Abstract
Background:
Metabolic syndrome (MetS), a cluster of cardiovascular risk factors, is one of the most common metabolic disorders, which lead to many chronic diseases. The link between childhood MetS and occurrence of atherosclerosis and its sequels in adulthood is well documented. This study aims to systematically review the prevalence of MetS among Iranian children and adolescents.
Materials and Methods:
An electronic search was conducted on studies published from January 1990 to January 2015. The main international electronic data sources were PubMed and the NLM Gateway (for MEDLINE), Institute of Scientific Information (ISI), and SCOPUS. For Persian databases, we used domestic databases. We included all available population-based studies and national surveys conducted in the pediatric age group aged 3–21-year-old.
Results:
In this review, 2138 articles were identified (PubMed: 265; SCOPUS: 368; ISI: 465; Scientific Information Database: 189; IranMedex: 851; Irandoc: 46). After quality assessment, 13 qualified articles were evaluated. The number of total population and points of data were 24,772 and 125, respectively. Regarding the geographical distribution, we found 2 national, 6 provincial, and 5 district level points of data. The prevalence range of MetS among children was 1–22% using different definitions. Reported range of pediatric MetS defined by different criteria was as follows: National Cholesterol Education Program-Adult Treatment Panel III; 3–16%, International Diabetes Federation; 0–8%, American Heart Association; 4–9.5%, The National Health and Nutrition Examination Survey III; 1–18%, de Ferranti; 0–22%.
Conclusion:
MetS is a common metabolic disorder among Iranian children and adolescents, with increasing trends during the last decades. This finding provides baseline useful information for health policy makers to implement evidence based-health promotion for appropriate controlling of this growing health problem for the pediatric population.
Keywords: Iran, metabolic syndrome, pediatrics, prevalence, systematic review
INTRODUCTION
Noncommunicable diseases (NCDs) are considered as a global health problem with more considerable increasing trend in low- and middle-income countries (LMIC).[1,2] NCDs are the main causes of morbidity and mortality, especially in LMICs. The Global Burden of Disease Studies in 1990, 2000, and 2013 have reported that metabolic risk factors are the most important determinants of emerging NCDs all over the world.[3,4,5,6,7] The most common causes of NCDs-related morbidity and mortality are cardiovascular disease (CVD).[8]
Metabolic syndrome (MetS), a cluster of cardiovascular risk factors, is one of the most common metabolic disorders, which leads to many chronic diseases as CVDs, diabetes mellitus, cancer, kidney disease, and mental illness.[9,10,11,12] The concept of MetS in children and adolescents gain great concern during last decades due to the factors such as epidemiologic transition, double burden of nutritional disorders, lifestyle changes, and considerably high prevalence of obesity.
Mentioned clustering may be associated with specific morbidity in childhood and different cardiometabolic disorders in adulthood.[13] In addition, there is growing body of evidence regarding the embryonic origin of the disorder.[14]
Though the prevalence of MetS among children and adolescents have been investigated in different populations worldwide, estimating the prevalence of MetS in children is a challenging issue due to the fact that different definitions used for MetS in children. The reported prevalence rates of MetS among children and adolescents ranged between 0 and 19.2%.[15]
Iran is facing a double burden of the diseases and is in a rapid epidemiological transition state. According to the findings of a nationwide survey, the prevalence of MetS in children have been reported to be 2.5%.[16] Moreover, some regional studies investigated the prevalence of pediatric MetS by using different diagnostic criteria.[17,18,19,20,21,22,23,24,25,26,27,28]
Given that MetS could be one of the most proper indexes for detecting people at high risk for NCDs and by considering that MetS and its components track from childhood to adulthood, it seems that determining the prevalence of Mets among Iranian children and adolescents would help us to assess the most effective preventive measures and interventional policies and consequently reduce the burden of NCDs and its related risk factors.
Therefore, this study aims to systematically review the prevalence of pediatric MetS among Iranian children and adolescents.
MATERIALS AND METHODS
This systematic review determined the prevalence of MetS among Iranian pediatric population; it is conducted as part of the National and Sub-national Burden of Diseases (NASBOD) study, from 1990 to 2014.[29,30] Methodology of the study (NASBOD) has been described in details, previously. The study protocol was approved by the Regional Ethics Committee of Isfahan University of Medical Sciences. Herein, we present the methods of current study in brief.
Outcomes definition
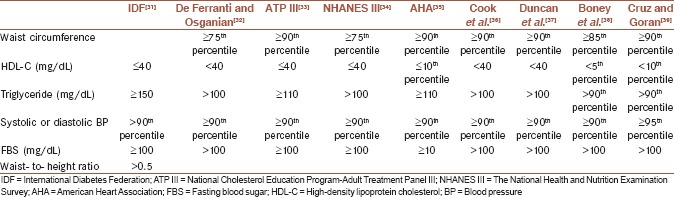
All included definitions of MetS in children and adolescents are presented in Appendix 1.[31,32,33,34,35,36,37,38,39]
Search strategy
To assess the English and Persian papers on pediatric MetS in Iranian children and adolescents, published papers were searched from January 1990 to January 2015. The main international electronic data sources were PubMed and the NLM Gateway (for MEDLINE), Institute of Scientific Information (ISI), and SCOPUS. Domestic databases with systematic search capability and the most coverage of national indexed Iranian scientific journals including IranMedex, Irandoc, and Scientific Information Database (SID) were used for Persian document [Table 1].
Table 1.
Search strategy for the prevalence of metabolic syndrome in Iranian pediatric population
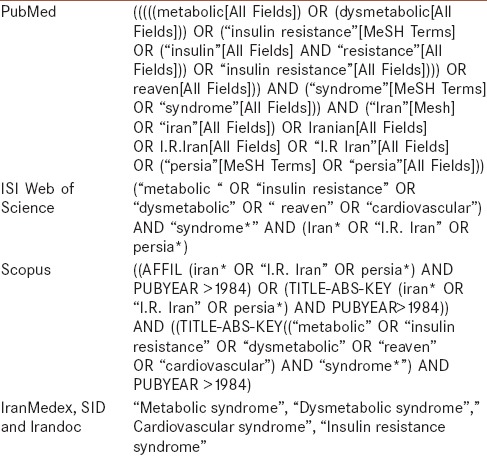
To have a more comprehensive search, the Emtree of SCOPUS and the medical subject headings (mesh) including entry terms of PubMed were used. The Persian keywords equivalent to their English search terms were used for national search.
The systematic search of electronic databases followed by the comprehensive hand searching process to obtain the highest level of access to the published, available unpublished and gray literature.
The new cases were added through register system of international database, for more data availability.
All the Iranian scientific journals not indexed in electronic databases, governmental reports, projects' reports, conferences, and reference lists were reviewed by hand searching [Table 1].
Study selection and eligibility criteria
We limited the search results to national, provincial, district, community population-based studies in child and adolescence, to Iran, to human subject (age 6–18 years) and to time period of January 1990–January 2014. There was no restriction on language. All research papers, abstracts, conference proceeding, titles of thesis, dissertations, and reports included to our inclusion criteria as document types.
We excluded papers of nonpopulation-based studies. The studies that focused on special populations such as school-based studies were excluded. When there were multiple publications from the same population, only the largest study or the main source of data was included.
Data management
The results of each of databases' search import to separate endnote library. Duplicated papers were deleted. Remained papers were assessed in three phases for relevancy: Title; title abstract and full text review.
Quality assessment and data extraction
Quality of each selected paper was determined using quality assessment form which contains three parts as follows; general information, sampling quality, and measurement quality. Using the forms each paper was ranked as excellent,[13,14,15,16,17,18,19] good,[6,7,8,9,10,11,12] or poor (≤5) based on total score. Data were extracted from papers with good and excellent quality score. The quality assessment has been followed independently by two research experts (Kappa statistic for agreement for quality assessment; 0.92) and probable discrepancy between them resolved based on third expert opinion.
Data from selected eligible papers were extracted using standardized data extraction sheet.[40] This process was conducted by two researchers. In the cases of discrepancy, a third expert consulted for resolving it.
Details of each study including its general information, characteristics of studied population, methodology of each study, total sample size, age and sex groups, urban/rural areas, different definitions of MetS, which was used and reported prevalence and study outcomes indicators (age specific prevalence of MetS) were recorded in the predefined standard electronic data extraction sheets.
RESULTS
In this review, 2138 articles were identified (PubMed: 265; SCOPUS: 368; ISI: 465; SID: 189; IranMedex: 851; Irandoc: 46). During three refine steps and after removing of duplicates, 179 articles related to the study domain were selected. After quality assessment, 197 studies were selected for text appraisal, of which 13 qualified articles were evaluated at the final step. Overall, 2 of 13 articles were from the CASPIAN I and III studies [Figure 1].
Figure 1.
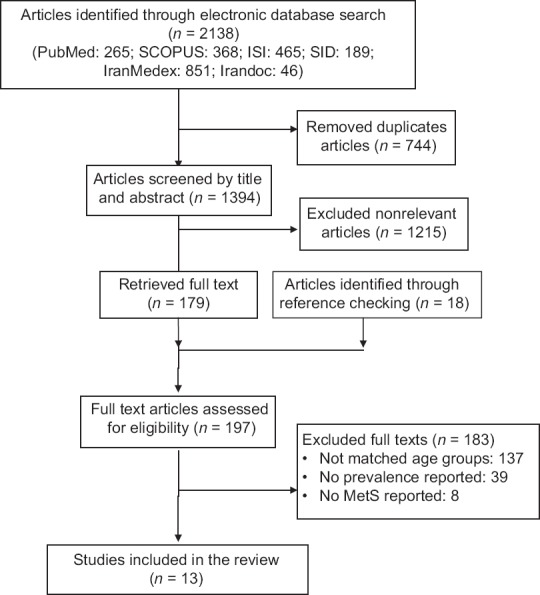
Flowchart of study selection
Considering the whole data of systematic review results and national data sources; the number of total population and points of data were 24,772 and 125, respectively. From reported points of data, 51 of them were for total population and 37 and 37 of them were not for girls and boys, respectively. Regarding the geographically distribution, we found 2 national, 6 provincial, and 5 district level points of data.
In one of the articles (1 out of 13), preschool children (aged <6 years) were included. In other papers, the age range of studied population was 6–21-year-old.
Table 2 represents the prevalence of MetS in Iranian children and adolescences during 1990–2013 using different definition for MetS.
Table 2.
The prevalence of metabolic syndrome in population-based studies in Iranian children and adolescences 1990-2013
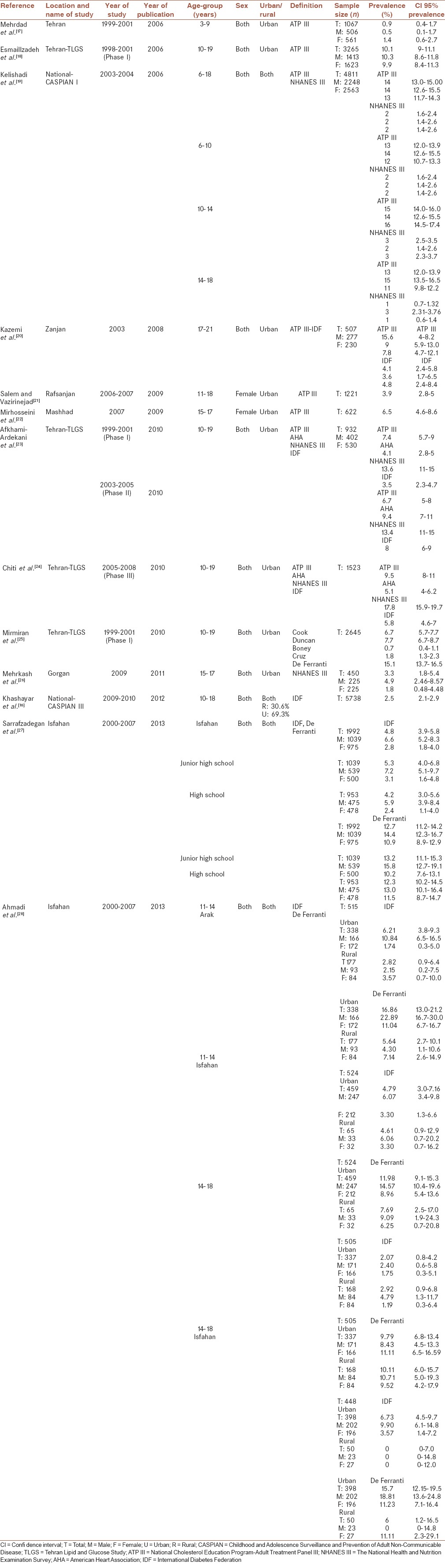
The prevalence range of MetS among children was 1–22% according to different definition. Reported range of pediatric MetS by different definition criteria were as follows: National Cholesterol Education Program-Adult Treatment Panel III (ATP III); 3–16%, International Diabetes Federation (IDF); 0–8%, American Heart Association (AHA); 4–9.5%, The National Health and Nutrition Examination Survey (NHANES III); 1–18%, de Ferranti: 0–22%.
DISCUSSION
In this study, for the 1st time in Iran, we systematically reviewed studies reporting the prevalence of MetS among Iranian pediatric population. Reviewing data of 24,772 total population with 125 point of data, indicated that as a result of nutritional transition, MetS is a common metabolic disorder among Iranian children. The summarized epidemiologic data of MetS provide us baseline information and identifies fields that should be investigated in future research.
A review study in 2004 reported an estimated prevalence rate of 3–4% for pediatrics MetS.[39] The corresponding figure in another review on 36 articles published between 2007 and 2009 was 1.2–22.6%.[41] A recent review on published reports worldwide in 2012 and showed that the prevalence of MetS ranged from 0 to 19.2% with a median of 3.3%.[15]
In this study, based on various definitions, the reported range for the prevalence of MetS was 1–22%. Reported range of pediatric MetS using different criteria was as follows: ATP III: 3–16%, IDF: 0–8%, AHA: 4–9.5%, NHANES III: 1–18%, de Ferranti : 0–22%. The results of the current review were similar to that reported for its worldwide prevalence.
As there is no consensus regarding the definition of pediatrics MetS, various prevalence rates of this disorder have been reported in different studies. Ford and Li have indicated that forty definitions of MetS in children have been used in 27 publications.[42] It seems that for determining how different definitions or cutoff values influence the prevalence rate of Mets, we should compare the rate reported by different criteria in the same population. Though some studies in Iran had reported the rate of MetS in children according to different criteria, but considering the range of reported rate of Mets, we could not reach accurate conclusion in this field. It is suggested that among different definitions, IDF definition for the pediatric age group is more appropriate.[43]
It seems that comparing the results of two CASPIAN survey could help us to suggest the changes in the prevalence of this disorder among Iranian pediatric population. Reevaluation and determining the prevalence of MetS in two surveys of the CASPIAN study according to the same criteria (IDF), showed that the prevalence of MetS had increased, i.e., in similar age groups of children and adolescents in CASPIAN I and III, it was 2.7% and 4%, respectively. It may be due to the effect of epidemiologic transition of our region.
In a study among 1018 Emirati adolescents, aged 12–18 years, the prevalence of MetS according to the IDF definition was 13% (21% in boys and 4% in girls).[44] The corresponding figure was 7.6% among Chinese adolescents with higher proportion in boys using IDF criteria.[45]
The results of current study regarding gender difference in the prevalence of Mets were heterogeneous. In some studies, it was similar in both sexes and in others, it was higher in boys. In a study in India, the prevalence of MetS was higher in girls than in boys.[46]
The results of a review study proposed higher prevalence of MetS in boys than in girls.[15]
In the current study, the prevalence of MetS was higher in older children than in younger ones; this finding was in line with some other studies.[15] It may be due to that by increasing age and during prepubertal and pubertal periods, some changes including increasing in insulin resistance, body fat, and blood pressure and decreasing in insulin sensitivity will be occurred. In addition, some other changes in lifestyle such as decreasing physical activity, smoking, or changes in eating habits may explain the higher rate of MetS in older children and adolescents.[47]
Most studies included in this review have reported the prevalence of MetS in urban population, but the results of three studies conducted in both urban and rural areas have demonstrated that the prevalence of MetS was higher among urban than in rural children and adolescents.[16,19,28] Tandon et al. in India have reported higher rate of MetS in urban population.[46,48,49] The lower prevalence of MetS in rural children might be because of their healthier lifestyle in terms of higher physical activity and more natural dietary habits.
This study is the first systematic review study about the prevalence of pediatric MetS in a country located in the Middle East and North Africa. We used all available national and sub-national sources of data using advanced comprehensive search approaches. We considered all published, unpublished and gray literature, as well as the main national sources.
The limitations of this review were large variations of data for the range of prevalence rates of MetS reported among Iranian children and adolescents, this variation is mainly because of different criteria used for definition of Mets, differences in the geographical location of populations studied as well as their nutritional, social and cultural characteristics, quality of the data, methodology of the studies and studied population. Therefore, we had limitation for appropriate comparison of available data. In addition, most of the data were related to children aged 6 years and older and scarce data existed for preschool-age children.
CONCLUSION
Reviewing the reports of available epidemiological data regarding the prevalence rate of MetS indicated that MetS is one important disorder in Iranian pediatric population, with a rate comparable to that reported worldwide. We also found that the prevalence of pediatric MetS has increased in Iran. The current findings underscore the necessity of implementation of evidence-based policies and programs for health promotion and primordial prevention of NCD.
Financial support and sponsorship
The study is granted by Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
AUTHORS’ CONTRIBUTIONS
All authors had contribution in the general designing of paper, designing of systematic review, primary draft preparation, and revision. All authors have given approval to the final version of the manuscript, and accepted the responsibility of its content.
APPENDIX
Appendix 1.
Different definitions of metabolic syndrome in the pediatric age group
REFERENCES
- 1.Boutayeb A, Boutayeb S. The burden of non communicable diseases in developing countries. Int J Equity Health. 2005;4:2. doi: 10.1186/1475-9276-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: Findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 3.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, et al. GBD 2010: A multi-investigator collaboration for global comparative descriptive epidemiology. Lancet. 2012;380:2055–8. doi: 10.1016/S0140-6736(12)62134-5. [DOI] [PubMed] [Google Scholar]
- 5.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 6.Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011;377:557–67. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stevens GA, Singh GM, Lu Y, Danaei G, Lin JK, Finucane MM, et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr. 2012;10:22. doi: 10.1186/1478-7954-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boutayeb A, Boutayeb S, Boutayeb W. Multi-morbidity of non communicable diseases and equity in WHO eastern mediterranean countries. Int J Equity Health. 2013;12:60. doi: 10.1186/1475-9276-12-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Borena W, Edlinger M, Bjørge T, Häggström C, Lindkvist B, Nagel G, et al. A prospective study on metabolic risk factors and gallbladder cancer in the metabolic syndrome and cancer (Me-Can) collaborative study. PLoS One. 2014;9:e89368. doi: 10.1371/journal.pone.0089368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maleki A, Montazeri M, Rashidi N, Montazeri M, Yousefi-Abdolmaleki E. Metabolic syndrome and its components associated with chronic kidney disease. J Res Med Sci. 2015;20:465–9. doi: 10.4103/1735-1995.163969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pan A, Keum N, Okereke OI, Sun Q, Kivimaki M, Rubin RR, et al. Bidirectional association between depression and metabolic syndrome: A systematic review and meta-analysis of epidemiological studies. Diabetes Care. 2012;35:1171–80. doi: 10.2337/dc11-2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jari M, Qorbani M, Motlagh ME, Heshmat R, Ardalan G, Kelishadi R. Association of overweight and obesity with mental distress in Iranian adolescents: The CASPIAN-III study. Int J Prev Med. 2014;5:256–61. [PMC free article] [PubMed] [Google Scholar]
- 13.Kursawe R, Santoro N. Metabolic syndrome in pediatrics. Adv Clin Chem. 2014;65:91–142. doi: 10.1016/b978-0-12-800141-7.00004-8. [DOI] [PubMed] [Google Scholar]
- 14.McMillen IC, Robinson JS. Developmental origins of the metabolic syndrome: Prediction, plasticity, and programming. Physiol Rev. 2005;85:571–633. doi: 10.1152/physrev.00053.2003. [DOI] [PubMed] [Google Scholar]
- 15.Friend A, Craig L, Turner S. The prevalence of metabolic syndrome in children: A systematic review of the literature. Metab Syndr Relat Disord. 2013;11:71–80. doi: 10.1089/met.2012.0122. [DOI] [PubMed] [Google Scholar]
- 16.Khashayar P, Heshmat R, Qorbani M, Motlagh ME, Aminaee T, Ardalan G, et al. Metabolic syndrome and cardiovascular risk factors in a national sample of adolescent population in the Middle East and North Africa: The CASPIAN III study. Int J Endocrinol 2013. 2013:702095. doi: 10.1155/2013/702095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehrdad SM, Hosseinpanah F, Azizi F. Metabolic syndrome prevalence in 3-9 years old children: Tehran glucose and lipid study. Res Med. 2006;30:337–46. [Google Scholar]
- 18.Esmaillzadeh A, Mirmiran P, Azadbakht L, Etemadi A, Azizi F. High prevalence of the metabolic syndrome in Iranian adolescents. Obesity (Silver Spring) 2006;14:377–82. doi: 10.1038/oby.2006.50. [DOI] [PubMed] [Google Scholar]
- 19.Kelishadi R, Ardalan G, Gheiratmand R, Adeli K, Delavari A, Majdzadeh R Caspian Study Group. Paediatric metabolic syndrome and associated anthropometric indices: The CASPIAN Study. Acta Paediatr. 2006;95:1625–34. doi: 10.1080/08035250600750072. [DOI] [PubMed] [Google Scholar]
- 20.Kazemi S, Koosha A, Sharifi F, Moosavi-Nasab SN, Mellati AA. Metabolic syndrome prevalence in 17-21 years old population of Zanjan: A new definition for waist circumference in Iranians in comparison with ATPIII and World Diabetes Association. Iran Diabetes Lipid J. 2008;7:393–8. [Google Scholar]
- 21.Salem Z, Vazirinejad R. Prevalence of obesity and metabolic syndrome in adolescent girls in South East of Iran. Pak J Med Sci. 2009;25:196–200. [Google Scholar]
- 22.Mirhosseini NZ, Yusoff NA, Shahar S, Parizadeh SM, Mobarhen MG, Shakery MT. Prevalence of the metabolic syndrome and its influencing factors among adolescent girls in Mashhad, Iran. Asia Pac J Clin Nutr. 2009;18:131–6. [PubMed] [Google Scholar]
- 23.Afkhami-Ardekani M, Zahedi-Asl S, Rashidi M, Atifah M, Hosseinpanah F, Azizi F. Incidence and trend of a metabolic syndrome phenotype among Tehranian adolescents: Findings from the Tehran lipid and glucose study, 1998-2001 to 2003-2006. Diabetes Care. 2010;33:2110–2. doi: 10.2337/dc09-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chiti H, Hoseinpanah F, Mehrabi Y, Azizi F. The prevalence of metabolic syndrome in adolescents with varying degrees of body weight: Tehran lipid and glucose study (TLGS) Iran J Endocrinol Metab. 2009;11:625–37. [Google Scholar]
- 25.Mirmiran P, Sherafat-Kazemzadeh R, Farahani SJ, Asghari G, Niroomand M, Momenan A, et al. Performance of different definitions of metabolic syndrome for children and adolescents in a 6-year follow-up: Tehran lipid and glucose study (TLGS) Diabetes Res Clin Pract. 2010;89:327–33. doi: 10.1016/j.diabres.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 26.Mehrkash M, Kelishadi R, Mohammadian S, Mousavinasab F, Qorbani M, Hashemi ME, et al. Obesity and metabolic syndrome among a representative sample of Iranian adolescents. Southeast Asian J Trop Med Public Health. 2012;43:756. [PubMed] [Google Scholar]
- 27.Sarrafzadegan N, Gharipour M, Sadeghi M, Nouri F, Asgary S, Zarfeshani S. Differences in the prevalence of metabolic syndrome in boys and girls based on various definitions. ARYA Atheroscler. 2013;9:70–6. [PMC free article] [PubMed] [Google Scholar]
- 28.Ahmadi A, Gharipour M, Nouri F, Sarrafzadegan N. Metabolic syndrome in Iranian youths: A population-based study on junior and high schools students in rural and urban areas. J Diabetes Res 2013. 2013:738485. doi: 10.1155/2013/738485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Farzadfar F, Delavari A, Malekzadeh R, Mesdaghinia A, Jamshidi HR, Sayyari A, et al. NASBOD 2013: Design, definitions, and metrics. Arch Iran Med. 2014;17:7–15. [PubMed] [Google Scholar]
- 30.Kelishadi R, Hovsepian S, Qorbani M, Jamshidi F, Fallah Z, Djalalinia S, et al. National and sub-national prevalence, trend, and burden of cardiometabolic risk factors in Iranian children and adolescents, 1990-2013. Arch Iran Med. 2014;17:71–80. [PubMed] [Google Scholar]
- 31.Zimmet P, Alberti KG, Kaufman F, Tajima N, Silink M, Arslanian S, et al. The metabolic syndrome in children and adolescents – An IDF consensus report. Pediatr Diabetes. 2007;8:299–306. doi: 10.1111/j.1399-5448.2007.00271.x. [DOI] [PubMed] [Google Scholar]
- 32.De Ferranti SD, Osganian SK. Epidemiology of paediatric metabolic syndrome and type 2 diabetes mellitus. Diab Vasc Dis Res. 2007;4:285–96. doi: 10.3132/dvdr.2007.055. [DOI] [PubMed] [Google Scholar]
- 33.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 34.de Ferranti SD, Gauvreau K, Ludwig DS, Neufeld EJ, Newburger JW, Rifai N. Prevalence of the metabolic syndrome in American adolescents: Findings from the Third National Health and Nutrition Examination Survey. Circulation. 2004;110:2494–7. doi: 10.1161/01.CIR.0000145117.40114.C7. [DOI] [PubMed] [Google Scholar]
- 35.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Arterioscler Thromb Vasc Biol. 2004;24:e13–8. doi: 10.1161/01.ATV.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 36.Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: Findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003;157:821–7. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- 37.Duncan GE, Li SM, Zhou XH. Prevalence and trends of a metabolic syndrome phenotype among U.S. Adolescents, 1999-2000. Diabetes Care. 2004;27:2438–43. doi: 10.2337/diacare.27.10.2438. [DOI] [PubMed] [Google Scholar]
- 38.Boney CM, Verma A, Tucker R, Vohr BR. Metabolic syndrome in childhood: Association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. 2005;115:e290–6. doi: 10.1542/peds.2004-1808. [DOI] [PubMed] [Google Scholar]
- 39.Cruz ML, Goran MI. The metabolic syndrome in children and adolescents. Curr Diab Rep. 2004;4:53–62. doi: 10.1007/s11892-004-0012-x. [DOI] [PubMed] [Google Scholar]
- 40.Forouzanfar MH, Sepanlou SG, Shahraz S, Dicker D, Naghavi P, Pourmalek F, et al. Evaluating causes of death and morbidity in Iran, global burden of diseases, injuries, and risk factors study 2010. Arch Iran Med. 2014;17:304–20. [PubMed] [Google Scholar]
- 41.Tailor AM, Peeters PH, Norat T, Vineis P, Romaguera D. An update on the prevalence of the metabolic syndrome in children and adolescents. Int J Pediatr Obes. 2010;5:202–13. doi: 10.3109/17477160903281079. [DOI] [PubMed] [Google Scholar]
- 42.Ford ES, Li C. Defining the metabolic syndrome in children and adolescents: Will the real definition please stand up? J Pediatr. 2008;152:160–4. doi: 10.1016/j.jpeds.2007.07.056. [DOI] [PubMed] [Google Scholar]
- 43.Zimmet P, Alberti G, Kaufman F, Tajima N, Silink M, Arslanian S, et al. The metabolic syndrome in children and adolescents. Lancet. 2007;369:2059–61. doi: 10.1016/S0140-6736(07)60958-1. [DOI] [PubMed] [Google Scholar]
- 44.Mehairi AE, Khouri AA, Naqbi MM, Muhairi SJ, Maskari FA, Nagelkerke N, et al. Metabolic syndrome among Emirati adolescents: A school-based study. PLoS One. 2013;8:e56159. doi: 10.1371/journal.pone.0056159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li P, Jiang R, Li L, Liu C, Yang F, Qiu Y. Prevalence and risk factors of metabolic syndrome in school adolescents of northeast China. J Pediatr Endocrinol Metab. 2014;27:525–32. doi: 10.1515/jpem-2013-0336. [DOI] [PubMed] [Google Scholar]
- 46.Tandon N, Garg MK, Singh Y, Marwaha RK. Prevalence of metabolic syndrome among urban Indian adolescents and its relation with insulin resistance (HOMA-IR) J Pediatr Endocrinol Metab. 2013;26:1123–30. doi: 10.1515/jpem-2013-0020. [DOI] [PubMed] [Google Scholar]
- 47.Jessup A, Harrell SJ. The metabolic syndrome: Look for it in children and adolescents, too! Clin Diabetes. 2005;23:26–32. [Google Scholar]
- 48.Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93(11 Suppl 1):S9–30. doi: 10.1210/jc.2008-1595. [DOI] [PubMed] [Google Scholar]
- 49.Singh N, Parihar RK, Saini G, Mohan SK, Sharma N, Razaq M. Prevalence of metabolic syndrome in adolescents aged 10-18 years in Jammu, J and K. Indian J Endocrinol Metab. 2013;17:133–7. doi: 10.4103/2230-8210.107849. [DOI] [PMC free article] [PubMed] [Google Scholar]


