Abstract
Background:
Disk herniation is the most common cause of radiating low back pain (LBP) in subjects under 60 years of age. The present study aims to compare the effect of dry needling (DN) and a standard conservative approach on the pain and function in subjects with discogenic radiating LBP.
Materials and Methods:
Fifty-eight subjects with discogenic radicular LBP were screened and randomized into control (Standard physical therapy, n = 29) and experimental group (Standard physical therapy and DN, n = 29). Radiating pain intensity and disability were measured using visual analog scale (VAS) and Oswestry Disability indices at baseline, at the end of treatment and 2 months after the last intervention session. The changes in pain intensity and disability were studied using a 3 × 2 repeated measures analysis of variance considering time as the within-subject factor and group as the between-subject.
Results:
Pain intensity and disability scores decreased significantly in both experimental and control groups (experimental group: VAS = 37.24, Oswestry Disability Index [ODI] =28.48, control group: VAS = 45.5, ODI = 32.96), following the intervention. The change continued during the follow-up period (P < 0.001 for all comparisons). Pain and disability improvement, however, were more significant in experimental group, both in post intervention (experimental group: VAS = 25.17, ODI = 22.17, control group: VAS = 42.4, ODI = 30.27) (P = 0.05 and P = 0.03, respectively) and follow-up measures (P = 0.006 and P = 0.002, respectively).
Conclusion:
Both intervention strategies seem to significantly improve pain and disability immediately following intervention, where the improvement continued during 2 months after the last active intervention. Therefore, supplementary DN application may enhance the effect of the standard intervention considerably.
Keywords: Discogenic, dry needling, low back pain
INTRODUCTION
Low back pain (LBP) is the most common and costly neuromusculoskeletal dysfunction in many countries.[1,2] It is most commonly categorized as specific and nonspecific ones. Nonspecific LBP refers to any type of back pain in the lumbar region that is not related to serious pathology and/or does not have a specific cause. The underlying cause of specific LBP is structural problems or obvious pathologic conditions such as disc herniation;[3] disk herniation is due for 1–3% of LBPs, and it is the most common cause of radiating LBP in subjects under 60 years of age.[4]
Radiating LBP is the pain radiating from the low back into the lower extremity and/or foot along the sensory distribution of the affected spinal nerve root. This pain may be due to compression of inflamed spinal nerves within the spinal canal[4] or release of biochemical mediators from the nucleus pulposis.[5]
Myofascial pain syndrome, characterized by the presence of myofascial trigger points (MTPs), may also lead to numbness and referred pain, which can mimic radicular pain.[6] An MTP is a hyperirritable spot within a taut band of skeletal muscle, which is painful on compression. Trigger points may produce referral pain, secondary hyperalgesia, motor dysfunction, and autonomic phenomena.[7]
More than two-thirds of patients with chronic LBP may suffer from MTPs.[8] Prolonged contractions of the paraspinal muscles, especially the multifidus, may result in radiculopathy with radicular pain due to narrowing of the disk space and intervertebral foramina.[9] There is no universal consensus regarding the optimal treatment of chronic MTPs.[10] Dry needling (DN) is a minimally invasive procedure during which a solid filament needle is inserted into an MTP.[11] As a management for myofascial pain,[12] DN is hypothesized to decrease pain and spontaneous muscle activity through various mechanisms. DN seems to be a highly effective strategy to alleviate MTPs' chronic pains.[13] However, because of invasive nature of DN, it raises the potential for procedural side effects. Common side effects are consisted bleeding, hematoma, and pain. Uncommon adverse effects included strong pain during needling, vegetative symptoms, nerve irritation, and injury. Rare and very rare adverse effects included infection and pneumothorax.[14] The above mentioned adverse effects may be avoided by clinicians who had better anatomical knowledge and critically concern hygiene.
The first study regarding the effect of DN on LBP was performed in 1980, where 56 male patients completed 8 weeks standard physical therapy and exercise without any progress (according to subjects' reports) before enrolling in a randomized control trial (RCT).[15] The patients were divided into two groups, including a group treated by standard physical therapy and a group treated by standard physical therapy plus DN. The improvement of experimental group was significantly better than control group in terms of pain intensity and functional disability. Although this approach was effective, MTPs do not always overlap with the muscle motor point; therefore, DN should not be restricted only to muscle motor points.[16] According to a Cochrane systematic review in 2005,[17] DN may be a useful adjunct to other therapeutic interventions in the management of chronic LBP; thus, several research studies have investigated the effect of DN on non-specific LBP.[15,18,19,20] However, the effect of DN in subjects with specific LBP has not been studied yet. The current study aims to compare the pain and function in subjects with discogenic radiating LBP following the standard conservative approach with or without DN. The main hypothesis was that supplementary DN may increase the effect of the standard conservative intervention in patients with discogenic LBP (DLBP).
MATERIALS AND METHODS
This study was a single-blinded (examiner) parallel RCT. The study was performed in a physical therapy clinic related to Isfahan University of Medical Sciences and approved by the Research Ethics Committee of Isfahan University of Medical Sciences (December 2013). All participants completed an informed consent form, after receiving information on DN treatment method and the research procedure. The recruitment commenced at January 2014 and followed up Until September 2014.
The target population includes the subjects with radiating DLBP. In accordance with the study by Edwards and Knowles,[21] the sample size was estimated 58 (n = 29 for each group) with α = 0.05, β = 0.08 and Δ =0.75 and φ = 1 using equation 1.
Seventy subjects were included to the study to save the power following unwanted attrition.
Participants were recruited from Orthopedic, Neurologic, and Neurosurgery Departments. All patients with discogenic radicular LBP were assessed at baseline for eligibility criteria by blinded registered physiotherapist that was blinded in terms of the study protocol and study groups. The inclusion criteria were age between 20 and 50 years and radiating pain into one or both legs.[22] Following participants were excluded from the study: The participants with any coagulation disorder, the participants receiving anticoagulant therapy for any reason due to a potentially increased risk of hematoma following needling, and the participants with any psychological disorder due to the potential unreliable pain reporting, the subjects suffering from needle phobia, any tumor or infection in the lumbar region, acute or chronic radiating LBP resulting from fracture or instability, and the patients with a contraindications to DN.[23]
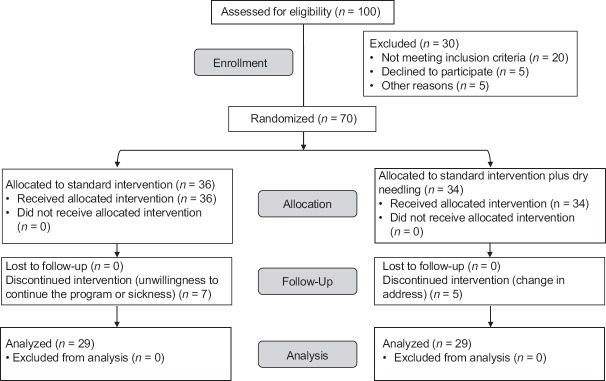
Using coin toss, the same equal number of participants were randomly assigned into control and intervention groups by a hospital staff that was blind to the study protocol. Control group received standard physical therapy, and experimental group received standard physical therapy plus DN. The subject’s attrition is presented in Figure 1.
Figure 1.
The CONSORT 2010 diagram for attrition of subjects in the study
Participants were assessed at baseline (during the first intervention session), in the last intervention session, and finally, 2 months after the last intervention session by a blinded physiotherapist. The primary outcome measure, pain intensity, was rated between 0 (no pain) to 10 (maximum pain) on visual analog scale (VAS) which is a reliable and valid measure to evaluate pain intensity in LBP subject.[24] Regarding the secondary outcome measure, disability, the Persian Version of the Oswestry Functional Disability Questionnaire (ODQ)[25] was used to measure the self-perceived level of functional disability resulted from discogenic radicular LBP. The Oswestry questionnaire included 10 items to assess how LBP affects the subjects' ability to manage their daily activity. The ODQ was scored from 1 to 5. The scores of all items were added up to obtain a possible score of 50, which was then doubled and expressed as a percentage. If an item was not answered, it was excluded from the total potential score and the total percentage was calculated according to the remaining items.
An independent and blinded physiotherapist performed the standard physical therapy. Another blinded physiotherapist with qualifications in DN performed DN. The physiotherapist has received a certification on needling of trunk and lower extremity. Patients in both groups received standard physical therapy for 10 sessions every other day, including application of a thermal modality, transcutaneous electrical nerve stimulator (Acupuncture like: Frequency = 1–4 Hz, Duration = 250 ms, Time = 20 min), ultrasound (Frequency = 1 MHz, pulsed, intensity = 1 w/cm2, Time = 1 min/1 cm2), and exercise therapy (McKenzie program and stabilizing exercise).[22] Each session took about 45 min.
Participants in the experimental group received five sessions of DN at the end of the second, forth, sixth, eighth, and tenth sessions. DN required an addition 15 min in each session. The DN application includes direct needling or deep DN.[11] Based on the estimated depth of targeted MTPs, 3–6 cm solid filament needles (Energy needles, Wuxi Jiajian Medical Instrument Co., Ltd, Wuxi, Jiangsu, China) were selected. The needles were inserted directly into MTPs or into a taut band by a physiotherapist experienced in palpation and treatment of MTPs. The accuracy of the needle insertion sites was confirmed through pain reproduction or observing local twitch response.[7] They were kept until there was no more pain and no more twitches. All needling was performed by the same blinded therapist for all MTPs and all participants. According to the presence of MTPs, paraspinals (iliocostalis, longissimus), multifidus, quadratus lumborum, gluteus maximus, gluteus medius, gluteus minimus, piriformis, psoas major, hamstrings (semimembranosus, semitendinosus, biceps femoris), and the gastrocnemius were needled. These muscles have a with high prevalence of active MTPs in DLBP.[26] DN was continued for each muscle as long as the subject reported MTP pain, in order words, DN sessions were canceled as soon as the subjects did not report MTP pain any more.
Statistical analysis
SPSS software (SPSS, version 22, SPSS Inc. Chicago, IL, USA) was used for the data analysis. Statistical significance was defined at α = 0.05. Normal distribution of the parameters was determined by the Shapiro–Wilk test. Since VAS data were not normally distributed, they were analyzed by the nonparametric Mann–Whitney U-test. ODQ data were analyzed through parametric independent t-tests to measure the between group differences, respectively. A 3 × 2 mixed model analysis of variance was used to calculate the change in pain intensity and disability. To control the effect of age and gender on the final pain and disability score, ANCOVA was admitted. Intention to treat (ITT) was analyzed and recorded for each group. Statistical power was analyzed using G*Power 3.0 software (Kiel, Germany).
RESULTS
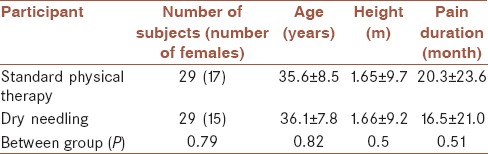
Table 1 provides demographic characteristics of the study groups.
Table 1.
Demographic characteristics of study groups
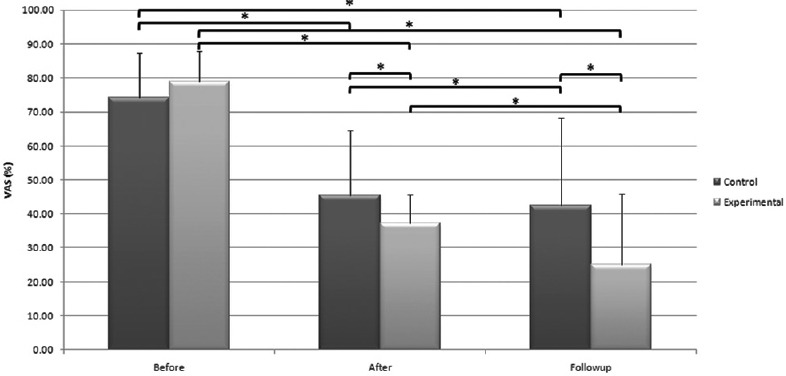
Statistical power was ≥0.8 for all the statistical tests administered in the study. The baseline pain intensity and disability scores were same in the surveyed groups (P > 0.05). Following intervention, pain intensity decreased significantly in both intervention (P < 0.001) and control groups (P < 0.001) and the change continued during follow-up period (P < 0.001 for both) [Figure 2].
Figure 2.
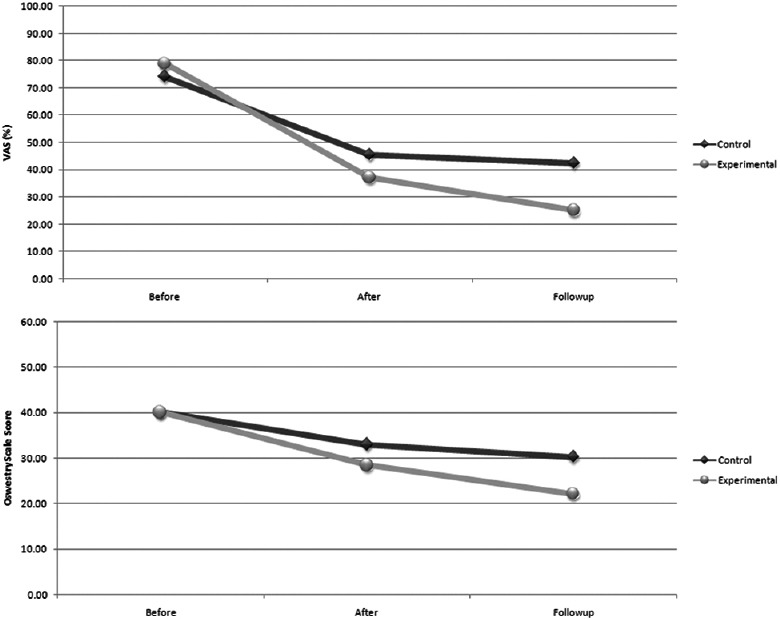
Comparing pain intensity among surveyed groups before, after, and 2 months after intervention. The asterisk represents a significant difference (α = 0.05). The standard deviations are presented as error bars
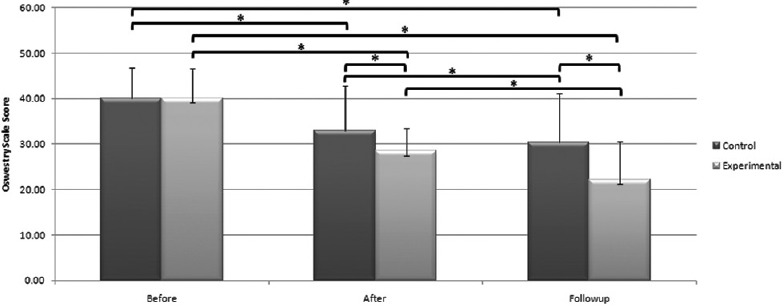
The same pattern was observed in the Oswestry Disability score (P < 0.001) [Figure 3].
Figure 3.
A comparison of pain intensity among surveyed groups before, after, and 2 months after interventions. The asterisk represents a significant difference (α = 0.05). The standard deviations are presented as error bars
However, the decrease in pain intensity (P = 0.006) and disability score (P = 0.002) were significantly more in the experimental group and at the follow-up phase [Figure 4].
Figure 4.
Comparison of disability score between study groups before, after, and 2 months after interventions. Asterisk represents significant difference (α = 0.05)
There was a significant effect for the measurement time (F [2, 57] = 80.36, P < 0.001, Wilks' Lambdatime = 0.26, multivariate partial eta squared = 0.75). Interaction between time and group was also significant (F [2, 57] = 6.22, P = 0.004, Wilks' Lambdatime × group = 0.82, multivariate partial η2 = 0.19).
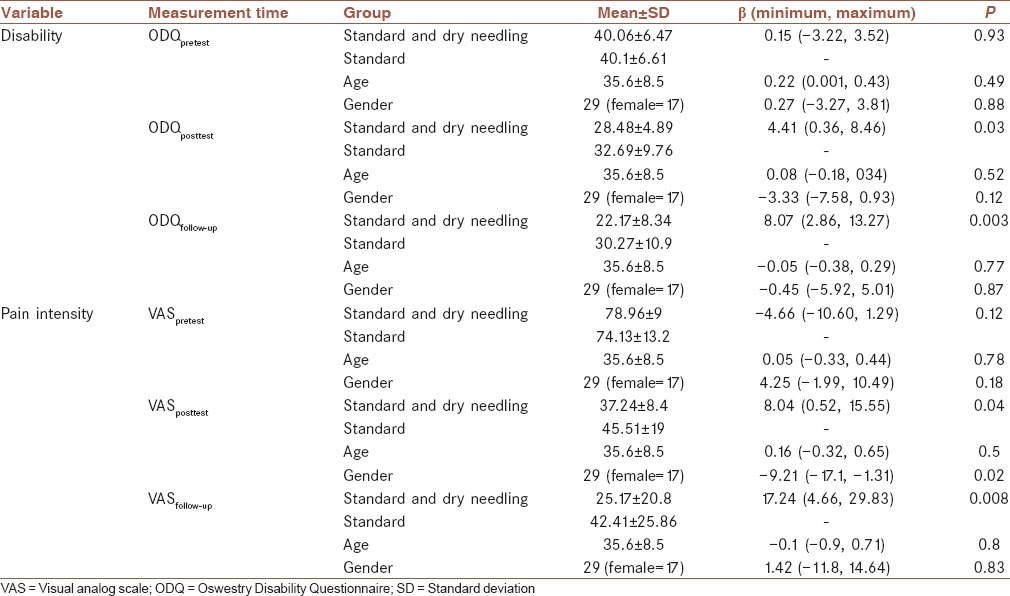
A bivariate general linear model (GLM) was also developed for adjusting the effect of the intervention type on pain and disability scores by age and gender [Table 2]. The model revealed that age and gender had no significant impact on pain and disability scores in surveyed samples.
Table 2.
Bivariate general linear model adjusting the effect of the intervention type on pain and disability scores by age and gender
In control group, ITT were 6.8–7.5% for VAS scores while they were 3.3–4.5% for disability scores (P > 0.05). In experimental group, ITT was 6.7–8.6% and 4.1–6.3% for VAS and disability scores, respectively. 19.4% of the participants in control group and 14.7% of subjects in experimental group left the study due to unwillingness to continue the program, sickness, or moving house. No harmful or unintended effects were observed in the groups.
DISCUSSION
The present single-blind randomized clinical trial was used to measure the effect of DN on pain intensity and functional disability in subjects with discogenic radiating LBP. The findings of the study confirm the hypothesis stating that DN improves pain and disability parameters in subjects treated with standard conservative physical therapy. GLM also showed that this impact is independent of subjects' age and gender. Although both intervention strategies improved pain and disability significantly, and this improvement lasted 2 months following the active intervention, it seems that adding DN to the intervention procedure increases the impact of standard intervention considerably.
Although several studies have examined the efficacy of DN for chronic LBP,[15,17,18,19,20] but the author found no study on the effect of DN on specific LBP including DLBP. The findings of the study are consistent with previous works on nonspecific LBP in term of improvement in pain and functional disability. However, because of the substantial variation in LBP pathogenesis, our results are not comparable to previous works. For example in a study by Gunn et al.,[15] subjects with chronic LBP were enrolled among whom traditional medical, rehabilitative, or surgical interventions were not successful.
Since muscle MTPs are highly susceptible to become activated in subjects with lumbar disk herniation,[26] inactivating MTPs may reduce the symptoms significantly. Our findings were consistent with the results of a recent study, where several parallel modalities were administered for the treatment of MTPs.[27]
Several previous studies indicate that DN is an effective method for subjects with chronic LBP,[15,16,17,18,19] although none of them has surveyed the effects of DN to relieve radiating pain in subjects with DLBP. Gunn hypothesized that MTPs in the multifidus muscles may result in long-term contractures with increased pressure on connective tissues surrounding the spinal cord as well as compression and irritation of the nerve roots.[9] Nerve root compression may produce radiating pain and may also contribute to the development of MTPs in corresponding myotomes through a vicious cycle.[9] It is conceivable that DN could restore the length of these paraspinal muscles.[28]
DN has also biochemical effects. It releases analgesic endorphins, increases blood flow, and improves chemical environment in the immediate vicinity of the active MTPs.[29] On the other hand, damage to the intervertebral disc increases the secretion of chemical inflammatory mediators such as phospholipase A2 and cytokinase from the nucleus pulposis, which induces nerve root inflammation and can contribute to the radiating pain commonly experienced in this kind of LBP.[5] The study demonstrated that measurement time critically affects the impact of DN on standard physical therapy improvement.
In addition, the present results imply that the radiating pain in DLBP may not be only due to a compression-induced irritation of the nerve roots, but it may also be due to the activation of MTPs in the natural course of the disorder. The muscles needled in the study were those with a high prevalence of active MTPs in DLBP and were the same muscles affected by extension and extension rotation impairments in Sahrmann approach.[30]
The muscles selected for DN in this study were practically important in managing DLBP: The quadratus lumborum muscle has an important role in spinal stability[31] and its MTPs may result in LBP;[7] the paraspinal muscles, including the iliocostalis and longissimus, are primary lumbar extensors[32] which are prone to tightness and MTP activation in DLBPs;[30] the pattern of referral pain due to gluteals' MTPs mimics that in DLBPs[7] since they are prime movers when standing from bending position.[30]
The psoas muscle contributes to lumbar lateral flexion, hip flexion, and stabilizing lumbar spine through producing compressive force.[33] It is also involved in mechanical dysfunction of the lumbar spine and LBP[30] due to its extensive spinal column attachments. It seems that management of psoas MTPs may relieve pain significantly in the subjects with LBP. Conversely, piriformis muscle is the most commonly involved muscle in LBP[8] that acts as one of the primary sources of sciatica and LBP.[34] Piriformis MTPs are common in nearly 64% of subjects suffering from LBP.[8] This muscle fills the greater sciatic foramen with the sciatic nerve passing deep inside it thus; piriformis tightness or spasm may resemble the symptoms of DLBP.
MTPs may change muscle activation patterns.[35] Lucas et al. revealed that muscle activation patterns for shoulder abduction in subjects with latent MTPs were different from the patterns observed in healthy subjects.[36] Besides, Hodges believes that the pain may change the mechanical behavior and movement patterns to protect subjects from more pain and potential damages.[37] Considering MTPs as a source of persistent activation of muscle nociceptors[38] combined with Hodge’s claims, DN may alter movement and activation patterns in paraspinals, and other muscles by deactivating MTPs.[39] Therefore, the pathological movement disorders would gradually fade and be replaced by new patterns. ITT analysis revealed that there was no significant ITT in both groups so that the observed changes may be the net effect of the intervention.
This study has some limitations; we needled various muscles at the same time that inhibits us to determine whether certain muscles are more relevant than others. Future studies may improve our understanding of the muscle involvement in DLBP through needling specific muscles.
The follow-up period was relatively short to minimize subjects' attrition. In future studies, longer follow-up along with periodical re-assessments are recommended to examine long-term effects of DN and providing a better insight of pain and symptom patterns.
CONCLUSIONS
The results of the clinical trial suggest that both intervention strategies significantly improved pain and disability immediately following the intervention while the improvement continued within 2 months after the last active intervention. The supplementary DN application enhanced the effect of the standard intervention considerably.
Financial support and sponsorship
The study was funded and ethically approved by Isfahan University of Medical Sciences as part of a Physical therapy master’s thesis (Registration code: 393082). The sponsor has no role in data collection, data analysis, and drafting the manuscript.
Conflicts of interest
There are no conflicts of interest.
AUTHORS’ CONTRIBUTIONS
All the authors contributed in the conception of the work, design of the work, data analysis, data interpretation, and drafting the work. Consequently, all the authors are accountable for all aspects of the work to ensure that accuracy and integrity of all parts of the work are appropriately investigated and resolved. The data were collected by AM.
Acknowledgments
The study is the results of a thesis for the M.Sc. degree in physical therapy registered at the Isfahan University of Medical Sciences (Grant 393082). The study protocol has been approved by the Iran Registry for Clinical Trials (IRCT Code: IRCT2015071121479N2).
REFERENCES
- 1.Vernon H. Spinal manipulation for chronic low back pain: A review of the evidence. Top Clin Chiropr. 1999;6:8–12. [Google Scholar]
- 2.Hoffman B. Confronting psychosocial issues in patients with low back pain. Top Clin Chiropr. 1999;6:1–7. [Google Scholar]
- 3.O'Sullivan P. Diagnosis and classification of chronic low back pain disorders: Maladaptive movement and motor control impairments as underlying mechanism. Man Ther. 2005;10:242–55. doi: 10.1016/j.math.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Haig AJ, Cowell M. Back Pain: A Guide for the Primary Care Physician. Philadelphia: American College of Physicians; 2005. [Google Scholar]
- 5.Saal JS, Franson RC, Dobrow R, Saal JA, White AH, Goldthwaite N. High levels of inflammatory phospholipase A2 activity in lumbar disc herniations. Spine (Phila Pa 1976) 1990;15:674–8. doi: 10.1097/00007632-199007000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Flax HJ. Myofascial pain syndromes – The great mimicker. Bol Asoc Med P R. 1995;87:167–70. [PubMed] [Google Scholar]
- 7.Simons D, Travell J, Simons L. Travell and Simons' Myofascial Pain and Dysfunction: The Trigger Point Manual. Baltimore, MD: Williams and Wilkins; 1999. [Google Scholar]
- 8.Chen CK, Nizar AJ. Myofascial pain syndrome in chronic back pain patients. Korean J Pain. 2011;24:100–4. doi: 10.3344/kjp.2011.24.2.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gunn CC. The Gunn Approach to the Treatment of Chronic Pain. 2nd ed. New York: Churchill Livingstone; 1996. [Google Scholar]
- 10.Rickards LD. The effectiveness of non-invasive treatments for active myofascial trigger point pain: A systematic review of the literature. Int J Osteopath Med. 2006;9:120–36. [Google Scholar]
- 11.Dommerholt J, Huijbregts P. Myofascial Trigger Points: Pathophysiology and Evidence-informed Diagnosis and Management. London: Jones and Bartlett Learning; 2010. [Google Scholar]
- 12.Ziaeifar M, Arab AM, Karimi N, Nourbakhsh MR. The effect of dry needling on pain, pressure pain threshold and disability in patients with a myofascial trigger point in the upper trapezius muscle. J Bodyw Mov Ther. 2014;18:298–305. doi: 10.1016/j.jbmt.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 13.Lewit K. The needle effect in the relief of myofascial pain. Pain. 1979;6:83–90. doi: 10.1016/0304-3959(79)90142-8. [DOI] [PubMed] [Google Scholar]
- 14.Witt CM, Pach D, Brinkhaus B, Wruck K, Tag B, Mank S, et al. Safety of acupuncture: Results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forsch Komplementmed. 2009;16:91–7. doi: 10.1159/000209315. [DOI] [PubMed] [Google Scholar]
- 15.Gunn CC, Milbrandt WE, Little AS, Mason KE. Dry needling of muscle motor points for chronic low-back pain: A randomized clinical trial with long-term follow-up. Spine (Phila Pa 1976) 1980;5:279–91. doi: 10.1097/00007632-198005000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Hong CZ. Comment on Gunn’s “radiculopathy model of myofascial trigger points”. J Musculoskelet Pain. 2000;8:133–5. [Google Scholar]
- 17.Furlan AD, van Tulder M, Cherkin D, Tsukayama H, Lao L, Koes B, et al. Acupuncture and dry-needling for low back pain: An updated systematic review within the framework of the cochrane collaboration. Spine (Phila Pa 1976) 2005;30:944–63. doi: 10.1097/01.brs.0000158941.21571.01. [DOI] [PubMed] [Google Scholar]
- 18.Itoh K, Katsumi Y, Kitakoji H. Trigger point acupuncture treatment of chronic low back pain in elderly patients – A blinded RCT. Acupunct Med. 2004;22:170–7. doi: 10.1136/aim.22.4.170. [DOI] [PubMed] [Google Scholar]
- 19.Haake M, Müller HH, Schade-Brittinger C, Basler HD, Schäfer H, Maier C, et al. German acupuncture trials (GERAC) for chronic low back pain: Randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007;167:1892–8. doi: 10.1001/archinte.167.17.1892. [DOI] [PubMed] [Google Scholar]
- 20.Téllez-García M, de-la-Llave-Rincón AI, Salom-Moreno J, Palacios-Ceña M, Ortega-Santiago R, Fernández-de-Las-Peñas C. Neuroscience education in addition to trigger point dry needling for the management of patients with mechanical chronic low back pain: A preliminary clinical trial. J Bodyw Mov Ther. 2015;19:464–72. doi: 10.1016/j.jbmt.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 21.Edwards J, Knowles N. Superficial dry needling and active stretching in the treatment of myofascial pain – A randomised controlled trial. Acupunct Med. 2003;21:80–6. doi: 10.1136/aim.21.3.80. [DOI] [PubMed] [Google Scholar]
- 22.Hertling D, Kessler RM. Management of Common Musculoskeletal Disorders: Physical Therapy Principles and Methods. New york, London: Lippincott Williams and Wilkins; 2006. [Google Scholar]
- 23.Dommerholt J, Fernández-de-las-Peñas C. Trigger Point Dry Needling, An Evidence and Clinical-Based Approach. New york, London: Elsevier Health Sciences; 2013. [Google Scholar]
- 24.Ogon M, Krismer M, Söllner W, Kantner-Rumplmair W, Lampe A. Chronic low back pain measurement with visual analogue scales in different settings. Pain. 1996;64:425–8. doi: 10.1016/0304-3959(95)00208-1. [DOI] [PubMed] [Google Scholar]
- 25.Mousavi SJ, Parnianpour M, Mehdian H, Montazeri A, Mobini B. The Oswestry Disability Index, the Roland-Morris Disability Questionnaire, and the Quebec back pain disability scale: Translation and validation studies of the Iranian versions. Spine (Phila Pa 1976) 2006;31:E454–9. doi: 10.1097/01.brs.0000222141.61424.f7. [DOI] [PubMed] [Google Scholar]
- 26.Motealleh AS, Yazdani S, Abbasi L. Tehran, Iran: 24th Iranian Annual Physical Therapy Congress; 2013. May 8-12, Determination of trigger point prevalence in some lumbar and lower extremity muscles in subjects suffering from lumbar disc bulging and protrusion. [Google Scholar]
- 27.Renan-Ordine R, Alburquerque-Sendín F, de Souza DP, Cleland JA, Fernández-de-Las-Peñas C. Effectiveness of myofascial trigger point manual therapy combined with a self-stretching protocol for the management of plantar heel pain: A randomized controlled trial. J Orthop Sports Phys Ther. 2011;41:43–50. doi: 10.2519/jospt.2011.3504. [DOI] [PubMed] [Google Scholar]
- 28.Langevin HM, Bouffard NA, Churchill DL, Badger GJ. Connective tissue fibroblast response to acupuncture: Dose-dependent effect of bidirectional needle rotation. J Altern Complement Med. 2007;13:355–60. doi: 10.1089/acm.2007.6351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shah JP, Gilliams EA. Uncovering the biochemical milieu of myofascial trigger points using in vivo microdialysis: An application of muscle pain concepts to myofascial pain syndrome. J Bodyw Mov Ther. 2008;12:371–84. doi: 10.1016/j.jbmt.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Sahrmann S. Diagnosis and Treatment of Movement Impairment Syndromes. New york, London: Elsevier Health Sciences; 2002. [Google Scholar]
- 31.McGill S, Juker D, Kropf P. Quantitative intramuscular myoelectric activity of quadratus lumborum during a wide variety of tasks. Clin Biomech (Bristol, Avon) 1996;11:170–2. doi: 10.1016/0268-0033(95)00056-9. [DOI] [PubMed] [Google Scholar]
- 32.Bogduk N, Macintosh JE, Pearcy MJ. A universal model of the lumbar back muscles in the upright position. Spine (Phila Pa 1976. 1992;17:897–913. doi: 10.1097/00007632-199208000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Santaguida PL, McGill SM. The psoas major muscle: A three-dimensional geometric study. J Biomech. 1995;28:339–45. doi: 10.1016/0021-9290(94)00064-b. [DOI] [PubMed] [Google Scholar]
- 34.Durrani Z, Winnie AP. Piriformis muscle syndrome: An underdiagnosed cause of sciatica. J Pain Symptom Manage. 1991;6:374–9. doi: 10.1016/0885-3924(91)90029-4. [DOI] [PubMed] [Google Scholar]
- 35.Fernández-Carnero J, Ge HY, Kimura Y, Fernández-de-Las-Peñas C, Arendt-Nielsen L. Increased spontaneous electrical activity at a latent myofascial trigger point after nociceptive stimulation of another latent trigger point. Clin J Pain. 2010;26:138–43. doi: 10.1097/AJP.0b013e3181bad736. [DOI] [PubMed] [Google Scholar]
- 36.Lucas KR, Rich PA, Polus BI. Muscle activation patterns in the scapular positioning muscles during loaded scapular plane elevation: The effects of latent myofascial trigger points. Clin Biomech (Bristol, Avon) 2010;25:765–70. doi: 10.1016/j.clinbiomech.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 37.Hodges PW. Pain and motor control: From the laboratory to rehabilitation. J Electromyogr Kinesiol. 2011;21:220–8. doi: 10.1016/j.jelekin.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 38.Fernández-Lao C, Cantarero-Villanueva I, Fernández-de-Las-Peñas C, Del-Moral-Ávila R, Arendt-Nielsen L, Arroyo-Morales M. Myofascial trigger points in neck and shoulder muscles and widespread pressure pain hypersensitivtiy in patients with postmastectomy pain: Evidence of peripheral and central sensitization. Clin J Pain. 2010;26:798–806. doi: 10.1097/AJP.0b013e3181f18c36. [DOI] [PubMed] [Google Scholar]
- 39.Dommerholt J. Dry needling – Peripheral and central considerations. J Man Manip Ther. 2011;19:223–7. doi: 10.1179/106698111X13129729552065. [DOI] [PMC free article] [PubMed] [Google Scholar]