Abstract
Objective
This study aimed to define the ethnographic composition and assess the health-related quality of life (HRQoL) of a large population of undocumented patients with end-stage renal disease (ESRD) seeking emergent dialysis in the emergency department (ED) of a large public hospital in the United States.
Design
All ESRD patients presenting to the hospital’s main ED were identified during a 4-week consecutive enrollment period. Consenting patients completed two surveys—an ethnographic questionnaire and the validated kidney disease quality of life-36 (KDQOL-36) instrument.
Setting
The study was conducted at a large county hospital in Dallas, Texas. In 2013, the hospital recorded >50,000 ED visits and administered approximately 6,000 dialysis treatments to ED patients.
Participants
88 of 101 unfunded patients presenting to the ED during the study period consented to participate, resulting in an 87.1% response rate. 65 of these patients were undocumented immigrants.
Main Outcome Measures
Quantitative scores for the 5 subscales of the KDQOL-36 were calculated for the study population.
Results
Measures of physical and mental health in our study population were lower than those published for scheduled dialysis patients. 79.5% of our patients lost employment due to their dialysis requirements. At least 71.4% of the study patients were unaware that they required dialysis before immigrating to the United States.
Conclusions
Quality of life scores were found to be low among our population of undocumented emergent dialysis patients. Our data also provide some evidence that availability of dialysis at no cost is not a primary driver of illegal immigration of ESRD patients to the United States.
Keywords: Kidney Failure, Chronic/ethnology, Kidney Failure, Chronic/therapy, Renal Dialysis, Quality of Life, Emigrants, Immigrants, Undocumented Immigrants
Introduction
Of the 11.7 million undocumented immigrants estimated to be living in the United States as of March 2013, an estimated 15,000 suffered from end-stage renal disease (ESRD) and required regular hemodialysis therapy for survival.1 Hemodialysis is a costly and time-consuming procedure that must be performed multiple times a week in perpetuity; however, the cost of this therapy for every US citizen is fully covered under law by Medicare, Medicaid and other secondary payers.2 Due to their legal status, undocumented immigrants are ineligible for these funding sources and, thus, have difficulty obtaining scheduled dialysis. In some states, including Texas, these individuals are almost exclusively treated in an emergency department (ED) setting. Unlike the ESRD patients who receive outpatient dialysis at regular intervals to keep their chronic disease in check, those who rely on the ED for therapy are only dialyzed after manifesting symptoms of complications such as volume overload, respiratory distress, or severe electrolyte imbalance.
Because treating ESRD requires considerable resources, many studies have examined the burden this disease places on the lives of affected patients. Specifically, these studies investigate health-related quality of life (HRQoL), a “multi-dimensional concept that includes domains related to physical, mental, emotional, and social functioning,”3 using validated, formalized surveys.4 Subsequently, HRQoL data have been linked to patient mortality and future hospitalizations.5 Little research has been done, however, to characterize the population of predominantly unscheduled ESRD patients, especially undocumented patients, who regularly seek emergent dialysis via the ED. The goal of our study, therefore, was to better define the ethnographic composition and assess the HRQoL of the undocumented patients among the unscheduled population presenting to a large county hospital for emergent dialysis.
Methods
Approval for this study was obtained from the institutional review board (IRB) of the University of Texas Southwestern Medical Center (UT Southwestern), and all procedures were in accordance with the ethical standards of the IRB and the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants included in the study. The study was conducted at Parkland Memorial Hospital, a county-funded tertiary care hospital in the Dallas, Texas metropolitan area. The hospital’s main ED, which recorded more than 150,000 visits in 2013, served as the primary entry point for the hospital’s population of unfunded, unscheduled ESRD patients requesting emergent dialysis. In 2013, Parkland administered 9,964 emergent dialysis treatments, an estimated two-thirds of which were provided to ED patients.
Two distinct surveys were chosen to be administered to the unfunded, unscheduled dialysis patients. The first survey, created by the Division of Nephrology at UT Southwestern, featured 21 ethnographic questions on each enrollee’s age, sex, ethnicity, nationality, immigration status, employment status, frequency of ED visits for dialysis, and ED wait times until beginning emergent dialysis therapy. The survey is available from the corresponding author.
The kidney disease quality of life (KDQOL™-36) instrument, previously validated in populations of undocumented Hispanic patients,6 was selected as the second survey and was used to obtain HRQoL data from our study population. Responses to the KDQOL-36 were used to calculate scores for 5 unique subscales for each patient: physical health component summary (PCS); mental health component summary (MCS); burden of kidney disease; symptoms of kidney disease; and effects of kidney disease on daily life.7 A score between 0 and 100 was derived for each of these subscales from an individual’s responses to the 36 questions of this survey. For a given subscale, a higher score corresponded to a superior level of perceived quality of life in that domain.
A group of five research associates worked in shifts to provide 24-hour coverage of the hospital ED and performed all patient enrollment and data collection over a four-week period from July 15, 2013 to August 9, 2013. Unscheduled patients were identified through the Epic Systems (Verona, Wisconsin, USA) electronic medical record as they checked into the ED requesting dialysis. After initial physician evaluation was completed and appropriate measures were performed to stabilize acutely ill patients, research team members approached each candidate patient to attempt enrollment. The study goals and all information necessary for providing informed consent were explained to each prospective enrollee with the assistance of licensed Spanish-language interpreters as needed. Each consented patient received copies of all study documentation in his or her language of preference. Enrolled patients then completed both study surveys, either in written form or by dictating his or her responses to a member of the research team.
Completed surveys were immediately placed into secure storage. Data points were transcribed from the paper surveys, double-checked for accuracy, de-identified, and entered into a password-protected Microsoft Excel (Redmond, Washington, USA) document stored on a secure network. Basic functions of the Excel software were used to organize and manipulate the dataset from the ethnographic survey. An Excel-based spreadsheet tool from the UCLA Division of General Internal Medicine and Health Services Research was used to calculate individual patient, mean population, and median population scores for all 5 subscales of the KDQOL-36 instrument.7
Results
A total of 101 unscheduled dialysis patients were identified upon arrival to the ED during the study period. Of these patients, 88 consented to participate resulting in an 87.1% response rate. For the 13 declining patients, reasons varied for why they were not enrolled in the study, including severe acute illness and unspecified personal decisions to not participate. Baseline characteristics of the surveyed population, drawn from the ethnographic questionnaire, are summarized in Table 1. All surveyed patients identified their ethnicity as Hispanic except one individual who self-identified as Asian. After removing resident aliens and US citizens from further consideration, a study population of 65 undocumented patients remained.
Table 1. Baseline characteristics of the study populationa.
| All respondents | Undocumented | |||
| Ageb | ||||
| Range | 19-79 | 19-79 | ||
| Mean (SD) | 46.3 (13.5) | 45.3 (13) | ||
| Sex | ||||
| Male | 51 | 63.0% | 39 | 65.0% |
| Female | 30 | 37.0% | 21 | 35.0% |
| Ethnicity | ||||
| Hispanic | 86 | 98.9% | 65 | 100.0% |
| Asian | 1 | 1.1% | N/A | |
| Primary language | ||||
| Spanish | 80 | 97.6% | 57 | 98.3% |
| English | 2 | 2.4% | 1 | 1.7% |
| Education | ||||
| None | 14 | 16.9% | 9 | 14.8% |
| < Secondary | 34 | 41.0% | 25 | 41.0% |
| Secondary | 31 | 37.3% | 24 | 39.3% |
| University | 2 | 2.4% | 1 | 1.6% |
| Graduate | 2 | 2.4% | 2 | 3.3% |
| Country of origin | ||||
| Mexico | 69 | 82.1% | 51 | 82.3% |
| El Salvador | 9 | 10.7% | 7 | 11.3% |
| Honduras | 4 | 4.8% | 3 | 4.8% |
| Guatemala | 1 | 1.2% | 1 | 1.6% |
| Philippines | 2 | 1.2% | NA | |
a. The n for each data category varies according to the number of respondents to each survey question.
b. Regarding the data on age, n=84 for All respondents, and n=64 for Undocumented respondents.
Responses from each undocumented patient’s KDQOL-36 survey were used to calculate scores for each of the 5 subscales previously described. Although a significant number of collected surveys contained at least one question that was left incomplete or was marked with multiple responses, the inherent design of the KDQOL-36 instrument allowed for usable subscale scores to be derived despite the omissions. Mean and median scores for all 5 KDQOL-36 subscales are reported in Table 2.
Table 2. Aggregate KDQOL-36 subscale scoresa for the undocumented study population.
| Subscale | Mean | SD | Median | nb |
| Physical health component summary (PCS) | 33.15 | 8.43 | 31.57 | 62 |
| Mental health component summary (MCS) | 42.37 | 9.59 | 40.65 | 62 |
| Burden of kidney disease | 25.78 | 25.28 | 18.75 | 64 |
| Symptoms of kidney disease | 61.56 | 18.19 | 61.46 | 64 |
| Effects of kidney disease on daily life | 59.70 | 22.05 | 61.61 | 64 |
a. Possible scores range from 0-100, where higher values indicate superior quality of life in a given domain.
b. The ‘n’ for each subscale score varies according to the number of respondents who sufficiently completed the corresponding sections of the KDQOL-36 survey.
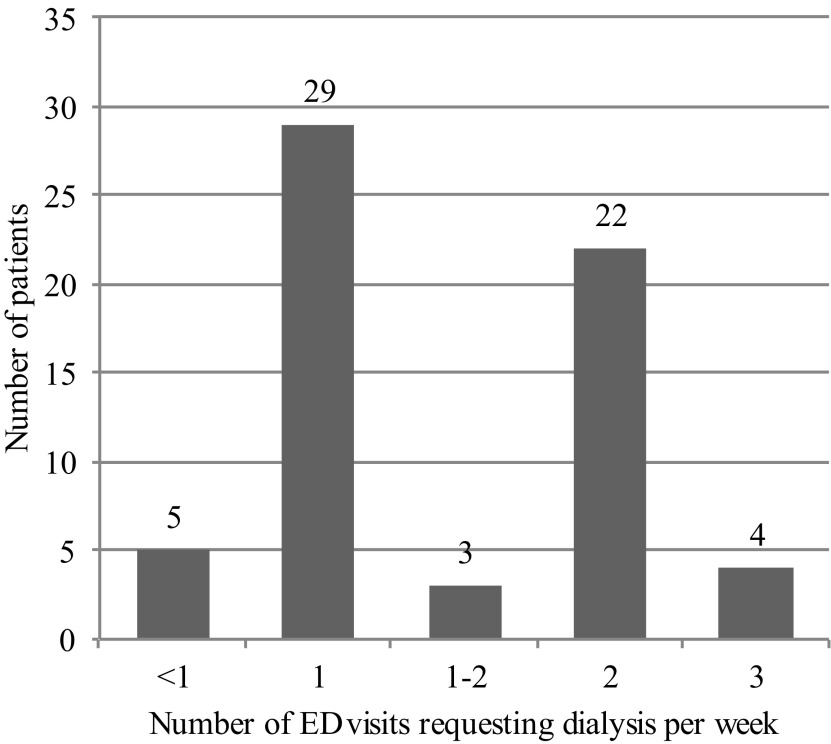
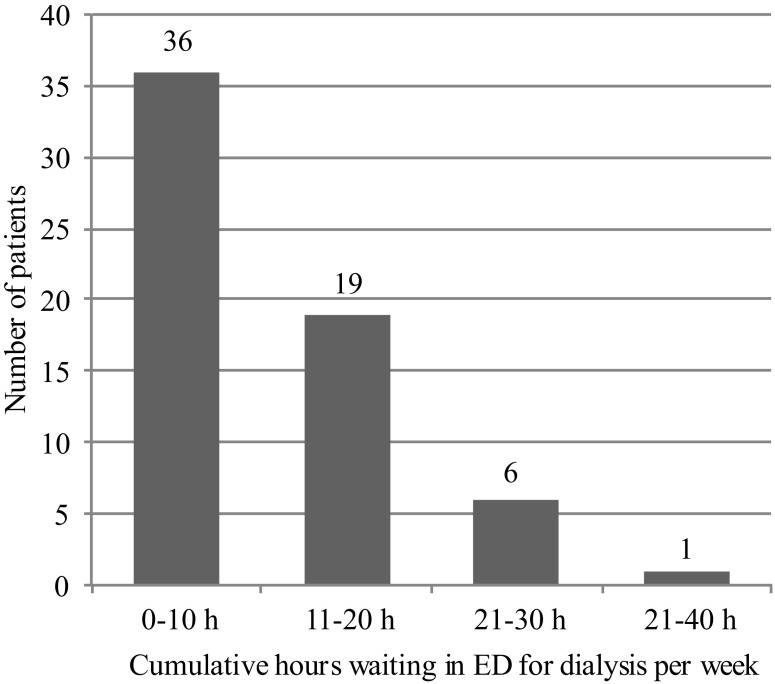
Figure 1 displays the frequency at which patients from our study population presented to the ED requesting dialysis on a weekly basis. Figure 2 illustrates the cumulative weekly ED wait times until dialysis for our study patients. The values in Figure 2 represent the sum of all hours spent waiting across all ED visits during a given week. Importantly, these data refer exclusively to the amount of time spent waiting in the ED prior to obtaining a dialysis chair and do not include the additional 2 or 3 hours spent undergoing hemodialysis.
Figure 1. Weekly patient visits for emergent dialysis, n=63.
Figure 2. Cumulative weekly ED wait times for emergent dialysis, n=62.
In response to a survey question on employment status, 44 of 59 study patients reported having been employed prior to diagnosis of ESRD requiring dialysis. Of these 44 patients who were employed prior to beginning dialysis, 35 (79.5%) reported losing their jobs as a direct result of the time and resource burden of obtaining emergent dialysis.
Two survey questions soliciting dates of immigration and ESRD diagnosis were answered completely by 56 undocumented individuals. When the responses to both questions were compared, at least 40 of the patients (71.4%) were shown to have immigrated to the US prior to being diagnosed with ESRD. Only one patient (1.8%) was demonstrated to have immigrated to the US after receiving an ESRD diagnosis. Due to survey responses, which categorized dates within broad date ranges, it was not possible to correlate both dates for the remaining 15 undocumented patients (26.8%).
Discussion
To the best of our knowledge, this study population constitutes the largest group of undocumented hemodialysis patients surveyed on HRQoL using a validated instrument. Although the collected data reflect only one moment in time within a relatively homogeneous group of patients at a single institution, they can be qualitatively compared with data from other studies of ESRD patients with similar demographics in the United States.
PCS and MCS subscale scores, which represent a group’s perceived physical and mental health, were derived from the KDQOL-36 survey for our study population and compared with scores from a smaller yet comparable group of patients receiving emergent dialysis at another large county hospital in a different major city in Texas.8 In that study by Sheikh-Hamad and colleagues, a group of eight undocumented dialysis patients were surveyed using the KDQOL-SF instrument and compared with a control group of 18 demographically similar patients who were allowed to continue receiving scheduled dialysis at the same institution by special exception.
Median PCS scores in the Sheikh-Hamad study were found to be significantly lower in their emergent dialysis group as compared with their scheduled dialysis group (26.90 vs. 42.96, respectively), with no significant difference found between the median MCS scores of their emergent and scheduled groups (50.61 and 51.78, respectively). In our population, the median PCS score (31.57) was similar to that of the emergent patient group in the Sheikh-Hamad study (26.90), but our population’s median MCS score of 40.65 was notably lower than in either of that study’s groups. This discrepancy in MCS scores may be explained by a difference in the average length of emergent dialysis dependency between the two studies. While all patients in the Sheikh-Hamad study received emergent dialysis for 23 months or less, our population included some patients dependent on emergent therapy for more than a decade.
Strong associations between lower PCS and MCS scores on KDQOL surveys and increased incidence of morbidity and mortality have been described elsewhere.5,9 Therefore, the results of our study suggest that unscheduled dialysis patients may have a poorer prognosis than demographically similar ESRD patients with access to routine dialysis.
Our ethnographic survey revealed that our unscheduled dialysis patients spent a significant amount of time waiting in the emergency department for hemodialysis therapy every week. By comparing the data sets in Figures 1 and 2, an estimated wait time of 5 hours per patient per ED visit was extrapolated. These long wait times and the irregular schedule of emergent dialysis likely contributed to exceptionally low scores on the KDQOL-36 ‘Burden of Kidney Disease’ subscale. Our results further suggest that a patient’s ability to hold gainful employment is greatly impaired by the time requirement associated with seeking routine emergent dialysis. It is noteworthy that 35 of the 44 unfunded patients (79.5%) in our study who were employed prior to developing ESRD reported having lost their jobs as a direct result of their emergent dialysis requirements. As described by Neri and coauthors, dialysis-related unemployment is a major factor contributing to low scores on KDQOL surveys.10
In addition to the social issues surrounding emergent dialysis, economic issues exacerbate and complicate an already suboptimal care delivery model. Long-term treatment of ESRD patients using emergent dialysis has been repeatedly shown to be more expensive than scheduled dialysis.8,11 Additionally, living-donor renal transplantation has been demonstrated to be a feasible and less costly alternative to emergent dialysis, although this process entails its own share of sociolegal challenges,12 which are even more difficult to navigate for undocumented patients.
Emergent dialysis is considered to be inadequate therapy for ESRD.13,14 Emergent treatments frequently fail to meet minimum thresholds of dialysis adequacy as assessed using objective metrics such as Kt/V calculations.8 The standard of care for ESRD consists of perpetual thrice-weekly hemodialysis.15 In contrast, patients routinely treated in emergent fashion receive substantially fewer sessions of hemodialysis on an annual basis than do scheduled patients, and therefore do not receive treatment meeting the standard of care.8
Our data also offer novel insight into one of the most hotly debated sociopolitical issues surrounding the practice of emergent dialysis. An unsubstantiated yet pervasive belief exists that most undocumented immigrants with ESRD immigrate to the United States primarily to receive free hemodialysis in spite of evidence to the contrary from California, which provides scheduled therapy to undocumented patients.12 This theory has long been the basis for refusing scheduled dialysis to undocumented ESRD patients in many communities with high numbers of undocumented immigrants. Of the 56 undocumented patients in our study who provided valid answers to both survey questions regarding dates of immigration and ESRD diagnosis, at least 40 (71.4%) were diagnosed after moving to the United States, with only one patient (1.8%) immigrating after receiving a diagnosis. Even if the 15 patients (26.8%) whose dates of immigration and ESRD diagnosis could not be established were conservatively assigned to the “after diagnosis” group, patients diagnosed after immigration still represent a majority of our survey population. This suggests that obtaining dialysis is not the primary driver of illegal entry into the United States among our population of undocumented ESRD patients.
Our study has several limitations. The study population was limited to the unscheduled patients who presented to the ED during a particular four-week window of time. While we drew comparisons from the literature, we did not survey a matched control population. Additionally, using the KDQOL-36 instrument, selected for its validity in surveying ESRD patients,6 limited the number of previously surveyed populations against which our data could be compared. This meant that while the PCS and MCS scores generated for our population using the KDQOL-36 could be directly compared with scores from other published studies that utilized different versions the KDQOL instrument,7 the three remaining KDQOL-36 subscales scores for our population could only be interpreted qualitatively.
The design of our ethnographic survey also posed limitations. Intended to solicit information on ethnographic topics of interest, deficiencies in the wording of some question prompts and answer choices did not become apparent until the data collection period had ended. For example, the question on time of ESRD diagnosis requiring dialysis listed “1–5 years” as a single answer choice, but the question on time of immigration to the US featured both “1–2 years” and “3–5 years” as possible selections. As such, a temporal relationship could not be established between the two events for 15 undocumented patients who answered both questions. Finally, allowing patients to complete surveys by hand likely contributed to more incomplete responses – and a smaller data set – than would have resulted if the survey questions had been dictated to every patient.
Despite these limitations, this study has in part inspired an initiative at our institution to improve the care of undocumented ESRD patients. A new type of insurance provided by Blue Cross Blue Shield of Texas has allowed for unfunded, noncitizen ESRD patients to receive thrice-weekly scheduled dialysis, and a sizable number of our known unfunded unscheduled ESRD patients have been enrolled in this program. Although the long-term sustainability of this funding is uncertain, an undocumented population receiving scheduled dialysis by this avenue would provide an excellent opportunity to compare data between emergent and scheduled therapies in an otherwise homogenous population.
Conclusion
HRQOL data collected from the largest population of undocumented ESRD patients to date reinforce the myriad of arguments against the practice of emergent dialysis. Providing dialysis in this manner constitutes inadequate therapy, impairs the quality of life of recipients across several domains, and costs more to all relevant parties than superior alternative therapies. Our data suggest that dependence on emergent dialysis contributes to a vicious cycle of employment loss, dependency, and further decline of quality of life. Additionally, our data provide some evidence against fears that scheduling dialysis for unfunded patients will stimulate widespread immigration of undocumented ESRD patients.
Acknowledgments
The authors thank Joseph Berger, MD, Department of Internal Medicine, University of Texas Southwestern Medical Center for his review and assistance with the research and article development.
References
- 1.Rodriguez RA. Dialysis for undocumented immigrants in the United States. Adv Chronic Kidney Dis. 2015;22(1):60-65. 10.1053/j.ackd.2014.07.003 [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez RA, Himmelfarb J, Hall YN. Tragic options and compromised care: undocumented immigrants with ESRD. Am J Kidney Dis. 2012;60(3):335-337. 10.1053/j.ajkd.2012.06.006 [DOI] [PubMed] [Google Scholar]
- 3.Health-Related Quality of Life and Well Being HealthyPeople.gov. https://www.healthypeople.gov/2020/about/foundation-health-measures/Health-Related-Quality-of-Life-and-Well-Being. Accessed September 16, 2016.
- 4.Edgell ET, Coons SJ, Carter WB, et al. A review of health-related quality-of-life measures used in end-stage renal disease. Clin Ther. 1996;18(5):887-938. 10.1016/S0149-2918(96)80049-X [DOI] [PubMed] [Google Scholar]
- 5.Mapes DL, Lopes AA, Satayathum S, et al. Health-related quality of life as a predictor of mortality and hospitalization: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney Int. 2003;64(1):339-349. 10.1046/j.1523-1755.2003.00072.x [DOI] [PubMed] [Google Scholar]
- 6.Ricardo AC, Hacker E, Lora CM, et al. ; CRIC Investigators . Validation of the Kidney Disease Quality of Life Short Form 36 (KDQOL-36) US Spanish and English versions in a cohort of Hispanics with chronic kidney disease. Ethn Dis. 2013;23(2):202-209. [PMC free article] [PubMed] [Google Scholar]
- 7.The KDQOL-36™ Survey. Kidney Disease Quality of Life Instrument (KDQOL). http://www.rand.org/health/surveys_tools/kdqol.html. Accessed March 24, 2015.
- 8.Sheikh-Hamad D, Paiuk E, Wright AJ, Kleinmann C, Khosla U, Shandera WX. Care for immigrants with end-stage renal disease in Houston: a comparison of two practices. Tex Med. 2007;103(4):54-58, 53. [PubMed]
- 9.Lowrie EG, Curtin RB, LePain N, Schatell D. Medical outcomes study short form-36: a consistent and powerful predictor of morbidity and mortality in dialysis patients. Am J Kidney Dis. 2003;41(6):1286-1292. 10.1016/S0272-6386(03)00361-5 [DOI] [PubMed] [Google Scholar]
- 10.Neri L, Rocca Rey LA, Gallieni M, et al. Occupational stress is associated with impaired work ability and reduced quality of life in patients with chronic kidney failure. Int J Artif Organs. 2009;32(5):291-298. [DOI] [PubMed] [Google Scholar]
- 11.Coritsidis GN, Khamash H, Ahmed SI, et al. The initiation of dialysis in undocumented aliens: the impact on a public hospital system. Am J Kidney Dis. 2004;43(3):424-432. 10.1053/j.ajkd.2003.11.004 [DOI] [PubMed] [Google Scholar]
- 12.Grubbs V. Undocumented immigrants and kidney transplant: costs and controversy. Health Aff (Millwood). 2014;33(2):332-335. 10.1377/hlthaff.2013.0462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nzerue C. Between a rock and a hard place. Am J Kidney Dis. 2011;58(4):A28-A29. 10.1053/j.ajkd.2011.08.004 [DOI] [PubMed] [Google Scholar]
- 14.Raghavan R. When access to chronic dialysis is limited: one center’s approach to emergent hemodialysis. Semin Dial. 2012;25(3):267-271. 10.1111/j.1525-139X.2012.01066.x [DOI] [PubMed] [Google Scholar]
- 15.Campbell GA, Sanoff S, Rosner MH. Care of the undocumented immigrant in the United States with ESRD. Am J Kidney Dis. 2010;55(1):181-191. 10.1053/j.ajkd.2009.06.039 [DOI] [PubMed] [Google Scholar]