum G, … Clark C. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part I: Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology. 1989;39:1159–1165. doi: 10.1212/wnl.39.9.1159. [DOI] [PubMed] [Google Scholar]
- National Institute of Neurological Disorders and Stroke (NINDS) NINDS Common Data Elements: Traumatic Brain Injury. 2012 Retrieved from https://commondataelements.ninds.nih.gov/TBI.aspx#tab=Data_Standards.
- Okie S. Traumatic brain injury in the war zone. New England Journal of Medicine. 2005;352(20):2043–2047. doi: 10.1056/NEJMp058102. [DOI] [PubMed] [Google Scholar]
- Ommaya AK, Ommaya AK, Dannenberg AL, Salazar AM. Causation, incidence, and costs of traumatic brain injury in the US military medical system. The Journal of Trauma and Acute Care Surgery. 1996;40(2):211–217. doi: 10.1097/00005373-199602000-00007. [DOI] [PubMed] [Google Scholar]
- Peltz CB, Gardner RC, Kenney K, Diaz-Arrastia R, Kramer JH, Yaffe K. Neurobehavioral characteristics of older veterans with remote traumatic brain injury. Journal of Head Trauma Rehabilitation. 2016 doi: 10.1097/HTR.0000000000000245. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry DC, Sturm VE, Peterson MJ, Pieper CF, Bullock T, Boeve BF, … Kramer JH. Association of traumatic brain injury with subsequent neurological and psychiatric disease: A meta-analysis. Journal of Neurosurgery. 2015;124:511–526. doi: 10.3171/2015.2.JNS14503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plassman BL, Grafman J. Traumatic brain injury and late-life dementia. Handbook of Clinical Neurology. 2015;128:711–722. doi: 10.1016/B978-0-444-63521-1.00044-3. [DOI] [PubMed] [Google Scholar]
- Plassman BL, Havlik R, Steffens D, Helms M, Newman T, Drosdick D, … Burke J. Documented head injury in early adulthood and risk of Alzheimer’s disease and other dementias. Neurology. 2000;55(8):1158–1166. doi: 10.1212/wnl.55.8.1158. [DOI] [PubMed] [Google Scholar]
- Qiu C, Fratiglioni L. A major role for cardiovascular burden in age-related cognitive decline. Nature Reviews. Cardiology. 2015;12(5):267–277. doi: 10.1038/nrcardio.2014.223. [DOI] [PubMed] [Google Scholar]
- Raymont V, Salazar AM, Krueger F, Grafman J. “Studying injured minds”–the Vietnam head injury study and 40 years of brain injury research. Frontiers in Neurology. 2011;2:15. doi: 10.3389/fneur.2011.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitan RM, Wolfson D. The Halstead-Reitan Neuropsychological Test Battery: Theory and Clinical Interpretation. Vol. 4. Mesa, AZ: Reitan Neuropsychology; 1985. [Google Scholar]
- Rey A. L’examen psychologique dans les cas d’encéphalopathie traumatique.(Les problems.) Archives de psychologie 1941 [Google Scholar]
- Rochat L, Ammann J, Mayer E, Annoni JM, Linden M. Executive disorders and perceived socio-emotional changes after traumatic brain injury. Journal of Neuropsychology. 2009;3(2):213–227. doi: 10.1348/174866408X397656. [DOI] [PubMed] [Google Scholar]
- Sayer NA. Traumatic brain injury and its neuropsychiatric sequelae in war veterans. Annual Review of Medicine. 2012;63:405–419. doi: 10.1146/annurev-med-061610-154046. [DOI] [PubMed] [Google Scholar]
- Scholten AC, Haagsma JA, Cnossen MC, Olff M, Van Beeck EF, Polinder S. Prevalence and risk factors of anxiety and depressive disorders following traumatic brain injury: A systematic review. Journal of Neurotrauma. 2016 doi: 10.1089/neu.2015.4252. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Schretlen DJ, Shapiro AM. A quantitative review of the effects of traumatic brain injury on cognitive functioning. International Review of Psychiatry. 2003;15(4):341–349. doi: 10.1080/09540260310001606728. [DOI] [PubMed] [Google Scholar]
- Selya AS, Rose JS, Dierker LC, Hedeker D, Mermelstein RJ. A practical guide to calculating Cohen’s f2, a measure of local effect size, from PROC MIXED. Frontiers in Psychology. 2012;3:111. doi: 10.3389/fpsyg.2012.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setnik L, Bazarian JJ. The characteristics of patients who do not seek medical treatment for traumatic brain injury. Brain Injury. 2007;21(1):1–9. doi: 10.1080/02699050601111419. [DOI] [PubMed] [Google Scholar]
- Shirk SD, Mitchell MB, Shaughnessy LW, Sherman JC, Locascio JJ, Weintraub S, Atri A. A web-based normative calculator for the uniform data set (UDS) neuropsychological test battery. Alzheimer’s Research and Therapy. 2011;3(6):32–32. doi: 10.1186/alzrt94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shively S, Scher AI, Perl DP, Diaz-Arrastia R. Dementia resulting from traumatic brain injury: What is the pathology? Archives of Neurology. 2012;69(10):1245–1251. doi: 10.1001/archneurol.2011.3747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DH, Johnson VE, Stewart W. Chronic neuropathologies of single and repetitive TBI: Substrates of dementia? Nature Reviews. Neurology. 2013;9:211–221. doi: 10.1038/nrneurol.2013.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitz G, Maller JJ, O’Sullivan R, Ponsford JL. White matter integrity following traumatic brain injury: The association with severity of injury and cognitive functioning. Brain Topography. 2013;26(4):648–660. doi: 10.1007/s10548-013-0283-0. [DOI] [PubMed] [Google Scholar]
- Stern RA, Daneshvar DH, Baugh CM, Seichepine DR, Montenigro PH, Riley DO, … McHale L. Clinical presentation of chronic traumatic encephalopathy. Neurology. 2013;81(13):1122–1129. doi: 10.1212/WNL.0b013e3182a55f7f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor EM. Psychological appraisal of children with cerebral defects. 1959. [Google Scholar]
- U.S. Department of Veterans Affairs, & National Center for PTSD. Using the PTSD Checklist for DSM-IV(PCL) 2014 Retrieved from http://www.ptsd.va.gov/professional/pages/assessments/assessment-pdf/PCL-handout.pdf.
- Verma M, Howard R. Semantic memory and language dysfunction in early Alzheimer’s disease: A review. International Journal of Geriatric Psychiatry. 2012;27(12):1209–1217. doi: 10.1002/gps.3766. [DOI] [PubMed] [Google Scholar]
- Wechsler D. WAIS-R manual: Wechsler adult intelligence scale-revised. San Antonio, TX: Psychological Corporation; 1981. [Google Scholar]
- Wechsler D. WMS-R: Wechsler memory scale-revised. San Antonio, TX: Psychological Corporation; 1987. [Google Scholar]
- Weintraub S, Salmon D, Mercaldo N, Ferris S, Graff-Radford NR, Chui H, … Galasko D. The Alzheimer’s disease centers’ uniform data set (UDS): The neuropsychological test battery. Alzheimer Disease and Associated Disorders. 2009;23(2):91. doi: 10.1097/WAD.0b013e318191c7dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaffe K, Vittinghoff E, Lindquist K, Barnes D, Covinsky KE, Neylan T, … Marmar C. Posttraumatic stress disorder and risk of dementia among US veterans. Archives of General Psychiatry. 2010;67(6):608–613. doi: 10.1001/archgenpsychiatry.2010.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yesavage JA, Brink T, Rose TL, Lum O, Huang V, Adey M, Leirer VO. Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research. 1983;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]