Abstract
Background:
Concha bullosa mucocele is a rare diagnosis that presents as a nasal mass. It impinges on surrounding structures and can easily be mistaken for a neoplasm.
Objective:
The objective of this study was to shed light on this rare entity and report its diagnostic features and treatment outcomes.
Methods:
A case series conducted in a tertiary health care center. Demographic data, clinical presentation, imaging, cultures, and treatments were recorded. Operative video illustration and key images were obtained. A review of the literature was also performed.
Results:
A total of five cases were reviewed, four of which were concha bullosa mucoceles and one was a mucopyocele. Three of the patients had some form of previous nasal trauma. Headache and nasal obstruction were the most common symptoms with a nasal mass finding on physical examination. Computed tomography was used in all the patients, and magnetic resonance imaging was used in four of the five patients. Four patients had coexistent chronic rhinosinusitis, and three had positive bacterial cultures. All these patients were treated endoscopically either with middle turbinate marsupialization or subtotal resection. No recurrence has been noted thus far.
Conclusion:
Concha bullosa mucocele is a rare diagnosis. Imaging characteristics are helpful in considering the diagnosis, although surgical intervention is often necessary to confirm the diagnosis and treat concha bullosa mucocele.
Keywords: Concha bullosa, middle turbinate, mucocele, mucopyocele, nasal mass, nasal obstruction, headache, endoscopic sinus surgery.
The middle turbinate can be pneumatized in 14–53% of the population.1–4 This air-filled cavity, known as a conchae bullosa is usually asymptomatic; however, it may develop into a mucocele or a mucopyocele if infected.1,3,5–7 Either of these entities can lead to sinonasal symptoms, such as headache, nasal congestion, rhinorrhea, anosmia, and snoring.7,8 In addition, results of a physical examination of patients with a concha bullosa mucocele (CBM) or mucopyocele often demonstrate an intranasal mass and septal deviation. Computed tomography (CT) findings may further demonstrate bone remodeling and extranasal involvement, which, when taken together with the clinical examination, may steer the physician to suspect a diagnosis of malignancy.1 This misidentified mass leads to further diagnostic investigations and invasive treatments as well as increased anxiety for patients and their families.7,9,10 Unfortunately, these consequences are difficult to avoid because there are still no clear guidelines available for this rare pathology.
There are no known predominant risk factors for CBMs, although certain studies indicate that nasal trauma, previous surgery, polyps, or infection are predisposing factors.5,9,11–13 There are 22 reported cases in the literature, of which 15 are mucopyoceles and 7 are CBMs. A CT was used in 21 cases, whereas magnetic resonance imaging (MRI) use was scarce. In this case series, we reported on five patients who presented with nasal masses confirmed to be CBMs or mucopyoceles. The objective of this study was to describe various case examples of this rare diagnosis and to report their outcomes.
METHODS
Ethics approval was obtained from McGill University Health Center Research Ethics Board. A case series of five patients who underwent surgery for CBM between April 2011 and August 2015 at McGill University Health Center sites was conducted. Demographic data, clinical presentation, imaging, cultures, and treatments were recorded. Operative video illustration and key images were obtained. A review of the literature was also performed.
RESULTS
Cases
Patient 1.
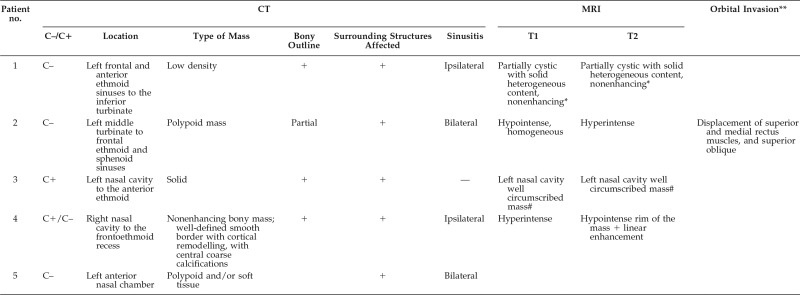
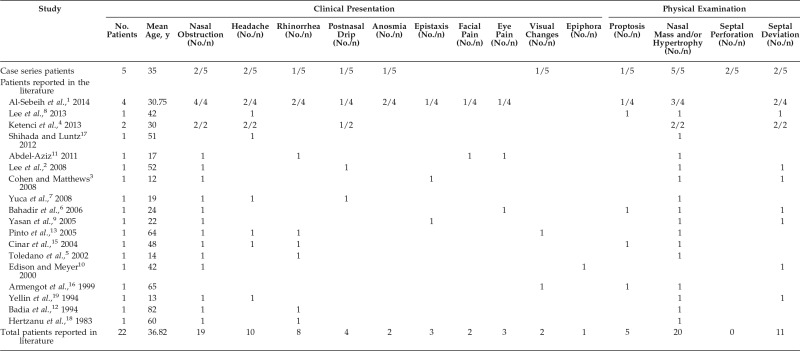
A 17-year-old man presented with a 3-week history of headache, decreased concentration, and fatigue. Results of the physical examination demonstrated a large mucosa-lined middle turbinate mass. Sinus CT (Fig. 1) and MRI findings are presented in Table 1. No organisms were isolated on middle turbinate aspirate cultures. The patient underwent endoscopic sinus surgery (ESS) for mucocele drainage. Final pathology results confirmed the presence of mucus and of Charcot-Leyden crystals, which indicate the presence of eosinophilic mucin. The patient recovered well after surgery but did experience one episode of vestibulitis, which was treated.
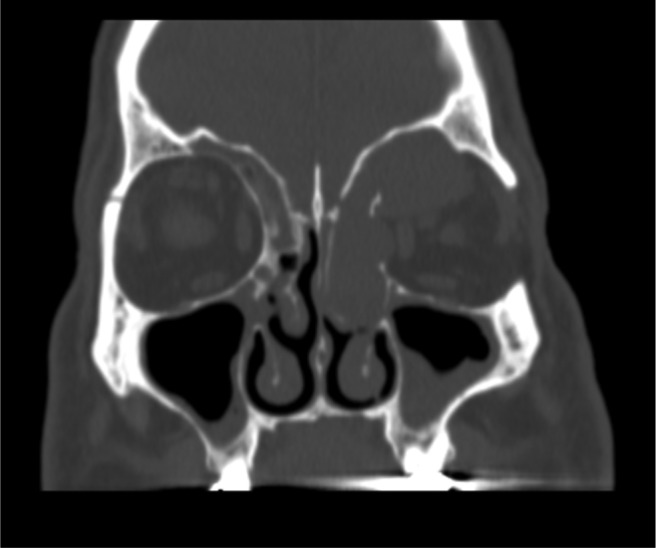
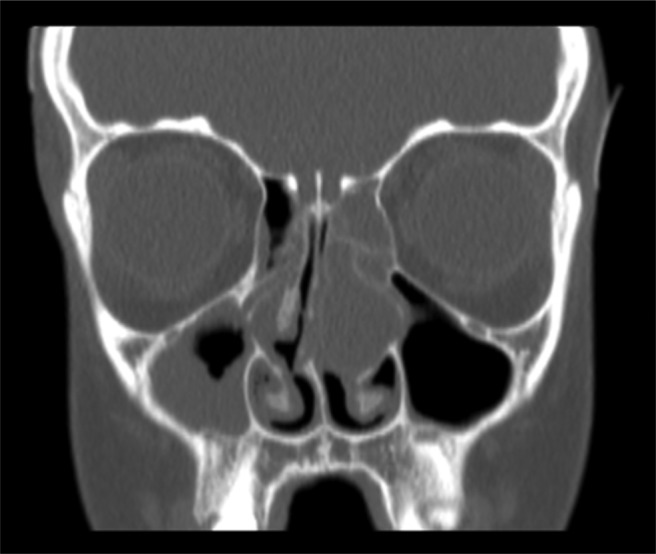
Figure 1.
Computed tomography (C–) of patient 1. (A) Coronal. A 4.2 × 3.5 × 2.2-cm nasal mass extends from the left frontal sinus through the anterior ethmoid until the inferior turbinate; the left frontal sinusitis is also seen. (B) Axial. Mass that fully occupies the nasal cavity, causing right septal deviation.
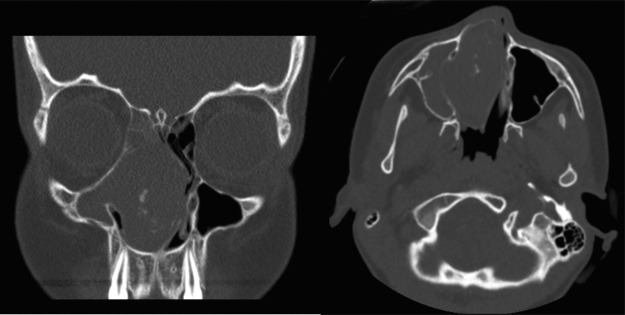
Table 1.
Sinus CT and MRI findings of the five patients in our case series
CT = Computed tomography; MRI = magnetic resonance imaging; C– = without contrast; C+ = with contrast; + = presence of described finding.
*T1- and T2-weighted imaging was not described.
#MRI of the brain. **Seen on CT and/or MRI.
Patient 2.
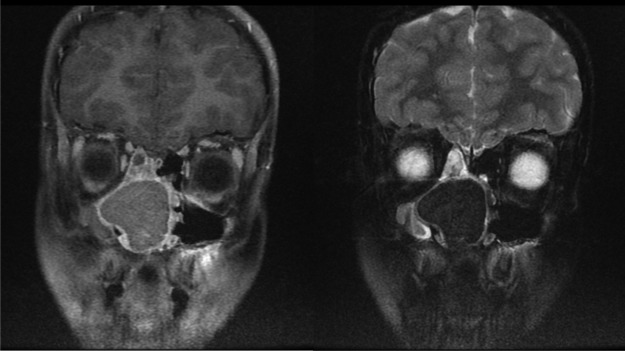
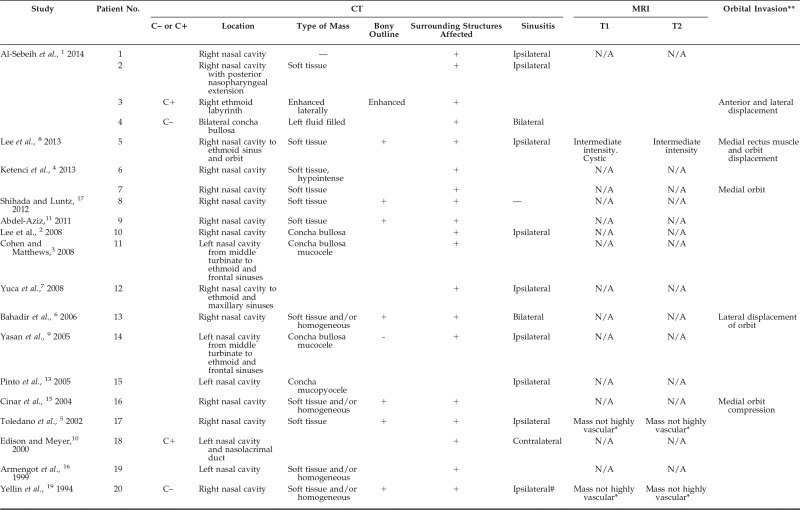
A 50-year-old man with a history of anosmia and chronic rhinosinusitis with nasal polyposis who had a frontal ESS and polypectomy 12 years earlier presented with left-sided frontal headache and visual changes. A trial of antibiotics and prednisone resulted in minor symptom improvement, with some worsening of his vision. Septal perforation and left exophthalmos were noted on a physical examination. A CT of the sinus revealed a large nasal mass with a thin bony outline laterally, which extended into the sphenoid recess and left orbit (Fig. 2, Table 1). Imaging reports indicated either a frontoethmoidal sinus mucocele or a slow-growing neoplasm. Bilateral maxillary, sphenoid, and frontal sinusitis as well as right ethmoidal sinusitis were also seen. Similarly, MRI demonstrated a 4.6 × 2.3 × 3.7-cm mass (Fig. 3, Table 1). Middle meatus cultures revealed normal flora. This patient underwent surgical drainage of the mucocele and ESS. A mucocele diagnosis was confirmed during surgery, given its extension into the middle turbinate, which resulted in secondary obstruction of the ipsilateral maxillary and sphenoid sinuses, and was addressed during the surgery. Three years after the surgery, he returned with anosmia, congestion, and frontal pressure secondary to an upper respiratory tract infection. Results of an examination demonstrated patent sinuses and small persisting septal perforation.
Figure 2.
A computed tomography of patient 2. Large left polypoid mass eroding the medial and superior wall of the left orbit, touching the globe and extending into the sphenoid recess. Bilateral frontal, maxillary, and sphenoidal sinusitis, and right ethmoidal sinusitis are seen. The right middle turbinate is what is left from a previous partial turbinectomy.
Figure 3.
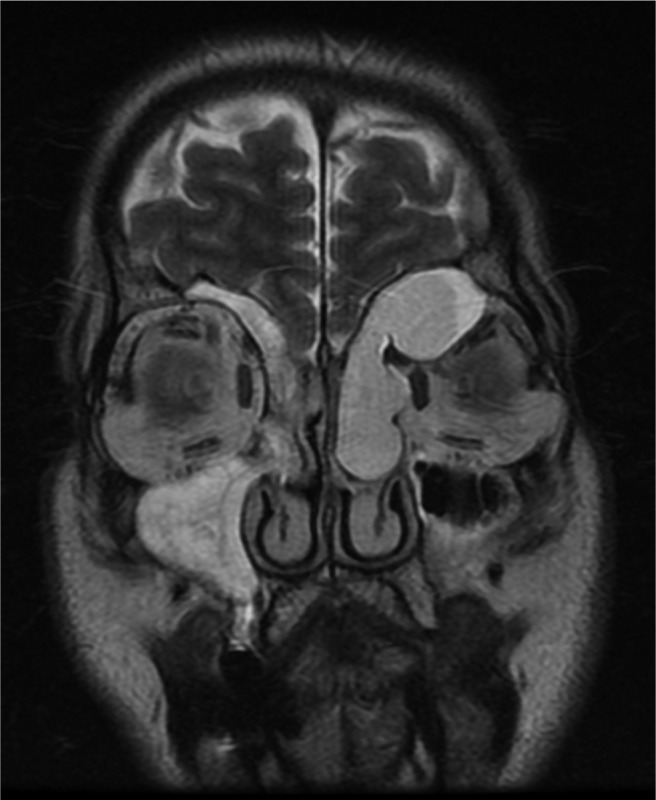
Patient 2. Magnetic resonance image, showing a 4.6 × 2.3 × 3.7-cm expansile lesion in the left frontal sinus, with well-defined lobulated contours and homogeneous T1 hypointensity and T2 hyperintensity, extending into the sphenoid and ethmoid sinuses, displacing the superior rectus, medial rectus, and superior oblique muscle, which allowed protrusion into the left orbit. Mucosal thickening was seen in all paranasal cavities, particularly in the right ethmoid and maxillary sinuses. The intracranial cavity seems unaffected.
Patient 3.
An 86-year-old man with a history of nasal bone fracture, gastroesophageal reflux disease, and diabetes mellitus presented with a left nasal mass incidentally found on an MRI of the brain (Fig. 4, Table 1). He reported rhinorrhea, and results of a physical examination revealed septal perforation and a large mass emerging from the left middle turbinate region. A CT showed a solid, well-circumscribed lesion (2.6 × 2.5 × 1.7 cm) that seemed to erode the middle turbinate, obliterate the left middle meatus, extend into the ethmoid air cells, and erode the left lamina papyracea (Fig. 5, Table 1). Although, generally, one would suspect malignancy to be more heterogeneous with less well-defined borders, in this case, radiologists suspected a neoplasm, including adenocarcinoma or squamous cell carcinoma. Middle turbinate cultures showed Escherichia coli and mixed skin flora with white blood cells. With the patient under local anesthesia, the mass was surgically drained and the anterior ethmoid chamber was opened, which revealed a thick yellow-green mucus discharge. The final diagnosis was a mucopyocele of an underlying concha bullosa.
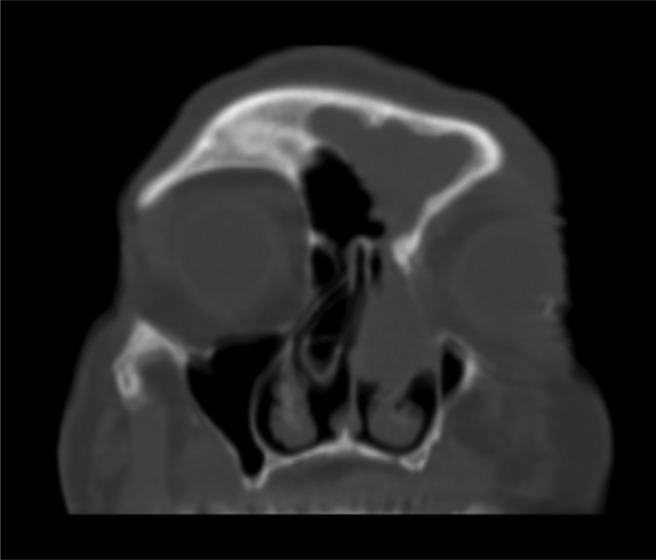
Figure 4.
Patient 3. Brain magnetic resonance imaging T2 image depicts the 2.4 × 2.5-cm left nasal mass, associated to inflammatory changes in the frontal sinus.
Figure 5.
Patient 3. Computed tomography C+ depicts a 2.6 × 2.5 × 1.7-cm solid left nasal mass obliterating the middle meatus, destroying the middle turbinate, and invading the anterior ethmoid air cells. There is erosion of the left lamina papyracea, but no orbital invasion is seen.
Patient 4.
A 10-year-old girl with a history of right nasal foreign body removed at the age of 3 years, presented with a prominent nasal deformity and right-sided nasal swelling and obstruction. Results of a physical examination revealed laterally displaced nasal bones, left septal deviation, and a nasal mass filling the entire right nasal cavity. A CT confirmed a bony mass in the right nasal cavity that was causing significant mass effect toward the left and obliteration of the frontal, ethmoid, and maxillary sinuses (Fig. 6, Table 1). An MRI confirmed the massive nasal mass (5.4 × 6.1 × 3.6 cm), which led to a differential diagnosis of CBM, fungus ball, or Wegener granulomatosis (Fig. 7, Table 1). Middle turbinate cultures isolated Staphylococcus aureus and Haemophilus influenzae organisms. Patient 4 underwent ESS for excision of the mucocele, wide maxillary antrostomy, ethmoidectomy, sphenoidectomy, and opening of frontal recess. The final pathology results supported a mucocele diagnosis, described as inflammation of a cystic lesion lined by nasal ciliated epithelium. Immediately and 10 days after surgery, the patient was asymptomatic and healing well.
Figure 6.
(A) Coronal view. (B) Axial view of a computed tomography of the sinus in patient 4, which depicts a massive 5.2 × 5.5 × 3.5-cm well-defined bony mass with cortical remodeling, extending to the frontoethmoidal regions. A severe mass effect is seen: there is lateral bowing of the right maxillary sinus, left septal deviation, and elevation of the right fovea ethmoidalis. There was no significant enhancement with contrast. All right-sided sinuses were opacified.
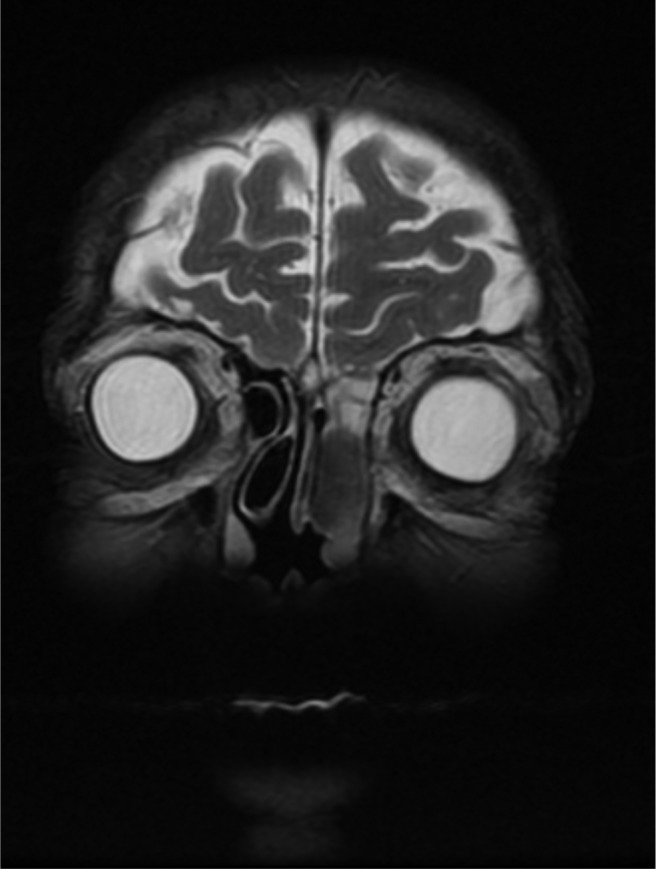
Figure 7.
Patient 4. Magnetic resonance image, (A) T1, (B) T2, showing a large expansile lesion in the right nasal cavity (5.4 × 6.1 × 3.6 cm) extending into the frontoethmoid recess, remodeling of the medial wall of the right maxillary sinus with lateral bowing, and severe nasal septum deviation. There was a T1 hyperintensity and T2 hypointense signal intensity without enhancement and a rim of high T2 signal associated with linear enhancement. Right frontal, ethmoid, and maxillary sinuses are opacified, the right maxillary with inspissated secretions.
Patient 5.
A 12-year-old boy with known adenoid hypertrophy and seasonal allergies presented with bilateral nasal obstruction and dry cough. Results of a physical examination demonstrated a middle meatal mass, right septal deviation, and hypertrophied adenoids. A CT of the sinus showed a bilaterally occluded airway, with a 2.8 × 1.5 × 1.6-cm mass substituting the left middle turbinate and causing remodeling of the medial wall of the left maxillary sinus and septal deviation to the right with impaction on the contralateral middle turbinate (Fig. 8, Table 1). Chronic pansinusitis and left otomastoiditis were also seen. White blood cells, S. aureus, and Corynebacterium were isolated on middle turbinate cultures. During ESS, incision into the mass determined it to be a concha bullosa filled with inspissated mucus, which did not seem to be infected. The CBM was marsupialized, and bilateral maxillary antrostomy, uncinectomy, ethmoidectomies, and sphenoidectomies as well as septoplasty and adenoidectomy were performed.
Figure 8.
Computed tomography of the sinus of patient 5, showing a 2.8 × 1.5 × 1.6-cm left polypoid lesion replacing the left middle turbinate and indicating nasal obstruction. The septum is deviated to the right.
Literature Comparison
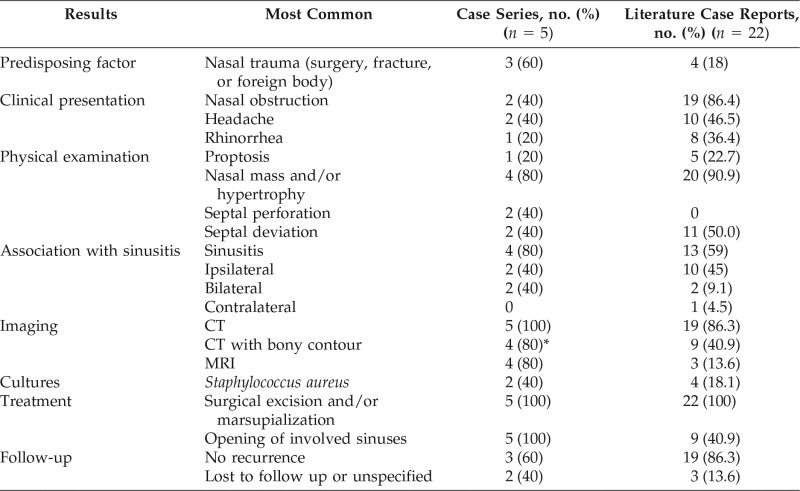
Findings from the five patients in our case series compared with the 22 cases reported in the literature are presented in Table 2.
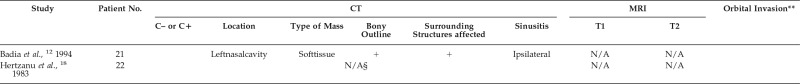
Table 2.
Findings from the five patients in this case series compared with literature case reports
CT = Computed tomography; MRI = magnetic resonance imaging.
*One of the four patients had a mass with partial bony contour seen on CT.
DISCUSSION
Fourteen to 15% of the population have a pneumatized middle turbinate, commonly referred to as a concha bullosa.1–6 Rarely, these can develop into a mucocele when filled with fluid or a mucopyocele when infected. With enlargement, they can cause significant nasal obstruction and orbital complications. Moreover, middle turbinate mucoceles can be mistaken for neoplasms. To date, little is known about the pathogenesis of middle turbinate CBM. It is believed that they form due to chronic blockage of the concha bullosa ostium, which prevents appropriate airflow between the pneumatized cavity and its originating compartment, usually, the anterior ethmoid, frontal recess, or middle meatus.2,6,9 Such an obstructive mechanism could explain why the epithelial contour remains intact in mucoceles of sinonasal compartments.12,13 This is in contrast to the conventional mucocele definition that refers to a trauma-induced, fluid-filled cavity that lacks an epithelial surrounding.12,13 However, for CBMs, a cause-effect mechanism is not yet clear. Previous studies indicate either a mechanical (history of trauma, surgery, nasal polyposis, or benign tumors) or an inflammatory etiology (infection, allergy, cystic fibrosis),5,8,12,14 whereas others did not support the obstructive causes of mucoceles.14
Four of the five patients presented in this case series (80%), had possible predisposing factors: patients 2, 3, 4, and 5 had a history of polyps and/or ESS, previous nasal fracture, foreign body in the ipsilateral nostril, and allergies, respectively. This is a higher proportion than reports in the literature, of only 27% (6/22) with possible risk factors: two patients with a history of nasal trauma5,11; one patient with a history of upper respiratory tract infection9; one with chronic rhinosinusitis13; one with previous polypectomy12; and one with nasal polyps, previous ESS, and known chronic rhinosinusitis combined.8 Thus, we found no pathognomonic predisposing history within our patient population or in the literature. However, the most common history was nasal trauma (e.g., nasal fracture, surgical intervention, foreign body): 60% of the patients in our case series had some form of previous nasal trauma (patients 2, 3, and 4), compared with 4 of 22 (18%) in the literature.
It has previously been suggested that nasal polyposis could cause mechanical obstruction of mucus flow and inflammatory changes that increase the risk of mucocele formation in paranasal sinuses. Patients with nasal polyposis who had previous surgical interventions had an increased risk compared with those without surgery.14 Although this hypothesis is specific to paranasal sinus mucoceles, the pathogenesis could be a plausible explanation for CBMs as well, such as in patient 2. In addition, one case report mentioned diabetes mellitus as a risk factor specific to concha bullosa mucopyoceles.15 In support of this statement, it is interesting to note that patient 3, the only patient in our case series who presented with a mucopyocele had diabetes mellitus. Clinical symptom evaluation did not reveal any predominant symptom indicative of a CBM (Table 3). The most common clinical symptoms experienced by the five patients in this series included nasal obstruction and headache. This slightly contrasts the literature that demonstrated the most common symptoms to be nasal obstruction (86%), followed by headaches (45%), and rhinorrhea (36%) (Table 3). It is important to note that patient 3 presented after an incidental scan that found his nasal mass and exhibited associated rhinorrhea only.
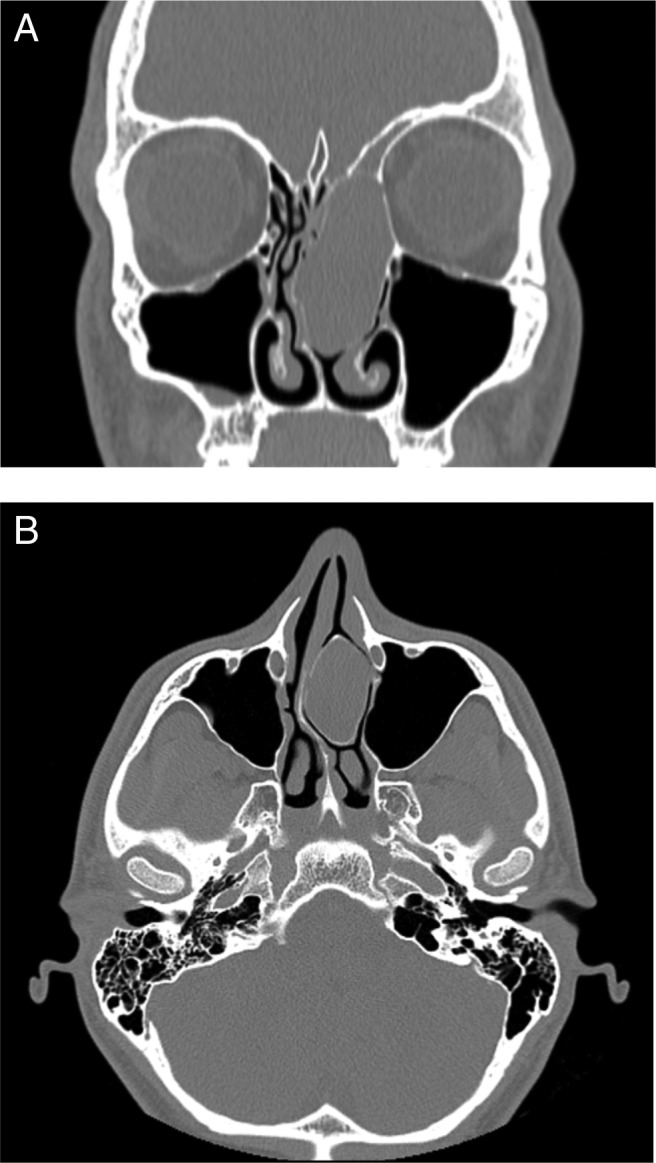
Table 3.
Signs and symptoms of the five patients at our institution with concha bullosa mucoceles or mucopyoceles and the 22 reported cases of concha bullosa mucoceles or mucopyoceles reported in the literature*
Blank cells indicate absent or no mention of symptoms in patient charts or case reports.
Results of the patients' physical examination were noteworthy, with the preponderance of patients (80%) presenting with a nasal mass or middle turbinate hypertrophy (Table 3). Nasal septum involvement (deviation or perforation) was also common (80%) (Table 2). These findings remained fairly consistent with the cases reported in the literature, in which, on examination, 20 of 22 (90%) had objectified a nasal mass or middle turbinate hypertrophy and 11 of 22 (50%) had septal deviation (Table 3). These findings can be explained by the gradual mass effect caused by the expansive nature of the CBM, which allowed an intact mucosa to remain.9,16 This could explain why many masses were described as mucosa-lined or simply hypertrophied middle turbinates and as having respiratory mucosa on final pathology. In addition, CBMs have more surrounding space than do mucoceles of frontal or ethmoid sinuses, which allows them to expand to large sizes before being detected.12 This could also explain the lack of prevalent symptoms on presentation and the large size of nasal masses in our patients.
CT remains the preferred imaging technique because it is ideal for visualizing bony structures; provides detailed information about the middle turbinate, nasal, and paranasal structures; and can differentiate between a CBM and a pneumatized middle turbinate.1,7,11,17 However, mucoceles and mucopyoceles cannot be differentiated on CT.18 The anticipated finding of a CBM on CT consists of a soft-tissue mass with a bony contour, which usually causes deviation or compression of surrounding structures.6 There also can be enhancement on the periphery of the mass.1 The bony rim is considered the main finding on CT that enables identification of a CBM compared with other masses, and its absence can lead to frequent misdiagnoses, including that of neoplasm.9,15 In this case series, CT readings for one of the five patients had no reports of characteristic bony surrounding on imaging, and one patient had a partial bony contour visualized laterally (patient 2) (Table 1). The absence or inconsistent presence of bony shell could be explained by an underlying mechanism of bone remodeling.9,16 Given these findings, it is important to consider CBM in one's differential diagnosis of a nasal mass despite the loss of the bony rim feature on imaging. It is interesting to note that patients 1, 2, 3 and 4 displayed nasal masses that extended from the nasal fossa to the frontal and/or ethmoid sinuses (Figs. 1, 2, 5, 7). Whether their origin began in the sinuses or in the concha bullosa is difficult to determine. However, because frontal and ethmoid sinus mucoceles are much more frequent than CBMs,4–6 it is possible that these could be overdiagnosed, whereas CBMs are less frequently considered in the differential diagnosis.
At our institution, CTs and MRIs are both used in conjunction to aid in obtaining a diagnosis. All five patients in our study had CTs, whereas 4 of 5 (80%) also had MRIs. This somewhat contradicts the prevalence of MRIs reported in the literature of CBM: only 13.6% had MRIs, whereas 86.3% of patients had CTs (Tables 2 and 4). Despite the low number of MRIs, several case studies mention the importance and usefulness of MRI in the investigation of these nasal masses due to the ability of MRI to depict extranasal involvement, such as orbital and intracranial extension.1,4,6,17 MRI also evaluates the vascularity of a mass and delineates secretions.6 A CBM is usually avascular5,6,19 and, in contrast to tumors, is nonenhancing with gadolinium. Therefore, in addition to CT, we recommend MRI in the investigation of all patients with nasal masses because it enables better identification of benign CBMs from nasal tumors; an important distinction to make.
Table 4.
CT and MRI findings of the 22 patients reported in the literature
CT = Computed tomography; MRI = magnetic resonance imaging; + = presence of described finding; C+ = with contrast; C– = without contrast; N/A = not available.
*T1- and T2-weighted imaging were not described.
#Seen on MRI.
§Radiograph was done, which showed left nasal mass and clouding of left ethmoid and frontal sinuses. **seen on CT and/or MRI.
There is also no consensus on the relationship between concha bullosa and sinus pathology.1 Yasan et al.,9 Lee et al.,2 and Armengot et al.16 describe CBM as the cause of ipsilateral sinusitis in their case studies. They hypothesize that the concha bullosa mechanically disrupts normal sinus ventilation and drainage. However, other studies refute this association.4 Nevertheless, 59% of cases in the literature (13/22) describe sinus involvement (Tables 2 and 4). Ten of these cases were of involvement that was ipsilateral to the conchal mass, which indicates a relationship between CBM and sinusitis. However, because some case reports did not discuss sinuses at all, this proportion and the suggested association are questionable. In the current case series, 80% of the patients presented with associated sinusitis seen on imaging, of which two were ipsilateral and two were bilateral (Tables 1 and 2). In addition, when an ethmoid mass and the middle turbinate are not seen as separate entities on CT or MRI, as is the case in four of our five patients (Figs. 1–7, Table 1), one should be more alert to the possibility of a CBM.
Microbiology results of cultures of the middle turbinate were available for all our patients. Two did not grow any microorganisms (in patients 1 and 2), and three did have bacteria isolated (patients 3, 4, and 5). S. aureus was the most common organism seen in our case series (2/5) as well as in the literature (4/22 [18.1%]).3,10,15,19 There are no reports of Corynebacterium species, E. coli, or H. influenza in the literature. With no fungi isolated in our series, and, to our knowledge, only one case in the literature, it can be suggested that there is probably no association between fungal infection and CBM. ESS is the favored treatment of mucoceles.7 Four techniques have been mentioned in the literature: transverse excision, crushing, and lateral or medial marsupialization.1,8 Lateral marsupialization is the preferred method at our institution, and opening of all sinuses obstructed by the CBM is an important part of what we consider to provide the highest rate of success for these surgeries. In addition, no change in surgical procedure is necessary for patients with orbital involvement because decompression and resolution of orbital symptoms occur almost immediately after surgery, as is seen in all the patients with orbital involvement: patient 2 and five patients reported in the literature.1,4,6,8,15 Of our five patients, two (patients 3 and 5) were lost to follow up, and none of the others had known recurrence of the mass. The mucocele recurrence rate reported in the literature is as low as 0% after ESS,20 and, despite our small patient population, our case series indicated that this could also be applied to CBMs.
CONCLUSION
Although a rare entity, it is important to consider CBM in the differential diagnosis of nasal masses. This case series of patients found to have CBM or mucopyocele depicts key elements in their presentation as well as imaging findings. The presence of a nasal mass, nasal septal involvement, and sinusitis were objectified on physical examination and imaging of most patients. In addition, CT and MRI are both helpful in reaching this diagnosis. Treatment of CBM remains surgical, and ESS with lateral marsupialization and opening of all involved sinuses is preferred.
Footnotes
No external funding sources reported
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Al-Sebeih KH, Bu-Abbas MH. Concha bullosa mucocele and mucopyocele: A series of 4 cases. Ear Nose Throat J 93:28–31, 2014. [PubMed] [Google Scholar]
- 2. Lee JS, Ko IJ, Kang HD, Lee HS. Massive concha bullosa with secondary maxillary sinusitis. Clin Exp Otorhinolaryngol 1:221–223, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cohen SD, Matthews BL. Large concha bullosa mucopyocele replacing the anterior ethmoid sinuses and contiguous with the frontal sinus. Ann Otol Rhinol Laryngol 117:15–17, 2008. [DOI] [PubMed] [Google Scholar]
- 4. Ketenci I, Sahin MI, Vural A, Ünlü Y. Mucopyocele of the concha bullosa: A report of two cases. Erciyes Tıp Dergisi/Erciyes Med J 35:157–160, 2013. [Google Scholar]
- 5. Toledano A, Herraiz C, Mate A, et al. Mucocele of the middle turbinate: A case report. Otolaryngol Head Neck Surg 126:442–444, 2002. [DOI] [PubMed] [Google Scholar]
- 6. Bahadir O, Imamoglu M, Bektas D. Massive concha bullosa pyocele with orbital extension. Auris Nasus Larynx 33:195–198, 2006. [DOI] [PubMed] [Google Scholar]
- 7. Yuca K, Kiris M, Kiroglu AF, et al. A case of concha pyocele (concha bullosa mucocele) mimicking intranasal mass. B-ENT 4:25–27, 2008. [PubMed] [Google Scholar]
- 8. Lee JH, Hong SL, Roh HJ, Cho KS, et al. Concha bullosa mucocele with orbital invasion and secondary frontal sinusitis: A case report. BMC Res Notes 6:501, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yasan H, Dogru H, Tuz M, et al. Polypoid degeneration of the middle turbinate mucocele mimicking intranasal neoplasia. J Otolaryngol 34:207–209, 2005. [DOI] [PubMed] [Google Scholar]
- 10. Edison BJ, Meyer DR. Nasolacrimal duct obstruction and dacryocystocele associated with a concha bullosa mucocele. Ophthalmology 107:1393–1396, 2000. [DOI] [PubMed] [Google Scholar]
- 11. Abdel-Aziz M. Mucopyocele of the concha bullosa presenting as a large nasal mass. J Craniofac Surg 22:1141–1142, 2011. [DOI] [PubMed] [Google Scholar]
- 12. Badia L, Parikh A, Brookes GB, Pyocele of the middle turbinate. J Laryngol Otol 108:783–784, 1994. [DOI] [PubMed] [Google Scholar]
- 13. Pinto JA, Cintra PP, de Marqui AC, et al. Mucopyocele of the middle turbinate: A case report. Braz J Otorhinolaryngol 71:378–381, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chobillon MA, Jankowski R. Relationship between mucoceles, nasal polyposis and nasalisation. Rhinology 42:219–224, 2004. [PubMed] [Google Scholar]
- 15. Cinar U, Yigit O, Uslu B, Alkan S. Pyocele of the middle turbinate: A case report. Kulak Burun Bogaz Ihtis Derg 12:35–38, 2004. [PubMed] [Google Scholar]
- 16. Armengot M, Ruiz N, Carda C, et al. Concha bullosa mucocele with invasion of the orbit. Otolaryngol Head Neck Surg 121:650–652, 1999. [DOI] [PubMed] [Google Scholar]
- 17. Shihada R, Luntz M. A concha bullosa mucopyocele manifesting as migraine headaches: A case report and literature review. Ear Nose Throat J 91:E16–E18, 2012. [DOI] [PubMed] [Google Scholar]
- 18. Hertzanu Y, Mendelsohn DB, Scott N. Pyocele of the middle turbinate. A case report. S Afr Med J 63:337–338, 1983. [PubMed] [Google Scholar]
- 19. Yellin SA, Weiss MH, O'Malley B, Weingarten K. Massive concha bullosa masquerading as an intranasal tumor. Ann Otol Rhinol Laryngol 103(pt. 1):658–659, 1994. [DOI] [PubMed] [Google Scholar]
- 20. Mohammadi G, Sayyah Meli MR, Naderpour M. Endoscopic surgical treatment of paranasal sinus mucocele. Med J Malaysia 63:39–40, 2008. [PubMed] [Google Scholar]