Abstract
Objective:
Studies related to sleep disorders and polysomnography (PSG) among chronic daily headache patients are rare. We studied this and compared chronic migraine (CM) with chronic tension-type headache.
Methods:
Eighty-three patients were recruited. They were evaluated by semi-structured interview, headache, and sleep diaries along with Epworth Sleepiness Scale score and insomnia symptom score. Overnight PSG was performed and data compared.
Results:
Chronic tension-type headache was more common than CM, both having female preponderance. Insomnia followed by excessive daytime sleepiness was prevalent sleep disorder. Sleep efficiency and Stage 3 sleep were lower in CM compared to chronic tension-type. ESSS was significantly increased among chronic tension-type patients. No significant correlation was found among PSG parameters in patients with or without sleep disorders.
Conclusion:
Insomnia being most common sleep disorder among chronic headache population. Chronic tension-type headache had slightly better slow-wave sleep than CM and significantly increased daytime sleepiness.
KEYWORDS: Chronic daily headache, insomnia, polysomnography, sleep
INTRODUCTION
Headache and sleep have a complex interrelationship with each other.[1] Many headache sufferers complaint that headache leads to sleep disruption in them while on the other hand, inadequate sleep leads to increased frequency, severity, and chronicity of headache.[2,3] This relationship is well documented in primary headache disorders, particularly in chronic headache sufferers as compared to episodic variety.[1,3]
Chronic daily headache (CDH) comprises a group of headache disorders occurring at least 15 days per month for 3 or more consecutive months. Around 5% of the normal population suffers from CDH.[4] Among the many sleep disorders described in the International Classification of Sleep Disorders,[5] insomnia, daytime sleepiness, and obstructive sleep apnea including snoring have been linked to chronic headache.[6] Insomnia had been suggested as an independent risk factor for chronification of headache.[7] Increased snoring incidence had been observed in chronic headache sufferers compared to episodic ones.[8] Sleep disordered breathing was found to be associated with migraine but not with tension headache.[9] These disorders are commonly left under diagnosed and when treated helps in better control of headache.[10]
Polysomnography (PSG) is used for objectively assessing sleep macro- and micro-architecture and aids in detecting sleep disorders. The majority of the earlier studies had studied migraine population,[11,12] few had studied tension-type headache,[13] and very few both.[14,15] The data on chronic headache type is very sparse.
We performed the study to evaluate subjectively and objectively sleep disorders in patients of primary CDH. A secondary subgroup analysis was performed in between chronic migraine (CM) and chronic tension-type headache (CTTH) patients and polysomnographic variables among them were compared.
METHODS
This was a prospective, hospital-based observational study carried out at our tertiary care hospital over a span of 2 years from October 2013 to December 2015. 83 patients of primary CDH were selected from patients attending outpatient department (OPD). Patients were diagnosed by the International Classification of Headache Disorder-3 beta classification.[16] These patients were evaluated by history, clinical examination, sleep questionnaires, and overnight PSG study. The Institutional Ethical committee approval was obtained for the study. Written informed consent was taken from all patients.
Evaluation
Clinical details regarding total disease duration, headache type, location, character, duration of attack, and severity were assessed. Visual pain analog scale was used for severity assessment of pain. Sleep history included insomnia, daytime sleepiness, snoring, and limb movements. All patients were asked to fill a sleep diary for 1 month. Body mass index was calculated.
Sleep questionnaire assessment
The Epworth Sleepiness Scale (ESS)[17] was used for assessment of excessive daytime sleepiness, and a score of 10 or more was considered abnormal. Sum of individual's response in eight different situations over a scale of 0–3 is total score.
Insomnia symptom score (ISS) was used for assessing insomnia. Each patient was asked about difficulty falling asleep, intermittent night arousals, and early morning awakenings. The patient was asked to respond according to usual perceivement felt on most of the days (≥4) of week. Any positive reply was given a score of 1, making total score range of 0–3. Score 1 or more was taken as having insomnia.
Overnight polysomnography evaluation
All the patients were explained prior about the procedure of study and risks involved. The patient was asked to report in the night after washing hairs that morning. They were asked to avoid nap during day and were allowed light dinner. Drugs having impact on sleep were discontinued on the day of study. The overnight recording was performed using “somnologica” software (Embla Systems, Broomfield, CO, USA). Various leads were attached. When lights were put off, it was labeled as “lights off” time. The recording was continued till the patient wakes up which is “lights on” time. The recording analysis was done according to the American academy of sleep medicine guidelines 2007.[18] Data stored was reviewed, and necessary correction was made. The characteristics noted were time in bed, total sleep time, sleep efficiency, sleep onset latency, duration of sleep stages, apnea–hypopnea index (AHI), periodic limb movement index (PLMI), isolated limb movement index (ILMI), number of awakenings, oxygen saturation, and heart rate.
Statistical analysis
Statistical analysis was done using SPSS software of windows version 16.0 (Chicago, IL, USA). All categorical variables were expressed as percentages, and continuous variables were expressed as mean ± standard deviation. Categorical variables were compared using Chi-square test/Fisher's exact test. Continuous variables since not normally distributed were compared using Mann–Whitney U-test. All P < 0.05 were taken as statistically significant.
RESULTS
The mean age of patients was 31.57 ± 10.26 years. Female patients were more than male (female = 69.9%, male = 30.1%). The mean duration of headache of all patients was 24.99 (±20.72) months, with a range of 4–144 months. Mean severity of headache was 4.23 (±1.42).
Out of total 83 patients, 50 (60.2%) were diagnosed as CTTH, 31 (37.3%) as CM, and only 2 (2.4%) were of chronic cluster headache (CCH). Both CCH patients were male, and one had complaint of insomnia. Forty-two patients had complaints of sleep disturbance either insomnia or daytime sleepiness. Four patients complained of snoring. The mean ISS and ESS score of all patients were 0.73 (±0.9) and 5.35 (±3.23), respectively.
Our main results had been summarized in Table 1. Since CCH patients were only two, we statistically compared CM patients with CTTH. Both CM and CTTH patients had complaints of insomnia (14 vs. 20, P = 0.65) and daytime sleepiness (1 vs. 20, P < 0.05). CTTH had more of ISS (0.86 vs. 0.55, P = 0.16) and ESS score (3.61 vs. 2.06, P < 0.05). Average sleep duration diary and prolonged sleep onset latency (>30 min) were comparable into two groups.
Table 1.
Demographic, headache, and sleep-related data including questionnaire for all patients: Counts or mean (standard deviation)
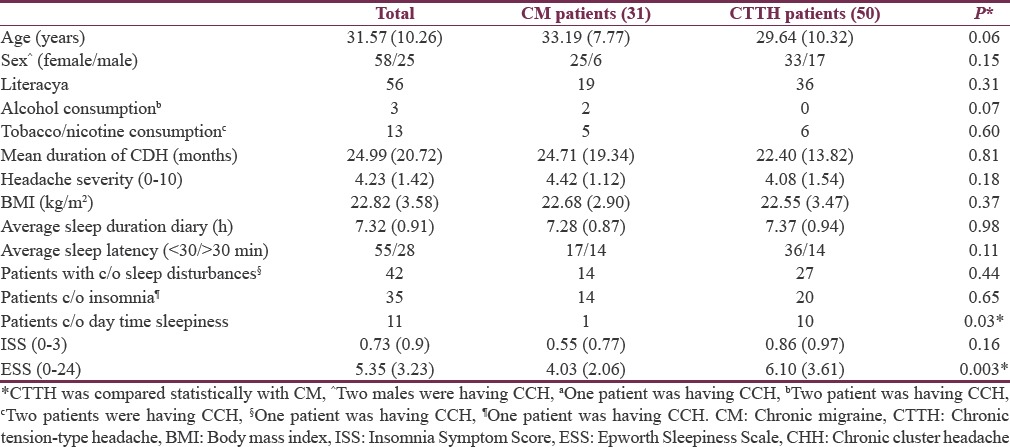
Table 2 summarizes the comparison of polysomnographic parameters among CM and chronic tension-type headache. Total sleep time, sleep efficiency, stage N3 sleep, and rapid eye movement sleep was prolonged in CTTH group though not statistically significant. Sleep onset latency, awakenings per hour, and wake time was more in CM group but not statistically significant. ILMI, PLMI, AHI, desaturation index, and heart rate were comparable among the two groups.
Table 2.
Comparison of polysomnographic parameters among chronic migraine and chronic tension-type headache patients: Mean (standard deviation)
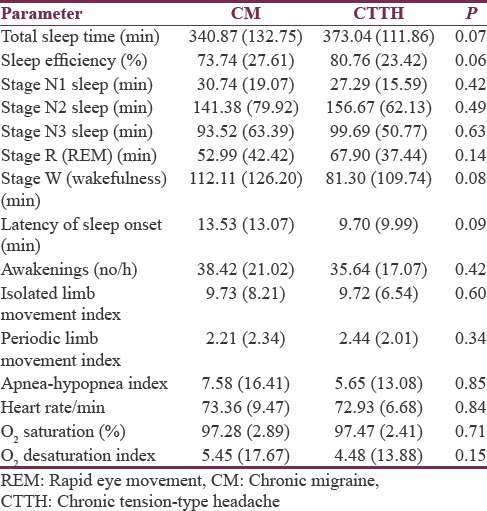
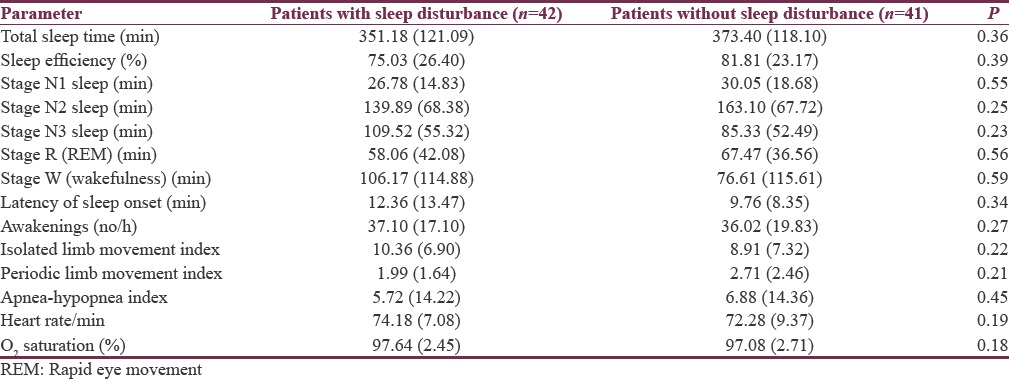
Table 3 summarizes the PSG parameters comparison among those complaining of sleep disturbance with those having no complaints. Total sleep time, sleep efficiency, stage N3 sleep, and sleep onset latency were comparable statistically among the groups along with ILMI, PLMI, AHI, heart rate, and O2 saturation.
Table 3.
Comparison of polysomnographic parameters among patients with/without symptom of sleep disturbances: Mean (standard deviation)
DISCUSSION
We studied 83 cases of CDH subjectively by history and questionnaire while PSG provided objective sleep parameters. Among those, more than half were of tension-type and females being more commonly affected which is similar to general population data. Nearly, half complained of sleep disturbances, insomnia being more common than excessive daytime sleepiness. Sancisi et al.[7] in his study found similar results. Increased prevalence of insomnia among headache sufferers had been described in the previous studies.[1]
Both CM and CTTH groups were comparable. Both ISS and ESS score were more in CTTH group with ESS score statistically significant. Sleep diaries revealed comparable average sleep duration and PSG showed comparable total sleep time and sleep onset latencies into two groups. It is well known that chronic insomniacs not always have poor EEG sleep.[19] In PSG, CTTH had more stage N3 sleep with lesser awakenings that is better sleep quality in comparison to CM group.[20] As De Gennaro et al.[21] in his study showed decreased arousals with increased slow wave sleep after sleep deprivation, our PSG findings could indicate more of sleep deprivation among chronic tension-type headache compared to CM.
Various PSG parameters such as ILMI, PLMI, AHI, and desaturation index did not differ significantly. Similar observation was found by Kristiansen et al.[12]
Certain limitations were in our study. We did not have control group in our study, but that is also the strength of study, for the first time a study comparing two major divisions of CDH had been performed. Second, we did not have follow-up of patients. A study design with repeating PSGs on follow-up probably will be more powerful. There was lack of gender matching among the groups. Our study group was population attending hospital OPD, thus more of chronic and severe sufferers.
CONCLUSION
Patients of CDH suffer from sleep disturbances, which are mainly subjective than objective. CTTH patients had marginally increased incidence of insomnia and excessive daytime sleepiness than CM. Calhoun and Ford[10] in his study, over migraine patients found that patients who received behavioral sleep therapy are more likely to revert to episodic migraine. Thus, earlier evaluation and timely management of these may help in better control of headache, improving its outcome, and possibly preventing chronification.[22]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ødegård SS, Engstrøm M, Sand T, Stovner LJ, Zwart JA, Hagen K. Associations between sleep disturbance and primary headaches: The third Nord-Trøndelag health study. J Headache Pain. 2010;11:197–206. doi: 10.1007/s10194-010-0201-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dodick DW, Eross EJ, Parish JM, Silber M. Clinical, anatomical, and physiologic relationship between sleep and headache. Headache. 2003;43:282–92. doi: 10.1046/j.1526-4610.2003.03055.x. [DOI] [PubMed] [Google Scholar]
- 3.Odegård SS, Sand T, Engstrøm M, Stovner LJ, Zwart JA, Hagen K. The long-term effect of insomnia on primary headaches: A prospective population-based cohort study (HUNT-2 and HUNT-3) Headache. 2011;51:570–80. doi: 10.1111/j.1526-4610.2011.01859.x. [DOI] [PubMed] [Google Scholar]
- 4.Castillo J, Muñoz J, Guitera V, Pascual J. Kaplan award 1998. Epidemiology of chronic daily headache in the general population. Headache. 1999;39:190–6. doi: 10.1046/j.1526-4610.1999.3903190.x. [DOI] [PubMed] [Google Scholar]
- 5.Daroff RB. The international classification of sleep disorders: Diagnostic and coding manual. Neurology. 1991;41:160. [Google Scholar]
- 6.Rains JC, Penzien DB. Chronic headache and sleep disturbance. Curr Pain Headache Rep. 2002;6:498–504. doi: 10.1007/s11916-002-0070-1. [DOI] [PubMed] [Google Scholar]
- 7.Sancisi E, Cevoli S, Vignatelli L, Nicodemo M, Pierangeli G, Zanigni S, et al. Increased prevalence of sleep disorders in chronic headache: A case-control study. Headache. 2010;50:1464–72. doi: 10.1111/j.1526-4610.2010.01711.x. [DOI] [PubMed] [Google Scholar]
- 8.Scher AI, Lipton RB, Stewart WF. Habitual snoring as a risk factor for chronic daily headache. Neurology. 2003;60:1366–8. doi: 10.1212/01.wnl.0000055873.71552.51. [DOI] [PubMed] [Google Scholar]
- 9.Vendrame M, Kaleyias J, Valencia I, Legido A, Kothare SV. Polysomnographic findings in children with headaches. Pediatr Neurol. 2008;39:6–11. doi: 10.1016/j.pediatrneurol.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 10.Calhoun AH, Ford S. Behavioral sleep modification may revert transformed migraine to episodic migraine. Headache. 2007;47:1178–83. doi: 10.1111/j.1526-4610.2007.00780.x. [DOI] [PubMed] [Google Scholar]
- 11.Göder R, Fritzer G, Kapsokalyvas A, Kropp P, Niederberger U, Strenge H, et al. Polysomnographic findings in nights preceding a migraine attack. Cephalalgia. 2001;21:31–7. doi: 10.1046/j.1468-2982.2001.00141.x. [DOI] [PubMed] [Google Scholar]
- 12.Kristiansen HA, Kværner KJ, Akre H, Overland B, Russell MB. Migraine and sleep apnea in the general population. J Headache Pain. 2011;12:55–61. doi: 10.1007/s10194-010-0268-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kristiansen HA, Kværner KJ, Akre H, Overland B, Russell MB. Tension-type headache and sleep apnea in the general population. J Headache Pain. 2011;12:63–9. doi: 10.1007/s10194-010-0265-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Drake ME, Jr, Pakalnis A, Andrews JM, Bogner JE. Nocturnal sleep recording with cassette EEG in chronic headaches. Headache. 1990;30:600–3. doi: 10.1111/j.1526-4610.1990.hed3009600.x. [DOI] [PubMed] [Google Scholar]
- 15.Engstrøm M, Hagen K, Bjørk MH, Stovner LJ, Sand T. Sleep quality and arousal in migraine and tension-type headache: The headache-sleep study. Acta Neurol Scand. 2014;129:47–54. doi: 10.1111/ane.12237. [DOI] [PubMed] [Google Scholar]
- 16.Road C. The international classification of headache disorders, 3rd edition (beta version) Cephalalgia. 2013;33:629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 17.Johns MW. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 18.Iber C, Ancoli-Israel S, Chesson AL, Jr, Quan SF. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology, and Technical Specifications. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 19.Rosa RR, Bonnet MH. Reported chronic insomnia is independent of poor sleep as measured by electroencephalography. Psychosom Med. 2000;62:474–82. doi: 10.1097/00006842-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Keklund G, Akerstedt T. Objective components of individual differences in subjective sleep quality. J Sleep Res. 1997;6:217–20. doi: 10.1111/j.1365-2869.1997.00217.x. [DOI] [PubMed] [Google Scholar]
- 21.De Gennaro L, Ferrara M, Bertini M. EEG arousals in normal sleep: Variations induced by total and selective slow-wave sleep deprivation. Sleep. 2001;24:673–9. doi: 10.1093/sleep/24.6.673. [DOI] [PubMed] [Google Scholar]
- 22.Rains JC. Chronic headache and potentially modifiable risk factors: Screening and behavioral management of sleep disorders. Headache. 2008;48:32–9. doi: 10.1111/j.1526-4610.2007.00972.x. [DOI] [PubMed] [Google Scholar]


