Abstract
Objectives
To examine changes in sleep problems over a 1.5 year period among Black/African American (AA) and White/European American (EA) college students, and consider the role of racial discrimination as a mediator of race differences in sleep problems over time.
Methods
Students attending a large, predominantly White university (N = 133, 41% AA, 57% female, Mean age= 18.8, SD=.90) reported on habitual sleep characteristics and experiences of racial discrimination at baseline and follow-up assessments. A latent variable for sleep problems was assessed from reports of sleep latency, duration, efficiency, and quality. Longitudinal models were used to examine race differences in sleep problems over time and the mediating role of perceived discrimination. Covariates included age, gender, parent education, parent income, body mass index, self-rated physical health, and depressive symptoms. Each of the individual sleep measures was also examined separately, and sensitivity analyses were conducted using alternative formulations of the sleep problems measure.
Results
AAs had greater increases in sleep problems than EAs. Perceived discrimination was also associated with increases in sleep problems over time, and mediated racial disparities in sleep. This pattern of findings was similar when each of the sleep indicators was considered separately, and held with alternative sleep problems measures.
Conclusions
Findings highlight the importance of racial disparities in sleep across the college years and suggest that experiences of discrimination contribute to group disparities.
Keywords: African American, Sleep Quality, Health Disparities, Perceived Discrimination, Stress
Sleep is a fundamental biological process, which plays a critical role in the maintenance of mental and physical health. In adult and college student samples, measures of sleep problems have been linked to declines in psychosocial functioning (Tavernier & Willoughby, 2014), poor health behaviors (Shochat, Cohen-Zion, & Tzischinsky, 2014), and diminished self-regulatory abilities (Yoo, Gujar, Hu, Jolesz, & Walker, 2007). Insufficient or low quality sleep has also been consistently associated with subsequent obesity (El-Sheikh, Bagley, Keiley, & Erath, 2014), metabolic disease (Knutson, 2010), and other morbidity sequelae (Cappuccio, Cooper, D’Elia, Strazzullo, & Miller, 2011). Sleep problems are a significant impediment across multiple dimensions of health and well-being, which collectively carry an economic burden of hundreds of billions of dollars each year in the United States alone (Institute of Medicine (US) Committee on Sleep Medicine and Research, 2006).
Recent meta-analyses reveal that individuals who are categorized as Black/African American (AA) show consistently poorer sleep than those who are categorized as White/European American (EA) (Petrov & Lichstein, 2015; Ruiter, DeCoster, Jacobs, & Lichstein, 2011). In particular, studies indicate shorter sleep duration, poorer sleep efficiency, greater onset latency, and worse overall sleep quality among AAs relative to EAs (Petrov & Lichstein, 2015; Ruiter, DeCoster, Jacobs, & Lichstein, 2010; Ruiter et al., 2011). Reviews of the literature reveal that longitudinal analyses of racial disparities in sleep are sorely needed, and mechanisms for group differences are not well understood (Petrov & Lichstein, 2015). Furthermore, several studies indicate that race differences in sleep measures endure after measures of socioeconomic status are controlled (Grandner et al., 2013; Whinnery, Jackson, Rattanaumpawan, & Grandner, 2014).
Studies of racial disparities in sleep among college students are scarce. However, such studies may be of particular importance because of the known stressors experienced by minority students attending predominantly White Universities, such as overt and covert racism and lack of support in classrooms and residence halls (Ancis, Sedlacek, & Mohr, 2000; Nora & Cabrera, 1996). Additionally, because sleep is robustly associated with academic performance and the ability to manage stress (Killgore et al., 2008; Taylor, Vatthauer, Bramoweth, Ruggero, & Roane, 2013; Yoo, Hu, Gujar, Jolesz, & Walker, 2007), identifying psychosocial predictors of race differences in sleep among college students is a needed area of research with important implications for the reduction of racial disparities.
Associations between social stress and sleep are well-established (De Lange et al., 2009; Kim & Dimsdale, 2007), and have been documented among adolescent and college student samples (Lund, Reider, Whiting, & Prichard, 2010), as well as at other points in the life span (El-Sheikh et al., 2013). As a social stressor disproportionately experienced by AAs, racial discrimination is a likely candidate mechanism for racial disparities in sleep. Several studies have considered the link between discrimination and sleep (Slopen, Lewis, & Williams, 2015) and have found that perceived discrimination or unfair treatment is associated with sleep disturbance among both AA and EA adults (Beatty et al., 2011; Grandner et al., 2012; Lewis et al., 2013; Tomfohr, Pung, Edwards, & Dimsdale, 2012). Associations between discrimination and sleep have also been found in other ethnic groups (Huynh & Gillen-O’Neel, 2013; Steffen & Bowden, 2006). However, none of these studies have considered the effects of discrimination on sleep longitudinally, and there is a lack of research examining the link between discrimination and sleep among college students.
The current study brings together the above lines of research in the context of advanced education. Specifically, we examined changes in sleep problems among AA and EA students attending a large, predominantly White university, and considered perceived racial discrimination as a mediator of expected group differences in sleep problems over time. Clarification of mechanisms of effects is key for understanding why individuals of different races may be more or less susceptible to sleep disturbance. To our knowledge, this is the first study to consider racial disparities in the longitudinal sleep patterns of college students, and the first to examine perceived discrimination as a mediator of racial/ethnic differences in sleep over time.
Experiences of discrimination vary in severity and can range from covert and subtle to overt and blatant (Sue, 2010; Williams & Mohammed, 2013). The majority of studies have used one of two types of approaches to assess perceived discrimination (Krieger, 2014). The first approach focuses on reports of general unfair treatment, which are not tied to any one domain or category (Krieger, Smith, Naishadham, Hartman, & Barbeau, 2005; Williams, Yu, Jackson, & Anderson, 1997). The second approach involves specifying the domain or type of discrimination (e.g., racial/ethnic) in the stem of the question (Fisher, Wallace, & Fenton, 2000; Ong, Fuller-Rowell, & Burrow, 2009). Both approaches have been commonly used, and have demonstrated predictive validity in AA and EA samples (Fuller-Rowell, Evans, & Ong, 2012; Kessler, Mickelson, & Williams, 1999; Sellers, Caldwell, Schmeelk-Cone, & Zimmerman, 2003; Williams et al., 2012). The latter approach allows for the possibility of a specific interpretation with respect to the domain of discrimination and was adopted for the current investigation with racial discrimination defined as unfair treatment due to one’s race/ethnicity.
Sleep is a complex and multi-faceted construct and assessment of various sleep parameters is imperative (Sadeh, 2015). In this study, sleep problems are indicated by reported sleep duration, efficiency (percent of time in bed spent sleeping), latency (number of minutes between going to bed and falling asleep), and overall quality, and such sleep assessments do not refer to clinically significant problems (e.g., apnea, restless leg syndrome). Towards explication of effects, the various sleep parameters were examined both individually and as a latent construct. The overarching hypotheses were (1) that AA students would show greater increases in sleep problems than EAs over time, and (2) that perceived racial discrimination would mediate this race difference.
Methods
Participants and Design
The analytic sample for the current study included 133 college students (mean age at baseline = 18.8, SD = 0.9; 41% AA, 57% female) who participated in baseline and follow-up assessments of a longitudinal study. The study was conducted at a large, Midwestern university in the United States with a predominantly White/European American student body (3% African American, 4% Asian, 4% Hispanic/Latino, 1% American Indian). Approval was obtained from the relevant institutional review board for all aspects of this research. All first and second year AA students and an equally sized stratified random sample of first and second year EA students were initially invited to participate by mailing information about the study. EA students without a parent who had graduated from college (first generation) were over-sampled to ensure that race and parent education were not confounded. Recruitment was stopped when the target sample size of 150 students had enrolled in the study.1 The initial assessment (T1) took place in the clinical research unit of an on-campus university hospital in 2012. During the study visit, physiologic measures were taken by researchers and nursing staff, and self-report measures were administered on a laptop computer. Respondents received $75 for participation. Out of the 150 students in the baseline sample, 133 (89%) also participated in a brief follow-up survey assessment (T2) administered 1.5 years later, for which participants received $15. The final analytic sample included those who participated in both waves of data collection. Individuals lost to attrition were more likely to be AA (p<.001). However, controlling for race, attrition was not associated with any other demographic or substantive variables. Furthermore, compared to AAs who remained in the study, AAs lost to attrition showed no differences on any demographic or substantive variables. Thus, differences in attrition on the basis of race, although a limitation, are not expected to introduce significant bias to the reported results.
Measures
Sleep problems
Sleep characteristics were measured using the Pittsburgh Sleep Quality Index (PSQI), a reliable self-administered questionnaire that is widely used to assess the following seven sleep domains: duration, efficiency, onset latency, quality, sleep disturbances, daytime dysfunction, and use of sleeping medication (Buysse, Reynolds III, Monk, Berman, & Kupfer, 1989). The PSQI has demonstrated validity across various populations, including college students, and has been associated with emotional and physical health as well as academic outcomes (Lund et al., 2010; Orzech, Salafsky, & Hamilton, 2011). The full PSQI questionnaire was administered at T2 and items from the PSQI relating to sleep duration, efficiency, latency, and quality were also assessed at the T1 baseline assessment. Because our main interest was in considering prospective associations with sleep, primary analyses focused on measures of sleep problems that were parallel across time and additional sensitively analyses were conducted to consider the full PSQI global score at T2. Duration was assessed as the number of hours of actual sleep each night, and was coded on a four point scale with higher scores indicating more duration problems: 7 to 9 hours (coded as 0), 6 to 6.99 hours (coded as 1), 5 to 5.99 hours (coded as 2), and less than 5 hours (coded as 3). Because long sleep duration (>9 hours) has established associations with ill health (Patel, Malhotra, Gottlieb, White, & Hu, 2006), three individuals with durations greater than 9 hours were given a score of 1. This method for coding sleep duration is based on the current recommendation of 7 to 9 hours for young adults (Hirshkowitz et al., 2015), with an equal scoring penalty applied for each hour outside of the recommended range in either direction.2 Efficiency is the percent of time in bed spent sleeping and was calculated from reports of number of hours in bed and number of hours spent sleeping. Latency was measured as the number of minutes taken to fall asleep each night. Quality was assessed with ratings of overall sleep quality on a four point scale: very bad (coded as 0), bad (coded as 1), good (coded as 2), and very good (coded as 3). These four sleep indicators were assessed at T1 and T2 and were included as observed indicators of latent constructs for sleep problems at each wave.3 The measurement model demonstrated good fit (χ2/df = 1.32; CFI = .95; RMSEA = .049, 90% CI: [.000, .092]), and all indicators significantly loaded onto the hypothesized constructs (ps < .001), with standardized factor loadings between .53 and .69 in magnitude. Each of the four sleep indicators was also considered separately in additional analyses.
Perceived discrimination
Perceived discrimination was assessed using 13 items drawn from the Racism and Life Experiences Scales (RaLES) (Harrell, 1994, 2000). Respondents indicated how often they had experienced each type of unfair treatment because of their race/ethnicity (e.g., “How often have you been treated as if you were stupid or talked down to?” and “How often have you been left out of conversations or activities?”). Response options were on a 6-point scale ranging from never (coded as 1) to several times a day (coded as 6). The RaLES has been used extensively in research on perceived discrimination, and psychometric properties have been documented (Sellers & Shelton, 2003; Utsey, 1998). In this study, all items loaded onto a single factor and the scale demonstrated good internal consistency (α = .91). Items were therefore averaged to create a composite score with higher values indicating higher levels of racial discrimination.
Demographic and control variables
All demographic variables were assessed at T1. Race/ethnicity was taken from university records and confirmed by student self-reports. Sex, age, parent education, and parent income were also assessed from student self-reports. Parent education—assessed for each parent on a seven point scale ranging from 8th grade or less (coded as 1) to graduate degree (coded as 7)—was scored as the mean education level for students from two parent families, and as a single item for students from single parent families. Parents’ combined household income was assessed on a scale from “less than $5,000” to “more than $200,000” with 28 possible response categories.
Measures of physical health (body mass index, self-rated health), and mental health (depressive symptoms) were also assessed at T1, and were considered in analyses as covariates. Body mass index (kg/m2) was calculated from measures of height and weight taken by trained nursing staff. Self-ratings of “overall physical health” were assessed on a five-point scale ranging from poor to excellent. This single-item measure of health has been shown to be a robust predictors of subsequent morbidity and mortality and is widely used in current research (DeSalvo, Bloser, Reynolds, He, & Muntner, 2006; Schnittker & Bacak, 2014). Depression was assessed with the Beck Depression Inventory-II (A. T. Beck, Steer, & Brown, 1996). Two items relating to sleep problems, from the original 21-item scale, were excluded to avoid conceptual overlap between the depression and sleep measures. The revised scale had good internal consistency (α = .79).
Analysis Strategy
Structural equation models were estimated to test the specified hypotheses, and Full Information Maximum Likelihood was used to deal with missing data on observed variables. Of the 133 individuals included in analyses, 97% had complete sleep-related data, and 95% had complete data on parents’ household income. All other variables had no missing data. Maximum likelihood estimation with robust standard errors was used and model fit was evaluated using the chi-square to degrees of freedom ratio, Bentler’s confirmatory fit index (CFI), and root mean squared error of approximation (RMSEA), and the 90% confidence interval (CI) of the RMSEA. Values of approximately 2 or less for χ2/df, .95 or greater for the CFI, .06 or less for the RMSEA, and .10 or less for the upper bound of the RMSEA CI, are indicative of good model fit (Hu & Bentler, 1999). Mediation was tested using the product of coefficients method with a bootstrapping procedure that estimates bias-corrected confidence intervals (Hayes & Scharkow, 2013; MacKinnon, Fairchild, & Fritz, 2007). Standardized parameter estimates are shown in Figure 1 and unstandardized coefficients are reported in the text unless otherwise specified.
Figure 1.
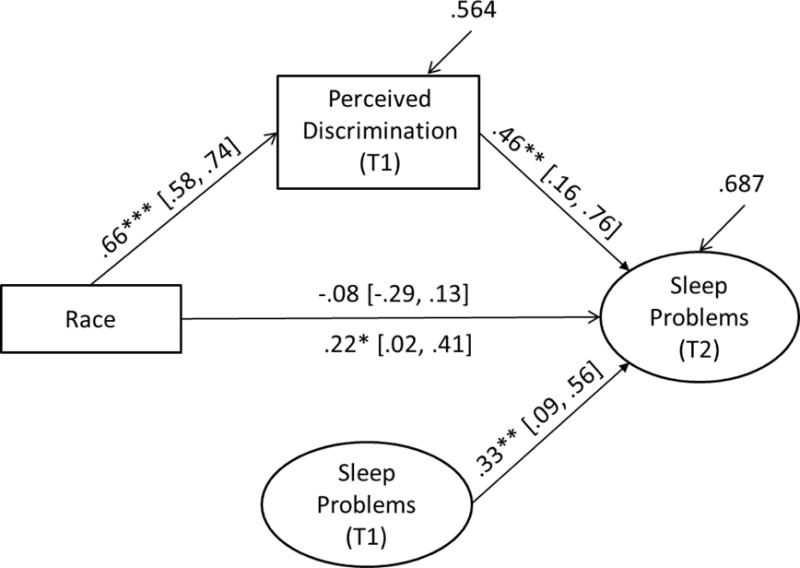
Model results showing longitudinal race differences in sleep problems, as mediated by perceived discrimination. Standardized coefficients are shown with 95% CI in brackets. Direct effects of race before mediation are shown on underside of path. Race is coded as White=0 and Black=1. *p < .05. **p < .01. ***p < .001.
Results
Preliminary Analyses
Table 1 shows descriptive statistics for AAs and EAs for all key variables. No significant differences in parent education were present between AAs and EAs. Parents’ income was, however, greater among EAs than AAs (Mdifference = 5.48, 95% CI [2.86, 8.11], p < .001), equivalent to approximately $27,000 more per year. Levels of racial discrimination (Mdifference = 0.80, 95% CI [.60, 1.00], p < .001) were higher among AAs than EAs.
Table 1.
Descriptive Statistics for African American (N = 54) and European American (N = 79) college Students
| African American
|
European American
|
Race Differencea
|
||||
|---|---|---|---|---|---|---|
| Mean (%) | SD | Mean (%) | SD | Cohen’s d | p | |
| Male (%) | (38.9) | (45.6) | .45 | |||
| Age (years) (T1) | 18.8 | 0.89 | 18.9 | 0.91 | .11 | .43 |
| Parents’ education (T1) | 4.76 | 1.33 | 4.93 | 1.20 | .13 | .44 |
| Parents’ income (T1) | 14.39 | 7.78 | 19.87 | 6.93 | .74 | <.001 |
| Perceived discrimination (T1) | 2.01 | 0.70 | 1.21 | 0.23 | 1.54 | <.001 |
| Depressive symptoms (T1) | 6.56 | 4.46 | 4.25 | 3.74 | .56 | .002 |
| Self-rated health (T1) | 3.57 | 0.86 | 3.78 | 0.78 | .26 | .144 |
| Body mass index (T1) | 25.03 | 4.88 | 23.40 | 2.80 | .41 | .030 |
| Sleep Quality (T1) | 1.96 | 0.58 | 2.06 | 0.51 | .18 | .30 |
| Sleep Duration Problems (T1) | 0.59 | 0.76 | 0.24 | 0.51 | .54 | .004 |
| Sleep Latency (T1) | 23.80 | 16.67 | 19.74 | 14.06 | .26 | .15 |
| Sleep Efficiency (T1) | 0.89 | 0.08 | 0.89 | 0.09 | .08 | .65 |
| Sleep Quality (T2) | 1.79 | 0.63 | 2.05 | 0.64 | .41 | .024 |
| Sleep Duration Problems (T2) | 0.81 | 0.92 | 0.39 | 0.63 | .53 | .005 |
| Sleep Latency (T2) | 29.79 | 23.45 | 21.45 | 18.59 | .39 | .025 |
| Sleep Efficiency (T2) | 0.87 | 0.11 | 0.90 | 0.10 | .29 | .12 |
For continuous variables, Cohen’s d statistic is reported to indicate the magnitude of the race difference. Independent samples t-tests and chi-squared tests were used to determine the statistical significance of group differences.
At T1, AAs had more sleep problems than EAs relating to duration (p = .004). Findings were in the same direction but were not significant for perceived overall sleep quality (p = .30) and latency (p = .13). Levels of sleep efficiency showed no differences across groups (p = .65). At the follow-up assessment, AAs showed greater sleep problems than EAs, as indexed by perceived quality (p = .024), duration (p = .005), and efficiency (p = .025). Findings were in the same direction but non-significant for efficiency (p = .12).
Changes in sleep problems during the 1.5 year period were investigated using structural equation models, with the four indicators of sleep problems creating latent factors at each wave. Results indicated that participants reported experiencing more sleep problems at T2 than at the baseline (Mdifference = .10, SE = .04, p = .013), equivalent to .32 SD units.
Primary Analyses
To test the first hypothesis, an initial model (M1) was estimated to assess the main effect of race on sleep problems at T2 controlling for sex, age and sleep problems at T1. As hypothesized, results indicated that AAs had larger increases in sleep problems over the 1.5 year period than did EAs (B = .17, p = .033, 95% CI [.01, .32]; βstandardized = .22). The magnitude of the estimated race difference was equivalent to a .56 standard deviations (SDs) greater increase in sleep problems among AAs than EAs (based on SD units of sleep problems at T1).
An additional model (M2) was then estimated to test the mediating effect of perceived discrimination (hypothesis 2). The full model (depicted in Figure 1 with standardized coefficients) showed good fit: χ2/df = 1.13; CFI = .97; RMSEA = .031, 90% CI [.000, .066]. As hypothesized, race was associated with perceived discrimination such that AAs reported higher levels than EAs (B = .77, p < .001, 95% CI [.60, .95]; βstand. = .66). Furthermore, perceived discrimination was associated with changes in sleep problems (B = .31, p = .011, 95% CI [.07, .55]; βstand. = .46), and accounted for race differences in sleep, such that they become non-significant and close to zero after perceived discrimination was included in the model (B = −.07, p = .47, 95% CI [−.24, .11]; βstand. = −.08). For each SD unit increase in perceived discrimination, the associated increase in sleep problems was .59 SD units. The indirect effect of race on sleep problems through perceived discrimination was found to be significant: B = .25, p = .021, 95% CI [.09, .46]; βstand. = .31.
Due to known associations with race and sleep (A. N. Beck, Finch, Lin, Hummer, & Masters, 2014; Magee, Caputi, & Iverson, 2011; Vorona et al., 2005), additional analyses were conducted to consider the findings when parent education, body mass index, self-rated physical health, and depressive symptoms were included as covariates. When all covariates were added as predictors of T2 sleep problems, the race effect remained similar and significant (B = .18, p = .033). Mediation findings also remained similar with the effects of perceived discrimination on sleep being significant and of a similar magnitude (B = .32, p = .010), and the indirect effect of race on sleep problems via perceived discrimination remaining unchanged (B = .25, p = .019). In models that were further adjusted for family income, the race effect on changes in sleep problems in M1 was attenuated 7% but remained marginally significant (p=.098). Analysis were also conducted to consider whether any of our model paths (i.e., direct or indirect effects) were moderated by background socioeconomic status (parents’ income or education). However, no such moderation effects were found.
Additional Analyses
Sensitivity analyses were also conducted to consider whether the above findings would hold under three alternative formulations of the sleep problems measures: (1) using composite scores for sleep problems at T1 and T2 instead of latent variables, (2) using the PSQI global score at T2 controlling for the sleep problems composite at T1, and (3) for each of the four sleep measures considered separately. All models included age, gender, and baseline sleep measures as controls.
Composite Scores
Non-latent composite scores were calculated separately at T1 and T2 as the mean of the four standardized sleep measures (latency, duration, efficiency, and quality) with higher scores indicating greater sleep problems. Results of the models with composite scores showed that AAs had greater changes in sleep problems from T1 to T2 (B = .29, p = .016, 95% CI [.05, .52]; βstand. = .20). Racial discrimination was also a significant predictor of changes in sleep (B = .47, p < .001, 95% CI [.22, .72]; βstand.= .38) and accounted for the race difference (B = −.07, p = .64). Moreover, the indirect effect of race on sleep problems through perceived discrimination was significant: B = .37, p = .017, 95% CI [.10, .81]; βstand. = .25. These findings are therefore consistent with those reported above for the latent variable models.
PSQI Global Score
A sleep problems global score was calculated using established PSQI scoring procedures, which involves summing sleep problems across seven domains: latency, duration, efficiency, quality, sleep disturbances, use of sleep medication, and daytime dysfunction (Buysse et al., 1989). Models were then estimated with the global score as the outcome and the T1 composite score for sleep problems included as a control. Although a measure of sleep problems at T1 is included as a control, because there is not measurement equivalence across time periods, analyses for these models cannot be interpreted in relation to “change” in sleep problems. Results of these models showed the same pattern of findings as reported above. Specifically, controlling for T1 sleep problems, AAs had higher PSQI global scores (i.e., more sleep problems) at T2 (B = 1.18, p = .012, 95% CI [.26, 2.10]; βstand. = .20). Racial discrimination was also a significant predictor of PSQI at T2 (B = 1.32, p = .012, 95% CI [.29, 2.34]; βstand. = .26) and accounted for the race difference (B = 0.20, p = .74). The indirect effect of race on sleep problems through perceived discrimination was as follows: B = 1.02, p = .13, 95% CI [−.21, 2.33]; βstand. = .35.
Individual Sleep Problems Measures
In models considering each of the sleep measures separately, the overall pattern of findings was comparable across the four measures with some variability in the magnitude of effects. Full support for the mediation model was found for sleep duration. AAs had greater increases in duration problems over the 1.5 year period than EAs (B = .30, p = .036; βstand. = .19). Discrimination was also associated with increases in duration problems (B = .45, p = .013; βstand. = .34), and the race difference became non-significant when discrimination was accounted for (B = −.04, p = .79). A significant indirect effect of race on sleep problems via perceived discrimination was found (B = 0.35, p = .017, 95% CI [.06, .64]; βstand. = .23). The findings were very similar but some paths were marginally significant for latency and perceived overall quality. AAs had marginally greater increases in sleep latency (B = 6.42, p = .095; βstand. = .15) and decreases in quality (B = −.20, p = .061; βstand. = −.15). Discrimination was also associated with increases in latency (B = 13.47, p = .036; βstand. = .37), and marginally associated with decreases in perceived overall quality (B = −.27, p = .092; βstand. = −.24). Additionally, the race difference was attenuated for both latency (B = −3.71, p = .46) and quality (B = .01, p = .97) when discrimination was accounted for. With respect to unstandardized estimates, indirect effects did not reach statistical significance (latency: B = 10.40, p = .061, 95% CI [.13, 1.47], βstand. = .25; quality: B = 0.21, p = .13, 95% CI [−.06, .50], βstand. = .16). However, the standardized estimate and confidence interval did indicate a significant indirect effect of race on sleep latency (p=.031). Findings for sleep efficiency were in the same direction but path estimates were not significant. In particular, changes in sleep efficiency were not significantly different across racial groups (B = −.03, p = .16; βstand. = −.12), nor was the association between racial discrimination and changes in efficiency (B = −.02, p = .29; βstand. = −.13).
Discussion
Racial disparities in health and wealth remain substantial in the United States (Williams, 2012). Illuminating mechanisms for the differential financial and health consequences of educational advancement across racial/ethnic groups may provide important insight into how such disparities endure as well as reveal potential barriers to upward mobility for marginalized groups (Fuller-Rowell, Curtis, Doan, & Coe, 2015; O’Hara, Gibbons, Weng, Gerrard, & Simons, 2012). For example, differential exposure to stressors during the college years may limit the extent to which individuals derive benefits from higher education. Herein, we examined changes in sleep problems among AA and EA college students attending a large, predominantly White university, and the mediating role of perceived discrimination. Results indicated that AA students had greater increases in sleep problems than EAs over a 1.5 year period. Additionally, perceived racial discrimination predicted changes in sleep problems, and accounted for race differences in sleep problems over time.
The findings extend previous cross-sectional research on racial disparities in sleep (Ruiter et al., 2011), and build on prior work indicating that AA students experience higher levels of racial discrimination than EA students across the college years (Nora & Cabrera, 1996; Priest et al., 2013). In particular, the findings show that perceived discrimination for AA students is impacting their sleep in ways that lead their sleep to diverge from their White majority peers. By documenting racial group differences in sleep over time, the findings suggest that experiences during the early years of college contribute to discrepancies in a fundamental bioregulatory system needed for good health and cognitive functioning – namely, sufficient and high quality sleep. That experiences of racial discrimination mediate this effect, underscores the idea that the process of pursuing higher education, a prerequisite for future life advancement, may be uniquely stressful and health compromising for under-represented minorities (Ancis et al., 2000; Smedley, Myers, & Harrell, 1993; Walton & Cohen, 2011).
The psychological and biological mechanisms linking discrimination to sleep remain to be elucidated (Slopen et al., 2015). However, extant research indicates that experiences of discrimination are associated with subsequent rumination, psychological distress, and substance use (Fuller-Rowell et al., 2011; Lewis, Cogburn, & Williams, 2015; Miranda, Polanco-Roman, Tsypes, & Valderrama, 2013). Such experiences in turn have physiologic consequences which when repeated over time can lead to dysregulation of biological systems including those associated with sleep (Juster & McEwen, 2015; Merritt, Bennett, Williams, Edwards, & Sollers, 2006). One important direction for future research will therefore be to explicate mechanisms for the effects of discrimination on sleep, of which there are likely to be several (e.g., perceived stress, physiologic dysregulation). Studies considering whether changes over time in reported levels of discrimination account for changes in sleep problems will also be an important extension of extant research.
An additional contribution of this study is to extend cross-sectional research on perceived discrimination and sleep in AA and EA samples (Grandner et al., 2012; Lewis et al., 2013; Tomfohr et al., 2012). In particular, the findings indicate a prospective effect of perceived discrimination on sleep problems, and that perceived discrimination accounts for race differences in sleep over time. The findings also add to this work by showing that perceived discrimination is prospectively associated with sleep disruption. That race-related experiences in college are linked to group differences in sleep over time, suggests that additional or different university-level programming to address the root causes of group disparities may be needed.
In addition to considering overall sleep problems, each of the four sleep indicators (duration, latency, quality, and efficiency) was considered separately. The pattern of findings was comparable across the four measures with some variability in the magnitude of effects. Full support for the mediation model was found for sleep duration and the findings were very similar but slightly reduced in magnitude for latency and quality. Findings for sleep efficiency were in the same direction, but the magnitude of the race difference in efficiency was two thirds that of duration, and the magnitude of the association between discrimination and efficiency was one third that of duration. Assessment of multiple sleep parameters allows for explication of effects and facilitates comparison of findings with extant literature. Overall, the results appear to be largely consistent across the sleep parameters and interpretation of the differences that were found in this study, in the context of this relatively young literature, would be overly speculative.
Some limitations should be noted. Firstly, although subjective measures of sleep are useful, objective measures should also be considered in future work (Sadeh, 2011). Secondly, because this study focused on a sample of students at one large predominantly White university in the Midwestern United States, the findings are not easily generalized to other contexts. Variability is likely to exist across colleges depending on the demographics of the student body, and the degree to which the institution actively cultivates an inclusive climate and provides support to students from underrepresented groups. Examination of this contextual variability and its determinants is an important avenue for future research. Furthermore, AA students in other types of university environments, such as historically Black colleges, would offer a valuable comparison. Students in such contexts may be insulated from the race-related stresses that influence sleep at predominantly White universities, and thus experience lower levels of discrimination and associated increases in sleep problems across the college years. Alternatively, if being Black in America is the operative variable, then experiences of discrimination and declines in sleep duration and quality similar to those found in this study would be expected among students attending historically Black institutions.
Common rater effects are also a threat to validity, and thus a limitation in all studies that consider associations between self-report measures. However, this limitation is decreased when considering changes over time (minimizing the effect of trait-based reporting biases), and when the mediator and the outcome are assessed at different time points (avoiding mood-state effects). Lastly, because this study was not experimental, untested third variable explanations cannot be ruled out. However, the results were robust to controls for socioeconomic status, body mass index, self-rated health, and depression.
Overall, the findings suggest that studies identifying factors that reduce experiences of racial discrimination for African Americans, or mitigate its damaging consequences, are warranted. Reducing racial discrimination may not only improve campus climate and sleep but also the enrollment, retention, and graduation rates of minority students (O’Hara et al., 2012; Wei, Ku, & Liao, 2011). Identifying specific programs on college campuses that can reduce racism and discrimination or improve campus climate is therefore likely to be of paramount importance in the broader movement to eliminate racial inequities in health and wealth. Furthermore, considering the relative impact of various types of initiatives to improve the college experience for minority students will be essential for illuminating the most impactful and cost-effective mechanisms for the reduction of group disparities.
Table 2.
Bivariate Correlations Among Study Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Race (Black=1, White=0) | – | |||||||||||||||
| 2. Gender (Male=1; Female=0) | −.07 | – | ||||||||||||||
| 3. Age (T1) | .07 | .23 | – | |||||||||||||
| 4. Parents’ education (T1) | −.07 | −.02 | −.15 | – | ||||||||||||
| 5. Parents’ income (T1) | −.35 | −.03 | −.15 | .44 | – | |||||||||||
| 6. Perceived discrimination (T1) | .66 | −.15 | .12 | .04 | −.14 | – | ||||||||||
| 7. Depressive symptoms (T1) | .27 | −.07 | .10 | −.24 | −.33 | .19 | – | |||||||||
| 8. Self-rated health (T1) | −.13 | .25 | .01 | .20 | .15 | −.08 | −.21 | – | ||||||||
| 9. Body mass index (T1) | .21 | .01 | −.03 | −.12 | −.17 | .10 | .06 | −.15 | – | |||||||
| 10. Sleep Quality (T1) | −.09 | −.09 | −.07 | .03 | −.02 | −.07 | −.32 | .15 | −.02 | – | ||||||
| 11. Sleep Duration Problems (T1) | .27 | −.11 | −.02 | −.12 | −.08 | .20 | .30 | −.22 | .26 | −.37 | – | |||||
| 12. Sleep Latency (T1) | .13 | .06 | .09 | .05 | −.05 | .02 | .33 | −.01 | −.08 | −.34 | −.02 | – | ||||
| 13. Sleep Efficiency (T1) | −.04 | .12 | .02 | .14 | .08 | .03 | −.21 | .08 | .03 | .25 | −.28 | −.30 | – | |||
| 14. Sleep Quality (T2) | −.20 | .10 | −.13 | .14 | .09 | −.28 | −.28 | .10 | −.01 | .31 | −.26 | −.17 | .16 | – | ||
| 15. Sleep Duration Problems (T2) | .26 | −.06 | .08 | .06 | −.11 | .38 | .12 | −.08 | .08 | −.17 | .38 | −.05 | −.04 | −.38 | – | |
| 16. Sleep Latency (T2) | .20 | .03 | .06 | −.01 | −.11 | .31 | .20 | −.14 | −.11 | −.14 | .04 | .36 | .00 | −.37 | .30 | – |
| 17. Sleep Efficiency (T2) | −.14 | −.01 | −.15 | .08 | .15 | −.16 | −.24 | .08 | −.01 | .26 | −.24 | −.20 | .14 | .32 | −.48 | −.31 |
Note. Bivariate correlations greater than .17 are significant at p < .05.
Acknowledgments
Support was provided by the Robert Wood Johnson Health and Society Scholars Program at the University of Wisconsin—Madison, and by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. An earlier version of this paper was presented at the Annual Meeting of the American Psychosomatic Society in Savannah, GA, March 2015. We thank Catasha Davis, Linn Jennings, Kristen McGuiggan, Taylor Mikulsky, and Ryan Svoboda for assistance with data collection.
Footnotes
It should be noted that, although the EA students targeted for recruitment were a stratified random sample, because recruitment was stopped when the target sample size was reached, the sample of actual participants is no longer completely random.
A continuously coded measure of duration was also considered as an alternative specification; the substantive findings using this measure were comparable to those reported below, but the magnitude of the race difference in sleep problems over time was smaller (both for duration and for the latent sleep problems construct).
Following best practices for longitudinal analysis of latent variables, factor loadings and intercepts of identical sleep indicators were constrained to be equal across time in all models. This ensures that latent factors are comparable across time. Residual variances between T1 and T2 latency and between T1 and T2 duration were allowed to covary. Error covariances within each time point were also allowed between latency and duration because short durations may lead to artificially short latencies.
References
- Ancis JR, Sedlacek WE, Mohr JJ. Student perceptions of campus cultural climate by race. Journal of Counseling & Development. 2000;78:180–185. http://doi.org/10.1002/j.1556-6676.2000.tb02576.x. [Google Scholar]
- Beatty DL, Hall MH, Kamarck TA, Buysse DJ, Owens JF, Reis SE, Matthews KA. Unfair treatment is associated with poor sleep in African American and Caucasian adults: Pittsburgh SleepSCORE project. Health Psychology. 2011;30:351–359. doi: 10.1037/a0022976. http://doi.org/10.1037/a0022976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AN, Finch BK, Lin SF, Hummer RA, Masters RK. Racial disparities in self-rated health: Trends, explanatory factors, and the changing role of socio-demographics. Social Science & Medicine. 2014;104:163–177. doi: 10.1016/j.socscimed.2013.11.021. http://doi.org/10.1016/j.socscimed.2013.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. 1996. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. http://doi.org/10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. European Heart Journal. 2011;32:1484–1492. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- De Lange AH, Kompier MAJ, Taris TW, Geurts SAE, Beckers DGJ, Houtman ILD, Bongers PM. A hard day’s night: A longitudinal study on the relationships among job demands and job control, sleep quality and fatigue. Journal of Sleep Research. 2009;18:374–383. doi: 10.1111/j.1365-2869.2009.00735.x. http://doi.org/10.1111/j.1365-2869.2009.00735.x. [DOI] [PubMed] [Google Scholar]
- DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality Prediction with a Single General Self-Rated Health Question. Journal of General Internal Medicine. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. http://doi.org/10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, Buckhalt JA. Economic adversity and children’s sleep problems: Multiple indicators and moderation of effects. Health Psychol. 2013;32:849–859. doi: 10.1037/a0030413. http://doi.org/10.1037/a0030413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Bagley EJ, Keiley MK, Erath SA. Growth in Body Mass Index From Childhood Into Adolescence: The Role of Sleep Duration and Quality. The Journal of Early Adolescence. 2014 0272431613519499. http://doi.org/10.1177/0272431613519499.
- Fisher CB, Wallace SA, Fenton RE. Discrimination Distress During Adolescence. Journal of Youth and Adolescence. 2000;29(6):679–695. http://doi.org/10.1023/A:1026455906512. [Google Scholar]
- Fuller-Rowell TE, Cogburn CD, Brodish AB, Peck SC, Malanchuk O, Eccles JS. Racial discrimination and substance use: Longitudinal associations and identity moderators. Journal of Behavioral Medicine. 2011;35:581–590. doi: 10.1007/s10865-011-9388-7. http://doi.org/10.1007/s10865-011-9388-7. [DOI] [PubMed] [Google Scholar]
- Fuller-Rowell TE, Curtis DS, Doan SN, Coe CL. Racial disparities in the health benefits of educational attainment: A study of inflammatory trajectories among African American and white adults. Psychosomatic Medicine. 2015;77(1):33–40. doi: 10.1097/PSY.0000000000000128. http://doi.org/10.1097/PSY.0000000000000128. [DOI] [PubMed] [Google Scholar]
- Fuller-Rowell TE, Evans GW, Ong AD. Poverty and health: The mediating role of perceived discrimination. Psychological Science. 2012;23(7):734–739. doi: 10.1177/0956797612439720. http://doi.org/10.1177/0956797612439720. [DOI] [PubMed] [Google Scholar]
- Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, Troxel WM. Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behavioral Sleep Medicine. 2012;10:235–249. doi: 10.1080/15402002.2012.654548. http://doi.org/10.1080/15402002.2012.654548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Petrov MER, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine. 2013;9(9):897–905. doi: 10.5664/jcsm.2990. http://doi.org/10.5664/jcsm.2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell SP. The racism and life experiences scales. 1994 Unpublished Manuscript. [Google Scholar]
- Harrell SP. A multidimensional conceptualization of racism-related stress: implications for the well-being of people of color. Am J Orthopsychiatry. 2000 Jan;70:42–57. doi: 10.1037/h0087722. [DOI] [PubMed] [Google Scholar]
- Hayes AF, Scharkow M. The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis: Does method really matter? Psychological Science. 2013;24(10):1918–1927. doi: 10.1177/0956797613480187. http://doi.org/10.1177/0956797613480187. [DOI] [PubMed] [Google Scholar]
- Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, Hazen N, Herman J, Katz ES, Kheirandish-Gozal L, Neubauer DN, O’Donnell AE, Ohayon M, Peever J, Rawding R, Sachdeva RC, Setters B, Vitiello MV, Ware JC, Hillard PJA. National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health. 2015 Mar;1(1):40–3. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- Huynh VW, Gillen-O’Neel C. Discrimination and sleep: the protective role of school belonging. Youth Soc. 2013 [Epub ahead of print]; Available from: http://yas.sagepub.com/content/early/2013/10/24/0044118X13506720.
- Colten HR, Altevogt BM, editors. Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington (DC): National Academies Press (US); 2006. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK19960/ [PubMed] [Google Scholar]
- Juster RP, McEwen BS. Sleep and chronic stress: new directions for allostatic load research. Sleep Medicine. 2015;16(1):7–8. doi: 10.1016/j.sleep.2014.07.029. http://doi.org/10.1016/j.sleep.2014.07.029. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999;40(3):208–230. [PubMed] [Google Scholar]
- Killgore WDS, Kahn-Greene ET, Lipizzi EL, Newman RA, Kamimori GH, Balkin TJ. Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep Medicine. 2008;9(5):517–526. doi: 10.1016/j.sleep.2007.07.003. http://doi.org/10.1016/j.sleep.2007.07.003. [DOI] [PubMed] [Google Scholar]
- Kim EJ, Dimsdale JE. The Effect of Psychosocial Stress on Sleep: A Review of Polysomnographic Evidence. Behavioral Sleep Medicine. 2007;5(4):256–278. doi: 10.1080/15402000701557383. http://doi.org/10.1080/15402000701557383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson KL. Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab. 2010 Oct;24:731–43. doi: 10.1016/j.beem.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Discrimination and Health Inequities. International Journal of Health Services. 2014;44(4):643–710. doi: 10.2190/HS.44.4.b. http://doi.org/10.2190/HS.44.4.b. [DOI] [PubMed] [Google Scholar]
- Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: Validity and reliability of a self-report measure for population health research on racism and health. Social Science & Medicine. 2005;61(7):1576–1596. doi: 10.1016/j.socscimed.2005.03.006. http://doi.org/10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- Lewis TT, Cogburn CD, Williams DR. Self-Reported Experiences of Discrimination and Health: Scientific Advances, Ongoing Controversies, and Emerging Issues. Annual Review of Clinical Psychology. 2015;11(1):407–440. doi: 10.1146/annurev-clinpsy-032814-112728. http://doi.org/10.1146/annurev-clinpsy-032814-112728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Troxel WM, Kravitz HM, Bromberger JT, Matthews KA, Hall MH. Chronic exposure to everyday discrimination and sleep in a multiethnic sample of middle-aged women. Health Psychology. 2013;32:810–819. doi: 10.1037/a0029938. http://doi.org/10.1037/a0029938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. Journal of Adolescent Health. 2010;46:124–132. doi: 10.1016/j.jadohealth.2009.06.016. http://doi.org/10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593. doi: 10.1146/annurev.psych.58.110405.085542. http://doi.org/10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magee CA, Caputi P, Iverson DC. Relationships between self-rated health, quality of life and sleep duration in middle aged and elderly Australians. Sleep Medicine. 2011;12:346–350. doi: 10.1016/j.sleep.2010.09.013. http://doi.org/10.1016/j.sleep.2010.09.013. [DOI] [PubMed] [Google Scholar]
- Merritt MM, Bennett GG, Williams RB, Edwards CL, Sollers JJ. Perceived racism and cardiovascular reactivity and recovery to personally relevant stress. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2006;25(3):364–369. doi: 10.1037/0278-6133.25.3.364. http://doi.org/10.1037/0278-6133.25.3.364. [DOI] [PubMed] [Google Scholar]
- Miranda R, Polanco-Roman L, Tsypes A, Valderrama J. Perceived discrimination, ruminative subtypes, and risk for depressive symptoms in emerging adulthood. Cultural Diversity & Ethnic Minority Psychology. 2013;19(4):395–403. doi: 10.1037/a0033504. http://doi.org/10.1037/a0033504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nora A, Cabrera AF. The role of perceptions of prejudice and discrimination on the adjustment of minority students to college. The Journal of Higher Education. 1996;67:119–148. http://doi.org/10.2307/2943977. [Google Scholar]
- O’Hara RE, Gibbons FX, Weng CY, Gerrard M, Simons RL. Perceived racial discrimination as a barrier to college enrollment for African Americans. Personality and Social Psychology Bulletin. 2012;38:77–89. doi: 10.1177/0146167211420732. http://doi.org/10.1177/0146167211420732. [DOI] [PubMed] [Google Scholar]
- Ong AD, Fuller-Rowell T, Burrow AL. Racial discrimination and the stress process. Journal of Personality and Social Psychology. 2009;96(6):1259–1271. doi: 10.1037/a0015335. http://doi.org/10.1037/a0015335. [DOI] [PubMed] [Google Scholar]
- Orzech KM, Salafsky DB, Hamilton LA. The state of sleep among college students at a large public university. Journal of American College Health: J of ACH. 2011;59(7):612–619. doi: 10.1080/07448481.2010.520051. http://doi.org/10.1080/07448481.2010.520051. [DOI] [PubMed] [Google Scholar]
- Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29(7):881–889. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrov ME, Lichstein KL. Differences in sleep between black and white adults: an update and future directions. Sleep Med [Internet] 2015 doi: 10.1016/j.sleep.2015.01.011. [cited 2015 Jan 27]; Available from: http://www.sleep-journal.com/article/S138994571500057X/abstract. [DOI] [PubMed]
- Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Social Science & Medicine. 2013;95:115–127. doi: 10.1016/j.socscimed.2012.11.031. http://doi.org/10.1016/j.socscimed.2012.11.031. [DOI] [PubMed] [Google Scholar]
- Ruiter ME, DeCoster J, Jacobs L, Lichstein KL. Sleep disorders in African Americans and Caucasian Americans: a meta-analysis. Behav Sleep Med. 2010 Sep 23;8:246–59. doi: 10.1080/15402002.2010.509251. [DOI] [PubMed] [Google Scholar]
- Ruiter ME, DeCoster J, Jacobs L, Lichstein KL. Normal sleep in African-Americans and Caucasian-Americans: a meta-analysis. Sleep Med. 2011 Mar;12:209–14. doi: 10.1016/j.sleep.2010.12.010. [DOI] [PubMed] [Google Scholar]
- Sadeh A. Sleep assessment methods. In: El-Sheikh M, editor. Sleep and Development: Familial and Socio-cultural Considerations. New York, NY, US: Oxford University Press; 2011. pp. 355–371. [Google Scholar]
- Sadeh A. Iii. Sleep Assessment Methods. Monographs of the Society for Research in Child Development. 2015;80(1):33–48. doi: 10.1111/mono.12143. http://doi.org/10.1111/mono.12143. [DOI] [PubMed] [Google Scholar]
- Schnittker J, Bacak V. The Increasing Predictive Validity of Self-Rated Health. PLOS ONE. 2014;9(1):e84933. doi: 10.1371/journal.pone.0084933. http://doi.org/10.1371/journal.pone.0084933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellers RM, Caldwell CH, Schmeelk-Cone KH, Zimmerman MA. Racial Identity, Racial Discrimination, Perceived Stress, and Psychological Distress among African American Young Adults. Journal of Health and Social Behavior. 2003;44(3):302–317. http://doi.org/10.2307/1519781. [PubMed] [Google Scholar]
- Sellers RM, Shelton JN. The role of racial identity in perceived racial discrimination. Journal of Personality and Social Psychology. 2003;84:1079–1092. doi: 10.1037/0022-3514.84.5.1079. [DOI] [PubMed] [Google Scholar]
- Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Med Rev. 2014 Feb;18:75–87. doi: 10.1016/j.smrv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- Slopen N, Lewis TT, Williams DR. Discrimination and sleep: a systematic review. Sleep Med. 2015 doi: 10.1016/j.sleep.2015.01.012. [Epub ahead of print] Available from: http://www.sciencedirect.com/science/article/pii/S1389945715000581. [DOI] [PMC free article] [PubMed]
- Smedley BD, Myers HF, Harrell SP. Minority-status stresses and the college adjustment of ethnic minority freshmen. The Journal of Higher Education. 1993;64:434–452. http://doi.org/10.2307/2960051. [Google Scholar]
- Steffen PR, Bowden M. Sleep disturbance mediates the relationship between perceived racism and depressive symptoms. Ethnicity & Disease. 2006;16:16–21. [PubMed] [Google Scholar]
- Sue DW. Microaggressions in Everyday Life: Race, Gender, and Sexual Orientation. John Wiley & Sons Inc; 2010. [Google Scholar]
- Tavernier R, Willoughby T. Bidirectional associations between sleep (quality and duration) and psychosocial functioning across the university years. Developmental Psychology. 2014;50(3):674–682. doi: 10.1037/a0034258. http://doi.org/10.1037/a0034258. [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Vatthauer KE, Bramoweth AD, Ruggero C, Roane B. The Role of Sleep in Predicting College Academic Performance: Is it a Unique Predictor? Behavioral Sleep Medicine. 2013;11(3):159–172. doi: 10.1080/15402002.2011.602776. http://doi.org/10.1080/15402002.2011.602776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomfohr L, Pung MA, Edwards KM, Dimsdale JE. Racial differences in sleep architecture: the role of ethnic discrimination. Biol Psychol. 2012 Jan;89:34–8. doi: 10.1016/j.biopsycho.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Utsey SO. Assessing the stressful effects of racism: a review of instrumentation. J Black Psychol. 1998 Aug 1;24:269–88. [Google Scholar]
- Vorona RD, Winn MP, Babineau TW, Eng BP, Feldman HR, Ware JC. Overweight and obese patients in a primary care population report less sleep than patients with a normal body mass index. Archives of Internal Medicine. 2005;165:25–30. doi: 10.1001/archinte.165.1.25. http://doi.org/10.1001/archinte.165.1.25. [DOI] [PubMed] [Google Scholar]
- Walton GM, Cohen GL. A brief social-belonging intervention improves academic and health outcomes of minority students. Science. 2011;331:1447–1451. doi: 10.1126/science.1198364. http://doi.org/10.1126/science.1198364. [DOI] [PubMed] [Google Scholar]
- Wei M, Ku TY, Liao KYH. Minority stress and college persistence attitudes among African American, Asian American, and Latino students: perception of university environment as a mediator. Cultural Diversity & Ethnic Minority Psychology. 2011;17(2):195–203. doi: 10.1037/a0023359. http://doi.org/10.1037/a0023359. [DOI] [PubMed] [Google Scholar]
- Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37(3):601–611. doi: 10.5665/sleep.3508. http://doi.org/10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR. Miles to go before we sleep: racial inequities in health. J Health Soc Behav. 2012 Sep 1;53:279–95. doi: 10.1177/0022146512455804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, John DA, Oyserman D, Sonnega J, Mohammed SA, Jackson JS. Research on Discrimination and Health: An Exploratory Study of Unresolved Conceptual and Measurement Issues. American Journal of Public Health. 2012;102(5):975–978. doi: 10.2105/AJPH.2012.300702. http://doi.org/10.2105/AJPH.2012.300702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Racism and health I: Pathways and scientific evidence. American Behavioral Scientist. 2013 doi: 10.1177/0002764213487340. http://doi.org/10.1177/0002764213487340. [DOI] [PMC free article] [PubMed]
- Williams DR, Yan Yu, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2(3):335–351. doi: 10.1177/135910539700200305. http://doi.org/10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Yoo SS, Gujar N, Hu P, Jolesz FA, Walker MP. The human emotional brain without sleep — a prefrontal amygdala disconnect. Current Biology. 2007;17(20):R877–R878. doi: 10.1016/j.cub.2007.08.007. http://doi.org/10.1016/j.cub.2007.08.007. [DOI] [PubMed] [Google Scholar]
- Yoo SS, Hu PT, Gujar N, Jolesz FA, Walker MP. A deficit in the ability to form new human memories without sleep. Nature Neuroscience. 2007;10(3):385–392. doi: 10.1038/nn1851. http://doi.org/10.1038/nn1851. [DOI] [PubMed] [Google Scholar]


