Abstract
Objective:
To study if nasal endoscope can be a reliable tool in assessing patients with allergic rhinitis.
Materials and Methods:
A prospective study. Patients who were diagnosed with allergic rhinitis underwent a nasal endoscopic examination performed by two physicians blinded to the scoring of each other. A correlation was made among symptom severity, endoscopic findings, and interrater variability.
Results:
Ninety patients were included in the study: 34 patients had mild disease and 56 had moderate-to-severe allergic rhinitis according to the Allergic Rhinitis and its Impact on Asthma guidelines. Increases in mucosal edema and bluish discoloration were predictive of the severity of allergic rhinitis disease (p < 0.05). The presence of nasal secretions was not predictive of allergic rhinitis. Interrater reliability was fair for mucosal edema, moderate-to-almost perfect for the rest of the endoscopic findings.
Conclusion:
Nasal endoscopy may reveal signs that are predictive of the severity of allergic rhinitis. A detailed checklist is needed for the nasal endoscopic examination to decrease interrater variability.
Keywords: Nasal endoscopy, allergic rhinitis, reliability, inter-rater variability, mucosal edema, nasal secretion, ARIA guidelines, nasal obstruction, congestion, postnasal drip.
Allergic rhinitis is defined as inflammation of the nasal mucosa that constitutes part of a systemic inflammatory process that affects mucous membranes and causes asthma, rhinosinusitis, and allergic conjunctivitis.1 It is a debilitating disease that affects people of all age groups, with a peak in the teenage years. It is estimated that the disease has a prevalence of 20% and affects ∼400 million people worldwide.2 These numbers were noted to be increasing over the past decade due to the change toward a more westernized life style, with a subsequent increase in economic burden on society not solely due to the medical cost of the disease but also to its effect on quality of life.3–5
With allergic asthma, allergic rhinitis is currently considered to be part of one global airway disease that can evolve and cause bronchial hyperresponsiveness if not treated appropriately.6,7 Patients usually present to the physician's clinic with one or more of the symptoms of nasal obstruction, congestion, rhinorrhea, sneezing, and itching. Some patients also report hyposmia, postnasal drip, and eye redness.8 The nasal mucosa of patients with allergic rhinitis is typically inflamed and hypertrophied. There is polypoid degeneration of the epithelium as well as a marked edema of the mucosa.9 Nasal tk;1obstruction is noted to be the most commonly presenting and debilitating symptom of allergic rhinitis, and it is caused by vasodilation of arterioles, venules, and capillaries as well as an increase in vessel permeability that leads to edema.10
Allergic rhinitis was traditionally classified as either seasonal or perennial based on the time of occurrence of symptoms. This classification has ceased to be used since the development of new Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines for the diagnosis and classification of allergic rhinitis.11 Allergic rhinitis is now diagnosed based on having the symptom of rhinorrhea along with one or more of the following symptoms: nasal itching, nasal obstruction, sneezing, or conjunctivitis.11 The diagnosis is clinical, based on symptoms and clinical examination findings. The first-line treatment in allergy is avoiding the allergen. Detection of the allergen might generally be required to apply the first steps of treatment even though the response to the treatment, i.e. avoiding the allergen, may hint towards the diagnosis. If available, allergy tests should be performed to support the diagnosis made during the physical examination and whenever a patient does not respond to empiric treatment or if the diagnosis is uncertain.12
The assessment of disease severity, according to the ARIA guidelines, is based on the clinical presentation and follow-ups.11 There are no objective measurements approved as a means for assessing disease severity. A nasal endoscopic examination is a quick test, which is part of the assessment of the otolaryngologist when examining a patient with nasal symptoms. It would be of great value if the nasal endoscope can have a role in the objective evaluation of patients with allergic rhinitis. The literature lacks enough studies that explored the role of nasal endoscope in assessing allergic rhinitis, and most studies highlighted the high rate of interrater variability while reporting endoscopic findings.13,14 The aim of this study was to evaluate the effectiveness of the nasal endoscope as a tool for assessing the severity of allergic rhinitis and for allowing better initial and further clinical assessments and thus better patient care.
METHODS
The institutional review board of the American University of Beirut approved this study. Patients > 18 years old who presented to the clinics of otolaryngology—head and neck surgery from September 2013 to August 2015 with symptoms of allergic rhinitis, such as nasal obstruction, serous rhinorrhea, and sneezing, were recruited. Patients who were taking any form of allergy treatment over the past 3 months and patients with a history of chronic rhinosinusitis and/or previous nasal surgery were excluded. The diagnosis of allergic rhinitis was confirmed by a skin-prick test (glycerol-based extracts; Allergopharma and Stallergenes). The patient was introduced to the two examining physicians (G.Z., M.M.) who performed, separately, the nasal endoscopic examination. Each physician filled out a similar checklist that includes a description of the septum, inferior turbinates, nasal valves, nasal mucosa, and secretions as well as the presence of nasal polyps. The patients were then divided into two groups, mild or moderate-severe, according to the ARIA guidelines.11 Each group was assessed separately by comparing the questionnaire results with the endoscopic examination findings. The associations were evaluated by using nonparametric tests, and significance was considered when the p value was <0.05. Also, the interrater variability was measured by using the Cohen κ coefficient. SPSS version 22 (SPSS Inc., Chicago, IL) was used to analyze the data obtained.
RESULTS
Demographic Data
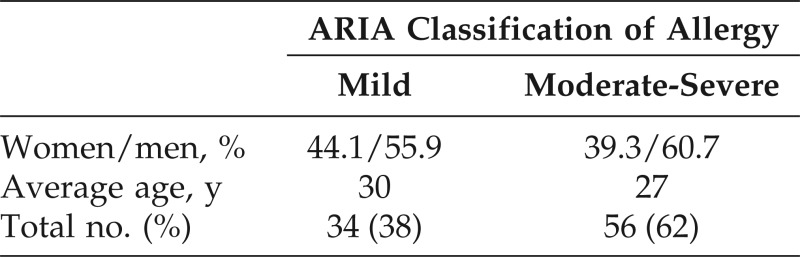
Ninety patients were included in the study. Thirty-four patients (38%) had mild disease and were listed as group 1, whereas 56 patients (62%) had a moderate-to-severe allergic rhinitis according to the ARIA guidelines and were listed as group 2.11 The mean age in groups 1 and 2 were 30 and 27 years old, respectively. In group 1, 19 were male patients (55.9%) and 15 were female patients (44.1%) compared with 34 male patients (60.7%) and 22 female patients (39.3%) in group 2 (Table 1).
Table 1.
Demographic data
ARIA = Allergic Rhinitis and its Impact on Asthma.
Nasal Endoscopic Findings
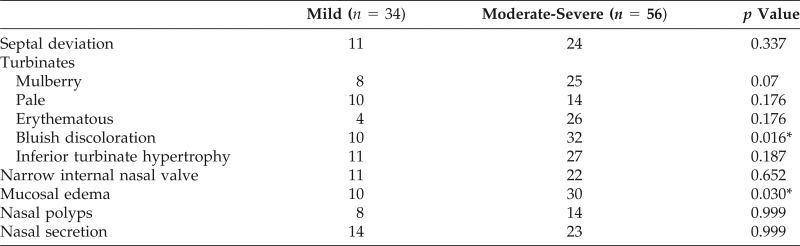
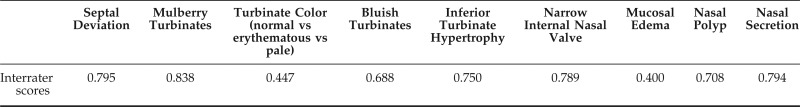
A comparison of nasal endoscopic findings between group 1 and 2 showed significant differences in mucosal edema and bluish discoloration (p < 0.05). The other parameters that did not show significant differences were nasal septum deviation, erythematous or pale nasal mucosa, inferior turbinate hypertrophy, narrow internal nasal valve, mucosal erythema, nasal polyps, and the presence of nasal secretions (Table 2). According to the κ interpretation table, the interrater agreement was fair regarding mucosal edema and moderate regarding turbinate color changes. The agreement was almost perfect regarding the mulberry aspect of the turbinates and substantial regarding inferior turbinate hypertrophy, bluish discoloration of turbinates, and septal deviation. The agreement was also substantial as far as abnormal internal nasal valve, nasal polyps, and nasal secretions (Table 3).
Table 2.
Nasal endoscopic findings
*Indicates significant result.
Table 3.
Interrater κ scores
DISCUSSION
Allergic rhinitis is a chronic disorder, with an increase in its future estimated prevalence; this was attributed to many risk factors, among which are improved hygiene and increased allergen exposure.15 The use of nasal endoscopy as a tool for the assessment and evaluation of allergic rhinitis disease severity remains understudied, and only a few studies in the literature focused on this subject. Jareoncharsri et al.16 were one of the first groups to report the findings of the nasal endoscope in patients with allergic rhinitis; of 83 patients examined with allergic rhinitis, 95.2% were reported to have an abnormal endoscopic examination result. Signs, such as abnormal middle turbinate, narrow entrance into frontal recess, septal deviation, nasal discharge, the presence of polyps, and edematous mucosa were reported.16
Moreover, Eren et al.13 assessed the issue of the nasal endoscope in diagnosing allergic rhinitis in which three physicians evaluated 108 patients diagnosed with allergic rhinitis by rigid nasal endoscope. They assessed various factors, such as mucosal edema, turbinate hypertrophy, nasal polyps, and the presence of secretions. There was significant interrater agreement with regard to the presence of nasal polyps, mucosal edema, polypoid degeneration of the inferior turbinate tail, and septal deviation. However, there was a significant interrater variability with regard to turbinate hypertrophy and color, which led to the conclusion that endoscopic examination is not a reliable diagnostic tool for allergic rhinitis.13 Furthermore, Raza et al.17 also evaluated the role of the nasal endoscope alone in the diagnosis of allergic rhinitis. Three physicians performed nasal endoscopy on 16 patients diagnosed with allergic rhinitis before history taking. The results showed significant interrater variability, except for the finding of nasal polyps. It was concluded that the physical examination alone without a proper history was not sufficient for the diagnosis of allergic rhinitis.
Ameli et al.18 also assessed 176 children with symptoms of allergic rhinitis. They assessed the severity of nasal obstruction by investigating the narrowing of the nasal opening and airway. The factors that were studied were the middle and inferior turbinates and the contact point between them and the adjacent structures, as well as the color of the inferior turbinate. It was concluded that inferior and middle turbinate contacts were reliable predictive factors for allergic rhinitis, whereas pale turbinates did not predict the presence of allergic rhinitis.18 Also, Brook et al.14 conducted a retrospective case control study in which the purpose was to determine whether abnormalities of the nasopharynx, oropharynx, and larynx correlate with the atopic status to aid in diagnosis of allergic disease. There were significant differences for abnormalities in the torus tubarius and increased nasopharyngeal secretions between patients with atopy and those without atopy. However, no other significant differences were noted concerning other anatomic structures.14 In our study, the patients were diagnosed with allergic rhinitis and classified according to the severity of their disease based on the last ARIA guidelines.11 Nasal endoscopy was studied as a tool for assessing the severity of the disease as well as the rate of interrater agreement between physicians performing nasal endoscopy.
Two endoscopic findings were found to be significant as indicators of the severity of the disease; the bluish discoloration of the inferior turbinate and the presence of mucosal edema. The bluish discoloration of the inferior turbinate was found to be an easily detectable endoscopic finding that had good interrater agreement. Although it was poorly described in the literature as an important endoscopic criterion for the assessment of allergic rhinitis, it was found to be a statistically significant finding in this study. The bluish discoloration of the inferior turbinate in allergic rhinitis is caused by mucosal edema as well as venous congestion in response to inflammatory mediators, e.g., histamine.19 All previously cited articles in which the investigators looked at reliable endoscopic signs for diagnosing and assessing the severity of allergic rhinitis did not specifically looked at mucosal bluish discoloration.13,14,16–18 The change in color of the turbinates was more defined as paleness of the nasal mucosa. Although a pale nasal mucosa should be ruled out during any nasal endoscopic examination, the bluish discoloration of the turbinate should definitely be among the physician's endoscopic checklist, especially if the patient has an inflammatory condition, e.g., allergy. The presence of mucosal edema as a significant endoscopic finding is consistent with the results of Jareoncharsri et al.16 but was subject to interrater variability, which contradicted the results portrayed by Eren et al.,13 The absence of interrater agreement was mainly related to the absence of specific criteria that defined the presence or absence of mucosal edema.
The distinction between normal versus pale nasal mucosa on one hand and normal versus erythematous mucosa on the other hand was also subject to interrater variability. Although this study showed that turbinate color was not a significant endoscopic variable for assessing the severity of allergic rhinitis, the absence of interrater agreement needs to be addressed to improve the accuracy of nasal endoscopic examination reports. The lack of interrater agreement, despite the use of the same light source and monitor, is mostly related to the absence of specific cutoff points between normal, pale, and erythematous mucosal color. Other nasal endoscopic findings did not reach statistical significance in the assessment of disease severity. The presence of nasal polyps, in contrast to the results of Jareoncharsri et al.16 was not found to be a reliable finding. The presence of the mulberry aspect of the inferior turbinates also failed to reach statistical significance; this conclusion was the same made by Brook et al.14
CONCLUSION
The presence of mucosal edema and bluish discoloration of the inferior turbinate on nasal endoscopy in patients with allergic rhinitis can be used as criteria for assessing the severity of the disease. Other findings on nasal endoscopy did not show any significance. Well-defined criteria for the description of nasal mucosal edema and color are needed to reduce interrater variability among physicians.
Footnotes
No external funding sources reported
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Rosati MG, Peters AT. Relationships among allergic rhinitis, asthma, and chronic rhinosinusitis. Am J Rhinol Allergy 30:44–47, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bousquet J, Khaltaev N, Cruz AA, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy 63:(suppl. 86):8–160, 2008. [DOI] [PubMed] [Google Scholar]
- 3. Mosges R, Klimek L. Today's allergic rhinitis patients are different: New factors that may play a role. Allergy 62:969–975, 2007. [DOI] [PubMed] [Google Scholar]
- 4. Ozdoganoglu T, Songu M, Inancli HM. Quality of life in allergic rhinitis. Ther Adv Respir Dis 6:25–39, 2012. [DOI] [PubMed] [Google Scholar]
- 5. Keil T, Bockelbrink A, Reich A, et al. The natural history of allergic rhinitis in childhood. Pediatr Allergy Immunol 21:962–969, 2010. [DOI] [PubMed] [Google Scholar]
- 6. Nathan RA. The burden of allergic rhinitis. Allergy Asthma Proc 28:3–9, 2007. [DOI] [PubMed] [Google Scholar]
- 7. Khan DA. Allergic rhinitis and asthma: Epidemiology and common pathophysiology. Allergy Asthma Proc 35:357–361, 2014. [DOI] [PubMed] [Google Scholar]
- 8. Canonica GW, Bousquet J, Mullol J, et al. A survey of the burden of allergic rhinitis in Europe. Allergy 62(suppl. 85):17–25, 2007. [DOI] [PubMed] [Google Scholar]
- 9. Salib RJ, Drake-Lee A, Howarth PH. Allergic rhinitis: Past, present and the future. Clin Otolaryngol Allied Sci 28:291–303, 2003. [DOI] [PubMed] [Google Scholar]
- 10. Ichimura K. Mechanism of nasal obstruction in patients with allergic rhinitis. Clin Exp Allergy Rev 10:20–27, 2010. [Google Scholar]
- 11. Brozek JL, Bousquet J, Baena-Cagnani CE. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol 126:466–476, 2010. [DOI] [PubMed] [Google Scholar]
- 12. Seidman MD, Gurgel RK, Lin SY, et al. Clinical practice guideline: Allergic rhinitis executive summary. Otolaryngol Head Neck Surg 152:197–206, 2015. [DOI] [PubMed] [Google Scholar]
- 13. Eren E, Aktaş A, Arslanoğlu S. Diagnosis of allergic rhinitis: Inter-rater reliability and predictive value of nasal endoscopic examination: A prospective observational study. Clin Otolaryngol 38:481–488, 2013. [DOI] [PubMed] [Google Scholar]
- 14. Brook C, Noordzij JP, Russel K, et al. Predictive findings of allergic disease in fiberoptic nasolaryngoscopy. Laryngoscope 125:286–290, 2015. [DOI] [PubMed] [Google Scholar]
- 15. Steinsvaag SK. Allergic rhinitis: An updated overview. Curr Allergy Asthma Rep 12:99–103, 2012. [DOI] [PubMed] [Google Scholar]
- 16. Jareoncharsri P, Thitadilok V, Bunnag C, et al. Nasal endoscopic findings in patients with perennial allergic rhinitis. Asian Pac J Allergy Immunol 17:261–267, 1999. [PubMed] [Google Scholar]
- 17. Raza SN, Yousuf K, Small P, Frenkiel S. Diagnosing allergic rhinitis: Effectiveness of the physical examination in comparison to conventional skin testing. J Otolaryngol Head Neck Surg 40:407–412, 2011. [PubMed] [Google Scholar]
- 18. Ameli F, Brocchetti F, Tosca MA. Nasal endoscopy in children with suspected allergic rhinitis. Laryngoscope 121:2055–2059, 2011. [DOI] [PubMed] [Google Scholar]
- 19. Naclerio R, Solomon W. Rhinitis and inhalant allergens. JAMA 278:1842–1848, 1997. [PubMed] [Google Scholar]